Intratympanic Dexamethasone for Sudden Sensorineural Hearing ...
Infantile variant of Bartter syndrome and sensorineural deafness: A new autosomal recessive disorder
-
Upload
daniel-landau -
Category
Documents
-
view
218 -
download
2
Transcript of Infantile variant of Bartter syndrome and sensorineural deafness: A new autosomal recessive disorder

American Journal of Medical Genetics 59:454459 (1995)
Infantile Variant of Bartter Syndrome and Sensorineural Deafness: A New Autosornal Recessive Disorder
Daniel Landau, Hana Shalev, Meli Ohaly, and Rivka Carmi Department of Pediatrics (D.L., H.S.), Clinical Genetics Unit (R.C.), Soroka Medical Center, Ben Gurion University of the Negev, Beer Sheva, and Department of Pediatrics, Barzilai Medical Center (M.O.), Ashkelon, Israel
The infantile variant of Bartter syndrome (IBS) is usually associated with maternal polyhydramnios, premature birth, postnatal polyuria and hypokalemic hypochloremic metabolic alkalosis and a typical appear- ance. IBS is thought to be an autosomal recessive trait. Several congenital tubular defects are associated with sensorineural deafness (SND). However, an association be- tween the IBS and SND has not been re- ported so far. Here we describe 5 children of an extended consanguineous Bedouin fam- ily with IBS and SND. In 3 of the cases, the typical electrolyte imbalance and facial appearance were detected neonatally. SND was detected as early as age 1 month, sug- gesting either coincidental homozygotiza- tion of 2 recessive genes or a pleiotropic ef- fect of one autosomal recessive gene. This association suggests that evaluation of SND is warranted in every case of IBS. 0 1995 Wiley-Liss, Inc.
KEY WORDS: Bartter Syndrome, deafness, recessive inheritance
INTRODUCTION Bartter syndrome (BS) was originally described by
Bartter et al. [1962], and is characterized clinically by normotensive hyperreninism, hyperaldosteronism, and hypokalemic hypochloremic metabolic alkalosis. Renal biopsy shows juxtaglomerular hyperplasia. Renal prosta- glandin metabolism is upregulated [Gill et al., 19761, manifesting itself, in renal biopsy, as hyperplasia of
Received for publication December 29, 1994; revision received April 20, 1995.
Address reprint requests to Daniel Landau, M.D., Department of Pediatrics, Soroka Medical Center, P.O.Box 151, Beer Sheva 84101, Israel.
0 1995 Wiley-Liss, Inc.
renal medullary interstitial cells, which are capable of substantial prostaglandin synthesis.
An infantile variant of BS (IBS) was previously de- scribed by Seyberth et al. in 1985. It usually causes ma- ternal polyhydramnion, premature birth and postnatal polyuria, associated with severe salt loss and failure to thrive. Some of the infants also have severe hypercalciuria. This particular variant is thought to be inherited as an autosomal recessive trait [Hogewind et al., 1981; Ohlson et al., 1984; De Rovetto et al., 1989; Leonhardt et al., 19921. Some of the infants with the IBS variant have been described as having a prominent forehead, trian- gular facies with drooping mouth and large eyes and pinnae [James et al., 1975; Ohlson et al., 19841. The patho- genesis of this, as well as the other BS variants, is not well understood. Different theories exist regarding the primary renal defect, and include, among others: impair- ment in sodium and chloride reabsorption [Rodriguez- Portales et al., 19861, increased tubular potassium loss [Korff et al., 19841, increased prostaglandin synthesis [Fujita et al., 1982; Calo et al., 19901 and angiotensin re- sistance [Bourke and Delaney, 1981; Sasaki et al., 1976; Kurtzman and Gutierrez, 19751. Treatment with prosta- glandin synthetase inhibitors, mainly indomethacin, with or without potassium supplements or potassium sparing diuretics, has been shown to be effective in this disorder [Bommen and Brook 1982; Seyberth et al., 1985; Matsumoto et al., 19891.
