2.13.12Health Plan Week
description
Transcript of 2.13.12Health Plan Week
Volume 22, Number 6 February 13, 2012
Published by Atlantic Information Services, Inc., Washington, DC • 800-521-4323 • www.AISHealth.comAn independent publication not affiliated with insurers, vendors, consultants or associations
3 Well Point No Longer Feelin’ Sassi; Another Top Exec Gets Pink Slip
3 Insurers Get Until Sept. to Create Consumer-Friendly Documents
4 Financial Briefs
5 Table: Health Net’s Stock Price Kicks Off 2012 With 24% Jump
7 Health Plan Briefs
Groups Want Generous, Yet Affordable, Essential Health Benefits, Larger Fed Role
Comments filed in response to CMS’s Dec. 16 bulletin on essential health benefits (EHBs) encourage states to strike a balance between comprehensive and affordable benefits. Other commenters want the federal government to take a more central role in developing standards for states to follow.
Several industry analysts tell HPW that developing appropriate standards are cru-cial to the overall success of the health reform law. And although the final regulation will likely please some and leave others dissatisfied, they add that HHS is not likely to make drastic changes for fear of a political backlash.
Benefit standards are “at the center of health reform failure or success,” says Chip Kerby, an attorney with Washington, D.C.-based law firm Liberte Group. “If the [final] definition of essential health benefits is too broad versus too narrow, it has cascading effects: The broader it is, the more expensive it’s going to be — [and then] will individu-als buy it?”
Kerby adds that while major reforms likely will take years or more to implement, insurance companies have much less time. By Oct. 1, 2013, insurers must be ready to
Contents Utilization Uptick, Greater Regulatory Scrutiny Could Spark Stormy Rate Battles
Nearly two years of low medical utilization — combined with more regulatory scrutiny, reductions in administrative expenses and increased pressure on providers to improve efficiencies — have helped many health insurers hold rate increases to single digits.
But a storm is brewing. At a conference in Boston this month, Martha Temple, presi-dent of Aetna Inc.’s New England market, said that sometime in 2012 or 2013, utiliza-tion could “tick up to historic levels,” according to a Feb. 9 article in The Boston Globe. And that could prompt double-digit rate hikes, she warned.
But any rate increase requests could be met with greater regulatory scrutiny than ever. Since September, federal regulators have been able to examine rate hike requests, although they lack the authority to reject them. And by June 1, HHS intends to publish state-specific thresholds for rate increases in the small-group and individual markets. HHS has been working with the National Association of Insurance Commissioners to determine what to look at when determining state-specific thresholds. In some cases, state thresholds could be higher than 10%.
Those new thresholds will take effect in September.Jesse Caplan, an attorney with the law firm Epstein Becker & Green, says it’s dif-
ficult to determine how effective the federal rate review program has been so far and whether it will influence future rate-hike requests. Since September, the federal gov-ernment has cited only a half-dozen rate filings by insurance carriers as excessive. The insurers, however, argued the rates were justified, and ultimately none was rescinded or reduced, he says.
continued on p. 5
Timely Business, Financial and Regulatory News of the Health Insurance Industry
Managing Editor Steve Davis [email protected]
Editor Jonathan Block
Associate EditorBJ Taylor
Executive Editor Jill Brown
Quarterly spreadsheets of financial data for 50 top health plans — free with your HPW subscription — are archived on your subscriber-only Web page. Log in at www.AISHealth.com/newsletters/healthplanweek and click on “Key Financial Indicators” in the “Subscriber Services” box on the right.
2 Health Plan Week February 13, 2012
go live with their plans for health insurance exchanges. “Between now and then, all of this stuff needs to be lined up and all insurance companies need to come up with plans and price tags,” he tells HPW.
Besides drawing feedback from stakeholders and in-dividuals, the bulletin also drew comments from a group of seven Democratic congressmen, led by Rep. Henry Waxman (Calif.), ranking member of the House Commit-tee on Energy and Commerce.
In their letter, the lawmakers expressed frustration with HHS for delegating the definition of essential health benefits to the states, noting that when the legislation was being drafted, they intended it to be a decision made by the feds.
“While we understand the goal of balancing compre-hensiveness and affordability, and ensuring an appropri-ate role for state input, we would reiterate that one of the primary goals of the Affordable Care Act (ACA) was to create a consistent and comprehensive level of coverage for people across the country,” the lawmakers wrote, adding they have concerns about delegating EHBs to the states and giving more discretion to insurers.
