Document
Transcript of Document

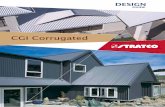
©2005 FASEB The FASEB Journal express article 10.1096/fj.05-3826fje. Published online June 29, 2005. Enzyme replacement therapy results in substantial improvements in early clinical phenotype in a mouse model of globoid cell leukodystrophy Wing C. Lee, Andrew Courtenay, Frederick J. Troendle, Melody L. Stallings-Mann, Chad A. Dickey, Michael W. DeLucia, Dennis W. Dickson, and Christopher B. Eckman Mayo Clinic College of Medicine, Departments of Pharmacology and Neuroscience, 4500 San Pablo Road, Jacksonville, Florida 32224 Corresponding author: Christopher B. Eckman, Mayo Clinic College of Medicine Birdsall Building, Room 327, 4500 San Pablo Road, Jacksonville, Florida 32224. E-mail: [email protected]
ABSTRACT
Globoid cell leukodystrophy (GLD) or Krabbe disease is a devastating, degenerative neurological disorder caused by mutations in the galactosylceramidase (GALC) gene that severely affect enzyme activity. Currently, treatment options for this disorder are very limited. Enzyme replacement therapy (ERT) has been shown to be effective in lysosomal storage disorders with predominantly peripheral manifestations such as type I Gaucher’s and Fabry’s disease. Little however is known about the possible benefit of ERT in GLD, which has a substantial central nervous system component. In this study, we examined the effect of peripheral GALC injections in the twitcher mouse model of the disease. Although we were unable to block the precipitous decline that normally occurs just before death, we did observe significant early improvements in motor performance, a substantial attenuation in the initial failure to thrive, and an increase in life span. Immunohistochemical and activity analyses demonstrated GALC uptake in multiple tissues, including the brain. This was associated with a decrease in the abnormal accumulation of the GALC substrate psychosine, which is thought to play a pivotal role in disease pathology. These results indicate that peripheral ERT is likely to be beneficial in GLD.
Key words: Krabbe disease • lysosomal storage disorder • protein therapy • twitcher • blood brain barrier
loboid cell leukodystrophy (GLD), or Krabbe disease, is a devastating, degenerative neurological disorder caused by mutations in the galactosylceramidase (GALC) gene that severely affect enzyme activity (1-4). Classical GLD is initially characterized by
irritability and fluctuating muscle tone followed by opisthotonic posturing, visual failure, hypertonic fits, and loss of tendon reflexes, with death typically occurring usually before 2 years of age (1). GALC enzymatic activity is localized predominately in lysosomes, where it hydrolyzes galactosylceramide, a major glycolipid of central and peripheral myelin. During this
G
Page 1 of 17(page number not for citation purposes)

process, psychosine is formed as a byproduct (5–7). Deficiency in GALC causes an abnormal accumulation of psychosine, which is believed to be cytotoxic (8–11), particularly in myelin-forming cells such as central nervous system (CNS) oligodendrocytes and Schwann cells. Loss of these myelin-forming cells leads to demyelination in both central and peripheral nerves during early developmental stages (12, 13). Other pathological features of the disease include axonal loss, astrocytic gliosis, and infiltration of macrophages with characteristic galactosylceramide inclusions (“globoid cells”) (14). Current treatment options for the disease are very limited. The most successful to date appears to be bone marrow transplantation. When performed either in individuals with late-onset disease or in those who were diagnosed with the disorder very early and before symptoms are present, it can be quite effective (15–17). Unfortunately, for many individuals bone marrow transplantation is not a viable option as there is little evidence of its effectiveness if performed after symptoms are apparent in the more common infantile form of the disease and the treatment strategy itself carries substantial risk.
Enzyme replacement therapy (ERT) has been shown to be safe and effective for the treatment of peripheral clinical manifestations in other lysosomal storage disorders (LSDs), such as type I Gaucher’s disease and Fabry’s disease, among others (18–23). The potential use of ERT for GLD, however, has received very little attention due predominately to the perceived need for the enzyme to cross the blood-brain barrier (BBB) to achieve a positive clinical outcome and the perceived inability for GALC to cross the BBB in an active form (2). We were intrigued recently by the findings from at least two ERT studies for other LSDs that have shown some evidence of storage reduction in the brain following peripheral injection of other enzymes (24, 25). Unfortunately, no follow-up biochemical or histological analysis of the brain to examine enzyme levels or activity was performed in either of these other studies to determine whether the enzyme itself reached the brain.
