A service improvement focused on frailty using an R&D approach, pop up uni, 3pm, 3 september 2015
-
Upload
nhs-england -
Category
Healthcare
-
view
668 -
download
1
Transcript of A service improvement focused on frailty using an R&D approach, pop up uni, 3pm, 3 september 2015
A service improvement focused on
Frailty using an R&D approach
facilitated by AQuA Lindsey Darley - Directorate Manager for North Manchester Community Services
Carol Kavanagh - Intermediate Care Manager, North Manchester
Adele Markland - Improvement Advisor, AQuA
Suzanne Wilson – Reablement Manager
Who we are Pennine Acute Hospitals NHS Trust •North East sector of GM – population 820,000 across urban and rural areas
•Approx 9,000 staff, approx 300 in North Manchester Community services (adults) •4 hospitals, 3 A&E departments, 1 Urgent care Centre
•4 CCG’s and 4 Local Authorities
Advancing Quality Alliance (AQuA) • Established in 2010 as a NHS health and care quality improvement
organisation www.AQuAnw.nhs.uk
• Our aim is to transform health and care quality • Membership: 73 commissioner and provider organisations, plus consultancy work
across the UK
National Context • Policy drivers:
– Five Year Forward View – Francis report
– Keogh report – NHS England – Safe,
compassionate care for frail older people using an integrated care pathway
• Demographic drivers:
– Ageing population • Guidance from clinical bodies
• Financial drivers
IHI 90 Day R and D Process
What it is
• Quick way to research innovative ideas to assess their
potential for rapid cycles of change
• Answers specific question
• Timeframe for investigation (90 days)
• Within each cycle a number of ideas are tested to find the
best solution
• Helps identify risk and factoring this into testing
What is isn’t
• Large scale transformational change
• Stakeholder engagement is important. If you find yourself
having to undertake a considerable engagement process
you should question whether it is R&D
• R&D is about discovery, not about a plan for
implementation. You may discard many ideas you have
tested but will be able to hone down to more intensive
tests in a narrower field.
Institute for Healthcare Improvement 90-Day Innovation Process
http://www.ihi.org/about/Documents/IHI%20Innovation%20Summary.pdf
IHI 90 Day R and D Process
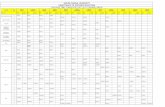
90 day cycle Phase What is involved
30 days Scan • Scanning the literature
• Conducting key interviews with relevant individuals /organisations to understand the dimensions of the problem or issue
• At the end of the 30 days AQuA workbook documentation is produced which includes: • Aim of the project
• Description of the current landscape • A set of theories for how to solve the problem
• The specifications for an effective solution • Bibliography
60 days Focus • A move from theory into practice
• Testing theories at the front line and refining details about what actually works • A key activity at this stage is describing the key components of the system that perform ‘to
specification’ • Creating a driver diagram to demonstrate learning
90 days Summarise
and disseminate
• Time spent:
• Concluding tests • Summarising lessons learned
• Preparing final report
Cycle 1
1/07/14 – 30/09/14
Cycle 2
1/10/14 – 31/12/14
Cycle 3 01/01/15 – 24/03/15
Scan
01/07 -31/7
Focus 01/08-31/8
Summarise and
disseminate 01/09-30/09
Scan 01/10-31/10
Focus 01/11-30/11
Summarise and
disseminate 01/12-31/12
Scan 01/01-31/01
Focus 01/02-28/02
Summarise and
disseminate 01/03-24/03
Wo
rksh
op
3
0/0
9
Wo
rksh
op
0
6/0
1
Wo
rksh
op
2
4/0
3
Coach support: - Weekly calls
- Monthly visits Participating site support:
- Monthly webexes?
Additional support: Analytics
Improving the patient experience Clinical lead
Master classes and visits as appropriate
AQuA’s R&D Approach
Coach support: - Weekly calls
- Monthly visits Participating site support:
- Monthly webexes?
Coach support: - Weekly calls
- Monthly visits Participating site support:
- Monthly webexes?
