ACLS Scenario
Transcript of ACLS Scenario

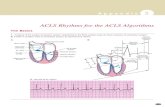
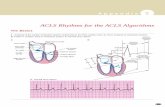
ADVANCED CARDIOVASCULAR LIFE SUPPORT
EVALUATION SCENARIOS
February 2007

1. These scenarios are NOT for student distribution and are considered CONFIDENTIAL. 2. Use these scenarios only for evaluation. Do not use for practice
scenarios. 3. Allow student to choose their own scenario by asking them to choose a letter
from A-S or; in consultation with course faculty, choose specific evaluation scenarios.
4. Scenarios are provided as guidelines for faculty use and can be modified to
suit your participant profile and related protocols. These are guidelines for use of the attached ACLS scenarios 'A' through 'S'. If you have any questions in regards to any of these scenarios please contact your local Service Centre.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO AACLS SCENARIO A
STUDENT INFORMATION: A 56 year old male (100 kg) is found on the living room couch at home. At 0300, the patient woke up with chest pain and called for help.
Depending on candidate, care takes place in either ambulance or
emergency department. Initial Assessment: SKIN: Pale/Diaphoretic/Clammy
CVS: No palpable radial or brachial pulse. No blood pressure available.
CNS: Responds to loud voice only. RESP: Equal air entry to all fields, RR 8
Monitor: third degree heart block with HR 30
INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted. Support airway and breathing with high flow oxygen or BVM
1. Prepare for transcutaneous pacemaker 3rd degree heart block
↓
V-Fib ↓
2nd Degree Block Type II
2. Give atropine 0.5 mg and repeat while pacemaker being set
up.
3. Rhythm changes to vf as pacemaker being turned on
4. Follow vf algorithm to amiodarone/lidocaine
5. After next defibrillation rhythm changes to 2nd degree block type II. VITALS: HR 56, BP 70/palp, R 20, conscious but confused
6. Prepare transcutaneous or transvenous pacing. Patient arrives in ER or is transferred to the CCU.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO B
STUDENT INFORMATION: A 53 year old female (80 kg) is found in a sauna. She appears to be unconscious.
Initial Assessment: SKIN: Ashen/Diaphoretic/Warm
CVS: Carotid pulse only. HR 30, no measurable BP RESP: RR 4, A/E equal all fields
CNS: No response to any stimulus Monitor: 2nd degree block Type II with HR 30 INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Ventilate with BVM (or insert invasive airway if BVM not adequate) and start IV.
2. Attempt transcutaneous pacing, but no capture. Give
Atropine, may consider Dopamine or Epinephrine infusion.
3. Rhythm changes to Asystole. 4. Follow Asystole algorithm to first dose of Epinephrine.
5. Rhythm changes to ventricular fibrillation. Follow algorithm to amiodarone/lidocaine and subsequent defibrillation. Rhythm changes to normal sinus rhythm.
VITALS: HR 70, BP 100/60, few spontaneous respirations 6. Provide supportive post-resuscitation care, consider
maintenance infusion of anti-arrhythmic of choice.
2nd Degree Block Type II ↓
Asystole ↓
V-Fib ↓
NSR with a pulse
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO C
STUDENT INFORMATION: A BLS ambulance crew initiates care to a 63 year old male (80 kg) complaining of general weakness. He denies chest pain or discomfort. Care is continued either in an advanced life support ambulance or emergency department.
SKIN: Pale/Warm/Dry
CVS: Slightly irregular pulse, HR 46, BP 80/50 RESP: Good air entry bilaterally, adequate volume, RR 14 CNS: Alert and oriented Monitor: 2nd Degree Block Type II
INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in the time frame allotted.
1. Follow Bradycardia algorithm, but pacemaker not immediately available.
2. After 2nd Atropine patient complains of increased weakness. HR 36, monitor shows 3rd degree heart block. Transcutaneous pacing now available if requested.
3. During pacing attempt, rhythm changes to ventricular
fibrillation. 4. Follow ventricular fibrillation algorithm, but amiodarone is not
available. 5. After Lidocaine and subsequent defibrillation, rhythm changes
to Sinus Bradycardia with PVCs, VITALS: HR 50, BP 100/70, RR 10 Ask candidate the maximum dose of lidocaine.
6. Provide supportive post-resuscitation care, consider
maintenance infusion.