A recent report by De Gasperi and colleagues showed that when animals transgenic for GALC were crossed into a mouse model of the disease, the resultant progeny were similar to nonaffected animals (26). While clearly not directly useful clinically, these data provided strong evidence that if GALC could reach the appropriate targets, a significant phenotypic correction could occur. This finding, coupled with the results of storage reduction in the brain in at least two other LSDs following peripheral ERT, led us to reevaluate the potential for the use of ERT for GLD.
MATERIALS AND METHODS
Chemicals and reagents
All chemicals were purchased from Sigma (St. Louis, MO). The CL1475 polyclonal antibody against GALC was custom prepared by Affinity Bioreagents (Golden, CO) raised against the purified murine GALC recombinant protein produced by HEK293 GALC stable cells. The antiserum was then affinity purified by the antigen immobilized on CNBr-activated sepharose 4B (Amersham Biosciences, Piscataway, NJ) according to the manufacturer’s instructions.
Page 2 of 17(page number not for citation purposes)

Cloning and construction of murine GALC expression vector
A GALC cDNA was cloned from murine testis total RNA using sequence previously published (27). Primers used were oligo dT, GALC forward (5′-GTAGGATCCGCACAATGGCTAACAG-3′) and GALC reverse (5′-GAGAATTCCTAGCGAGCAGCTTC-3′). The cDNA was inserted into pSecTag2b (Invitrogen, Carlsbad, CA) using the following primers: 5′ prime GALC (5′-GAGAGGATCCCATCATCATCATCATCATGATGACGATGACAAGTACGTGCTAGACGACTCCGACGG-3′), 3′ prime GALC (5′-TTTTCCTTTTGCGGCCGCCTAGCGAGCAGCTTCCACG-3′). The 5′ prime GALC primer contained a 6-histidine tag to facilitate purification of GALC.
Development of a stably transfected GALC-expressing cell line
The GALC cell line was generated by transfecting HEK 293 cells with pSecTag2b-mGALC DNA using Lipofectamine (Invitrogen) according to the manufacturer’s instructions. Stable transfectants were selected for 4 wk in Opti-MEM plus 400 μg/ml Zeocin (Invitrogen). Surviving clones were individually picked and expanded. GALC enzymatic activity was measured in media taken from each clone, and the clone that expressed the highest level of GALC enzymatic activity was used. For protein production, the cells were grown in Opti-MEM medium (Invitrogen).
Production of recombinant GALC protein
GALC-293 cells were grown in Opti-MEM with 10% fetal bovine serum (FBS) and maintained in 400 μg/ml Zeocin (Invitrogen). Medium was routinely collected every 3 days once the cells attained 80% density. One liter of medium was added with 5 ml of Ni-NTA agarose (Qiagen, Valencia, CA) and slowly stirred for 1 h at 4°C. The beads were then packed into a column by gravity flow and equilibrated in buffer A (50 mM sodium phosphate, pH 8, 300 mM sodium chloride, 10 mM imidazole). Ten bed-volumes of buffer B (50 mM sodium phosphate, pH 8, 300 mM sodium chloride, 20 mM imidazole) were used to wash the column at gravity flow, and the recombinant protein was eluted with buffer C (50 mM sodium phosphate, pH 8, 300 mM sodium chloride, 250 mM imidazole). The purified protein was desalted by dialysis in 0.9% sodium chloride solution and sterile concentrated by the centrifugal filtration (Ultrafree Biomax-50, Millipore, Bedford, MA) according to the manufacturer’s instructions. The protein concentration was measured by BCA protein assay kit (Pierce, Rockford, IL), and GALC purity was checked by silver staining following polyacrylamide gel electrophoreses. Recombinant enzyme was stored at –80°C before use.
Animals
The animal protocol used in this study has been approved by the Institutional Animal Care and Use Committee at the Mayo Clinic. Breeding pairs of twitcher heterozygotes and C57Bl/6J mice were purchased from Jackson Laboratory (Bar Harbor, ME). The genotypes of pups born from the twitcher heterozygotes were determined by PCR (27).
