Clinical Radiation Safety.pdf
-
Upload
giermin-sahagun -
Category
Documents
-
view
230 -
download
0
Transcript of Clinical Radiation Safety.pdf

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 1/27
CLINICAL RADIATION SAFETY

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 2/27
PATIENT HANDLING AND
PROTECTION STANDARDS

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 3/27
1. A patient has just undergone an oralradiotherapy and will be staying in thehospital for 2 days. How can the hospitalsafely transfer the patient to his/her room?
What should be the precautions of thehospital to prevent contamination?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 4/27
HOW TO SAFELY TRANSPORT THEPATIENT ?
• Transport the patient by the most direct route.
• The patient shall not be left in public waiting areasor corridors. If necessary the transporter shall
remain in the area to keep other people at least 6feet from the patient.
•
When transporting the patient, do not shareelevators with other staff or patients.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 5/27
PRECAUTIONS TO PREVENTCONTAMINATION
•
The patient is restricted to his/her room where the walls haveproper shielding.
• The patient must use disposable eating utensils. Theseutensils should be placead in the special waste container afteruse.
•
The patient should flush the toilet two or three times aftereach use. This will insure that all radioactive urine is washedfrom the toilet bowl.
•
Both male and female patients must sit down on the toilet to
prevent urine splatter.• Adult family visitors are encouraged but avoid physical contact
with visitors.
• The floor should be covered with plastic.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 6/27
2. A patient was implanted with 192Ir and will be staying in the hospital for one nightafter the operation. What are theprotection standards that the nurses and
hospital staff should observe?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 7/27
PROTECTION STANDARDS TO BEOBSERVED
•
The nurses should not stay at the patient’s room after doingnecessary care to to the patient.
•
There should be a specific “stay times” posted at the patient’sdoor.
•
Housekeeping can only enter the room when escorted by anurse.
• The laundry should be placed in a linen bag and be saveduntil surveyed and released by the radiation oncologist.
• Visitors should be above 18 years old and should not bepregnant.
•
Visitors should be 6 feet away from the patient and should notstay for more than 2 hours.
• A radiation survey must be performed before the patient is
discharged.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 8/27
OPTIMIZATION OF RADIATION
THERAPY

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 9/27
3. Head-and –Neck Cancer was the case of one
patient in the hospital, treatment planningcame with the Neurosurgeons, RadiationOncologist, and medical Physicist. What istheir objective in creating a treatment plan?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 10/27
GOAL IN DESIGNING A TREATMENTPLAN
The objective is simply to deliver a prescribeddose to targets while sparing, to the greatestextent possible, critical structures.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 11/27
4. A study had eight cases of head and neck cancer.Two beam arrangements were placed in the treatmentplanning system, the B/L and the A-P fields. TheDVH’s for the cord does were recorded and compared
in both plans with a standard fraction size of 200cGy/fraction. The results showed that in the A-Parrangement 168.06cGy was the mean dose to thespinal cord whereas only 133.75cGy only in the B/L
arrangement. What are the possible effects for suchdoses? What can you conclude given the results?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 12/27
• Delivering a high dose to the spinal cord is the samething as cutting it down
• The A-P field arrangement delivered a higher dose
compared to the B/L hence, there is a need to sparethe cord at an earlier dose limit.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 13/27
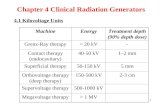
RADIATION THERAPY
• External-Beam Radiation Therapy
• Intensity-modulated radiation therapy (IMRT)
• Image-guided radiation therapy
•
Tomotherapy• Stereotactic radiosurgery
• Stereotactic body radiation therapy
• Proton therapy
•
Other charged particle beams
• Internal Radiation Therapy (Brachytherapy)
•
Systemic Radiation Therapy

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 14/27
5.
A patient comes in and complains of a sore throat
that has been on for 4 weeks, and is experiencingpain when swallowing. After evaluating the patient’smedical history, physical examination and tests havebeen run, the doctor diagnoses the patient as having
Oropharyngeal cancer. Radiation Oncologists,Medical Physicists, Medical Dosimetrists convenefor the patient’s treatment planning. What areconsiderations in such planning and what doesoptimization have to do with the treatmentplanning?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 15/27
WHEN A RADIOTHERAPY TREATMENTIS CREATED
• Physician provides prescription dose
•
Treatment planner chooses incident beam directions
•
Determines radiation fields
• Calculates final dose distribution
•
Physician reviews/approves the plan
Treatment plans can be of different strengths of weaknesses and it is thephysician’s goal to choose the best possible treatment that will provide theneeded dose to the tissue/organ whilst sparing other healthy tissues and
organs around it’s vicinity.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 16/27
MEDICAL EQUIPMENTMAINTENANCE

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 17/27
6. A radiation technician is about to commence
a linearity test for their dose calibrator using a 50mCi Tc-99m source (half life is 6 hours). Thetechnician started at 8am, and recorded thereadings in regular intervals. The recorded
activity was plotted against time, but the graphlooked scattered and not linear at all. Whatpossible reasons could explain this?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 18/27
WHAT COULD’VE HAPPENED?
• Loss of battery voltage on the chamber
• Pressure leak from the chamber
• Temperature changes in the chamber due to
environmental conditions (change in heat or air-conditioning systems)
• Operator / human error

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 19/27
7. A radiation technician forgot to set-up the
collimators for their clinic’s gamma camera. Hefailed to notice this and continued to use thegamma camera on a patient for diagnosticpurposes. What would happen?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 20/27
WHAT WOULD HAPPEN?
The Images will be blurry.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 21/27
TREATMENT VENUE
SPECIFICATIONS & STRATEGIES

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 22/27
8. A female patient was treated for thyroidcarcinoma. After a few hours ofradioiodine administration, it was foundthat she was 3 weeks pregnant. What can
happen? What should be done?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 23/27
The dose will endanger the development of thefetus. To reduce the risks, advise the patient to
drink lots of water and urinate frequently.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 24/27
9. After performing the daily warm-up routines
for their linear accelerator, a radiation therapistprepares the treatment for a breast cancerpatient. What should be done if the patient has ahistory of twitching and restlessness?

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 25/27
A mold should be prepared for the patient sothat she will stay still during treatment.

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 26/27
REFERENCES
•
https://rpop.iaea.org/RPOP/RPoP/Content/SpecialGroups/1_PregnantWomen/PregnancyNuclearMedicine.htm
•
https://www.mskcc.org/cancer-care/patient-education/radiation-therapy-breast-chest-wall
•
http://www.nuclearfields.com/collimators-nuclear-medicince.htm
•
http://www.biodex.com/sites/default/files/documents/tips/tip-dose-calibrator-linearity-testing-14194.pdf
•
http://web.stanford.edu/dept/EHS/prod/researchlab/radlaser/Hospital_Guidance_document.pdf
•
http://www.ucalgary.ca/rop/node/174
•
http://gray.mgh.harvard.edu/attachments/article/166/166_lecture0_intro.pdf

8/20/2019 Clinical Radiation Safety.pdf
http://slidepdf.com/reader/full/clinical-radiation-safetypdf 27/27
CLINICAL RADIATION SAFETY
ALCANTARA. JIMENEZ. MUNGCAL