2nd Degree Block Type II ↓
3° Block ↓
V-Fib ↓
Sinus Bradycardia
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO D
STUDENT INFORMATION: A 45 year old male (90 kg) is brought into the Emergency Department by his wife. He is complaining of flu like symptoms which started 24 hours ago.
Initial Assessment: SKIN: Pale/Dry/Warm CVS: Palpable peripheral and central pulses, rapid pulse. BP
100/70 RESP: Air entry equal bilaterally, no respiratory distress. RR18 CNS: Anxious but alert Monitor: Ventricular tachycardia, HR approximately 140 INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Appropriate supportive care including IV, O2, cardiac monitor
2. Follow stable Tachycardia algorithm to amiodarone and preparation for cardioversion.
3. Patient then complains of chest pain and SOB.
VITALS: BP 60/palp, HR >150, RR28
4. Follow unstable tachycardia algorithm to sedation and 1st
attempt at cardioversion.
5. Rhythm changes to ventricular fibrillation, with no palpable pulse.
6. Follow Ventricular Fibrillation algorithm to first defibrillation.
Rhythm changes to Asystole.
Stable V-Tach with pulse
↓
Unstable V-Tach with pulse ↓
V-Fib ↓
Asystole ↓
Deceased 7. There is no response to epinephrine/vasopressin or atropine.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO E
STUDENT INFORMATION: A 60 year old male (75 kg) collapses outside his home while shoveling his sidewalk.
SKIN: Cyanotic/Cold/Diaphoretic CVS: No pulses RESP: Apneic CNS: No response Monitor: Asystole INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Initiate CPR, follow Asystole algorithm to ventilation with BVM (or insert invasive airway if BVM not adequate) and first dose of epinephrine.
2. Rhythm changes to ventricular tachycardia, there is no
palpable pulse.
3. After Amiodarone/Lidocaine and defibrillation, rhythm changes to 3rd degree heart block, with a palpable pulse.
Asystole ↓
V-Tach ↓
3rd Degree Heart Block
VITALS: HR 32, BP 80/60, no respiratory effort
4. Initiate transcutaneous pacing.
VITALS: HR 70, BP 100/palpation, RR 4
5. Continue to support ventilations, maintain TCP pacing. Admit to Coronary Care Unit.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO F
STUDENT INFORMATION: You are called to assess a patient who is “found down”. On arrival you see a 45 year old male (100 kg) is having a seizure. The seizure ceases 30 seconds after your arrival.
SKIN: Cyanotic/Diaphoretic/Clammy CVS: Carotid pulse only, HR 24, unable to obtain a BP RESP: RR 4 CNS: Unresponsive Monitor: Sinus Bradycardia with HR 24 INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
Support Airway and Breathing, obtain IV access
1. Follow Bradycardia algorithm to 2nd Atropine or TCP. Consider H’s and T’s.
2. Patient goes to Asystole. Follow to Epi/Vasopressin and
Atropine.
3. Rhythm changes to Ventricular Fibrillation. Follow to Amiodarone/Lidocaine and subsequent defibrillation.
4. Rhythm changes to NSR with PVCs.
VITALS: HR 66, BP 120/70, spontaneous RR 6
Sinus Bradycardia ↓
Asystole ↓
V-Fib ↓
NSR with PVCs
5. Maintain airway, oxygenate, and follow post-resuscitation care. Consider Amiodarone/Lidocaine maintenance infusion.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO G
STUDENT INFORMATION: You are presented with a 30 year old male (80 kg) who requires assistance after playing sports. He states his heart rate will not slow down. He now has chest pain and increasing weakness. One hour has passed since the onset.
SKIN: Ashen/Moist/Cool CVS: HR approximately 200, BP 70/palp. RESP: 32, equal air entry CNS: Alert, but feels extremely weak and dizzy with chest pain
7/10 Monitor: SVT (Narrow Complex) INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted. Provide oxygen, obtain IV access, place patient on monitor.
1. Candidate should consider cardioversion as first treatment, with sedation. May consider Adenosine while preparing for cardioversion.
2. After two synchronized shocks, rhythm becomes Ventricular
Fibrillation. Student should turn off synchronized mode.