Page 3 of 17(page number not for citation purposes)

GALC administration
In the initial experiment (Fig. 1; Table 1), twitcher mice were injected i.p. once per week at a concentration of 6 mg/kg in 0.9% saline in a total volume of 100 μl on postnatal day (PND) 10 or 20 as indicated in Fig. 1. The administration frequency was increased to once every other day in all subsequent experiments (Fig. 2–4; Table 1) given that the half-life of the recombinant enzyme was subsequently determined to be in the range of 1–2 days in the liver following injection (data not shown).
Body weight assessment
Mice were weighed by using a triple beam balance every other day immediately before each injection beginning at day 20. Weights are presented as the percent increase in the animal relative to their own weight at day 20.
Gait analysis
Front paws were painted blue, and hind feet were painted red with nontoxic paint. The mice were placed in a plastic tunnel with a strip of white paper covering the floor. At the end of the tunnel was an enclosed black box to encourage the mouse to cross the paper and into the box. The test was repeated until the mouse left at least five pairs of adjacent footprints.
Determination of survivability
Experimental mice were maintained until becoming moribund in accordance with the acceptable practice of laboratory animal care without forced feeding or other substantial interventions. The date the animals became moribund was recorded as the last day of survival and the animals were killed.
Tissue harvesting and processing
Mice were killed by CO2 asphyxiation followed by perfusion with phosphate buffer saline (PBS), pH 7.4. Brain, liver, kidney, and sciatic nerve were rapidly dissected. Tissues for GALC substrate cleavage assays and psychosine determination were stored at –80°C. Tissues for histopathology studies were immersion-fixed in 10% formalin overnight at room temperature. Tissues were processed for paraffin embedding using an autoprocessor (Shandon, Pittsburgh, PA). Paraffin-embedded serial sections were cut at 5 μm.
Colorimetric in vitro GALC substrate cleavage assay
The method was used essentially as described previously by Gal et al. (28) with a modification in homogenization procedures. Kidney and liver tissues were dounced in 6 volumes modified RIPA buffer (50 mM Tris-HCl, pH 7.4, 150 mM sodium chloride, 1 mM EDTA, 1 mM sodium orthovanadate, 1 mM sodium fluoride, and Complete protease inhibitor cocktail tablet (1 tablet per 50 ml; Roche, Indianapolis, IN). Brains were homogenized in 4 volumes of the same solution. The homogenates were centrifuged at 20,000g for 1 h at 4°C. The supernatants were collected and used for the assays. For the colorimetric assay, 50 μl reactions were set up containing 35 μl homogenate, 5 μl assay buffer (0.5 M sodium phosphate, 1 M sodium citrate,
Page 4 of 17(page number not for citation purposes)

pH 4), 5 μl taurocholate-oleic acid mixture (20 mg/ml oleic acid, 70 mg/ml sodium taurocholate), and 5 μl of a 5 mg/ml solution of 2-hexadecanoylamino-4-nitrophenyl-β-D-galactopyranoside (HNG; synthesized at the Mayo Clinic Chemistry Core facility). The reaction mixture was incubated for 16 h at 37°C. After incubation, 0.1 ml of stop solution (0.1 M glycine, 0.1 M NaOH, pH 10.5) was added, followed by 0.2 ml absolute ethanol. The reaction mixture was vortexed and centrifuged for 10 min at 20,000g. The absorbance of the supernatant was read at 410 nm. We have previously directly compared the results obtained in the assay to the more commonly used radioisotopic assay and found similar results in tissue homogenates from twitcher animals when compared with their wild-type littermates (data not shown).
Luxol-Fast blue (LFB)/periodic acid Schiff (PAS) staining
Paraffin-embedded sections were stained according to a standard protocol (29). Analysis was performed with light microscopy.
Immunohistochemistry
Paraffin serial sections (5 μm thick) were deparaffinized and rehydrated in xylene and a graded series of alcohol (100%, 100%, 95%, and 70%). Antigen retrieval was performed in double distilled water in a steam bath for 30 min. The sections were subsequently cooled to room temperature. The Dako (Carpinteria, CA) Autostainer was used with the Dako EnVision HRP system for staining with CL1475 antibody (1:500) diluted in Dako Antibody Diluent with background reducing components. Dako Liquid DAB Substrate-Chromogen system was used as the chromogen. The slides were counterstained with hematoxylin (Thermo-Shandon, Pittsburgh, PA) and subsequently dehydrated and coverslipped. Analysis was performed with light microscopy.