Sensorineural deafness (SND) has been described in association with various congenital renal diseases. These include glomerular diseases, such as Alport syn- drome, in which SND is typically a late phenomenon [Gubler et al., 19811, and several tubular disorder, in- cluding: familial distal renal tubular acidosis [Dunger et al., 1980; Anai et al., 1984; Bentur et al., 1989; Caldas et al., 19921, pseudohypoaldosteronism [Tungland et al., 19901, Fanconi syndrome [Chevalier, 19831 and others [Kobayashi et al., 1985; Goto et al., 19901. SND in these cases manifests itself early in life, potentially impair- ing language development. So far, no case of SND has been described in association with the IBS variant. Here we describe 5 patients with IBS and congenital SND, all of whom are members of an extended, inbred Bedouin family.

Deafness in Infantile Bartter Syndrome 455
by polyhydramnios. Birth weight was 1445 g. On the third day of life polyuria and weight loss of up to 25% of birth weight were evident. This caused a transient azotemia that was corrected by intravenous fluids. In addition, hyponatremia, hypochloremia and hypo- kalemic alkalosis were found together with increased excretion of these salts in urine (Table 11). Marked hy- percalciuria (calciudcreatinine ratio in spot urine = 0.42, normal <0.21 [Kruse et al., 19841) was also noted. Plasma renin activity and aldosterone levels were markedly elevated (Table IT), as well as urinary prosta- glandin E2 levels (230 ngM1.73 m2; n = 4-27 ng/h/m2) [Leonhardt et al., 19921. The infant was treated with dietary supplementation of NaCl and KC1. Hypo- natremia gradually improved and enabled weaning of NaCl supplementation, but hypokalemia persisted. Prominent forehead, triangular face with drooping mouth and large eyes and pinnae were noted at age 6 months. Renal ultrasound study at the age of 7 months showed medullary nephrocalcinosis. Severe failure to thrive and moderate developmental delay were noted early in infancy. Because of delay in speech develop- ment, hearing evaluation was performed. Brain audi- tory evoked response ( B U R ) test showed complete lack of neural transmission of sound stimuli. After es- tablishing the diagnosis of BS at age 7 months, therapy with indomethacin (2-3 mgkglday) was added to oral KC1 supplementation. This treatment helped normal- ize the low serum potassium and chloride levels as well
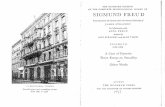
CLINICAL REPORTS The five family members (Fig. 11, 2 sisters and their
3 male cousins, are of Bedouin ancestry, and were 1 month, and 2,3,2.5 and 16 years old at the time of the report. They are all products of first-cousin marriages. There was polyhydramnios and subsequent premature birth in all cases. Data about the postnatal course are available on the 4 younger patients (Table I). They all presented soon after birth with severe polyuria which caused loss of up to 25% of their birth weight, as well as salt loss. The 4 infants had a typical facial appearance, with: triangular face with a wide forehead, prominent eyes, large ears and a small mouth (Fig. 2). Three of the 4 older children failed to thrive and were developmen- tally delayed. Hearing tests were done as part of the investigation of the developmental delay or because of the family history, and disclosed complete SND. None of the described patients received aminoglycosides or high dose furosemide therapy. There were no other rel- atives with a similar appearance without BS or SND, or individuals with any other renal disease or deafness. All but the oldest patient were treated with oral indo- methacin and showed an improved weight gain, de- crease in polyuria and improvement of the electrolyte imbalances.
Case 1 V-3, a 3-year-old girl, was born spontaneously at 31
weeks of gestation. Pregnancy course was complicated
I
I1
I11
IV
V
8 NBS + SND (ZI PREMATtiRE STILLBIRTH + POLYHYDRAMNIOS # PREMATURE STILLBIRTH
Fig. 1. Pedigree of the IBS-SND family.

456 Landau et al.
TABLE I. Patient Data
Age at Dx" Gestational age Developmental Deafness Pt. no. (months) Polyhydramnios (weeks) AGAISGA~ FTT' delay v-2 0.5 + v-3 0.5 + v-4 42 + V-5 180 + v- 1 Birth +
32 AGA + + + 31 AGA + + + 33 AGA 33 AGA + 38 SGA + ? +
+ +
- + -
"Dx age: age of diagnosis of BS. b ~ ~ ~ ~ ~ A appropriate or small for gestational age. 'FTT: failure to thrive.
as the high levels of calcium, magnesium and phospho- rus. However, growth improvement was only slight. At the age of 3 years the child is still developmentally and physically delayed. Deafness and lack of compliance with special education programs do not enable appro- priate estimation of her true developmental potential.