When the bulletin came out in December, it pro-posed that states use an existing health plan to deter-mine benefits that must be included in individual and
small-group plans beginning in 2014 (HPW 12/26/11, p. 1) . However, two consultants interviewed by HPW say punting the decision of what benefits to include could end up making coverage less affordable.
“I would tend to agree that the federal government does need to make a decision. [Otherwise] it defeats the purpose of the ACA to have potentially 51 different inter-pretations of what essential health benefits are,” Chantel Sheaks, a principal in government relations in Buck Con-sultants’ Washington, D.C., office, tells HPW. “When you require having different benefit packages and the more expansive it is, an insurer loses economies of scale.”
She and Kerby agree that the feds may have decided to leave the decision to the states after the flak the Obama administration received when it said birth control would be treated as a women’s preventive benefit. That an-gered some religious groups because the determination resulted in a mandate for some affiliates of religious organizations to cover contraceptive items. However, the administration tweaked its policy Feb. 10 to appease the groups.
“This is the most important decision that has to be made and no one is making it.…[The feds] are putting it off,” Kerby says. “If you’re going to do health reform and make the feds in charge of it, you have to have someone [there] make decisions.”
AHIP Wants Appropriate BalanceIn its comments, industry trade group America’s
Health Insurance Plans (AHIP) said it wants HHS to ensure that benefit packages are affordable for individu-als and small businesses. And while AHIP supports the idea of allowing states flexibility in selecting a bench-mark plan, the group says that after a two-year transition period, “the public policy goal should be to support an affordable evidence-based benefit package reflective of the 10 categories included in the ACA.”
In addition, AHIP wants HHS to examine the cost impact of the benchmark approach during the two-year transition period, focusing on affordability for small busi-nesses and families buying coverage on their own. The group also contends that the benefits should be based on the best available scientific evidence and clinical practice.
Beginning in 2016, AHIP suggests that HHS exclude state-mandated benefit requirements that go above and beyond the reform law’s 10 categories. Along with the cost impact, AHIP cited “the lack of strong medical evi-dence on the safety, effectiveness, and value of many state mandates.”
Because developing new products can take between 12 and 18 months, AHIP recommends that HHS set a deadline of June 30 for states to select an EHB bench-mark. Also, the organization wants HHS to issue guid-
Call Bailey Sterrett at 202-775-9008, ext. 3034 for rates on bulk subscriptions or site licenses, electronic delivery to multiple readers, and customized feeds of selective news and data…daily, weekly or whenever you need it.
Health Plan Week (ISSN: 1937-6650) is published 45 times a year by Atlantic Information Services, Inc., 1100 17th Street, NW, Suite 300, Washington, D.C. 20036, 202-775-9008, www.AISHealth.com.Copyright © 2012 by Atlantic Information Services, Inc. All rights reserved. On an occasional basis, it is okay to copy, fax or email an article or two from HPW. But unless you have AIS’s permission, it violates federal law to make copies of, fax or email an entire issue, share your AISHealth.com subscriber password, or post newsletter content on any website or network. To obtain our quick permission to transmit or make a few copies, or post a few stories of HPW at no charge, please contact Eric Reckner (800-521-4323, ext. 3042, or [email protected]). Contact Bailey Sterrett (800-521-4323, ext. 3034, or [email protected]) if you’d like to review our very reasonable rates for bulk or site licenses that will permit weekly redistributions of entire issues.
Health Plan Week is published with the understanding that the publisher is not engaged in rendering legal, accounting or other professional services. If legal advice or other expert assistance is required, the services of a competent professional person should be sought.
Managing Editor, Steve Davis; Editor, Jonathan Block; Associate Editor, BJ Taylor; Executive Editor, Jill Brown; Publisher, Richard Biehl; Marketing Director, Donna Lawton; Fulfillment Manager, Corey Hughes; Production Editor, Carrie Epps
Subscriptions to HPW include free electronic delivery in addition to the print copy, quarterly Key Financial Indicators for major health plans (in print and posted on the subscriber Web page), e-Alerts when timely news breaks, and extensive subscriber-only services at www.AISHealth.com that include a searchable database of HPW content and archives of past issues.
To order an annual subscription to Health Plan Week ($537 bill me; $507 prepaid), call 800-521-4323 (major credit cards accepted) or order online at www.AISHealth.com.
February 13, 2012 Health Plan Week 3
ance to states on selecting benchmark plans, as well as on standards on cost-sharing and actuarial value, as soon as possible.
