Acute Glomerulonephritis
-
Upload
jhaziel-bermejo -
Category
Documents
-
view
216 -
download
8
Transcript of Acute Glomerulonephritis

ACUTE GLOMERULONEPHRITIS
By: Jhaziel E. Bermejo

•DEFINITION•CAUSES•LABORATORY•MANIFESTATIONS
INTRODUCTION

DEFINITION
Aka glomerular nephritis, (GN) is a renal disease characterized by
inflammation of the glomeruli, or small blood vessels in the kidneys.
refers to a specific set of renal diseases in which an immunologic mechanism triggers inflammation and proliferation of glomerular tissue that can result in damage to the basement membrane, mesangium, or capillary endothelium.

CAUSES
Post infectious etiologies Streptococcus species
(i.e., group A, beta-hemolytic).

Systemic causes
Vasculitis (ie, Wegener granulomatosis causes glomerulonephritis that combines upper and lower granulomatous nephritides).
Collagen vascular diseases (ie, systemic lupus erythematosus causes glomerulonephritis through renal deposition of immune complexes).
Cryoglobulinemia causes abnormal quantities of cryoglobulin in plasma that result in repeated episodes of widespread purpura and cutaneous ulcerations upon crystallization.

Polyarteritis nodosa causes nephritis from a vasculitis involving the renal arteries.
Henoch-Schönlein purpura causes a generalized vasculitis resulting in glomerulonephritis.
Goodpasture syndrome causes circulating antibodies to type IV collagen and often results in a rapidly progressive oliguric renal failure (weeks to months).
Drug-induced (ie, gold, penicillamine)

Renal diseases
Idiopathic rapidly progressive glomerulonephritis is a form of glomerulonephritis characterized by the presence of glomerular crescents. Three types have been distinguished. Type I is an antiglomerular basement
membrane disease, type II is mediated by immune complexes,
and type III is identified by antineutrophil
cytoplasmic antibody.

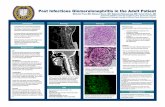
Laboratory tests
Antistreptolysin-O (ASO) Titer. Urinalysis. Renal Biopsy. Is the most
confirmatory diagnostic procedure. Electrolytes, including BUN and
creatinine (to estimate the glomerular filtration rate [GFR]): The BUN and creatinine levels will exhibit a degree of renal compromise.

Complete blood cell count Streptozyme test Erythrocyte sedimentation ratio (ESR)
usually is increased. Urine or plasma creatinine level greater
than 40; decreased renin level is noted. Cultures of throat and skin lesions to
rule out Streptococcus species may be obtained.
Blood cultures

Imaging Studies Radiography Echocardiography renal ultrasonography CT scan

MANIFESTATIONS
Hematuria Hypertension Generalized
edema Proteinuria Oliguria Anorexia
Nausea and vomiting
fatigue and tiring easily,
headaches, twitchy
movements mental confusion
and disorientation.

Diagram presentation
PATHOPHYSIOLOGY

•Antibiotic and antihypertensive drugs•Follow up care•Patient teachings
MANAGEMENT

MANAGEMENT
Antibiotics. Antihypertensive. Bed rest. Increase oral fluid intake.

Antibiotic and antihypertensive drugs
Antibiotics The Penicillin is the DOC in treating acute
glomerulonephritis of a poststreptococcal group A beta-hemolytic etiology.
Penicillin V (Veetids)
Inhibits enzymes and cell wall receptors, resulting in cell wall synthesis inhibition. Other autolytics enzymes are also activated, degrading the bacterial cell wall.

Nonselective beta-blocker with cardioselective alpha1 blocker Labetalol is used for hypertensive
encephalopathy and malignant hypertension. Labetalol (Normodyne)
Has nonselective beta-antagonist and cardioselective alpha1-antagonist effects. Beta-blocking effects predominate, particularly when used IV. Low lipid solubility means bioavailability is reduced by first pass metabolism and enhanced by coadministration of food. Drug is not removed by hemodialysis.

Loop diuretics Loop diuretics are used for hypertensive
encephalopathy with CNS signs and circulatory congestion or pulmonary edema. Furosemide is DOC for this indication.
Furosemide (Lasix)
Inhibits absorption of sodium and water in ascending limb of loop of Henle by interfering with Na+/K+/Cl- channel. An antihypercalcemic effect is mediated by an increased excretion of calcium.

Corticosteroids Methylprednisolone is used for
nonstreptococcal etiologies of acute glomerulonephritis, particularly in lupus nephritis and in idiopathic progressive glomerulonephritis.
Methylprednisolone (Medrol)
Has anti-inflammatory effect and is immunosuppressive. Metabolized by hepatic transformation and renal excretion.

Follow-up
Further Outpatient Care Urinalysis at 2, 4, and 6 weeks and at 4, 6,
and 12 months Cessation of follow-up care when urinalysis
is normal Blood pressure monitoring during each visit Serum creatinine level monitoring at 2, 6,
and 12 months Serum complement usually normal by 6
weeks

Patient Education
Upon discharge from the ED, patient education should emphasize the importance of close follow-up care.
Indicate that strenuous exercise should be avoided because exercise can induce proteinuria, hematuria, and cylindruria (renal cylinders or casts in the urine) in healthy individuals.
Limit the patient to a diet with no added salt until edema, hypertension, and azotemia clear.
Restrict fluids in patients with significant edema. Restrict protein in the presence of azotemia and
metabolic acidosis (ie, approximately 0.5 g/kg/d). The patient should avoid high-potassium foods.