Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxins, and Allergens
-
Upload
richard-l-tyndall -
Category
Documents
-
view
305 -
download
0
Transcript of Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxins, and Allergens

IndoorAir 1995. 5: 171--178 Printed i n Dminiark . all rights reserved
Copyright 0 Munksgaard 1995
Indoor Air ISSN 0905-6947
Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxins, and Allergens Richard L. Tyndall', Eva S. k h a n 2 , Elicia K. Bowman3, Donald K. Milton4, James M. Barbaree5
Abstract The propensity of various types of home humidzjiers w support and disseminate microbial contaminants inw indoor air was tested. Reservoir water and air discharged fiom humidifiers seeded in the laboratory or naturally contaminated in the home were analyzed by standard microbiological methods. Clin- ically insignificant as well as overt or potentially pathogenic microorganisms were found to colonize the reservoirs of all types of humidzjiers, but only cool mist and ultrasonic units readily aerosolized bacteria and endotoxin. Only cool mist units emitted hydrophobic fungal spores. Cool mist units dis- charged the greatest number of water particles in the inhalable size range (4-16 pm) while ultrasonic units were more likely to emit respirable-sized water particles (<O. 2-4 pm). Overt pathogens isolated fiom humidifiers in homes included Le- gionella and a pathogenic Acanthamoeba. Aerosolizing hu- midifiers should thus be avoided qfiequent, thorough cleaning of the units is not practical.
KEY WORDS: Aerosols, Bacteria, Endotoxin, LRgioneUa
Manuscript received: 14 October 1993 Accepted for publication: 24 October 1994 The views expressed in this article are strictly those of the authors and do not necessarily represent those of the Consumer Product Safety Commission. This study, conducted at the ex- pense of the U.S. Government, is considered in the public domain
Oak Ridge National Laboratory, P.O. Box 2008, Bdg. 9207 MS-8077, Oak Ridge, TN 37831-8077, USA Tel.: (6 19574-0686. Fax: (615)574-1274
USA A&G Technical Associates, Knoxville, TN, USA Harvard University, School of Public Health, Boston, MA, USA Centers for Disease Control, Atlanta, GA, USA
* Consumer Product Safety Commission, Washington, D.C.,
Introduction The U.S. Consumer Product Safety Commission initiated and supported a study to address concerns about airborne transmission of bioaerosols from a variety of humidifiers. Humidifiers, used by thou- sands of consumers, have been implicated in nu- merous published episodes of hypersensitivity pneu- monitis, humidifier fever and infections in hospitals, industrial settings and homes (Kreiss and Hodgson, 1984). Klein and Kunze (1971) showed that Pseudomonads were aerosolized by cool mist hu- midifiers, and Covelli et al.. (1973) demonstrated that Pseudumonas could also be aerosolized by four other types of humidifiers. Solomon (1974) found a three-fold increase of airborne fungi in a majority of test homes during operation of cool mist humidi- fiers. Burge et al. (1 980) demonstrated the presence of bacteria and fungi in both furnance and evaporat- ive console home humidifiers. Amoebic antigens and bacterial endotoxins isolated from humidifier fluids have been implicated in cases of hypersensit- ivity pneumonitis occurring in homes (Burke et al., 1977; Miller, 1976, Tourville et al., 1972; Shiue et al,, 1990) and in outbreaks of humidifier fever diag- nosed in industrial settings (Edwards, 1980; Ry- lander and Snella, 1983; Ashton et al., 1981). Free- living amoebae, such as Naegleria, were frequently detected in these studies (Edwards, 1980; Edwards, 1986). Gram-negative bacteria, such as Pseudomon- as species, have been implicated as a source of air- borne bacterial endotoxins (Shiue et al., 1990; Ry- lander and Haglind 1984, American Conference of Governmental Industrial Hygienists 1990).
While these studies identified humidifiers as a source of indoor microbial contamination, they did not systematically compare types of humidifiers with the microbial populations in their reservoirs or

172 Tyndall et al.: Home Humidifiers os o Potential Source of Exposure to Microbial Pathogens, Endotoxions, and Allergens
their abilities to aerosolize microorganisms and en- dotoxins into the environment. The current study was undertaken to address these issues.