Lingering questions remain over the level of flex-ibility states will have in terms of setting benchmarks, an issue that directly impacts insurers that want to move forward, says Jennifer Kowalski, a director in the health reform practice at Washington, D.C.-based health care consulting firm Avalere Health, LLC.
“I think there’s a real need to strike a balance be-tween comprehensive benefits that give people the cov-erage they need, while at the same time [insurers] want to be responsive to the marketplace and want to offer plans consumers are able to afford while offering a range of options,” she tells HPW.
Coalition Wants Flexibility in CoverageIn its comments, the Essential Health Benefits Co-
alition, which represents employers, pharmacy benefit managers and health plans, echoed many of the sug-gestions brought by AHIP. However, the group strongly emphasizes that benefits should be evaluated from a cost and medical effectiveness perspective, noting that this recommendation also was made by IOM.
In addition, the group says that the benefits package should not limit cost-sharing tools available to employers that allow them to offer affordable health coverage. The coalition also argues that the EHB should include only current benefits in effect as of March 1, 2012, and new state mandates should not be allowed to be included retroactively (HPW 2/6/11, p. 8).
The organization warns that a final rule that does not balance benefits with affordability for employers and
Web addresses cited in this issue are live links in the PDF version, which is accessible at HPW’s subscriber-only page at http://aishealth.com/newsletters/healthplanweek.
employees could negatively impact employers’ ability to create new jobs.
Another element that should not be left out of the final reg, says Paul Fronstin, Ph.D., a senior research as-sociate at the Employee Benefit Research Institute, is that the benefits included should be spelled out enough so that people understand their coverage.
There needs to be “a level of granularity so individu-als know…what services are covered,” he tells HPW. “But getting to that level of granularity is a challenge. Most plans don’t provide that level of granularity, [and it’s] not going to happen overnight.”
Contact Kerby at [email protected], Sheaks via Ed Gadowski at [email protected], Kowalski at [email protected] and Fron-stin at [email protected]. G
WellPoint No Longer Feelin’ Sassi; Another Top Exec Gets Pink Slip
Brian Sassi, executive vice president of market-ing and president and chief executive for WellPoint’s consumer business, was terminated “without cause,” according to an 8-K filed with the Securities & Exchange Commission late Feb. 8. Sassi will remain with the com-pany until early next month “to assist in the transition of his duties,” according to the filing. A replacement was not named.
Over the past 18 months, WellPoint has eliminated several top executives due to “execution missteps and the public affairs issues” that surfaced during the lead-up to the health reform law, notes Ana Gupte, an equities analyst at Sanford C. Bernstein.
Health insurers have a little more breathing room to develop and distribute standardized and easy-to-understand health coverage-summary documents as required by the reform law. In a joint press conference on Feb. 9, HHS, the Dept. of Labor and the Dept. of Treasury issued the final rule, which gives insurers until Sept. 23 to comply, rather than the March 23 date set by the reform law.
“For too many Americans, choosing a health plan means reading through a human resources booklet usually the size of a small phone book. It can be con-fusing to compare plans,” said acting CMS Adminis-trator Marilyn Tavenner.
In a letter, the trade association America’s Health Insurance Plans (AHIP) said the rule would cost its members $188 million in initial implementation costs and $194 million for “one year of ongoing operations,” well above the three-year cost estimate of $156 million in the proposed rule. AHIP complained that the time-line is still too short and had encouraged CMS to give employers and insurers 18 months to develop the new documents.
To see AHIP’s statement on the rule, visit the newsroom at www.ahip.org. View the final rule at www.ofr.gov/inspection.aspx and the template at http://cciio.cms.gov/resources/other/index.html#sbcug.
Insurers Get Until Sept. to Create Consumer-Friendly Documents
continued
4 Health Plan Week February 13, 2012
In a Feb. 9 note to investors, CreditSuisse analyst Charles Boorady noted that Sassi heads “the most im-portant business unit” within WellPoint, and added that “talent management” continues to be a key challenge for the company. WellPoint is expected to replace Sassi with someone from the outside. One analyst expressed sur-prise that Sassi was let go without a replacement.
WellPoint’s fourth-quarter 2011 earnings were sig-nificantly impacted by an adverse-selection issue in its Medicare Advantage (MA) regional PPO in northern California (HPW 1/30/12, p. 3).
