1 Coding for Local Health Department Clinic & School Sites Presented by: Cynthia H. Robinson...
-
Upload
amice-gibbs -
Category
Documents
-
view
219 -
download
0
Transcript of 1 Coding for Local Health Department Clinic & School Sites Presented by: Cynthia H. Robinson...
1
Coding for Local Health Department
Clinic & School Sites
Presented by: Cynthia H. Robinson
Kentucky Department for Public Health
AFM/LHO
July 17, 2012
2
Table of Contents
1. Coding on the PEF
2. Determination of New or Established Patients
3. Coding of Preventive Visits
4. Components for coding “Other than Preventive E/M Visits”
5. Coding of Problem Visits – New Patients
6. Coding of Problem Visits – Established Patients
7. Multiple Visits for the Same Patient on the Same Day
3
This presentation was done to aid employees of health department clinics in coding and reporting of services. It could
not possibly cover all of the circumstances which occur in these clinics on a day to day basis. This
presentation is intended to assist in the training of new employees and to refresh
existing employees.
4
1. Only provide the level of care that is medically necessary per clinical judgment.
2. Always provide and document services in accordance with the Core Clinical Services Guidelines (CCSG) and with established best practices.
3. Always code and document exactly what care was provided.
Guiding Principles
6
Coding on the PEF
• The state-updated CH-45 (PEF) is used in most health department clinics. (Shown on next slide.)
• Some health departments prefer to create and use an abbreviated PEF at off site clinics (e.g. Flu Clinics & School sites). This is entirely permissible.
• Health Departments using their own forms are responsible for keeping these forms up-to-date.
8
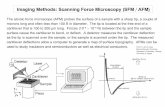
CodesCurrent Procedural Terminology (CPT) – A set of codes,
descriptions, and guidelines intended to describe procedures and services performed by physicians and other health care providers.
CPT codes describe WHAT was done for the patient.
International Classification of Disease 9th Revision 2009 (ICD-9) – This system is required for reporting diagnoses and diseases to all U.S. Public Health Service and Department of Health and Human Services Programs, such as Medicare and Medicaid.
ICD-9 codes describe WHY it was done.
9
Examples of Codes
CLINIC SETTING:
•99211– Office or other outpatient visit for the evaluation and management of an established patient that may or may not require the presence of a physician.
•99393 – Periodic comprehensive preventive medicine – reevaluation & management of an individual late childhood (age 5 through 11 years)
SCHOOL SETTING:
•99212 – Office or other outpatient visit for the E/M of an established patient, which requires at least 2 of these 3 key components: History, exam, & medical decision making
•V741 – Special Screening Examination For Pulmonary Tuberculosis
•V202 - Routine Infant Or Child Health check
•7840 – Headache ; Facial Pain; Pain in head NOS
CPT codes - WHAT ICD-9 codes - WHY
10
• Coding E/M visits in health department clinics consists of: – Preventive Visits E/M visits (e.g. well child
exam, well woman checks)– Evaluation/Management visits, which LHD’s
commonly refer to as “problem visits” (e.g. supply visits, STD’s, cancer screenings)
Coding E/M visits on the PEF
11
• Preventive Visits (e.g. Well Child Exams)– Top left corner of PEF– 99381-99397 for Physicians/mid-level providers– W9381-W9397 for Nurses
Coding on the PEF
12
• Other E/M Visits (Problem Visits)– Top right corner of PEF– 99201-99215 for Physicians/mid-level providers– W9201-W9215 for Nurses
Coding on the PEF
13
• REMEMBER:
– 992 codes - for use by physicians and mid level providers only
– W92 codes - for use by nurses (RN’s)
Coding on the PEF – Provider Level
• Physicians and mid level providers code in the upper portion of the Preventive and Other Than Preventive Sections.
•Nurses code in the lower portion of the Preventive and Other Than Preventive Sections.
14
Coding on the PEF- CPT codes• CPT codes for lab tests, etc. that are done
as part of the visit must be....– Checked in the appropriate
box on the PEF
– OR, if the service is not listed on the PEF it should be written in the area provided
15
• ICD codes need to be written on the PEF in the section that corresponds with the office visit that was checked.
• ICD codes will reflect why the patient presented. They are assigned based on the presenting problem(s) of the patient.
• REMEMBER: ICD codes for LHDs must be five digits. If the code is 3 or 4 digits, add dashes to make the code 5 digits long.