Materials and Methods Five different types of humidifiers were tested in the laboratory. Three models each of cool mist and ultrasonic units and two models each of warm mist, console, and steam units were tested. Test models represented seven different manufacturers. Humidi- fication by steam vaporizers and warm mist units is effected by heating the water in the reservoir and discharging the water as steam. Cool mist units dis- charge various sized droplets of unheated water di- rectly from the reservoir by impeller action. Ultra- sonic units discharge water from the bottom of the reservoir via a vibrating nebulizer. Evaporative con- sole units produce water vapor by fan-forcing air through a fabric belt wetted by moving through the water reservoir. In addition to the laboratory hu- midifiers, a variety of humidifiers in homes in the Oak Ridge, Tennessee area were also studied.
In order to produce scale and biofilm in labora- tory humidifiers which in turn facilitated growth of microbes, the units were operated continuously for a period of five months and were filled as required with tap water. Maintenance was not performed on any unit during the five-month period. The reser- voirs of the units were not emptied or rinsed during this period. After this “conditioning” period, scale formation was apparent on various internal surfaces of the humidifiers. The conditioned units were then sterilized by exposure to ethylene oxide. New un- conditioned humidifiers were used in endotoxin studies.
For various laboratory tests, the conditioned, sterilized humidifiers were filled with sterile tap water, inoculated with microbes, and operated in two room-sized chambers (2.4 mX2.4 mX2.4 m). Morning and afternoon samples were taken from the reservoir or from the air in the chamber. Air samples were collected approximately one meter from the humidifier discharge. The air exchange rates within the chambers were monitored on an intermittent basis by releasing CO as a tracer gas. The data from the CO monitor and the relative hu- midityhemperature probe were recorded on a data logger, and the information from the data logger was regularly downloaded onto magnetic media for processing. The air exchange rate in the test chambers was 1.2-1.5 air changes per hour. During
operation, relative humidity in the test chambers generally ranged from 4675% with the steam-gen- erating models producing the lowest humidity. Temperatures ranged from 18” to 24°C.
A Portable Continous Aerosol Monitor (PPM, Inc., Knoxville, Tennessee) was used to determine droplet size emitted from various types of humidi- fiers without added microbes operating within the test chambers. The laser-scattering-based system determined the size range and mass concentrations of emitted aerosols. Samples were taken for five- minute periods, and the data reported are the aver- age of at least two separate five-minute periods.
A spectrum of microbial genera was used to seed the laboratory humidifiers. The test microbes were Bacillus, Micrococcus, Pseudomonas, Flavobacter, As- pergillus spores, and Acanthamoebae ruyreba. The bacteria were originally isolated from either labora- tory or home humidifiers. The bacterial cultures were grown on trypticase soy agar (TSA). Bacterial lawns were harvested from the TSA plates, sus- pended in sterile, distilled water, centrifuged, and washed in additional sterile distilled water. The re- sultant pellets were frozen in aliquots at -80°C until needed. The laboratory reservoirs were seeded with 104-105 total bacteria per ml. Fungal spores were supplied by Optima Company (New Haven, Con- necticut) as washed preparations from fungal cul- tures (295% pure with <3% contamination of the fungal mycelia) and were grown on malt extract (ME) media. Acanthamoebae ruyreba cultures were grown in tissue culture flasks (75 cm2) in a liquid casitone-based media (CGV). The protozoa were concentrated and washed by centrifugation in a 10% solution of Dulbecco-balanced salts solution. The amoebae were harvested immediately prior to their introduction into the test humidifiers.
Microbial concentrations in the laboratory and home humidifiers’ reservoir water were determined as follows: 10 ml samples were removed with sterile pipettes, and aliquots were titrated on TSA , ME, or on non-nutrient agar plates spread with a lawn of live E. coli (”AE). Plating of ten-fold dilutions of the water samples on TSA and ME at 23-25°C and NNAE at 35°C determined the concentrations of the bacterial, fungal, and Acanthamoebae titers, respectively. For detection of Legionella, samples were plated on BCYE agar either directly or after a 10-14 day incubation of the water sample at 35°C. In addition, iodine was added to aliquots of water from the home humidifiers to effect a 1% solution. These preparations were observed microscopically

Tyndall et a1 , Home Humidifiers as a Potential Source of Ex
for the presence of protozoa. Pathogenicity of some Acanthamoebae isolated on NNAE from home hu- midifier water was tested by inoculating approxi- mately 1 O5 trophozoites intranasally into weanling BABUc mice. Three to six weeks after inoculation, mice were sacrificed and brain and lung tissues were plated on NNAE plates to determine the presence of amobae in the test tissue.