3. Follow Ventricular fibrillation algorithm to after 1st epinepherine/vasopressin and subsequent defibrillation.
4. ECG becomes PEA (Sinus Bradycardia without pulses), HR
45
5. Follow PEA algorithm, including differential diagnosis. Patient will improve after fluid boluses, to sinus rhythm.
Unstable SVT ↓
V-Fib ↓
PEA (sinus bradycardia) ↓
Sinus rhythm
VITALS: HR 70, BP 100/60, occasional spontaneous respiration Continue supportive post-resuscitation care and transfer to CCU.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO H
STUDENT INFORMATION: A 55 year old female (90 kg) complains of chest pain. Her past medical history includes a myocardial infarction 2 years ago. This chest pain is the same as her heart attack pain, only worse.
SKIN: Pale/Cool/Moist CVS: HR 64 irreg, BP 120/80 RESP: RR 14, breathing slightly labored CNS: Alert and oriented Monitor: Sinus rhythm with multi-focal PVC’s INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Provide supportive care including IV, O2, place patient on a cardiac monitor
2. Monitor shows NSR with multifocal PVC’s. Patient complains
that the pain is getting worse and then collapses.
3. Rhythm changes to Ventricular Fibrillation.
4. Follow to first dose of amiodarone/lidocaine -- the rhythm changes to Asystole.
5. Follow Asystole algorithm to airway control (BVM or advanced
airway if BVM not adequate) and epinephrine/vasopressin, then rhythm changes to Ventricular Fibrillation.
6. De-fib X 1, converts to Sinus Bradycardia with frequent
PVC’S
Sinus rhythm with PVC’s ↓
V-Fib ↓
Asystole ↓
V- Fib ↓
Sinus Bradycardia VITALS: HR 50, BP 80/50, occasional spontaneous respiration
7. Student should perform appropriate post-resuscitation care
and consider whether to treat bradycardia/hypotension. Consider anti-arrhythmic loading dose and maintenance infusion if/when BP adequate.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO I
STUDENT INFORMATION: A 50 year old man (100 kg) is admitted to the ward with episodes of syncope NYD. Two hours later he starts to complain of chest pain. He has no cardiac history whatsoever.
SKIN: Pale/Cool/Diaphoretic CVS: Weak radial pulses, BP 60/0 RESP: Equal air entry all fields, RR 28 CNS: Very anxious Monitor: Ventricular Tachycardia, HR 220 INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. When the student begins to ask for the crash cart, the patient becomes unconscious and pulseless, student should start BLS and call for help.
2. Rhythm changes to Ventricular Tachycardia without a pulse.
3. Follow algorithm to first epi/vasopressin and defibrillation.
4. Rhythm changes to Ventricular Fibrillation.
5. Follow algorithm to first Amiodarone/Lidocaine and
defibrillation. Rhythm changes to Pulseless Electrical Activity, with NSR HR 75.
V-Tach (with a pulse) ↓
V-Tach (pulseless) ↓
V-Fib ↓
PEA
6. Follow PEA algorithm but patient fails to respond to all appropriate treatment.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO J
STUDENT INFORMATION: While taking the BP of a 75 year old male (80 kg) he becomes limp and unresponsive.
SKIN: Pale/Warm/Dry CVS: No pulse RESP: Absent, no respirations CNS: No response Monitor: Ventricular tachycardia without a pulse. INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Student should start BLS and call for help. 2. Rhythm is pulseless Ventricular Tachycardia. Follow to first
Lidocaine and defibrillation, amiodarone is not available. 3. Rhythm changes to type II, 2nd Degree Heart Block rate of 40.
Student should attempt TCP.
4. Rhythm changes to paced rhythm with good capture.
VITALS: HR paced at 70, BP 80/44, R 12 spontaneous, unresponsive.
5. Student should consider fluids, increasing pacer rate, and/or
inotropes. Rhythm changes to Asystole, and there is loss of pacemaker capture.
V-Tach without pulse ↓
2nd Degree Heart Block, Type II
↓
Paced rhythm ↓
Asystole ↓
Deceased
6. Unable to pace asystole, unresponsive to epinephrine and atropine
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO K
STUDENT INFORMATION: At 0230, while making rounds, you hear a noise from a room and find a 60 year old female (50 kg) on the floor.
SKIN: Cyanotic/Cool/Moist CVS: No pulse RESP: Absent CNS: Unresponsive Monitor: Ventricular Fibrillation INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted. BLS measures then immediate defibrillation when crash cart arrives
1. Follow algorithm to first dose Amiodarone/Lidocaine and defibrillation.
2. Rhythm changes to NSR with a rate of 45, no spontaneous
respirations, no pulse. Student should work through differential diagnosis of PEA.