Coding on the PEF - ICD codes
16
• There is a box for a primary (P) ICD and a secondary (S) if needed.
• For example...a 4 y/o established patient, receives preventive exam by a nurse (V202-) and also receives vaccines (V069-).
• This would be coded on the preventive side of the PEF
Coding on the PEF - ICD codes
V069-
V202-
√
17
ICD Codes In Health Department Sites
• ICD codes are revised annually and are effective on October 1 of each year.
• ICD9 is changing to ICD10 effective October 1, 2014.
• Many LHDs create their own listing of most commonly used ICD codes. – REMEMBER: These lists must be updated
annually.
ICD Codes In Health Department Sites
• ICD-9 Codes that start with “ E ”are not eligible as the FIRST diagnose code.
• Therefore, if you put an “ E ” code as the primary ICD-9 Code, please expect your claim to be denied from all payors,
as “ E ” codes are not valid PRIMARY
ICD-9 codes for claims payment.
18
20
New & Established Patients
The Patient Encounter Form (PEF or CH-45) distinguishes between New Patients and Established Patients:
•New Patients visits are coded in the areas highlighted in PINK.
•Established Patients visits are coded in the areas highlighted in BLUE.
21
New & Established Patients
• NEW PATIENT - a patient who has not received a professional service (i.e., preventive, problem focused, or procedure) at any health department or satellite clinic in the COUNTY within the past three years.
• Determination of new or established status is made on a COUNTY basis, not a district basis.
22
New & Established Patients
• The PSRS (Patient Services Reporting System) determines whether the patient is new or established at computer registration when the PEF label is created.
• The computerized registration process is generally not done at the satellite site itself, often making it difficult for the provider to know whether the patient is new or established.
23
New & Established Patients• If the provider cannot determine whether
the patient is new or established by looking at the medical record, the provider should check the appropriate new patient level of visit and the appropriate established patient level of visit on the PEF. (See examples on next two slides.)
• This will save time for the provider and for staff doing the data entry. The PEF will not need to be sent back to the nurse for determination of level of visit.
24
• Patient presents to nurse requesting pregnancy test:
• Staff doing data entry should look at label to determine if it is a new patient or established, then...– Enter correct office visit– Mark through other visit
New & Established PatientsClinic Setting: If the system is down or off-site
V7241
√ √
25
• Patient presents to nurse with headache...
• Staff doing data entry should look at label to determine if it is a new patient or established, then...– Enter correct office visit– Mark through other visit
New & Established PatientsSchool Setting:
7840-
√√
26
New & Established Patients
• Under NO circumstances should staff entering data change the level of visit to accommodate a new or established patient (unless that level was also marked on the PEF, as discussed in the previous slides).
• The provider must determine the level of visit.
28
Coding of Preventive Visits• Preventive visits are reported when the
patient receives a full preventive physical exam per the guidelines in the Core Clinical Services Guidelines (CCSG).
• Coding of these visits require three components: – New or established patient status– Age of patient – Completion of physical exam by protocols
which are listed in the CCSG
• A9900 Vaginal Contra Film is actually included in the A4269
This will now be on the PEF as:
A4269 – Foam/Spermicide/Gel/VagFilm
30
In an effort to reduce confusion on Immunization Components, LHO has added the number of components contained in each Immunization to the outside of the vaccine. For example:
Diagnose codes for Ky Women’s Cancer Screening Program (KWCSP)
LHO wanted to make it easier to provide the correct diagnose codes for this program. We have added the codes the program would like to see listed for this procedure to the PEF in order to assist in correct coding.
Multi-vitaminsDefinitions
W0506 – Multi-vitamin FIRST BOTTLE – 3 month supply – Payment from Program
W0506FR – Multi-vitamin – Additional bottles FREE – thru Local Funds ---
W0506CH – Charge to the patient
34
Commonly Referred to as “Problem Visits” in Health
Department Settings
Components for coding “Other than Preventive E/M Visits”
35
Components of Problem Visits
• Problem Visits are made up of three components which are directly linked to the coding of these services.
1. History-consists of a combination of three parts:– History of present illness– Review of systems– Past, family and social history
2. Exam3. Decision making
• These three components are the driving forces behind the coding of Problem Visits.
• Understanding these three components is extremely important in accurate coding of problem visits.
36
History
• Subjective – documentation that is reported by the patient.