Microorganisms in air were collected and enu- merated by use of Andersen samplers using the sixth-stage plate. Air was sampled at a rate of 28.3 Vmin for two minutes. Vacuum pumps used in con- junction with the Anderson samplers were tested periodically with a rotameter to ensure the proper airflow rate. The colonies on the test plates were counted by the “positive hole” method.
For the endotoxin studies, Pseudomonas endo- toxin (Sigma Chemical Coy St. Louis MO) was se- lected because this organism is frequently found as a contaminant of home humidifiers (Rylander, 1986). Background aerosol samples were obtained from in- door (chamber) and outdoor air and from humidi-- fier emissions when reservoirs were filled with pyro- gen-free water before endotoxin addition. Endo- toxin levels in water samples were measured directly by the LAL test. Aerosol samples were collected from humidifier emissions at approximately 0.5 m and 1.5 m from the aerosol discharge by passage through polyflow filters and into condensate traps. The filter extracts and condensates were then ana- lyzed according to recently published methods (Mil- ton et al., 1992).
45.000
40,000
35,000
5 30,000 6 25,000 z (r 20,000 W a 2 15,000 :: 10,000 2 2,000 0
W 5 1,500
1,000
500
COOL-MIST
CONSOLE I STEAM
II ULTRASONIC
I- =- 0 WARM-MIST
rl
BACTERIA FUNGI
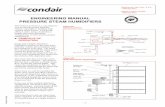
Fig. 1 Aerosolizotion of mixed bacterial flora and fungi by various humidifer types in laboratory studies. The data shown are the aver- age of six tests with each humidifier
:posure to Microbial Pathogens, Endotoxions, and Allergens 1 7 3
lL
z ULTRASONIC
W
25,000
(r 20,000 a
m
15,000 LL ; 10,000
2 2,000 0
W 2 1,500
1,000
500
0 BACTERIA FUNGI
Fig. 2 Airborne bacterial and fungal concentration in discharge of vorious humidifier types in area homes. The doto ore the overage of duplicate tests carried out on four ultrasonic units, four cool mist units, two console units, three steam units and nine furnonce humidi- fiers
To relate the laboratory studies with operation of humidifiers in the home environment, the microbial content and aerosolization by home humidifiers were investigated. On two separate occasions, Feb- ruary-April in 1987 and 1988, samples from reser- voirs of home humidifiers were collected in sterile 250 ml containers. A total of 88 samples were ob- tained and analyzed for microorganisms as pre- viously described. In addition, volunteers re- sponded to questions on humidifier use. Air samples were also taken in some of the homes as described in the laboratory studies. After the hu- midifiers had been turned off overnight, back- ground air samples were collected using duplicate TSA, ME, and NNAE plates in the Andersen sam- pler. Water samples were collected from the reser- voirs of the humidifiers. The units were then turned on and after running for 5 min, air samples were taken again using duplicate TSA, ME, and NNAE plates. Sampling took place in the air stream, gener- ally at a distance of 0.9 to 1.8 m from the humidi- fier. Additional samples were taken 30 minutes later.
Resu I ts Laboratory Studies Experiments to evaluate the potential of selected humidifiers to disperse bioaerosols under laboratory conditions showed marked differences in the vari- ous humidifiers’ ability to aerosolize fungal spores

174 Tyndall et al.: Home Humidifiers as a Potential Source of Exposure to Microbial Pathoqens, Endotoxions. and Alleraens
Table 1 Air particle percentages in humidifier plumes*
Humidifier Concentration Particle percentages type (mg/m3) <0.2 pm 0.24.0 pm >4.0-15.9 pm
Steam 16 49 6 43 Steam 19 35 8 57
Ultrasonic Ultrasonic Ultrasonic
5 33 24 44 5 27 48 22 5 13 10 76
Cool mist 14 1 13 86 Cool mist 4 4 8 87 Cool mist 18 1 5 93
* Measured concentrations and sizes at the aerosol monitor sensor; sizes and concentrations may be slightly larger due to possible evaporation during transit in tubing Console humidifier units did not discharge detectable particles
and bacteria (Figure 1). The cool mist humidifiers discharged high numbers of both fungi and bac- teria. The ultrasonic humidifiers showed marked discharge of bacteria but not of Aspergillus niger spores. Console units showed a slightly higher dis- charge of microbes than steam vaporizers and warm mist units but much less than cool mist or ultrasonic units.