Case 2 V-2, a 21-month-old girl, is V-3's younger sister. Pre-
natal course was complicated by polyhydramnios, for which the mother was treated with repeated amniocen- teses and oral indomethacin. She was born a t 32 weeks of gestation, weighing 1,800 g. Like her sister she pre- sented soon after birth with polyuria, which caused a 16% loss of birth weight. Hyponatremia associated with natriuresis but without hypokalemia was noted and was treated with NaCl supplementation. Serum mag- nesium was elevated transiently. Plasma renin activity and aldosterone levels were markedly elevated (Table 11). NaCl supplementation could be weaned off at age one month. However, hypokalemia and kaliuresis, as- sociated with metabolic alkalosis were noted at that age, and were treated with oral KC1 supplementation. Urinary PGE, excretion was evaluated at age 3 months, one week after the discontinuation of indomethacin
therapy, and was found elevated. A typical facial ap- pearance was noted during the first year of life. SND was diagnosed by BAER test a t the age of 8 months. Since this was the second case of BS in this family, in- domethacin treatment was introduced rather early. This caused an improvement in weight gain, as well as normalization of serum sodium and potassium levels. At age 21 months the child still suffers from severe fail- ure to thrive and developmental delay.
Case 3 V-4, a 4-year-old boy is a cousin of the two previously
described sister. His mother had had five previous preg- nancies, one of which ended at 22 weeks of gestation in stillbirth. The other four pregnancies produced 4 healthy girls. The course of the current pregnancy was complicated by polyhydramnios which was treated with indomethacin. The child was born a t 33 weeks of gestation, weighing 1,995 g. After birth, polyuria was noted which caused a weight loss of 20%, azotemia, hy- ponatremia, and natriuresis (Table 11). Hypochloremia and hypokalemia were also found during the first week of life. He was treated with intravenous infusion of sodium and potassium chloride solutions, which halted the weight loss and corrected the electrolyte imbal-
Fig. 2. a: Patient V-3; b: Patient V-5.

Deafness in Infantile Bartter Syndrome 457
TABLE 11. Biochemical Data
Age a t Dx Pt. no. (months)
v-2 1 v-3 1 v-4 15 v- 5 15 y rs v- 1 1 week Normal
-____ S N a a S K
meq/L meq/L
120 2.3 128 2.5 117 2.5 140 2.1 128 2.8
SCl S H C 0 3 PRAb SAldo UN: U K meq/L mey/L mgAIUL/hr pg/L meq/L mey/L
>1,200 70 50 80 31 >50 78 31 >50 >1,200 100 55 90 N A ~ >so 647 52 20
460 NA 20 90 34 19.35 85 39 >50 >1,200 74 31
52.5 10-16
30 0.42 230 30 NA 149
NA NA NA NA NA NA 107 0.8 NA
<0.21" 4-27f
"Serum (S) and Urine (U) data are in meq/L. Urine electrolytes are spot tests performed simultaneously with the serum tests. 'PRA: plasma renin activity in mgAII/L/hr and serum aldosterone (S,,,,) in pg/L performed in a supine position after full rehydration with NaCl and correction of S,. 'UpcEa: urinary PGEQ, measured in nghd1.73 m2. dNA not available. 'Kruse et al. [19841. 'Leonhardt et al. [19921.
ances. The infant was gradually weaned off the i.v. flu- ids and was discharged home with normal serum urea and creatinine levels. Soon afterwards he developed re- current episodes of bowel distention. The diagnosis of Hirschprung disease was based on rectal biopsy and the infant underwent a colostomy procedure at the age of 1 month. During this hospitalization he was found to have mild hyponatremia and hypokalemia. During the first year of his life the infant failed to thrive. At the age of 15 months his weight and length were at the 50th centile for age 6 and 10 months, respectively. A reeval- uation at this point revealed the persistence of hypo- natremia, hypokalemia and hypochloremia (though no metabolic alkalosis was found). Magnesium, calcium and phosphorus levels were normal. Plasma renin ac- tivity and aldosterone levels were elevated for age. These findings, together with the child's facial appear- ance, established the diagnosis of IBS. BAER test dis- closed SND. Indomethacin therapy improved growth rate and corrected the electrolyte imbalances. Cur- rently the child's height and weight are at the 10th cen- tile and his psychomotor development is within the lower range for his age.