Local Context
North Manchester focus
•Population – very diverse, very deprived, frailer at a younger age
•Living Longer Living Better programme of transformation
•New Delivery Model for Frail Older People and Adults with Dementia •Re-design of local Intermediate care and Reablement teams
•North Early Implementer for the city of Manchester •Limited numbers of COTE physicians
•No focus on frailty in PAHT or MCC
City of Manchester Aim
“To understand how identifying frailty can impact on a
persons choice of care pathway”
North Manchester Aim
“To assess frailty within Intermediate Care and Crisis
Services to ensure patients are referred on to the correct
pathway”
Intermediate Care Locations
Team
• Crisis Response
• Home Pathway
• Henesy House
• ICT Suite (opened Nov 2014)
Function • 72hr intervention with a 2 hour response
time to people with a medical or social crisis and at serious risk of admission to hospital.
• Intermediate Care within a person’s home setting.
• 15 bedded residential Intermediate Care unit with GP input.
• 9 bedded Enhanced Intermediate Care unit, nurse led with GP input.
Cycle 1 Jul-Sep 14
1. Identified a frailty tool
2. Used Edmonton Frail Scale (EFS) tool with patients referred to:
- Intermediate Care Unit – Henesy House
- Intermediate Care at Home
- Crisis Response
3. Analysed impact of tool on a patients pathway
Cycle 2 Oct-Dec 14
1. Continued to use EFS with all teams from cycle 1 then started to test with ICT Suite
2. Reviewing patient outcomes at day 30 and day 91 to see if there is any correction with a pathway
3. Undertook a focus group with practitioners to understand how a frailty tool impacts on practitioners decision making process
Cycle 3 Jan-Mar 15
1. Continued to use EFS with all teams from cycle 1 and 2 then started to test with Reablement
2. Training for Reablement staff
3. Starting to link work into Primary Care via CGAs
4. Sharing the learning from this work with internal and external networks
5. Reviewing the outcomes from the project to identify what is needed to make the connection across palliative areas
What we did…
Usability
• How easy was the tool to use?
• How long did the tool take to complete?
• How would the tool work in other services outside Intermediate Care?
Output from the tool
• How is frailty scored?
• How reliable is the frailty score?
• How could information from the tool be used to inform what pathways patients should be referred on to after Intermediate Care?
Experience
• What did patients think of the tools?
• What did staff like or dislike about the tools?
Frailty tools evaluation criteria
The team
were testing
the tools
against
the specific
criteria of:
Summary of Tools
Groningen Edmonton Rockwood
Usability
• 10 minutes
• Easy to complete and self
explanatory
• Could w ork in a IMC, hospital
or community environment
• 10 minutes
• Easy to complete and self explanatory
• Could w ork in a IMC, hospital or community
environment
• 15 to 30 minutes
• Little harder to complete as no supporting
descriptions to start the conversation w ith
patient
• Could w ork in a IMC, hospital or
community environment
Output from
the tool
Score >= to 4 indicates frailty
4/15 (Patient 1) Age 81
4/15 (Patient 2) Age 93
4/15 (Patient 4)Age 98
6/15 (Patient 3) Age 94
6/15 (Patient 5) Age 82
Not frail
5/17 (Patient 1) Age 81
4/17 (Patient 2) Age 93
Apparently vulnerable
6/17 (Patient 3) Age 94
7/17 (Patient 4)Age 98
Mild frailty
8/17 (Patient 5) Age 82
• Couldn’t score the frailty of a patient
• Patients scored themselves higher on the
function questions than a professional
w ould
Experience
Patient views:
• Patients didn’t mind
answ ering the questions and
w ere happy w ith the format
Staff view:
• All 6 staff preferred this tool
Patient views:
• Patients didn’t mind answ ering the questions and
w ere happy w ith the format
Staff view:
• Staff liked the practical tests and the frailty scores
w ere reflective of how they w ould assess patients
• Concerns about how the practical tests w ould
w ork w ith patients w ith cognitive impairment
Patient view:
• 2/5 patients like this tool
Staff view:
• This tool generated lots of discussion e.g.