The aerosolization of both bacteria and fungal spores by cool mist units and bacteria by the ultra- sonic units was seen in both models of each type. The lack of aerosolization by steam vaporizers, warm mist, and console units was also consistent between models. Airborne amoebae were seen in only three samples: two from cool mist units and one from a console unit. Background and other air samples were negative for amoebae.
Analysis of reservoir populations showed a con- tinuing presence of the various microorganisms throughout the 72-hour test period except for loss of fungal spores and amoebae from one cool mist unit. The dispersal rate of the microbial population could not be determined because of lack of infor- mation concerning the percent of dead airborne mi- crobes at sampling time, the rate of loss of viability when airborne, and the effects of concentrating and diluting the microbial population as water is lost and replaced in different amounts.
Results of a modest effort to characterize the physical nature of aerosols from humidifiers in the laboratory using the aerosol monitor are shown in Table 1 and indicate the particle size profiles and the measured output of the humidifiers.
The ultrasonic units expelled 13% to 33% of their output as particles below 0.2 pm i.e. diffusing particles. From 22% to 76% of their output was in
the 4.0 to 16 pm range and 10% to 48% in the 0.2- 4.0 pm range. The cool mist units ranged from 86% to 93% of their output in the 4.0 to 15.9 pm range. The highest percentage of particles emitted by ste- am vaporizers was in the <0.2 pm and the 4.0 to 15.9 pm range. The console humidifiers gave no detectable measurements with the aerosol monitor since water loss was due to evaporation.
The results of the endotoxin studies are shown in Tables 2 and 3. The outdoor samples measured 0.18 and 0.10 ng/m3. One indoor background sample was 0.02 ng/m3, and endotoxin was not de- tectable in the other indoor background sample. Endotoxin levels that exceed background levels by 1 00-fold may be associated with respiratory toxicity (American Conference of Governmental Industrial
Table 2 Endotoxin emitted by aerosolizing humidifiers during four hours of operation (ng/m3)
Humidifier Filte?
ULTRASONIC cleanb spikedc
clean spiked
outdoord indoord
COOL MIST
BACKGROUND
Close" Fa? (0.5 m) (1.5 m)
0.33 0.08 620 360
0.04 0.13
Sample 1 Sample 2 0.10 0.18 0.02 N.D.
1100 530
a - Distance from source b - Pyrogen free water c - Seeded with 1000 ng/ml of Pseudomonas endotoxin d - Before turning on humidifiers nd - None detected

Tyndall et 0 1 . : Home Humidifieis as a Potential Source of Exposure to Microbial Pathoaens. Endotoxions. and Alleraens 175
Table 3 tndotoxin emitted by evaporotive humidifiers during four hours o f ooeration (ng/m3)
Humidifier FilteP
Close" Far" (0.5 m) (1.5 m)
WARM MIST clean" spiked' clean spiked
clean spiked
clean spiked
STEAM- 1
STEAM-2
0.04 0.10 0.06 0.29
0.03 0.07
0.15 0.04
0.27 0.18 0.07 0.32
0.03 0.1 1
0.11 0.21
BACKGROUND Sample 1 Sample 2 outdoor 0.10 0.18 indoord 0.02 N.D.
a - Distance from source b - Pyrogen free water c - Seeded with 1000 ng/ml of Pseudomonas endotoxin d - Before turning on humidifiers nd - None detected
Hygienists, 1990). Therefore, the aerosol levels as measured on collecting filters in this study which exceeded 18.0 ng/m' are likely to be significant.
Air levels of endotoxin from ultrasonic and cool mist units, as shown by the close filter collections (Table 2), exceeded control background levels by about 15,000-fold for the cool mist and almost 8,000-fold for the ultrasonic unit. The largest emis- sions of endotoxin collected on the far filters also came from the cool mist (530 ng/m3) and the ultra- sonic unit 360 ng/m3. Evaporative humidifiers such as the warm mist and steam vaporizers did not aero- solize endotoxin (Table 3).
Home Studies Table 4 summarizes the results obtained from the humidifier reservoir samples obtained from homes
in 1987 in the Oak Ridge, Tennessee area. Bacteria were recovered from 84% of the samples. The pre- dominating genera were Pseudomonas, Flavobacter, and Bacillus. Micrococcus, Diphtheroides, and Staphy- lococcus were found in a few units. Only 33% of hu- midifiers contained recoverable fungi which were predominantly Cladosporium, Penkllium, and Asper- gillus. Candida, Rhodowrula, Fusarium, and Rhi- zobium were isolated from a few units.