Among other things, Sassi oversees WellPoint’s Medicare business. While the SEC filing doesn’t specify whether this was related to the termination, several equi-ties analysts tell HPW that it probably was.
WellPoint “had some execution issues on pricing in their Medicare book of business, and the termination appears to be largely related to that,” Gupte says, adding that individual and Medicaid segments also have seen recent margin pressure.
WellPoint’s Medicare business has been “very incon-sistent” over the past few years, and in 2011 didn’t per-
form as well as other large MA carriers such as Humana Inc., adds Matt Coffina, a health care industry analyst at Morningstar, Inc. “It’s hard to say how much of the northern California MA underwriting issue can really be blamed on the senior executive. Occasional underwrit-ing missteps are probably inevitable, particularly given a rapidly changing competitive environment and benefit designs,” he says. “However, it comes with the territory of being the guy on top.”
A spokesperson for WellPoint said the company doesn’t comment on executive departures.
In October 2010, WellPoint announced the termina-tion of Dijuana Lewis, who was one of the company’s top-paid executives. Two months later, the company unexpectedly dismissed Bradley Fluegel, executive vice president and chief strategy and external affairs officer, and Cynthia Miller, executive vice president and chief actuary (HPW 12/6/10, p. 3). Miller, who had been with the company for 23 years, testified before a House sub-committee after the company’s California subsidiary came under fire for steep rate hikes in the individual market (HPW 3/1/10, p. 1). In its 2010 filing, WellPoint
Subscribers who have not yet signed up for Web access — with searchable newsletter archives, Hot Topics, Recent Stories and more — should click the blue “Login” button at www.AISHealth.com, then follow the “Forgot your password?” link to receive further instructions.
u Humana Inc. reported strong fourth-quarter 2011 results Feb. 6 as membership gains and lighter medical utilization helped boost earnings 86% compared with the year-ago period. Hu-mana’s fourth-quarter profit of $199 million ($1.20 a share) handily beat the $107 million (63 cents a share) from the fourth quarter of 2010. In addition, the insurer’s medical loss ratio (MLR) fell to 81.8% from 84.5% a year earlier. Medicare Advantage (MA) membership rose 12% or 179,600 during the year, to 1.64 million by Dec. 31. Some of that gain — 12,100 members — was due to Humana’s acquisition of MDCare, which was completed on Dec. 30. Humana also boosted its 2012 earnings per share (EPS) projec-tion 20 cents to $7.70 and projected MA enrollment would grow between 185,000 and 195,000 by the end of the year. In a note to investors, Citigroup Global Markets analyst Carl McDonald wrote that “the big picture has improved for Humana,” adding the MA growth could mean the insurer will exceed its 2012 EPS projection. Visit www.humana.com.
u Medicaid provider Centene Corp. beat Wall Street expectations for its fourth-quarter earnings as profit grew 19% compared with the prior-year period, driven by new business in three states. Centene on Feb. 7 posted net income of $30.1 million
(57 cents per share) for the fourth quarter of 2011 compared with $25.4 million (50 cents per share) for the same period the year before. Revenue also rose 28% to $1.51 billion from $1.18 billion. Analysts were expecting earnings of 55 cents per share on $1.43 bil-lion in revenue. Total membership in 2011 increased to 1.82 million, up from 1.54 million at the end of 2010. The insurer’s MLR also declined 0.3 percentage points year-over-year to stand at 85.2%. Centene also maintained its 2012 EPS guidance of between $2.60 and $2.80. Visit www.centene.com.
u Coventry Health Care, Inc.’s fourth-quarter earn-ings fell 43% as enrollment declined compared with the prior-year period as its MLR rose for both the quarter and full-year 2011. Coventry reported a profit of $85.7 million (60 cents a share) down from $150.3 million ($1.01 a share) a year earlier. Analysts had been expecting earnings of 63 cents per share on just over $3 billion in revenue. Overall membership also declined nearly 7% to 4.76 million from 5.13 mil-lion a year earlier. For 2011, the insurer’s MLR was 82.1%, up from 79.4% a year earlier. For 2012, Coven-try projects full-year earnings of $3.10 to $3.30 a share on revenue between $13.86 billion and $14.05 billion. Visit www.coventryhealthcare.com.