Case 4 V-5, a 16-year-old boy, is a cousin to V-2,3, born at 33
weeks of gestation. Eight of his mother's 10 pregnan- cies produced healthy children and two were compli- cated by polyhydramnios and subsequent stillbirths. This boy's prenatal period was also complicated by polyhydramnios. At age 6 months his parents noticed that the infant was not responding to noise. A BAER test disclosed complete SND. At 9 months of age the child was hospitalized for investigation of failure to thrive. He had an unusual appearance, with prominent forehead, triangular face and drooping mouth. How- ever, his blood potassium, sodium and magnesium lev- els were normal. At age 42 months he was readmitted because of failure to thrive and developmental delay. His bone age was retarded (15 months). Serum potas- sium levels were found persistently low. Thereafter, he was lost to follow-up, and was hospitalized at age of 15 years because of septic arthritis. Weight and height at that time were at the 50th centile of age 8 and 9.5 years, respectively. He was found to have hypokalemic
hypochloremic metabolic alkalosis. Plasma renin activ- ity and aldosterone levels were elevated. Potassium chloride supplementation was introduced. The patient is currently enrolled in a special education program for the deaf and is doing well.
Case 5 V-1, a 1-month-old infant, is another cousin to V-2,3
with first cousin parents. Pregnancy course was com- plicated with polyhydramnion, for which no cause could be found, since there was no indication regarding the relationship to the previous cases. The infant was de- livered by a cesarean section on the 38th week ofges- tation due to suspected fetal distress. After birth the in- fant was found to have asymmetric intrauterine growth retardation (birth weight: 1,580 g; OFC: 31.5 cm). The infant experienced more than 15% weight loss, leading to a transient azotemia. Hyponatremia with natriure- sis (fractional excretion of sodium: 5%; normal for this gestational age <1% [Arant, 19781) appeared on the second day of life, followed by hypochloremic hypo- kalemic metabolic alkalosis. Hypomagnesemia devel- oped in the second week of life. Plasma renin and aldosterone levels were elevated. Hypercalciuria was found during the first week of life. Renal sonogram at that stage showed bilateral increased echogenicity. Upon further questioning of the parents, the relation- ship with the previous IBS cases was discovered (Fig. 1). BAER, performed at age 3 weeks, showed evi- dence of sensorineural deafness. Indomethacin up to 3 mgkglday was started at the age of 5 days, together with KC1 and NaCl supplementation. This caused a gradual weight gain. NaCl supplementation was dis- continued and the infant was discharged home at age of 5 weeks.
DISCUSSION These 5 relatives have IBS and congenital SND, the
latter being probably a major contributor to their de- velopmental delay. The presented pedigree shows some clinical variability with regard to the course of the re- nal disease and especially its early manifestations and severity. However, the SND seems to be uniform, se- vere, and of very early onset in all patients. There is only one previous report of such an association in a case

458 Landau et al.
with oculocerebral hypopigmentation syndrome [White et al., 19931, which is clearly different from our cases. Both BS [Hogewind et al., 19811 and SND have been re- ported to be autosomally recessively transmitted. In- deed, our pedigree with multiple consanguineous mar- riages illustrates this mode of inheritance. Three explanations for the cosegregation of BS and SND in our family can be put forward. The first is a coinciden- tal homozygotization of two independent recessive genes. The occurrence of five affected individuals, all manifesting both traits and the absence of patients with either IBS or SND in spite of a high rate of con- sanguinity, necessitates the assumption of a very close linkage between the two gene loci. The second explana- tion is that SND is a complication of IBS. Two clinical presentations, a rare adolescent form of renal tubular acidosis (RTA) with mild to moderate SND and a rela- tively more common infantile type with severe SND, have been reported [Konigsmark and Gorlin, 19761. One of the forms of RTA associated with SND is due to the absence of the enzyme carbonic anhydrase 2 [Sly et al., 19831. The differences in severity of the SND could argue for a causal effect of the renal disease on hearing. Indeed, it has been shown that brisk serum electrolyte imbalances in end-stage renal disease patients may cause deafness [Bergstrom et al., 19731. Moreover, cases of early onset RTA and late occurrence of SND have been reported [Brown et al., 19931 as well as dis- cordant manifestations of RTA and SND in dizygotic twins [Caldas et al., 19921, suggesting a late complica- tion of the basic renal disease. However, while early correction of electrolyte imbalance in distal RTA helps prevent growth retardation, it does not ameliorate the severity of deafness associated with this disorder [Brown et al., 19931. In addition, it appears that deaf- ness is associated only with the familial-inherited form of distal RTA but not with the sporadic form, pointing again in favor of the genetic origin for the hearing im- pairment. Moreover, the classic SND-renal syndrome of Alport, in which several mutations have been lately identified in the a5 chains of type lV collagen [Hostikka et al., 19901, manifests itself with late onset appear- ance of both deafness and progressive deterioration of glomerular filtration rate, Therefore, the more likely third explanation for this association of BS and SND is a pleiotropic effect of one autosomal recessive gene. The existence of a similar gene is now well established for RTA and nerve deafness [McKusick #267300, McKusick, 19941. The fact that our patients had hearing impair- ment of very early onset, without any improvement fol- lowing the correction of electrolyte imbalance, also sup- ports this possibility.