“I rode a bike until I was 96 and I still like
going dancing”
• Some of the pictures are misleading or
slightly unpleasant
What the Data Shows
• The services are achieving what they were intended and commissioned to do
• Patients are travelling within the correct pathways
• Provides and understanding of the impact of frailty levels on other services
• Has the potential to demonstrate acuity at a service level over a period of time
• It supports clinicians to recognise patients that are more suited to a palliative approach to care
• Moderate and severely frail patients are moving to palliative care pathways, recognising this shifts a focus of care and supports continuity
• Can inform commissioning plans at a population level
What is the impact of using a
frailty tool on practitioner
decision making?
Learning: • Has hi-lighted the ‘red flags’ of frailty and heightened
awareness • No impact on clinical decision making
• No value as an outcome measure within individual services
• It provides a good snapshot of levels of dependency and would appear to demonstrate acuity.
• Enhanced ICT have used HCA’s to administer the tool, and have found it supports more focused feedback
• Could be used to trigger a CGA request across all services.
• Use of a frailty tool has allowed some practitioners to start thinking differently in relation to more severely frail patients, having palliative care requirements.
• Worthwhile to consider identifying ‘less frail’ people who may benefit from a more preventative approach.
A focus group comprising of:
• Mix of professions – nursing, Occupational Therapy, Physiotherapy
• Across the range of Intermediate Care services.
Questions included:
• What difference does the tool make to practitioners decision making?
• How has the tool been used?
• Did the tool influence the MDT approach?
• What pathw ays are frail patients referred on to?
• How transferable is the tool to other services?
• Did the outcome make a difference to patient care?
• What questions is it raising for staff about frailty?
• What matters to us?
• What are the key learning from the measurements?
• What are the key learning form the outcomes?
• What are the next steps?
• Do w e test something new ?
What we did next… • CGA’s - Explore the triggers for a CGA, how primary care can support a CGA,
gaps in CGA information in Intermediate Care
• Use of the frailty score across the whole pathway – changes between point of entry and point of discharge.
• Palliative needs – exploring further how identifying frailty can support a shift in care when it is required
• Expand the use to other services – particularly Re-ablement who work alongside Intermediate Care, and District Nurses as high referrers and onward referrals.
• Focus on the ‘less frail’ and further preventative approaches.
• Links to levels of dependency – test how this relates to activity and intensity of input, and acuity across the services pre and post a service change.
Sustainability and Spread –
March 2015 Total score – 53.9
0.0
4.0
8.0
12.0
16.0Benefits
Credibility of the evidence
Adaptability
Monitoring progress
Involvement and training
Behaviours
Senior leaders
Clinical leaders
Fit with goals and structure
Infrastructure
Portal Diagram
Factor Score
Maximum Score
CQUIN CCG recognising the importance of addressing frailty and embedding this within commissioning
of services
1: To identify and assess frailty within North Manchester community
Intermediate Care, Social Care and Crisis Response Services.
2: Identification of Severe Frailty within the community crisis response
service and onward referrals to the Enhanced Community Palliative care
team.
CQUIN
CQUIN Sector wide CCG’s recognising the importance of addressing frailty and embedding this within
commissioning of services
1: Development of a vision and strategy for frail elderly populations across the NE sector
CQUIN
Frailty Champion for North
Manchester Community Services Voice
Education and Training
Supporting and Leading with others
Clinical Impact of current evidence and research
Influencing strategic development and vision around frailty
Integrated health and social
care delivery End to end CASS pathway
Screening at assessment and discharge
Integrated Key Performance Indicators
Embedded in documentation
Empowered HCA’s and Reablement staff
Informing decisions and discussions about long term care
Sustainability and Spread –
September 2015 Score – 91.7
0.0
4.0
8.0
12.0
16.0Benefits
Credibility of the evidence
Adaptability
Monitoring progress
Involvement and training
Behaviours
Senior leaders
Clinical leaders
Fit with goals and structure
Infrastructure
Portal Diagram
Factor Score
Maximum Score
Outcomes for North
Manchester People
• Frailty Champion raising the profile of frailty across services
• Frailty screening is ensuring the right pathways are identified for
individuals
• Pathways are tailored for their needs in context to degrees of frailty
• A more rounded picture of individuals is apparent
• Hi-lighted individuals perception of their frailty
• Re-focused care on people as individuals
Reminder: Why are we doing this?