Amoebae were detected in 71 of 88 units. Thirty amoebic isolates were tested for pathogenicity by in- tranasal inoculation of weanling mice. Twelve of these were later isolated from mouse lungs and one from brain tissue. Other protozoa including En- terobius were found in 35% of the units. In a subset of 27 homes with either ultrasonic or cool mist hu- midifiers, the water was also analyzed specifically for Legwnella. Two of the water samples yielded viable Legionella. Serotyping showed that one of the iso- lates was L. pneumophila serogroup one. This isolate had the antibody typing profile indicative of virulent Legionella most frequently associated with Legion- naires' disease outbreaks (Barbaree, 1993). The other LRgwneUa isolate is as yet unidentified.
Data obtained in response to questions addressed to humidifier owners indicated no obvious relation- ship between the type of water used, the thermostat setting, or the room where the units were used (Tyndall et al., 1989, 1991). All units receiving no decontamination treatment had microbial reservoir concentrations from lo5 - lo7 viable colony form- ing units (CFU) per ml. Units treated infrequently with chlorine bleach or vinegar had similar counts. Units with low microbial concentrations (< 1 05/ml) had been treated routinely with chlorine and/or hy- drogen peroxide by owners (Tyndall et al., 1989, 1991).
Air, reservoir, and scale samples collected from humidifiers in 22 homes during the spring of 1988 showed that the predominating bacteria and fungi in the reservoirs and scale were akin to those pre-
Table 4 Types of miciobial contaminants found in 88 reservoir water samples in different types of home humidifier
Type of Number Number and (%) of units containing humidifier evaluated Bacteria Fungi Amoebae Protozoa
Steam 6 6 (100) 2 (33) 4 (67) 2 (33) Ultrasonic 15 10 (66) 2 (13) 7 (47) 3 (20) Cool-Mist 15 12 (80) 8 (53) 15 (100) 5 (33) Console 16 15 (93) 2 (12) 13 (81) 10 (63) Furnace 36 31 (86) 15 (42) 32 (87) 11 (31)
Total 88 74 (84%) 29 (33%) 71 (81%) 31 (35%)

176 Tyndall et 01.: Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxions, and Allergens
viously encountered in the 1987 sampling of the home humidifier reservoirs. Even though the bac- terial concentrations in reservoirs of furnace and console units were similar to those in cool mist and ultrasonic units, only the latter units generally showed a marked propensity for aerosolization of the bacterial flora (Figure 2). The wide range, but high average concentration, of airborne bacteria in the cool mist and ultrasonic units is indicative of the few units that were treated routinely and had low bacterial reservoir concentrations. Airborne amoe- bae were detected in only one home where a cool mist humidifier was operated.
Discussion In these laboratory studies, mechanically produced aerosols from microbially seeded cool mist and ultra- sonic humidifiers contained microbes and endo- toxins. Consistent with these studies, ultrasonic and cool mist humidifiers from homes also aerosolized microbes while console, steam and fb-nace humidi- fiers showed little propensity for aerosolization of their bacterial contents. Whether in a clinical or home environment, aerosolization of potentially pathogenic microorganisms, allergens and associated endotoxins may present a respiratory health hazard.
The isolation of Legionella and pathogenic amoe- bae from humidifiers in homes in eastern Tennessee underscores the need to minimize or eliminate this potential source of exposure to microbial pathogens.
Legionella, the causative agent of the flu-like Ponti- ac fever and pneumonic Legionnaires’ disease, has previously been isolated from humidifiers and respir- atory equipment (Zuravleff et al., 1983; Arnow et al., 1982; Woo et al., 1986; Fields et al., 1989) in hospi- tals and from both hospital and home hot water heaters (Fields et al., 1989; Alary and Joly, 199 1; Bol- lin et al., 1985). This report confirms the isolation of L. pneumophila from home humidifier reservoirs and their potential for aerosolization.
Since amoebic dispersion from humidifiers is probably infrequent due to the relatively large size of the microorganism, the importance of free-living am- oebae in humidifier reservoirs relates to their interac- tions with Legionella. Initially laboratory studies (Rowbotham, 1980; Tyndall and Dominque, 1982; Anand et al., 1984, Barbaree, 1986) showed that free-living amoebae such as Acanthamoebae and Nae- gleria could be infected by and markedly amplify Le- gwnella. Subsequently, the presence of Hartmannella in tap water and hot water heaters was also linked to
the amplification and consequent aerosolization, via shower heads, of Legionella (Bollin et al., 1985; Wa- dowsky et al., 1991). Thus, the isolation of both Le- gionella and free-living amoebae from home humidif- er reservoirs suggests that the concomitant presence of these two microbes could result in amplification and dissemination of Legwnella.
