The term fluid means water and the components it contains Chemical compounds are the principal...
-
Upload
antony-harrison -
Category
Documents
-
view
220 -
download
2
Transcript of The term fluid means water and the components it contains Chemical compounds are the principal...
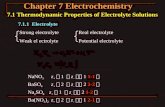
The term fluid means water and the components it contains Chemical compounds are the principal components of most
body fluids An electrolyte is a compound contained in fluids The body needs at least 1500ml of water per day in
addition to water from foods we eat (700ml) and from the oxidation of food (300ml)
Fluids transport nutrients and wastes to and from cells and acts as a solvent for electrolytes and nonelectrolytes
Fluids also help maintain body temperature, facilitate digestion and elimination, maintain acid-base balance, and lubricate joints and other body tissues
Fluid Therapy
Intravascular fluids are extracellular fluids contained within arteries, veins and capillaries
Having too little blood (fluid) within these vessels greatly affects the nutrient and oxygen supply to all tissues
Having too much fluid within these vessels can damage the intimal lining of blood vessels and the tissues
Electrolyte imbalance via deficit or excess poses many complications….
Fluid Therapy
Body fluid is considered in a state of balance (equilibrium) when the following occurs: water and electrolyte components are in proper proportions; lost body water and electrolytes are replaced; fluids are distributed normally between compartments; excess water and electrolytes are eliminated;
In the average adult, 50% to 60% of the body weight is from fluids
70% of fluid is intracellular and 30% is extracellular
Fluid Therapy
http://what-when-how.com/nursing/fluid-and-electrolyte-balance-structure-and-function-nursing-part-1/
Located outside body cells-in between cells- and serve as the body’s transport system
Extracellular fluids carry water, nutrients, electrolytes and oxygen to the cells
Extracellular fluids also remove the waste products from cellular metabolism
**Excess fluid within the interstitial space is Edema
Extracellular Fluid- 3 Main locations: 1. Interstitial Fluid
Is plasma within the blood Mainly transporting blood cells Intravascular fluids are a component
(compartment) of extracellular fluids By definition it is the spaces within veins,
arteries, and capillaries
2. Intravascular Fluids
Special fluids◦ Cerebrospinal◦ Pleural◦ Peritoneal◦ Synovial◦ Digestive juices
3. Transcellular Fluid
When illness occurs and fluid moves into an area that makes it physiological unavailable-fluid is trapped. Not interstitial and not intravascular!
Examples: ◦ Ascites◦ Pericardial effusion◦ Vesicles-blisters
Third Spacing
Fluid can move between compartments through selectively permeable membranes by:◦ Diffusion◦ Active transport◦ Filtration◦ Osmosisin order to maintain homeostasis
Movement of Fluids
Hypovolemia: body loses both water and electrolytes from the ECF◦ Can lead to hypovolemic shock
Dehydration: water is lost from the body, but there is no loss of electrolytes
Fluid Volume Deficits
Vital signs: hyperthermia, tachycardia, thready pulse, hypotension, orthostatic hypotension, decreased central venous pressure
Neuromuscularskeletal: dizziness, syncope, confusion, weakness, fatigue
GI: thirst, dry furrowed tongue, nausea/vomiting, anorexia, acute weight loss
Renal: Oliguria Other signs: diminished capillary refill,
cool clammy skin, diaphoresis, sunken eyeballs, flattened neck veins
Expected Client Findings in Volume Deficits
Hypervolemia: both water and sodium are retained in abnormally high proportions
Overhydration: occurs when more water is gained than electrolytes
Fluid Volume Excesses
Vital Signs: tachycardia, bounding pulse, hypertension, tachypnea, increased central venous pressure
Neuromuscularskeletal: confusion, muscle weakness
GI: weight gain ascites Respiratory: dyspnea, orthopnea, crackles Other Signs: edema, distended neck veins
Expected Client Findings in Volume Excess
Electrolytes
http://www.cnsweb.org/extra/digestvertebrates/GITFigures/ElectrolytesCompositionExtracellularIntracellularCompartments%20F10_01.gif
Ionized substances that perform specific functions within a fluid compartment
The most plentiful electrolytes found within the cells are potassium, magnesium, phosphate and protein.