Determination of tissue psychosine level
Approximately 200 mg of mouse tissues (brain, kidney, or liver) was added with the internal standard lactosylsphingosine (2.5 μg total). Three milliliters of 1% formic acid in methanol (FA:MeOH) was added and homogenized with a Polytron Tissue Tearer (Brinkmann Instruments, Westbury, NY) in a 10 ml round-bottomed glass tube. The homogenate was allowed to stand at room temperature for 1 h. It was then centrifuged at 1800g for 15 min at 4°C, and the pellet was discarded. The supernatant was blown to dryness with nitrogen gas and resuspended in 1 ml of 78% methanol containing 0.1% formic acid. The material was sonicated in a water bath sonicator (Branson Ultrasonics, Danbury, CT) for 15 min, and then centrifuged again at 1800g for 15 min. The supernatant was removed by syringe and filtered with a 0.45 μm × 17 mm filter (Osmonics Cameo 17GP syringe filter, Glass/Polypro) before analysis on an API 365 LC/MS system (Applied Biosystems, Foster City, CA).
Page 5 of 17(page number not for citation purposes)

RESULTS
Peripherally administered recombinant GALC results in substantial improvements in failure to thrive, gait, and survival in the twitcher mouse model of GLD
Twitcher mice are an enzymatically authentic model of GLD (30, 31) carrying a G>A mutation in the GALC gene that results in a premature stop codon and complete deficiency of GALC activity. Clinical pathology of these animals includes a failure to thrive followed by progressive limb weakness and paralysis of the hind limbs by approximately PND 35. Demyelination in the central and peripheral nervous system can be detected by PND 20 accompanied by involuntary head tremor, and the animals ultimately die at about PND 40 (30–32). This model has been extensively used for studies of pathogenesis of GLD and for evaluating novel therapeutic approaches (26, 33–38).
Weekly i.p. injection of recombinant GALC showed a significant increase in life span from 40 to 47 days (Fig. 1). This increase is likely to be clinically very relevant given that the pathological changes in the twitcher mice are particularly aggressive and that changes in the life span of these animals due to therapeutic interventions can result in even greater improvements in human patients (36, 37, 43, 44). Importantly, the improvement in life span we observed was similar regardless of whether treatment was begun at PND 10 or PND 20 (after CNS and PNS demyelination is typically apparent) (Fig. 1, Mann-Whitney nonparametric analysis: PND 10, P=0.0022; PND 20, P=0.0097).
To follow up on these findings, we examined the influence of recombinant GALC administration on other pathologies characteristic of the twitcher mouse model. In these experiments, we increased the dosing frequency to every other day but maintained the same dose of GALC per injection. As shown in Fig. 2A, twitcher mice normally show a significant failure to thrive in early life when compared with their wild-type littermates. GALC-treated animals, however, gained weight at a rate essentially indistinguishable from the unaffected wild-type mice up until approximately PND 32, resulting in a 70% difference in weight between the treated and control twitcher mice at this age. At day 32, the weight of the GALC-treated animals began to decline precipitously at a rate similar to the saline-injected twitcher mice. The mechanism behind this phenomenon that occurs almost invariably at approximately PND 32 in both the treated and control twitcher mice is currently not clear but is obviously independent of the treatment regimen. Interestingly, the improvement in life span of the mice injected every other day with recombinant GALC (note moribund endpoints in Fig. 2, last data point) is essentially identical to that in the mice treated once per week (Fig. 1).
Twitcher mice normally begin to show significant gait abnormalities at approximately PND 35. As shown in Fig. 2B, this is characterized by an irregular dragging pattern due, at least in part, to hind limb paralysis. While not completely corrected, GALC-treated mice showed a substantial improvement in gait. Thus, GALC-treated twitcher animals showed a significant increase in life span, an almost complete attenuation of their early failure to thrive, and a noticeable gait improvement.
Page 6 of 17(page number not for citation purposes)

Biodistribution of peripherally administered GALC and reduction in the levels of psychosine in treated animals
Given these substantial early phenotypic improvements, we were interested in assessing the biodistribution of the recombinant enzyme and evaluating histopathology in these animals. Table 1 shows an analysis of GALC enzymatic activity in both treated and untreated twitcher tissues isolated from animals that had become moribund as compared with normal wild-type mice. As might be expected for a peripherally administered enzyme, the largest percent elevation in GALC enzymatic activity was observed in the liver. Albeit that the levels are low, we did detect a significant increase in GALC substrate cleavage in brain homogenates from treated animals (P=0.0311). To determine if this increase in enzyme levels was physiologically relevant we examined the amount of psychosine, a cytotoxic GALC substrate and the main biochemical marker in GLD, that accumulated in the brains of twitcher and control animals. Consistent with an increase in GALC activity in the brain, mass spectral analysis of psychosine levels showed a significant 18% decrease (P=0.0008) in psychosine accumulation in the brain at PND 29 in treated animals (Table 1).