FINANCIAL BRIEFS
February 13, 2012 Health Plan Week 5
Rate Scrutiny Could Intensifycontinued from p. 1
When you look at it from that perspective, the federal oversight doesn’t appear to be very successful, says Caplan. On the other hand, the threat of federal rate review might have caused some health insurers to “sharpen their pencils” when calculating rate increases and more aggressively negotiate lower reimbursement rates from providers, he says. “If that has allowed insur-ers to file rates that are below the 10% threshold, then arguably the program has had some measure of success,” he tells HPW.
Kansas Insurance Commissioner Sandy Praeger (R) agrees that the new federal oversight might not have much of a direct impact on coverage costs, but says it could help to shine a spotlight on the underlying medical costs, which is a contributing factor in driving up pre-mium increases.
Copyright © 2012 by Atlantic Information Services, Inc. All rights reserved. Please see the box on page 2 for permitted and prohibited uses of Health Plan Week content.
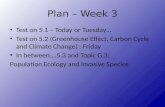
Health Net’s Stock Price Kicks Off 2012 With 24% Jump, but Falls in FebruaryStock prices for the 11 health plan operators tracked by HPW collectively increased more than 10% in January. Gains were led by Health Net Inc.’s stock price, which ended January with a 52-week high of $37.74 — up a whopping 24.1% from the end of December. But after peaking at $30.04 on Feb. 1, Health Net’s stock price began to tumble after it reported its fourth-quarter 2011 earnings declined 25% and enrollment remained flat (HPW 2/6/12, p. 6). The company’s results, however, did top analyst expectations. WellPoint, Inc. and Coventry Health Care, Inc. were the only carriers to see stock prices decline in January.
Tennessee-based Health Spring, Inc., which saw its stock price more than double in 2011, officially became part of Cigna Corp. on Jan. 31. The $3.8 billion acquisition makes Cigna a much bigger player in the Medicare space. Cigna’s stock price increased 6.7% in January. Overall Medicare Advantage (MA) premiums declined 16% and enrollment jumped 17% since 2010, according to new data from HHS. About 11.7 million people are now covered by an MA plan.
Closing Stock Price on 1/31/2012
January Gain (Loss)
Full-Year Gain (Loss)
Consensus 2012 EPS*
Consensus 2011 P/E Ratio*
COMMERCIAL
Aetna Inc. $43.70 3.6% 3.6% $5.10 8.5 x
Cigna Corp. $44.83 6.7% 6.7% $5.67 8.4 x
Coventry Health Care, Inc. $30.07 (1.0%) (1.0%) $3.27 10.2 x
Health Net, Inc. $37.74 24.1% 24.1% $3.35 12.2 x
UnitedHealth Group $51.79 2.2% 2.2% $4.81 11.3 x
WellPoint, Inc. $64.32 (2.9%) (2.9%) $7.72 9.1 x
Commercial Mean 5.4% 5.4% 9.9 x
MEDICARE
Humana Inc. $89.02 1.6% 1.6% $8.08 11.0 x
Medicare Mean 1.6% 1.6% 11.0 x
MEDICAID
Amerigroup Corp. $68.01 15.1% 15.1% $4.03 16.9 x
Centene Corp. $45.20 14.2% 14.2% $2.73 16.6 x
Molina Healthcare, Inc. $30.61 37.1% 37.1% $1.79 17.1 x
WellCare Health Plans, Inc. $59.76 13.8% 13.8% $4.22 14.2 x
Medicaid Mean 20.0% 20.0% 16.2 x
Industry Mean 10.4% 10.4% 12.0 x
* Estimates are based on analysts' consensus estimates for full-year 2012.SOURCE: Bank of America Merrill Lynch. Compiled by Atlantic Information Services, Inc., February 2012.
explained that the staff changes would allow it to “streamline its operations and lower administrative costs” by consolidating work for greater efficiency and effectiveness. As a result of the streamlining, Sassi, who was president of the consumer business division, took over marketing.
Coffina says the company has been unable to fully capitalize on the “considerable potential” of its manage-ment team. While investors tend to prefer management stability, the news about Sassi’s termination didn’t seem to impact stock prices. In the same Feb. 8 filing, WellPoint said that its officers were expected to reaffirm the com-pany’s earnings per share guidance for 2012 to be at least $7.60 per share. Stock prices on Feb. 9 closed at $64.65, unchanged from the previous day’s close.
Contact Lori McLaughlin for WellPoint at [email protected], Coffina at [email protected] and Gupte at [email protected]. G
continued
6 Health Plan Week February 13, 2012
But former Maryland insurance commissioner Al Redmer says the additional level of federal oversight is redundant and “will only add cost to the very product they want to moderate.” He contends that rate review should be left at the state level. Redmer, who also is a former CEO for Coventry Health Care of Delaware, is now president of Redmer Insurance Group.