• Comparable to the “S” (subjective) portion of the SOAP note
• Combination of three components – – History of present illness – what the patient reports as
problems, symptoms, time frames, etc.– Review of systems – what body systems are affected
by the presenting problems– Past, family and social history – what past, familial or
social influences there might be on the seriousness and resolution of the problem
37
Exam
• Objective – what the provider notes when assessing the patient
• The exam is comparable to the “O” (objective) portion of the SOAP note
• The exam portion will be discussed in detail in the Coding of Problem Visits - New Patients section of this presentation
38
Decision Making
• The decision making component consists of three parts...
1. Presenting problem management options• Comparable to the “A” (assessment) portion of a
SOAP note.• After looking at the patient history and performing
exam as needed, the assessment of what the patient’s problem(s) are
39
2. Diagnostic procedures ordered • Provider must decide what, if any, diagnostic
procedures should be done
3. Management options selected• What treatment the patient should receive• The last two parts combined are comparable
to the “P” (plan) portion of a SOAP note
Decision Making
41
• American Medical Association (AMA) rules require that you have documented some of each of these components for new patients: 1. History 2. Exam 3. Decision making
• The AMA rules state that you must code Other E/M Office Visits for new patients to the lowest of these three components. By lowest of these three components, they mean the component which has the least impact on the visit.
• Should you be missing one of the three components on a new patient, an 80000 code will have to be used. – This code gives you no reimbursement and no Work Resource
Based Relative Values. So the time spent with this patient will be as though it never happened.
Coding of Problem Visits – New Patients
42
• The exam component will be the lowest of the three components 99% of the time.
• New patients should be coded by the amount of exam performed (which are commonly referred to as “exam bullets” because this is how they are identified in CPT classification).
Coding of Problem Visits – New Patients
43
Exam – New Patients
• A complete list of exam bullets can be found in the 1997 Documentation Guidelines for Evaluation & Management Services (developed jointly by the AMA & HCFA).
44
Exam – New Patients• The five most common bullets are:
• General Appearance/Nutritional Status. (Although these appear on two lines of the HP/CH-13 and HP/CH-14 exam forms, they only count as one bullet.)
• Mood and Affect• Orientation• Skin (2 bullets possible)
• Inspection – looking (e.g. pink, tan, intact)• Palpation - touching (e.g. warm, dry)
• Vital signs can be used as an exam bullet also, but three vital signs from the following list MUST be done for it to count as a bullet:– Sitting or standing blood pressure – Supine blood pressure– Height– Weight– Temperature– Pulse– Respiration
45
• Following is a list of the number of exam bullets that corresponds to the level of office visit to code for new patients:– 1 to 5 exam bullets = 99201 or W9201 Brief– 6 to 11 exam bullets = 99202 or W9202 Expanded – 12 to 17 exam bullets = 99203 or W9203 Detailed– 18 to 23 exam bullets = 99204 or W9204 Comprehensive
• A comprehensive office visit has the same requirements as full preventive visit (per the preventive guidelines in the CCSG). If this level of exam is performed, the provider should look at coding a full preventive exam on the patient.
– 24 or more bullets = 99205 or W9205 Complex • Comprehensive and Complex levels of new patient visits should
seldom occur in a health department site. These have been addressed here in case of rare emergencies.
Coding of Problem Visits – New Patients
46
Coding of Problem Visits – New Patients
• The AMA expects medical providers to do a more thorough exam, within reason, on a new patient to provide a good base line for future visits (see 907 KAR 3:130).
47
• Remember to have some History, some decision making, however the Coding for new patients is directly related to the amount of exam bullets performed, as it’s usually the lowest component in HD.
– Count the number of exam bullets and code accordingly.
Coding of Problem Visits – New Patients
49
• To code a Problem Visit for an established patient, the AMA requires that only two of the three components be documented.
1. History 2. Exam 3. Decision making
• The visit should be coded by the lowest of the two components.
Coding of Problem Visits – Established Patients
50
• The level of visit chosen for established patients will be driven by the lowest of either the history component or the medical decision making component.
• Exam performed should be what is required by protocol and medically necessary.
Coding of Problem Visits – Established Patients
51
Coding of Problem Visits – Established Patients (Clinic)
• 99211 and W9211 Brief– No history is taken– Decision making is minimal– No ROS (review of systems)
•Examples:–Negative TB skin test reading
(NEVER write a SOAP note for a negative TB skin test reading. That raises the level of visit and is never
medically necessary.)