3. Despite epinephrine and atropine, rhythm changes to
Asystole.
4. Follow Asystole algorithm, but patient fails to respond to all appropriate treatment.
V-Fib ↓
PEA ↓
Asystole ↓
Deceased
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO L
STUDENT INFORMATION: A 58 year old male (70 kg) is found beside a table in the hospital cafeteria. He appears to have been eating supper.
SKIN: Cyanotic/Cool/Moist CVS: No pulse RESP: No resps CNS: No response Monitor: NSR rate 50 INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Student should identify a full airway obstruction, follow BLS algorithm, obstruction can be relieved with chest thrusts or laryngoscope and McGills.
2. Follow PEA algorithm to second epinephrine/vasopressin.
3. Rhythm changes to Ventricular Tachycardia.
4. Follow Ventricular tachycardia algorithm to the first
Amiodarone/Lidocaine.
5. Rhythm changes to NSR.
VITALS: HR 70, BP 100/56, RR few spontaneous breaths.
Airway Obstruction ↓
PEA ↓
Ventricular Tachycardia ↓
NSR 6. Assist and maintain airway and move to emergency
department.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO M
STUDENT INFORMATION: A 40 year old male (80 kg) is brought to Emergency with CPR in progress, having collapsed in a park while jogging.
SKIN: Blue/Cool/Mottled CVS: No pulse RESP: No respirations CNS: No response Monitor: Ventricular Fibrillation INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Follow Ventricular Fibrillation to 2nd epi/vasopressin and defibrillation
2. Rhythm changes to PEA, with NSR rate of 80, but still no
pulse or respirations are present. Student to review the differential diagnosis of PEA.
3. After next epinephrine the rhythm changes to VF.
4. After next defib rhythm changes to NSR.
VITALS: HR 70, BP 80/palpable, no spontaneous respirations.
5. Consider fluids/inotropes. Transfer to CCU for transvenous
pacing.
V-Fib ↓
PEA ↓
V-Fib ↓
NSR
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO N
STUDENT INFORMATION: A 55 year old female (85 kg) is complaining of weakness. No chest pain, but has occasional 'fluttering' sensation in her chest.
SKIN: Pale/Dry CVS: HR: 110, BP 120/80 CNS: Alert and Oriented RESP: Equal air entry all fields Monitor: Sinus Tachycardia INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. During assessment, patient has run of VentricularTachycardia with the sensation of weakness lasting 3-5 seconds then converts spontaneously back to NSR.
2. When student requests IV patient goes into sustained
Ventricular Tachycardia. There are no radial pulses present and only weak carotid pulses. Patient becomes more obtunded.
3. After 3rd synchronized cardioversion attempt, patient goes into
Ventricular Fibrillation.
4. Follow Ventricular fibrillation algorithm to Amiodarone/Lidocaine. Monitor changes to Asystole.
5. Follow Asystole algorithm, but patient does not respond to
appropriate treatment
Sinus Tachycardia ↓
Run of V-Tach with pulse ↓
V-Tach with pulse ↓
V-Fib ↓
Asystole
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO O
STUDENT INFORMATION: You find an 80 year old make (60 kg) collapsed on a hospital hallway floor.
SKIN: Cyanotic/Clammy/Cool CVS: No pulse CNS: No response RESP: No respirations Monitor: Ventricular fibrillation INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Student to follow BLS-One Rescuer CPR. Crash Cart will arrive after student manages BLS for two minutes.
V-Fib ↓
Asystole ↓
V-Tach without pulse ↓
Sinus rhythm with bigeminy PVCs
2. Follow Ventricular Fibrillation algorithm to
Amiodarone/Lidocaine. The rhythm changes to Asystole.
3. Follow Asystole algorithm to second dose of epinephrine. Rhythm changes to Ventricular Tachycardia without a pulse.
4. After defibrillation, the patient converts to sinus rhythm with
frequent PVCs. Vitals are HR 82, occasional spontaneous respiration, BP 90/60.
5. Supportive care, consider maintenance infusion of anti-
arrhythmic.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO P
STUDENT INFORMATION: A 60 year old male (100 kg) is brought into the Emergency Department with chest pain. The pain decreases slightly after O2 is administered by EMS. As you continue assessing the patient, he complains of feeling faint.