The most plentiful electrolytes found in the extracellular fluid is sodium, chloride, calcium, bicarbonate and hydrogen
Intracellular and extracellular fluids contain the same electrolytes, but in differing amounts
Electrolytes
Fluid balance is regulated by thirst mechanisms – the stimulation or inhibition of thirst response depends on changes in plasma osmolality; lymphatic system – soaks up excess fluid not reabsorbed into the capillaries; Neuroendocrine system – by producing and secreting hormones that stimulate or inhibit osmotic receptors in carotid arteries and aortic arch (these receptors very sensitive to blood volume); GI system – fluid absorption from dietary and also secretes fluid from glands and tissues; Renal system – regulates the volume of extracellular fluid
Pediatric clients are at great risk for impaired fluid balance because of their size and immaturity, the younger the child the greater the risk for fluid deficit. Elderly are at great risk due to increased incidences of chronic diseases.
Regulation of Fluid Balance
Fluid imbalance rarely exits without electrolyte imbalance
Excess losses through urine, vomiting, suction, diarrhea, tachypnea, and wounds place a client at risk for electrolyte imbalances
Electrolyte Imbalances
Intravenous therapy is a means to provide supplemental nutrition, medication, fluid and electrolytes when the client is in a deficient state
If a client has been without food through oral or gastric route for three days, an IV route may be chosen to provide this nutrition
Total parenteral nutrition (TPN) is defined as providing carbohydrates, proteins, fats, and other electrolytes via an intravenous route
When a client is on TPN, close monitoring of hyperglycemia and polyuria must take place due to the risk for osmotic diuresis from the high glucose levels in the solution
Intravenous Therapy
Establish or maintain a fluid or electrolyte balance
Administer continuous or intermittent medication
Administer bolus medication Administer fluid to keep vein open (KVO) Administer blood or blood components Administer intravenous anesthetics Maintain or correct a patient’s nutritional state Administer diagnostic reagents Monitor hemodynamic functions
Indications for Intravenous Therapy
Venipuncture is a procedure of accessing a vein by inserting a needle or catheter in the vein for short or long term IV therapy
The normal maintenance fluid is not enough when a person is experiencing an actual, moderate to severe fluid loss
When a client’s homeostatic fluid needs cannot be met through an oral route or tube, or replacement is needed more quickly than these routes can offer, IV therapy is the method of choice
Intravenous Therapy
Mimic body’s extracellular fluid Used to expand both intravascular and
extravascular fluid volume
Crystalloid Fluids
Isotonic Hypotonic Hypertonic
Crystalloid Types of IV Solutions
http://www.phschool.com/science/biology_place/biocoach/biomembrane1/solutions.html
◦There is no net movement of fluid between compartments (between blood and cells)
ISOTONIC
http://internalandexternalenvironments2012.wikispaces.com/Hypertonic,+hypotonic+and+isotonic+effects+on+plants+and+animal+cells.
This would increase the amount of fluid in the vascular space.
Examples of this type of IV solutions are:
NS Ringer’s lactate
Isotonic con’t.
Fluid moves from a place of less solutes to a place of more solutes (fluid would move from the vascular space into the cell)
HYPOTONIC
http://internalandexternalenvironments2012.wikispaces.com/Hypertonic,+hypotonic+and+isotonic+effects+on+plants+and+animal+cells.
This will help cellular dehydration.
Fluid would move out of the vascular space into interstitial space and/or cell.
Cells swell.
Examples of this type of IV solutions:
O.2% saline (1/4 normal saline)
0.45 saline (1/2 normal saline)
D2.5/W D5W
Hypotonic con’t
Fluid moves from a place of less solutes to a place of more.
HYPERTONIC
http://internalandexternalenvironments2012.wikispaces.com/Hypertonic,+hypotonic+and+isotonic+effects+on+plants+and+animal+cells.
Fluid would move from the interstitial tissue and/or the cell into the vascular space.
Works well to decrease swelling in the cell or interstitial tissues (cells shrink).