In addition to overt pathogens such as Legionella and Acanthamoebae, discharge of Pseudomonads from humidifiers is of potential concern since they are opportunistic pathogens, can release endotoxins and cause infection in compromised individuals (Lennette et al., 1985). Similarly, allergies to fungal antigens are not uncommon, and amoebic antigens have been associated with allergic responses such as hypersensitivity pneumonitis and humidifier fever. Considering the size of water droplets dispersed by cool mist and ultrasonic humidifiers, it is not sur- prising that Legionella and other bacteria can be aerosolized by such units (Table 1). Laser analysis of droplet size showed that cool mist units generate and expel1 the greatest proportion of large water droplets of all tested units. The most likely expla- nation for the dissemination of bacteria but not of hydrophobic Asper~llus spores by ultrasonic units, is that aerosolized water was drawn from the bottom of the unit while the hydrophobic spores float on the surface of the water. Hydrophilic yeast cells were aerosolized by ultrasonic units (Tyndall et al., 1989, 199 1). While a greater percentage of smaller water droplets were aerosolized from ultrasonic units rela- tive to those emitted from cool mist units, a signifi- cant percentage of the drops was large enough to contain viable microorganisms. The lower concen- tration of microbial aerosolization by the console units in this study and as previously noted by Schul- ze et al. (1 976) probably relates to the evaporation of water from the belt as the means of humidifi- cation. It was not surprising that the steam vapor- izers and warm mist units showed little dissemi- nation of viable microbes since thermally induced evaporation of water is unlikely to produce aerosols containing viable microorganisms.
A recent report by Highsmith and Rodes (1 988) also compared the particulates discharged by vari- ous humidifier types. As in the studies reported here, these researchers showed that cool mist units discharged larger-sized particles compared to ultra- sonic and steam units. These authors also pointed out that the concentration of particulates discharged by ultrasonic and cool mist humidifiers exceeded the EPA standards for outdoor ambient air. Thus,

Tyndall et 0 1 . : Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxions, and Allergens 177
these types of humidifiers may discharge not only high levels of particulate matter, but also copious amounts of microorganisms and associated endo- toxin which may potentially affect the health of ex- posed individuals.
As was seen with bacteria, endotoxin was also readily aerosolized from the reservoirs of some home humidifiers. While both cool mist and ultra- sonic humidifiers aerosolized endotoxin from their reservoirs, warm mist and steam vaporizers did not. Seeding the reservoirs with 1000 ng/ml of endotoxin was based on studies (Rylander, 1986) where con- centrations of 160 to 5000 ng/ml were associated with illness. Rylander reported that inhalation chal- lenges with endotoxin from Gram-negative bacteria produce symptoms typical of acute episodes of hu- midifier fever (Rylander, 1986). Endotoxins from Gram-negative bacteria have been identified in res- ervoir water and in aerosols of humidifiers where outbreaks of humidifier fever have occurred (Flah- erty, 1984a; Flaherty, 1984b; Burrell, 1990; Ry- lander and Snella, 1983). In 32 out of 39 water samples from humidifiers associated with clinical cases of humidifier fever, the endotoxin level was in excess of 100 ng/ml (Rylander and Haglind, 1984).
The air levels of endotoxin obtained in the experi- mental chamber in the current study were above the levels that have been associated with the humidifier fever syndrome. According to recent guidelines from the American Conference of Governmental Industrial Hygienists, significant health effects may occur at inhalation exposures of 100 to 1000 times background levels and as such indicate that re- medial action should be taken. Endotoxin aerosoliz- ation by the cool mist and ultrasonic units in this study exceeded these criteria.
Both physicians and the public should be aware of the potential health hazard associated with hu- midifiers which aerosolize reservoir contents since they may contain overt pathogens, opportunistic pathogens, endotoxins, and allergens. To reduce this hazard, effective cleaning and maintenance practices as described elsewhere are essential (United States Consumer Product Safety Com- mission, 1988; United States Environmental Pro- tection Agency, 199 1).
Acknowledgements The authors would like to thank Kevin S. Ironside, Rebecca A. Jernigan, and Diana S. Katz for their expert technical assistance.