52
Coding of Problem Visits – Established Patients (School)
• 99211 and W9211 Brief– No history is taken– Decision making is minimal– No ROS (review of systems)
•Examples:
– Daily Rx or OTC medication administration to patients who have: • One stable chronic illness well controlled (minimal risk)
– i.e. Ritalin, Tegretol, Singulair• One previously diagnosed acute uncomplicated illness or injury (minimal risk)
– i.e. amoxicilin, eye drops
53
Coding of Problem Visits – Established Patients (Clinic)
• 99212 or W9212 Limited– Requires at least 2 of these 3 key components;
• Problem specific history;• Straight forward decision making;• ROS
– Patients who have one or more self-limited or minor problem(s)• Examples
– Supply Visit (no complaints or problems)– STD Visit (no problems or negative results)– Head lice (either suspected or found)
54
Coding of Problem Visits – Established Patients (School)
• 99212 or W9212 Limited– Requires at least 2 of these 3 key components;
• Problem specific history;• Straight forward decision making;• ROS
– Patients who have one or more self-limited or minor problem(s)• Examples
– Headache– Upset stomach– Head lice (either suspected or found)– Earache – Menstrual cramps– Daily Rx or OTC medication administration with a complaint/problem
i.e.: Ritalin, Singulair, amoxicilin
55
Coding of Problem Visits – Established Patients (Clinic)
• 99213 or W9213 Expanded– Requires at least 2 of these 3 key components;
• Expanded problem focused history;• Expanded problem focused examination;• Decision making of low to moderate complexity
• Examples– Pt to receive depo – wt gain 5 lb since last visit, c/o occasional
headaches – counseled & depo adm.– Positive TB skin test reading– Positive STD visit with treatment– Daily Rx medication administration to patients who have one
stable chronic illness w/o problems (i.e. DOT – Communicable Disease)
56
Coding of Problem Visits – Established Patients (School)
• 99213 or W9213 Expanded– Requires at least 2 of these 3 key components;
• Expanded problem focused history;• Expanded problem focused examination;• Decision making of low to moderate complexity
• Examples– Daily Rx medication administration to patients who have one
stable chronic illness (i.e.: insulin) – Injuries that require the patient to go home– Medication unavailable and coordination of care with parent or
physician is necessary
57
Coding of Problem Visits – Established Patients (Clinic)
• 99214 or W9214 Detailed– Requires at least 2 of these 3 key components;
• Detailed history;• Detailed examination;• Decision making of moderate complexity
– Presenting problems are of moderate to high complexity • Examples
– True contraindication to contraceptive methods• OCs - B/P 160/92, c/o severe HA’s daily with visual impairment - no
contraceptive given until patient is further evaluated – Patients presenting with problems significant enough that more case
management is necessary• Pt with abnormal breast exam
*******Please keep in mind: 907 KAR 3:010 Section 4PHYSICIAN’S MEDICAID only pays Doctors for TWO 99214 visits
per 12 months
Coding of Problem Visits – Established Patients (Clinic)
• 99214 or W9214 Detailed– Requires at least 2 of these 3 key components;
• Detailed history;• Detailed examination;• Decision making of moderate complexity
– Presenting problems are of moderate to high complexity • Example: Positive Preg test – initial PN Visit
- HIGH RISK PREGNANCY - includes
2 or More RISK Factors
For Example: - Smoker- Obesity - Age (under or over)
- History of Miscarriage/High Blood Pressure/Early labor
- Preeclampsia -STI with pregnancy 58
59
Coding of Problem Visits – Established Patients (School)
• 99214 or W9214 Detailed– Requires at least 2 of these 3 key components;
• Detailed history;• Detailed examination;• Decision making of moderate complexity
– Presenting problems are of moderate to high complexity • Examples
– Patients who experience exacerbation of chronic illnesses (i.e.: diabetes, asthma, ADHD, epilepsy)
– Patients who present with acute uncomplicated problems requiring more care coordination (i.e.: broken bones, emergency room, stitches, adverse reactions)
*******Please keep in mind: 907 KAR 3:010 Section 4PHYSICIAN’S MEDICAID only pays Doctors for TWO 99214 visits
per 12 months
60
Coding of Problem Visits – Established Patients (Clinic)
• 99215 or W9215 Comprehensive– Requires at least 2 of these 3 key components:
• Comprehensive history;• Comprehensive examination;• Decision making of high complexity