Examples of IV solutions:
D5LR (5% dextrose in ringer’s lactate)
D5NS D51/2NS D50
Hypertonic con’t
Contain undissolved particles such as protein, sugar, and starch molecules which are too big to pass through capillary walls
Draws fluid from interstitual and intracellular spaces, increasing intravascular volume
Albumin – most frequently usedUsed when crystalloids are inadequateHypovolemic shockMassive hemorrhage
Colloid IV Fluid
Usually given as RBCs, platelets, and plasma
Packed RBCs usually used: this gives the RBC mass without the volume overload
Blood and Blood Products
The nurse is hanging an intravenous (IV) solution of D5NS with 20 mEq of KCL. The nurse notices the label from the pharmacy is correct as indicated; however, the solution is D5W. Which actions should be taken by the nurse to safely administer the IV infusion? Select all that apply.
Check for one unique client identifier before administration.
Consult the supervisor Administer the IV Solution Call the pharmacist First, initiate the new stat
orders for another client . Know the organization’s
policy for medication administration.
Description: short (3/4 to 1-1/4 inches) plastic cannula around a short stylet
Length of use: 72-96 hours per insertion (Aultman policy is 96 hours)
Insertion location: superficial veins in the dorsal venous network, basilic, cephalic, and median veins and their branches
Short-Term Dwell Catheters: Short Peripheral Catheters
The cannula selected should be the shortest and smallest gauge that is appropriate for the prescribed therapy.
Recommended gauges are:14-16 gauge used for surgery18-20 gauge for infusion of hypertonic or isotonic
solutions with additives18-20 gauge for blood administration22-24 gauge for pediatric patients22 gauge for fragile veins in elderly persons if unable
to place a 20 gauge catheter
Needle Selection
If infusing irritating medications, a smaller gauge catheter should be selected and inserted in a larger vein to facilitate hemodilution
Bigger isn’t necessarily better!
Avoid the hand veins in older adult clients or active clients
Avoid palm-side veins and veins 4 to 5 inches proximal to the wrist
Avoid veins in the fingers and thumb; their smaller diameter allows little blood flow and they easily infiltrate
Avoid veins on an extremity with lymphedema (for example, post-CVA or mastectomy), paralysis or a dialysis graft/fistula
Start with most distal location and move proximally when selecting site
Soft straight vein is best choice. Avoid bruised veins, red or swollen veins, veins near previously infected areas or recently discontinued sites
Location Selection Factors
Veins of the hands and arms are most commonly used to infuse IV fluids.
Veins of the Hand1. Digital Dorsal veins2. Dorsal Metacarpal veins3. Dorsal venous network4. Cephalic vein5. Basilic vein
Veins of the Forearm1. Cephalic vein2. Median Cubital vein3. Accessory Cephalic vein4. Basilic vein5. Cephalic vein6. Median antebrachial vein
Initiate process by explaining procedure to the client
Verify “six rights” Gather supplies Prepare IV adaptor (prime) Find a suitable vein:
-position arm on a flat surface-apply tourniquet-lower client’s arm below heart level-apply warm, moist compress-have client make a fist and hold it-gently tap or stroke vein in the direction of blood flow
Venipuncture Technique
If you are unsuccessful in entering the vein and there is no flashback, then slowly withdraw the catheter, without pulling all the way out, and carefully watch for the flashback to occur.
If you are still not within the vein, then advance it again in a 2nd attempt to enter the vein.
While withdrawing always stop before pulling all the way out to avoid repeating the painful initial skin puncture.
If after several manipulations the vein is not entered, then release the tourniquet, place a gauze over the skin puncture site, withdraw the catheter and tape down the gauze.
Try again in the other arm.