References Alary, M. and Joly, J.R. (1991) “Risk factors for contamination
of domestic hot water systems by Legionella”, Applied amd En- vironmental Microbwlogy, 57, 2360-2367.
h a n d , C., Skinner, A., Malic, A. and Kurtz, J. (1984) “Intra- cellular replication of Legionella pneumophila in Acanthamoeba palesrinensis”. In: Thomsbeny, C., Balows, A., Feeley, J.C., Jakubowski, W. (eds). Legionella: Proceedings of the Second Inter- national Symposium, Washington D.C., American Society for Microbiology, pp. 330-332.
Amow, P.M., Chou, T., Wed, D., Shapiro, E.N. and Kretzsch- mar, C. (1982) “Nosocomial Legionnaires’ disease caused by aerosolized tap water kom respiratory devices”, Journal of In- fectious Diseases, 146,460-467.
Ashton, I., Axford, A.T., Bevan C. and Cotes J.E. (1981) “Lung function of office workers exposed to humidifier fever anti- gen”. British Journal of Indusrrial Medicine, 38, 34-37,
Barbaree, J.M., Fields, B.S., Feeley, J.C., Gorman, G.W. and Martin, W.T. (1986) “Isolation of protozoa from water associ- ated with a Legionellosis outbreak and demonstration of intra- cellular multiplication of LegioneUa pneumophila”, Applied and Environmental Microbiology, 51, 422424 .
Barbaree, J. (1993) “Selecting a subtyping technique for use in epidemic investigations”. In: Breiman, R., DuFout, A., Le- gionella: Proceedings of the Fourth Internarional Symposium, Or- lando, Florida, January 2 6 2 9 1992, American Society for Microbiology, pp. 162-1 72.
Bollin, G.E., Plouffe, J.F., Para, M.F. and Hackman, B. (1985) “Aerosols containing Legionella pneumophila generated by shower heads and hot-water faucets”, Applied and Environmen- tal Microbwlogy, 50, 1 128-1 13 1 .
Burge, H.A., Solomon, W.R. and Boise, J.R. (1980) “Microbial prevalence in domestic humidifiers”, Applied and Environmen- tal Microbwlogy, 39, 840-844.
Burke, G.W., Carrington, C.B., Strauss, R., Fink, J. and Gaensl- er, E. (1977) “Allergic alveolitis caused by home humidifiers”, Journal of the American Medical Association, 238, 2705-2708.
Burrell, R. (1 990) “Immunomodulation by bacterial endotoxin”, Critical Reviews in Microbwlogy, 17(3), 189-209.
Covelli, H.D., Kleeman, J., Martin, J., Landau, V. and Hughes, R. (1973) “Bacterial emission kom both vapor and aerosol humidifiers”, American Review of Respiratory Diseases, 108,
Edwards, H. (1986) “The contribution of different microbes to the development of humidifier fever antigens”, Maladies des climatisseurs et des humidicateurs. Molina, C. (ed). Colloque
Edwards, J.H. (1 980) “Microbial and immunological investi- gations and remedial action after an outbreak of humidifier fever”, Britkh Journal of Industrial Medicine, 37, 55-62.
Fields, B.S., Sanden, G.N., Barbaree, J.M., Morill, W.E., Wa- dowsky, R.M., White, E.H. and Feeley, J.C. (1989) “Intra- cellular multiplication of Legionella pneumophila in amoebae isolated from hospital hot water tanks”, Current Microbwlogy,
Haherty, D.K. (1984a) “A cytophaga species endotoxin as a putative agent of occupation-related lung disease”, Infect& and Immunity, 43(1), 213-216.
Flaherty, D.K. (1984b) “Bacterial endotoxin isolated from a water spray air humidification system as a putative agent of occupation-related lung disease”, Infection and Immunity, 43(1), 20C212.
Gudelines for the Assessment of Bwaerosols in t k Indoor Environment (1990) Cincinnati, OH, American Conference of Govern- mental Industrial Hygienists.
Highsmith, V.R. and Rodes, C.E. (1988) “Indoor particle con- centrations associated with use of tap water in portable hu-
698-701.
INSERM, 135, 171-178.
18, 131-137.

178 Tyndall et 01.: Home Humidifiers as a Potential Source of Exposure to Microbial Pathogens, Endotoxions, and Allergens
midifiers”, Environmental Science and Echnology, 22, 1109- 11 12.
Klein, H.J. and Kunze, M. (1971) “Experimental investigations on the spread of Pseudomonas aeruginosa by a cold aerosol apparatus for moistening of the room temperature”, Zentral- blattfur BakreriOlogy (Orid, 216(2):199-209.