GALC immunohistochemistry and histopathology studies reveal significant improvement in the pathology normally present in the twitcher mice following peripheral administration of recombinant GALC
The pathological hallmarks of GLD in the twitcher mouse, which are similar to those of human GLD, include demyelination associated with loss of oligodendrocytes and infiltration of multinucleated peripheral macrophages or “globoid cells” (31, 39, 40). To assess histopathological improvement, we repeated the study in another cohort of animals. At PND 29, mice were killed, perfused, and analyzed immunohistochemically with LFB/PAS staining, which stains for myelin and globoid cells, respectively, and with an antibody against GALC.
GALC staining was readily observable in tissues from wild-type animals, but no staining was observed in tissues from untreated twitcher animals (Fig. 3). Upon i.p. injection of GALC, the enzyme was detected in Schwann cells, hepatocytes, and kidney cuboidal cells in subcellular localizations that appeared similar to that of the endogenous GALC in the wild-type mice. Consistent with the small increase in GALC activity and the reduced psychosine levels we observed in the brain in treated animals, diffuse mild staining of GALC was readily observed in the white matter of cerebellum, where considerable pathology is normally apparent in this mouse model at this age (41, 42). LFB/PAS staining of the longitudinal sections of sciatic nerve showed significant improvements in myelination, and we observed less PAS-positive globoid cells (Fig. 4). Interestingly, however, the endoneurial edema was not obviously diminished. This may indicate pathology resistant to this treatment. Despite increases in enzymatic activity, increased enzyme levels and decreased psychosine accumulation in the brain, LFB/PAS staining of the cerebellum showed no observable improvement in myelination or apparent difference in the number of PAS-positive globoid cells in the treated mice (data not shown). While tempting to speculate, it is not clear whether it is this pathology ultimately contributes to the precipitous decline that occurs following day 32 in both the treated and control animals.
Page 7 of 17(page number not for citation purposes)

DISCUSSION
ERT has been successfully used for the treatment of lysosomal storage disorders with predominant peripheral symptoms. Little information concerning the effects of ERT on diseases with a predominant CNS component such as GLD is available. This is presumably due not only to the perceived difficulty in getting the active enzyme to the brain but also to the presumed need for it to reach the brain to achieve any clinical benefit. In this study, we found a perhaps surprising but nonetheless significant improvement in several major aspects of early pathology in the twitcher mouse model of GLD following peripheral ERT. Although we were not able to prevent the later precipitous decline occurring just before death, we did observe an increase in life span, an attenuation of the early failure to thrive, and an improvement in the gait of GALC-treated animals.
While it is likely that much of the clinical benefit we observed in the treated animals is due to peripheral improvements, we did observe a relatively small amount of enzyme in the brain and a resultant reduction in psychosine levels. Notably, at least two ERT studies for other LSDs have shown evidence of storage reduction in the brain following peripheral injection of other enzymes (24, 25). While no follow-up biochemical or histological analysis of the brain was performed in either of those studies to examine enzyme levels or activity to determine whether the enzyme itself reached the brain, it is tempting to speculate that small amounts of enzyme that effectively crossed the BBB may be the underlying mechanism in those studies as well.
The simplest explanation of how the enzyme reached the brain in the present study would be that twitcher mice have a compromised BBB. At least two previous studies have examined the BBB in these animals with differing results (45, 46). To examine this further, we i.v. injected Evans blue dye into similarly aged twitcher mice and compared the extent of extravasations in the brain to those in wild-type mice and in mice with a compromised BBB due to liver toxicity as a positive control. No substantial failure of the BBB was observed in the twitcher mice in this study as evidenced by a lack of extravasations (data not shown). While we cannot rule out subtle changes or transient permeability in the BBB, these data would suggest that GALC might get into the CNS by some other fashion. One intriguing possibility is that exogenous GALC might be carried into the CNS by peripheral macrophages. Previous work has shown that peripheral macrophages first appear in the cerebellar white matter at about PND 27 in twitcher mice (47) and that hematogenous cells can take up GALC through the mannose-6-phosphate receptor pathway (48). Given these results, it is possible that these cells might take up the recombinant GALC in the periphery before entering the CNS. Further studies will be necessary to determine whether this or other mechanisms are involved.