– Presenting problems are of moderate to high complexity– Significant risk to the life of the patient
• Examples– HIV – Rape– Abrupt neurological changes– Anaphylactic reaction to vaccine– Emergency treatment necessary via EMS
*******Please keep in mind: 907 KAR 3:010 Section 4PHYSICIAN’S MEDICAID only pays Doctors for TWO 99215 visits per
12 months
61
Coding of Problem Visits – Established Patients (School)
• 99215 or W9215 Comprehensive– Requires at least 2 of these 3 key components:
• Comprehensive history;• Comprehensive examination;• Decision making of high complexity
– Presenting problems are of moderate to high complexity– Significant risk to the life of the patient
• Examples– Severe or prolonged seizures– Diabetic coma– Head injuries with prolonged unconsciousness or abrupt
neurological changes– Emergency treatment necessary via EMS*******Please keep in mind: 907 KAR 3:010 Section 4
PHYSICIAN’S MEDICAID only pays Doctors for TWO 99215 visits per 12 months
63
• A 25 modifier may be reported with a Preventive visit, if there is a significant enough and separately identifiable problem . The 25 modifier would be listed with problem-focused E/M visit.
• When immunizations are given, problem-focused E/M with a 25 modifier may be reported if there is a distinct and separately, identifiable reason for the E/M visit (i.e., a different diagnosis code).
• When an E/M is reported on the same day as another procedure , such as a MNT; the E/M will require a 25 modifier and the diagnosis code for the E/M needs to different from the diagnosis code for the MNT.
The 25 modifier is located beneath the Other Then Preventive codes section.
You may either check or circle the 25.
Multiple Visits for the Same Patient on the Same Day with Different Problem
(Clinic)
OTHER THAN PREVENTIVE HEALTH CHECK E/M -PHYSICIAN/MID LEVEL CPT NEW Visit Type CPT EST. Visit Type PROVIDER
99201 Brief 99211 Brief99202 Expanded 99212 Limited99203 Detailed 99213 Expanded99204 Comprehensive
99214 Detailed ICD (P)
99205 Complex 99215 Comprehensive
25 MODIFIER Separate E/M by same provider/same day NURSE ICD (S)
W9201 Brief W9211 Brief
W9202 Expanded W9212 LimitedW9203 Detailed W9213 Expanded REF/DISPW9204 Comprehensive W9214 DetailedW9205 Complex W9215 Comprehensive
Example of when to use the 25 Modifier:
39 year old established pt comes in for Family Planning preventive visit, while doing this pt’s family planning preventive visit, the APRN finds vaginal warts, and with the permission of the pt, treats.
Coding would consist of:
99395
9921325
64
Another Example of when to use the 25 Modifier:
17 year old established pt comes in for family planning supplies and RN finds out she has not received the Gardasil vaccine. Pt wants to receive this vaccine and is counseled per component.
Coding would consist of:
9921225
90460 1unit
9064965
66
Multiple Visits for the Same Patient on the Same Day with Different or Same
Problem (School)• If a patient presents to the local health department satellite school site more than one time on the same day for a different or same problem, only one Office Visit (OV) can be billed – per Medicaid
• However, each visit must be documented in the patient’s medical record
Clarification:•If a patient is seen multiple times on the same day, following
the last visit of the day; the nurse should review the documentation & select the most complex
level of visit for billing
Clarification of the Only Example of when to use the 25 Modifier in a
School Setting:
7 year old established pt comes in at 8:00am for daily therapeutic insulin administration. Same pt comes back before lunch to find out what to eat. Same pt returns for symptoms present; RN meets all the needed components for a problem visit and codes to the most complex for the day.
Coding would consist of:
W921325
96372
67
68
1. Only provide the level of care that is medically necessary.
2. Always provide and document services in accordance with the Core Clinical Services Guidelines (CCSG) and with established best practices.
3. Always code and document exactly what care was provided.
Guiding Principles
69
References:
1) Current Procedural Terminology 2012 2) International Classification of Disease 9th Revision 2012 3) 1995 CMS document: Documentation Guidelines to
Evaluation & Management Services4) 1997 CMS document: Documentation Guidelines to
Evaluation & Management Services5) CMS Evaluation & Management Service Guide