Kreiss, K. and Hodgson, M.J. (1 984) “Building-associated epi- demics”. In: Walsh, P.J., Dudney, C.S., Copenhaver E.D. (eds), Indoor Air Qd i ry , Boca Raton, CRC Press, pp. 87-106.
Lennette, E.H., Ballows, A., Hausler, W.J. Jr and Shadomy, H.J. (eds) (1985) Manual of Clinical Microbiology, 4th ed., Wash- ington, DC, American Society for Microbiology, pp. 350-372.
Miller, M.M. (1976) “Chronic hypersensitivity lung disease with recurrent episodes of hypersensitivity pneumonitis due to a contaminated central humidifier”, Clinical A k a , 6,45 1462.
Milton, D.K., Feldman, H.A., Neuberg, D.S., Bruckner, R.J. and Greaves, I.A. (1992) “Environmental endotoxin measure- ment: the Kinetic Limulus Assay with Resistant-parallel-line Estimation”, Environmental Research, 57(2):2 12-30.
Rowbotham, T.J. (1980) “Preliminary report on the pathogen- icity of LegzbneUa pneumophila for fkeshwater and soil amoe- bae”, Journal of Clilnical Pathology, 33, 1179-1 183.
Rylander, R. and Snella, M.C. (1983) “Endotoxins and the lung: cellular reactions and risk for disease”, Clinical Ahrgy, 33,
Rylander, R. and Haglind. P. (1984) “Airborne endotoxins and humidifier disease”, Clinical A l b , 14, 109-1 12.
Rylander, R. (1986) “The role of endotoxins in humidifier dis- ease” Maladies des climatisseurs et des humidicateurs. Moline C (ed). Cohque INSERM, 135, 179-192.
Schulze, T., Edmondson, B.E., Pierce, A.K. and Sanford JP (1976) “Studies of a new humidifjmg device as a potential source of bacterial aerosols”, American Revia0 of Respiratory Diseases, 96, 5 17-5 19.
Shiue, S.T., Schener, H.H., DeGraff, A.C. and Cole, S.R. (1990) “Hypersensitivity pneumonitis due to contamination of
332-244.
home humidifier”, Journal of Allergy and Clinical Immunology,
Solomon, W.R. (1974) ‘‘Fungus aerosols arising from cold-mist vaporizers”, Journal of Allergy and Clinical Immunology, 54,
Tourville, D.R., Weiss, W.I., Wertlake, P.T. and Leudemann, G.M. (1972) “Hypersensitivity pneumonitis due to contami- nation of home humidifier”, Journal of Allergy and Clinical Im- munology, 49, 245-25 1.
Tyndall, R.L., Dudney, C.S., Katz, D.S., Ironside, K.S., Jerni- gan, R.A. and Lehman, E.S. (1989 and 1991) Characterizatzbn of Microbial Conrent and Dispersion fiom Home Humidjk-s, Fi- nal Reports on Phase I, 11, and 111. Washington, D.C., Con- sumer Product Safety Commission (Project Number 86- 1283, 1989 and 1991).
Tyndall, R.L. and Dominque, E.L. (1982) “Cocultivation of Le- gionella pneumophila and kee-living amoebae”, Applied and En- vironmental Microbwlogy, 44, 954-959.
United States Consumer Product Safety Commission (1 988) “Dirty humidifiers may cause health problems”, Consumer Product SAFETY ALERT
United States Environmental Protection Agency (199 1) “Use and care of home humidifers”, EPA Indoor Air Facts, No. 8.
Wadowsky, R.M., Wilson, T.M., Kapp, N.J., West, A.J., Kuchta, J.M., States, S.J., Dowling, J.N. and Yee, R.B. (1991) “Multi- plication of Legionella spp. in tap water containing Hurtman- n e b verminformi?, Applied and Environmental Microbwlogy, 57,
WOO, A.H., Yu, V.L. and Goetz A. (1986) “Potential in-hospital modes of transmission of Legzbnella pneumophila”, American Journal of Medicine, 80, 567-573.
Zuravleff, J.J., Yu, V.L., Shonnard, J.W., Rihs, J.D. and Best, M. (1 983) “Legwnella pneumophila contamination of a hospital hu- midifier”, American Reviav of Respiratory Diseases, 128, 657- 661.
49, 245-251.
222-228.
1 950-1 955.