The most effective current treatment for these patients is a bone marrow transplant. Unfortunately, this treatment needs to be initiated very early for it to be effective and the procedure carries a relatively high mortality rate. Unless there is a family history of the disease, many patients with the infantile and most aggressive form of the disease will miss the window of opportunity for an effective transplant. We are particularly intrigued that the increase in life span we observed in the twitcher mice that had been given recombinant GALC was independent of whether the treatment started at PND 10 or PND 20, because by PND 20, signs of both peripheral and CNS demyelination are typically observed in this model. Collectively, our data
Page 8 of 17(page number not for citation purposes)

suggest that peripheral ERT is likely to be beneficial in patients with GLD and perhaps may even increase the effective therapeutic window for effective bone marrow transplantation.
ACKNOWLEDGMENTS We wish to acknowledge funding from the Mayo Foundation for Medical Education and Research and the National Institute of Neurological Disorders and Stroke (NS44230). REFERENCES 1. Suzuki, K., and Suzuki, Y. (1989) Galactosylceramide lipidosis: globoid cell leukodystrophy
(Krabbe disease). In The Metabolic Basis of Inherited Disease (Scriver, C. R., Beaudet, A. L., Sly, W. S., and Valle, D., eds) pp. 1699–1720, McGraw-Hill, New York
2. Wenger, D. A., Rafi, M. A., Luzi, P., Datto, J., and Costantino-Ceccarini, E. (2000) Krabbe disease: genetic aspects and progress toward therapy. Mol. Genet. Metab. 70, 1–9
3. Wenger, D. A., Suzuki, K., Suzuki, Y., and Suzuki, K. (2001) Galactosylceramide lipidosis. globoid cell leukodystrophy (Krabbe disease). In The Metabolic and Molecular Basis of Inherited Disease (Scriver, C. R., Beaudet, A. L., Sly, W. S., and Valle, D., eds) 3, 3669–3694, McGraw-Hill, New York
4. Wenger, D. A. (1997) Krabbe disease (globoid cell leukodystrophy). In The Molecular and Genetic Basis of Neurological Disease (Rosenberg, R. N., Prusiner, S., DiMauro, S., and Barchi, R. L., eds) pp. 421–431, Butterworth-Heinemann, Boston
5. Vanier, M., and Svennerholm, L. (1976) Chemical pathology of Krabbe disease: the occurrence of psychosine and other neutral sphingoglycolipids. Adv. Exp. Med. Biol. 68, 115–126
6. Miyatake, T., and Suzuki, K. (1972) Globoid cell leukodystrophy: additional deficiency of psychosine galactosidase. Biochem. Biophys. Res. Commun. 48, 539–543
7. Suzuki, K., and Suzuki, Y. (1970) Globoid cell leukodystrophy (Krabbe's disease): deficiency of galactocerebroside beta-galactosidase. Proc. Natl. Acad. Sci. USA 66, 302–309
8. Tohyama, J., Matsuda, J., and Suzuki, K. (2001) Psychosine is as potent an inducer of cell death as C6-ceramide in cultured fibroblasts and in MOCH-1 cells. Neurochem. Res. 26, 667–671
9. Tanaka, K., and Webster, H. D. (1993) Effects of psychosine (galactosylsphingosine) on the survival and the fine structure of cultured Schwann cells. J. Neuropathol. Exp. Neurol. 52, 490–498
10. Sugama, S., Eto, Y., Yamamoto, H., and Kim, S. U. (1991) Psychosine cytotoxicity toward rat C6 glioma cells and the protective effects of phorbol ester and dimethylsulfoxide: implications for therapy in Krabbe disease. Brain Dev. 13, 104–109
Page 9 of 17(page number not for citation purposes)

11. Sugama, S., Kim, S. U., Ida, H., and Eto, Y. (1990) Psychosine cytotoxicity in rat neural cell cultures and protection by phorbol ester and dimethyl sulfoxide. Pediatr. Res. 28, 473–476