“Frailty, understood as a vulnerability state with an increased risk of adverse
outcomes, can be quantified. This method of quantifying frailty can aid our
understanding of health and frailty related health characteristics and outcomes
in older adults” (Searle et al, 2008)
Outcomes for North
Manchester Staff • Developed skill and knowledge in understanding frailty and its impact
• Engaged staff to be part of the big picture in relation to Frailty
• Demonstrates acuity • Created a ‘common language’, binding practitioners and managers to a
common goal
• Provide non-registered staff with a framework for a conversation with a person, enabling a story to be told
• Recognises a shift from active rehabilitation to a palliative rehabilitation approach
• Discrepancy between customer and staff scores on the screening tool generated conversations
• Highlights when a Comprehensive Geriatric Assessment is • required
Outcomes for North
Manchester Commissioners
• Provides an evidence base for commissioning on a needs based approach
• Clear understanding of how frailty links to appropriate pathways
• Supports future commissioning plans for services more accurately
understanding need
• Provided assurance of services targeted appropriately
• Demonstrates changes in acuity and dependency over time, enabling
evidence based adjustment to local commissioning plans
Benefit for AQuA Members Highlights:
• Topics have created a breadth of learning
• Opportunities for individuals to develop clinical leadership and quality improvement knowledge
• Developed staff confidence around new ways of working
• Teams valued the opportunity to test small cycles of change in a safe environment and on a topic that was important to them
• Sites benefitted from the research element of the process as improvement projects don’t always include this
Lessons learnt:
• Sites benefitted from the research element of the process as improvement projects don’t always include this
• R and D process is not easily applied to all types of projects
• Ok to test theories which don’t work in reality
• Small test of change provide ownership
AQuA’s 12 top tips to aid with
successful R and D cycles
1. Be clear from the outset who your project team is 2. Have a clear ‘Aim’ and which all stakeholders are signed up to 3. Have regular meetings and calls with the project team 4. Patient and carer participation is a must, and this needs to involve more than passive
activities like a questionnaire 5. This is about testing small cycles of innovative change, not large scale redesign 6. Be clear about what you want to deliver within the cycle and any tests you do need to
be tested against your specification 7. Collect baseline and outcome measures 8. Make sure people who need to know, know what is happening 9. Engage with key stakeholders to promote your work 10.Speak to people who have tried and tested similar things 11.Celebrate successes, but also feedback on challenges as this will provide a wealth of
learning 12.Share your story; consider who you want to share your story with and how the story
should be framed
Why has it been a success for Integration?
• Strong interaction and collaboration between health and social care
• Takes local politics out of the equation
• Frailty is now very much in the social care agenda, forming part of the MCC Adult Social Care Improvement Programme
• Developing work with NM GP’s– generating real conversation and intrigue from this piece of work
• Common aim & common outcome measures
• Closing the gap on missed opportunities by collecting discharge destinations across health and social care
• Frailty is made real in strategic terms
Not stopping and building on
from this • 2 PDSA cycles led by frailty champion
• Focus on the ‘less frail’ -self care options and further preventative approaches
• Links to palliative care with Active Case Managers
• Education
• Use data to challenge current thinking
• Testing in primary care
Not stopping and building on
from this • Frailty training package roll out from September 1st
onwards, following CASS roll-out
• Frailty Network
• Monthly reporting across CASS pathway
• Roll-out into Heywood Middleton and Rochdale
• Link into secondary care Integrated Discharge Teams to support pathway identification
• Aim for strategic buy-in for developing a Manchester wide Frailty strategy
Team reflection and learning
Improving outcomes and pathways for patients has been
central to this project and remains central
Has developed a practice forum and
brought people together who have
not worked together before
Made me want to be a clinician again.
Sophie Wallington Jason Holland Jen Littler Amelia Smith
Paul Teale Anne Nicholas Suzanne Wilson
Lucy Degisi
Acknowledgments
Contact details
Lindsey Darley
Pennine Acute Hospitals NHS Trust
Directorate Manager for North Manchester Community Services
Carol Kavanagh
Pennine Acute Hospitals NHS Trust
Intermediate Care Manager
Adele Markland
Advancing Quality Alliance (AQuA)
Improvement Advisor
Contact Details