In conclusion, we describe here an autosomal reces- sive disorder of the infantile variant of BS associated with deafness. Although the association of SND and congenital renal diseases has been previously reported, the specific combination in the described family is apparently a new one. Further similar reports will sug- gest whether all infants born with this particular tubu- lar defect should be screened for SND in order to facili- tate early intervention.
REFERENCES Anai T, Yamamoto J, Matsuda I, Taniguchi N, Kondo T, Nagai B
(1984): Siblings with renal tubular acidosis and nerve deafness. The first family in Japan. Hum Gen 66:282-285.
Arant BS (1978): Developmental patterns of renal fractional matura- tion compared in the human neonate. J Pediatr 92:705-712.
Bartter FC, Pronove P, Gill JR, Mc Cardle RC, Diller E (1962): Hyper- plasia of the juxtaglomerular complex with hyperaldosteronism and hypokalemic alkalosis: A new syndrome. Am J Med 33:
Bentur L, Alon U, Mandel H, Pery M, Berant M (1989): Familial dis- tal renal tubular acidosis with sensorineural deafness: Early nephrocalcinosis. Am J Nephrol9:470474.
Bergstrom L, Jenkins P, Sando I, English GM (1973): Hearing loss in renal disease: Clinical and pathological studies. Ann Otol 82: 555-575.
Bommen M, Brook CGD (1982): Pseudohypoaldosteronism: Response to long term treatment with indomethacin. Arch Dis Child 57: 718-720.
Bourke E, Delaney V (1981): Bartter’s syndrome: A dilemma of cause and effect. Nephron 27:177-186.
Brown MT, Cunningham MJ, Inglefinger JR, Becker AN (1993): Pro- gressive sensorineural hearing loss in association with distal renal tubular acidosis. Arch Otolaryngol Head Neck Surg 119:458460.
Caldas A, Broyer M, Dechaux M, Kleinknecht C (1992): Primary dis- tal renal tubular acidosis in childhood: Clinical study and long term follow up of 28 patients. J Pediatr 121:233-241.
Calo L, Cantaro S, Picoli A, Favaro S, Bonfante L, Borsatti A (1990): Full pattern of urinary prostaglandins in Bartter’s syndrome. Nephron 56:451452.
Chevalier RL (1983): Hypercalciuria in a child with primary Fanconi syndrome and hearing loss Int J Pediatr Nephrol4:53-457.
De Rovetto CR, Welch T, Hug G, Clark K, Bergstrom W (1989): Hyper- calciuria with Bartter syndrome: Evidence for an abnormality of vitamin D metabolism. J Pediatr 115:397404.
Dunger DB, Brenton DP, Cain AR (1980): Renal tubular acidosis and nerve deafness. Arch Dis Child 55221-225.
Fujita T, Ando K, Sat0 T, Yamashita K, Nomura M, Fukui T (1982): Independent roles of prostaglandins and the renin-angiotensin system in abnormal vascular reactivity in Bartter’s syndrome. Am J Med 73:71-76.
Gill JR, Frolich JC, Bowden RE, Taylor AA, Keiser HR, Seyberth HW, Oates JA, Bartter FC (1976): Bartter’s syndrome: A disorder char- acterized by high urinary prostaglandins and a dependence of hyperreninemia on prostaglandin synthesis. Am J Med 61:43-51.