If not successful:
Limit number of attempts to two attemps before obtaining another healthcare provider to try
Immediately stop and remove the catheter if the client reports a new onset of paresthesia, numbness, or sharp shooting pain
Insertion Technique (con’t)
Tunica Adventitia: outer layer of connective tissue that supports the vessel
Tunica Media: muscular and elastic tissue with nerve fibers for vasoconstriction and vasodilation
Tunica Intima: Innermost layer referred to as endothelial lining
NOTE: If tip of catheter nicks adventitia or is placed in tunica media, small amount of blood will appear in the catheter; however, catheter will not thread because it is trapped between layers.◦ If no steady backflow of blood is present, advance stylet
of catheter slightly before advancing the catheter
Layers of Tissue in Veins
Phlebitis – inflammation of the intimal layer of the vein; pt. will complain of pain and tenderness, warmth and redness may develop-intervention: remove catheter when tenderness first present, apply warm, moist pack (avoid massage because might dislodge clots)
Infiltration – IV fluid (a nonvesicant fluid) has leaked through the venous wall into the interstitial tissue surrounding the vein; area will feel hard and cold and will be painful- intervention: remove catheter, elevate arm, apply warm, moist pack
Extravasation – Leaking of a vesicant IV fluid into surrounding tissues - intervention: Turn IV off but DO NOT remove catheter, physician may need to order antedote.
Potential Complications of Venipuncture
Infection – warmth at site, heat pain, redness, possible fever and sepsis- intervention: blood cultures, antibiotic therapy
Air Embolism – dec. BP, cyanosis, tachycardia, JVD, loss of consciousness- intervention: notify Dr., administer oxygen, monitor VS’s
Other Potential Complications
Speed Shock – IV’s that contain certain additives if administered too fast can cause cardiac arrest.
Examples might be KCL, or calcium
Complications cont.
Depends on institutional policy, commonly change peripheral IV site every 72-96 hours
Commonly assess IV site every shift and prn (depends on policy, may be every 1-2 hours)
Site care
Baseline assessment includes vitals, LOC, mucous membranes for color and moisture, jugular venous distention, heart sounds, lung sounds, abdominal assessment, peripheral pulses, and urinary output
Focused Assessment Prior to Venipuncture
At insertion: 18 gauge,1 1/4in. Angiocath and prn adapter inserted on first attempt in left hand. Adaptor flushed with 3 ml NS. IV secured and op-site dressing applied. Pt tolerated procedure well.
If re-assessing: IV site L. hand without infiltration (edema) or erythema (redness), op-site dressing dry and intact.
Sample Venipuncture Documentation
IV of 1000 ml of D5W started in the L. forearm with a 18ga. 2 in. angiocath on the second attempt. IV secured and op-site dressing applied to insertion site. IV pump infusing at 125 ml/hr. Pt tolerated the procedure well.
Documentation cont.
Mrs. Katz has been admitted to the intermediate care unit with a diagnosis of acute gastrointestinal bleeding. Her blood pressure is 88/50 mm Hg, and her pulse is 120 beats/min. The nurse would expect Mrs. Katz’s IV therapy to be:
1 2 3 4
25% 25%25%25%
1. a blood transfusion2. an isotonic fluid,
such as normal saline.
3. a peripheral IV lock.4. a hypotonic fluid,
such as 5% dextrose.
Mr. Shoen has congestive heart failure. In obtaining a dietary history from Mr. Shoen, the nurse notes that his meals consist of many high-sodium foods. The nurse should teach the patient which of the following?
1 2 3 4 5
20% 20% 20%20%20% A diet high in sodium will
cause him to lose too much fluid volume and his blood pressure to fluctuate.
. A diet high in sodium will cause him to retain fluid, increasing the workload of his heart.
. A diet high in sodium will cause him to lose potassium, putting him at risk for cardiac arrhythmias.
A diet high in sodium will cause him to lose calcium, putting him at risk for osteoporosis.
The nurse notes that a patient on her unit has had a very high temperature for the past 2 days. Today, the patient’s skin turgor is poor, and she tells the nurse her mouth feels very dry. Which of the following is the nurse’s best response?
1 2 3 4
25% 25%25%25%1. Call the physician to request an IV fluid bolus
2. Place the patient on intake and output measurements.
3. Restrict the patient’s fluid intake to 600 mL for the rest of the shift
4. Encourage the patient to increase oral fluid intake
The tip of all central venous access devices infuses IV fluids into the:
1 2 3 4
25% 25%25%25% jugular vein. superior vena cava. subclavian vein. brachial vein.
A goal of administering albumin intravenously is to increase oncotic pressure in the vascular space.
1 2
50%50%1. True2. False
The best overall measurement of total body fluid loss or gain is the measurement of intake and output?
1 2
50%50%
1. True2. False