Calif. Pushes for More AuthorityBlue Shield of California intends to increase rates by
as much as 14.9% for more than 200,000 members, the advocacy group Consumer Watchdog warned on Feb. 8. In a letter to the Los Angeles Times this month, Sen. Di-anne Feinstein (D-Calif.) said she was the first person to sign a petition for a new ballot that would give insurance regulators in her state the power to reject health insur-ance rate hikes. In an email, she urged supporters to sign the petition so that it could receive the 505,000 signatures needed to get onto the ballot in November. In Califor-nia, regulators can reject rate hikes for homeowner and auto insurance, but lack the same authority over health insurance. Past efforts to give California regulators more power over health insurance rates have failed.
The legislation would allow California to “open the books” and determine for itself whether a proposed rate increase is justified, says Carmen Balber, director of Con-sumer Watchdog’s Washington, D.C., office. “They need to be able to look at the numbers and reject rates that aren’t justified,” she tells HPW. Last April, the California Dept. of Managed Health Care determined that a 16%
rate increase from Anthem Blue Cross was excessive, but lacked the authority to reject it, Balber adds.
Even in states where regulators can’t deny rates, they typically can assert some pressure on insurers, says Prae-ger. She says her office has 30 days to approve or disap-prove a filing, but it can’t deny increases unless it can demonstrate the request is excessive or discriminatory.
“I don’t know of a state that doesn’t require substan-tial justification for a rate increase. And just because [a state] can’t deny rates, that doesn’t mean [carriers] don’t have to justify it,” adds former Oklahoma Insurance Commissioner Kim Holland, now executive director of state affairs at the Blue Cross and Blue Shield Associa-tion. “There is not a state out there that doesn’t take the rate review process seriously. And there isn’t a plan out there that doesn’t take the process of rate evaluation seriously.”
Moreover, she says, if a health plan doesn’t spend enough of its premium dollars on claims, it has to refund the difference under the medical loss ratio (MLR) provi-sion of the reform law. “I don’t know of any other indus-try that is in that position.”
In Maryland, Redmer says his office had “a whole team of pros that scrutinized the numbers” when carriers proposed a rate hike. But he adds that “every carrier has a level of expertise where they are able to hide additional percentages of margin in different line items.”
Last year, CMS’s Center for Consumer Information and Insurance Oversight (CCIIO) determined that seven
Web addresses cited in this issue are live links in the PDF version, which is accessible at HPW’s subscriber-only page at http://aishealth.com/newsletters/healthplanweek.
Overcoming the Challenges of Bundled Payments: Health Plans’ Strategies and Results to Date
¾¾ What¾goes¾into¾the¾negotiation¾process¾of¾a¾bundled¾payment¾for¾an¾episode¾of¾care?
¾¾ How¾can¾health¾plans¾respond¾to¾challenges¾in¾developing¾a¾bundled¾payment¾model,¾such¾as¾avoiding¾cherry¾picking¾healthy¾patients¾and¾administrative¾hurdles?¾
¾¾ What¾can¾be¾learned¾from¾the¾experience¾of¾states¾that¾are¾already¾taking¾an¾interest¾in¾testing¾these¾models¾of¾care?
¾¾ What¾procedures¾and¾episodes¾will¾be¾an¾early¾focus¾for¾plans¾and¾employers?
¾¾ What¾outcomes-based¾payments,¾technologies,¾reporting¾requirements¾and¾quality¾metrics¾are¾being¾considered¾for¾use¾in¾bundled¾payment¾models?
¾¾ What¾are¾the¾pros¾and¾cons¾of¾bundled¾payments¾in¾relation¾to¾other¾value-based¾payment¾methodologies,¾such¾as¾accountable¾care¾organizations?
Join¾Mark Lutes of¾Epstein¾Becker¾&¾Green¾and¾Colleen Matthewsof Horizon¾Healthcare¾Innovations¾for¾a¾Feb. 28 Webinar.
Visit www.AISHealth.com or call 800-521-4323
February 13, 2012 Health Plan Week 7
states — Alabama, Arizona, Idaho, Louisiana, Missouri, Montana and Wyoming — lack the resources and/or authority needed to properly regulate the individual and small-group markets. In three other states, Iowa, Penn-sylvania and Virginia, federal regulators can review only the small-group market while state regulators are respon-sible for the individual market. In some states, small-group insurance products had not previously required rate filings (HPW 8/1/11, p. 1).