SKIN: Pale/Clammy CVS: Weak radial pulse, HR 180, BP 80/Palpation RESP: Equal air entry, RR 28 CNS: Responds to loud voice only Monitor: PSVT INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Follow PSVT algorithm, to 3rd synchronized cardioversion. Consider sedation prior to cardioversion. It is also acceptable to try adenosine while preparing to cardiovert, but it has no effect.
2. Rhythm changes to Ventricular Fibrillation.
3. Follow ventricular fibrillation algorithm to
Amiodarone/Lidocaine then defib. Rhythm changes to Asystole.
4. Follows Asystole algorithm to 2nd epi/vasopressin. Student
should review the differential diagnosis for asystole.
5. After fluid bolus, the rhythm changes to Normal Sinus Rhythm.
VITALS: HR 90, BP 100/80, RR 8
6. Student to perform supportive post-resuscitation care. May
consider maintenance infusion of anti-arrhythmic.
PSVT ↓
V-Fib ↓
Asystole ↓
NSR
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO Q
STUDENT INFORMATION: An 80 year old female (75 kg) calls EMS. She has had dizziness and weakness for two hours. She has no chest pain or discomfort.
SKIN: Pale/Cyanosed lips CVS: Weak radial pulse, BP 70/40, HR 36 CNS: Slow, but responds to all questions. RESP: Equal air entry, RR 16 Monitor: 3rd Degree Block INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Follow Bradycardia algorithm to TCP. There is no clinical or mechanical capture. Student to consider inotropic infusion. The patient then becomes unresponsive. Rhythm changes to Ventricular Fibrillation.
2. Follow Ventricular Fibrillation algorithm to
amiodarone/lidocaine and subsequent defibrillation. Rhythm changes to Asystole.
3. Follow Asystole algorithm, but patient fails to respond.
3rd Degree Heart Block ↓
V-Fib ↓
Asystole ↓
Deceased
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO R
STUDENT INFORMATION: An 80 year old female complains of weakness, dizziness and slight non-radiating chest pain.
SKIN: Pale/Cyanosed CVS: Weak radial pulse, HR 36, BP 70/palpation. CNS: Responds to all questions appropriately. RESP: Equal air entry all fields, RR 24 Monitor: Sinus Bradycardia with frequent PVCs. INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. Follow bradycardia algorithm. Have patient go from sinus bradycardia to 2nd Degree Type II Block then 3rd Degree Block.
2. While student considers TCP, patient becomes
pulseless/apenic. Rhythm changes to Ventricular Fibrillation.
3. Follow Ventricular Fibrillation algorithm to Lidocaine and subsequent defibrillation, amiodarone is not available. Rhythm changes to Normal Sinus Rhythm.
VITALS: HR 80, BP 110/70, starting to make respiratory effort
Sinus Bradycardia with frequent PVC’s
↓
2nd degree type II ↓
3rd degree block ↓
V-Fib ↓
NSR
4. Supportive care should be given en route to the hospital.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007

ACLS SCENARIO S
STUDENT INFORMATION: A 38 year old man arrives at the Emergency Department with friends complaining of palpitations following an old timer's hockey game.
SKIN: Pale, warm and dry CVS: Strong peripheral pulse HR 170, BP 110/70 CNS: Responds to all questions appropriately. RESP: Equal air entry all fields, RR 22, no respiratory distress Monitor: Narrow complex SVT INSTRUCTOR INFORMATION: Note to Instructor: Student to complete as much as possible in time
frame allotted.
1. O2, IV, monitor. Student to attempt vagal maneouvers. 2. Follow stable tachycardia to 2nd Adenosine.
3. Patient develops chest pain, altered LOC. Vitals are HR 220,
BP 70/palpation.
4. Follow unstable Tachycardia algorithm to 3rd attempt at synchronized cardioversion. Consider sedation prior to cardioversion.
5. Rhythm changes to pulseless Ventricular Tachycardia with
patient unconscious.
6. Follow Ventricular Tachycardia algorithm to Amiodarone/Lidocaine and subsequent defibrillation.
7. Rhythm changes to Normal Sinus Rhythm.
Stable SVT ↓
Unstable SVT ↓
V-Tach ↓
NSR
VITALS: HR 90, BP 110/70, occasional spontaneous respiration
8. Initiate post-resuscitation supportive care. Consider infusion
of maintenance anti-arrthymic.
Developed by MacEwan College, Edmonton, Alberta, Canada Revised by Heart and Stroke Foundation of Canada - ACLS Workgroup February 2007