Goto Y, Itami N, Kajii N, Tochimaru H, Endo M, Horai S (1990): Renal tubular involvement mimicking Barterr syndrome in a patient with Kearns-Sayre syndrome. J Pediatr 116:904-910.
Gubler MC, Levy M, Broyer M, Naizot C, Gonzalez G, Perrin D, Haib R (1981): Alport’s syndrome: A report of 58 cases and a review of the literature. Am J Med 70:493-505.
Hostikka SL, Eddy RL, Byers MG, Hoyhtya M, Shows TB, Tryggvason K (1990): Identification of a distinct type IV collagen a chain with restricted kidney distribution and assignment of its gene to the locus of the X-linked Alport syndrome. Proc Natl Acad Sci USA
Hogewind BL, Van Brummelen P, Veltkamp JJ (1981): Bartter’s syn- drome: An autosomal recessive disorder? Study of four patients in one generation of the same pedigree and their relatives. Acta Med Scand 209:463-467.
James T, Holland NH, Preston DBS (1975): Typical facies and normal plasma volume. Am J Dis Child 129:1205-1207.
Kobayashi Y, Hiki Y, Shigematsu H, Tateno S, Mori K (1985): Renal retinal dysplasia with diffuse glomerular cysts. Nephron 39: 201-205.
Konigsmark BW, Gorlin R J (1976): “Genetics and Metabolic Deaf- ness.’’ Philadelphia: WB Saunders Co.
Korff JM, Siebens AW, Gill AR (1984): Correction of hypokalemia cor- rects the the abnormalities in erythrocyte sodium transport in Bartter’s syndrome. J Clin Invest 74:1724-1729.
811-828.
87:1606-1610.

Kruse K, Kracht U, Kruse U (1984): Reference values for urinary cal- cium excretion and screening for hypercalciuria in children and adolescents. Eur J Pediatr 143:25-31.
Kurtzman NA, Gutierrez LF (1975): The Pathogenesis of Bartter’s syndrome. JAMA 234:758-759.
Leonhardt A, Timmermans G, Roth B, Seyberth HW (1992): Calcium homeostasis and hypercalciuria in hyperprostaglandin E syndrome. J Pediatr 120546-554.
Matsumoto J , Kim Han B, De Rovetto C, Welch T (1989): Hypercalci- uric BS: Resolution of nephrocalcinosis with indomethacin. AJR 152:1251-1253.
Me Kusick VA (1994): “Mendelian Inheritance in Man. Catalogues ofAu- tosomal Dominant, Autosomal Recessive andX-Linked Phenotypes.” 11th edition. Baltimore: The Johns Hopkins University Press.
Ohlson A, Sieck U, Cumming W, Akhtar M, Serenius F (1984): A vari- ant of Bartter’s syndrome. Acta Pediatr Scand 73:868-874.
Rodriguez-Portales JA, Delea CS (1986): Renal tubular reabsorption of chloride in Bartter’s syndrome and other conditions with hypo- kalemia. Clin Nephrol 6:269-272.
Deafness in Infantile Bartter Syndrome 459
Sasaki H, Okumura M, Ikeda M, Kawasaki T, Fukyiama K (1976): Hypotensive response to angiotensin I1 analogue in Bartter’s syn- drome. New Engl J Med 294:611-612.
Seyberth HW, Rascher W, Scweer H, Kuhl PG, Mehls 0, Scharer K (1985): Congenital hypokalemia with hypercalciuria in preterm in- fants: A hyperprostaglandiuric syndrome different from Bartter syndrome. J Pediatr 107:694-701.
Sly W, Hewell-Emmett D, Whyte MP, Yu YL, Tashian RE (1983): Carbonic anhydrase I1 deficiency identified as the primary defect in the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcifications. R o c Natl Acad Sci USA 80:2752-2756.
Tungland OP, Savage MO, Bellman SC (1990): A new syndrome: Hearing loss and familial salivary insensitivity to aldosterone in two brothers. J Laryngol Otol104:956-958.
White CP, Waldron M, Jan JE, Carter J E (1993): Oculocerebral hypo- pigmentation syndrome associated with Bartter syndrome. Am J Med Gen 46592-596.