But Redmer doesn’t think giving some states more authority over rates will lead to better industry oversight. Even state regulators that lack the authority to reject rates do have an indirect influence over them. “So I question whether rates are really being scrutinized any more now than they were a couple of years ago,” he says.
When it comes to rising coverage costs, insurance companies are an easy target, says Praeger. It’s much more difficult to get your arms around a real solution to the rising cost of health care. Regulators, she says, are limited in what they can do to control rate hikes “until we have a more meaningful or rational delivery system. And that deals with changing fee-for-service medicine, which just encourages overutilization. I always try to remind folks that premium increases are just the mes-senger and the truth is…health care costs continue to go up,” Praeger tells HPW.
Moreover, in the often hyper-competitive world of health insurance, carriers could be at a disadvantage if their prices are too high, she adds.
Regardless of the federal oversight, rates will push higher over the next several years because there
is no downward pressure on provider charges, says Joseph Berardo, Jr., president and CEO of MagnaCare, a health plan management company. “The cost shifting that is occurring — and will continue to occur — by hospitals to the commercial sector because of reductions in reimbursements from Medicare and Medicaid will exacerbate the problem,” he says. “If the government wants to truly have an impact they need to regulate hospital rates that are charged to commercial health plans.”
And if aggressive rate reviews artificially suppress rates, insurers “almost certainly” will need to request larger future rates in the future. Or the burden of regulation and fear of potential losses could cause some carriers to exit the market, says Jim Galasso, president and consulting actuary at Atlanta-based Actuarial Modeling.
“A helpful regulatory response would be greater reli-ance on…MLR ratios versus saddling the industry with both effective price controls, via the MLRs, and onerous rate reviews that almost always devolve into political football.”
To see California’s state ballot petition, visit www.justifyrates.org.
Contact Katelyn Peterson for Berardo at [email protected], Karen Rippel for Praeger at [email protected], Kelly Miller for Holland at [email protected], Scott Ladd for Caplan at [email protected], Redmer at [email protected], Balber at [email protected] and Galasso at [email protected]. G
Subscribers who have not yet signed up for Web access — with searchable newsletter archives, Hot Topics, Recent Stories and more — should click the blue “Login” button at www.AISHealth.com, then follow the “Forgot your password?” link to receive further instructions.
u Kentucky Cabinet for Health and Family Ser-vices (CHFS) Secretary Janie Miller resigned her post, effective Feb. 29, Gov. Steve Beshear’s (D) office said Feb. 7. Miller had held the position for four years. CHFS Deputy Secretary Eric Friedlander will serve as interim secretary until Beshear finds a permanent replacement. Although a statement from Beshear’s office says Miller is leaving to pursue other opportunities, the Louisville Courier-Journal reported that her resignation follows many problems with the state’s new Medicaid managed care system. Begin-ning in the fourth quarter of 2011, Kentucky began converting 560,000 Medicaid members into managed care plans from Coventry Health Care, Inc., Centene Corp. and WellCare Health Plans, Inc. In a Feb. 8 note to investors, Deutsche Bank equity analyst Scott Fidel noted “several red flags that suggest it could
be challenging for Medicaid managed care plans to achieve profitability here in 2012.” View Beshear’s statement at http://tinyurl.com/6ntmb5c.
u A new study finds that medical claims submit-ted electronically tend to be reimbursed faster and more fairly when compared with paper claims. IVANS, Inc. a national health information exchange, determined that while 39% of providers still use paper to submit paper claims, only 11% use paper for Medicaid claims, and just 1% use paper for Medicare claims. The survey also found that 65% of respondents say Medicare was the fastest payer, followed by Medicaid at 26% and commercial at 9%. The company says the findings indicate more work is necessary to increase automation in claims process-ing. IVANS also reports that 93% of providers think
HEALTH PLAN BRIEFS
8 Health Plan Week February 13, 2012
Medicare is fair either all or most of the time with claims, compared with 65% for Medicaid. More than 60% of providers said they do not believe commer-cial payers are fair all or most of the time. Visit www.ivans.com.
u A Consumer Reports analysis of mini-med health insurance plans released Feb. 7 finds most of them inadequate because they offer limited health coverage. Although mini-med plans continue to operate, they will be nonexistent by 2014 when ad-ditional provisions of the health reform law go into effect. The magazine says 50 health insurance compa-nies have federal waivers to offer mini-meds through 2014. The health plan operators with the highest enrollment include Cigna Corp.’s Cigna Starbridge (265,000 enrollees), Aetna Inc.’s Aetna SRC (209,423), BCS Insurance (115,000) and American Heritage Life Insurance Co. (69,945). Visit www.consumerreports.org.
u Aetna on Feb. 8 launched a new program, dubbed Aetna In Touch Care, that is designed to improve care management for members. Under the program, a member is assigned a nurse care manager who serves as a single point of contact. Enrollees also receive an individualized health action plans that uses the insurer’s personal health record tool, a predictive algorithm that identifies potential health issues earlier and virtual care for members with less urgent care needs. The program is available to self-insured customers, though the insurer intends to expand it into other segments in the future. Visit www.aetna.com.
u On Feb. 7, the head auditor for Montana Com-missioner of Securities and Insurance Monica Lindeen recommended approval for PacificSource Health Plans to purchase a portion of New West Health Services’ commercial business, the Associ-ated Press reports. New West, Montana’s third-larg-est insurer, has about 8,600 members in that segment. PacificSource was able to get the $1.5 million deal after state and federal regulators expressed con-cerned over Blue Cross and Blue Shield of Montana’s proposal to pay $26 million to get 11,000 New West hospital employee members (HPW 11/21/11, p. 3). An antitrust settlement, however, breaks New West into three parts: the hospital employees go to the Mon-tana Blues plan, the commercial business to Pacif-
icSource, while New West gets to keep its Medicare business. Visit http://sao.mt.gov.
u Anthem Blue Cross and Blue Shield in Connecti-cut and Empire BlueCross BlueShield in New York both unveiled initiatives borrowing from patient-centered medical homes that will pay primary care physicians (PCPs) more for improving member outcomes and reducing costs. Both plans say they will collaborate with PCPs on information sharing, care management coordination and shared savings. In addition, doctors will be paid for “non-visit” ser-vices not currently reimbursed, such as developing care plans. The New York Blues plan said one of its medical homes pilot showed a 12%-to-23% decrease in acute inpatient admissions and an 11%-to-17% drop in total emergency room visits. WellPoint un-veiled the initiative last month, saying it would be rolled out in stages (HPW 2/6/12, p. 3). Visit www.anthem.com.
u Cigna CEO David Cordani says the insurer, which already sells insurance in 30 countries, has no intentions of entering additional markets, Bloomberg reported Feb. 2. “From a prioritization of new countries, we did Turkey and India, so we are where we want to be,” he told the news organization. In August, Cigna expanded operations to Turkey (HPW 8/15/11, p. 8). And in November, the insurer entered into an agreement with Indian conglomerate TTK Group to offer products in that country (HPW 12/5/11, p. 1). Cigna’s international revenue rose 31% last year, though new accounting rules cut 2011 earn-ings for the international segment by $70 million. Visit www.cigna.com.
u On Feb. 6, the White House Office of Manage-ment and Budget said it has begun to review the final insurance exchange regulations, CQ Health-Beat reported. However, it’s too soon to tell when the final reg will be finalized and published in the Federal Register. Review could take anywhere from a few days to weeks or months. In an interview with HPW sister publication Inside Health Insurance Exchanges, Joel Ario, who headed HHS’s Office of Health Insur-ance Exchanges until last fall, confirmed that the regulations are expected to be out this month. Also under review is a final regulation on reinsurance and risk adjustment in exchanges, which arrived there Jan. 23, according to CQ HealthBeat.
HEALTH PLAN BRIEFS (continued)
Call Bailey Sterrett at 202-775-9008, ext. 3034 for rates on bulk subscriptions or site licenses, electronic delivery to multiple readers, and customized feeds of selective news and data…daily, weekly or whenever you need it.
If You Don’t Already Subscribe to the Newsletter, Here Are Three Easy Ways to Sign Up:
1. Return to any Web page that linked you to this issue
2. Go to the MarketPlace at www.AISHealth.com and click on “Newsletters.”
3. Call Customer Service at 800-521-4323
If you are a subscriber and want to provide regular access to the newsletter — and other subscriber-only resources at AISHealth.com — to others in your organization:
Call Customer Service at 800-521-4323 to discuss AIS’s very reasonable rates for your on-site distribution of each issue. (Please don’t forward these PDF editions without prior authorization from AIS, since strict copyright restrictions apply.)