12. Taniike, M., Mohri, I., Eguchi, N., Irikura, D., Urade, Y., Okada, S., and Suzuki, K. (1999) An apoptotic depletion of oligodendrocytes in the twitcher, a murine model of globoid cell leukodystrophy. J. Neuropathol. Exp. Neurol. 58, 644–653
13. Tanaka, K., Nagara, H., Kobayashi, T., and Goto, I. (1989) The twitcher mouse: accumulation of galactosylsphingosine and pathology of the central nervous system. Brain Res. 482, 347–350
14. Kolodny, E. H. (1996) Globoid leukodystrophy. In Handbook of Clinical Neurology (Moser, H. W., ed) 22, 187–210, Elsevier, Amsterdam
15. Shapiro, E. G., Lockman, L. A., and Kennedy, W. E. A. (1991) Bone marrow transplantation as treatment for globoid cell leukodystrophy. In Treatment of Genetic Diseases (Desnick, R. J., ed) 223–238, Churchill Livingstone, New York
16. Krivit, W., Shapiro, E. G., Peters, C., Wagner, J. E., Cornu, G., Kurtzberg, J., Wenger, D. A., Kolodny, E. H., Vanier, M. T., Loes, D. J., et al. (1998) Hematopoietic stem-cell transplantation in globoid-cell leukodystrophy. N. Engl. J. Med. 338, 1119–1126
17. Kaye, E. M. (1995) Therapeutic approaches to lysosomal storage diseases. Curr. Opin. Pediatr. 7, 650–654
18. Neufeld, E. F. (2004) Enzyme replacement therapy. In Lysosomal Disorders of the Brain (Platt, F. M., and Walkley, S. V., eds) 327–338, Oxford University Press
19. Desnick, R. J., and Schuchman, E. H. (2002) Enzyme replacement and enhancement therapies: lessons from lysosomal disorders. Nat. Rev. Genet. 3, 954–966
20. Bembi, B., Zanatta, M., Carrozzi, M., Baralle, F., Gornati, R., Berra, B., and Agosti, E. (1994) Enzyme replacement treatment in type 1 and type 3 Gaucher's disease. Lancet 344, 1679–1682
21. Cohen, I. J., Katz, K., Kornreich, L., Horev, G., Frish, A., and Zaizov, R. (1998) Low-dose high-frequency enzyme replacement therapy prevents fractures without complete suppression of painful bone crises in patients with severe juvenile onset type I Gaucher disease. Blood Cells Mol. Dis. 24, 296–302
22. Eng, C. M., Guffon, N., Wilcox, W. R., Germain, D. P., Lee, P., Waldek, S., Caplan, L., Linthorst, G. E., and Desnick, R. J. (2001) Safety and efficacy of recombinant human alpha-galactosidase A–replacement therapy in Fabry's disease. N. Engl. J. Med. 345, 9–16
23. Schiffmann, R., Kopp, J. B., Austin, H. A., III, Sabnis, S., Moore, D. F., Weibel, T., Balow, J. E., and Brady, R. O. (2001) Enzyme replacement therapy in Fabry disease: a randomized controlled trial. JAMA 285, 2743–2749
Page 10 of 17(page number not for citation purposes)

24. Dunder, U., Kaartinen, V., Valtonen, P., Vaananen, E., Kosma, V. M., Heisterkamp, N., Groffen, J., and Mononen, I. (2000) Enzyme replacement therapy in a mouse model of aspartylglycosaminuria. FASEB J. 14, 361–367
25. Roces, D. P., Lullmann-Rauch, R., Peng, J., Balducci, C., Andersson, C., Tollersrud, O., Fogh, J., Orlacchio, A., Beccari, T., Saftig, P., et al. (2004) Efficacy of enzyme replacement therapy in alpha-mannosidosis mice: a preclinical animal study. Hum. Mol. Genet. 13, 1979–1988
26. De Gasperi, R., Friedrich, V. L., Perez, G. M., Senturk, E., Wen, P. H., Kelley, K., Elder, G. A., and Gama Sosa, M. A. (2004) Transgenic rescue of Krabbe disease in the twitcher mouse. Gene Ther. 11, 1188–1194
27. Sakai, N., Inui, K., Tatsumi, N., Fukushima, H., Nishigaki, T., Taniike, M., Nishimoto, J., Tsukamoto, H., Yanagihara, I., Ozono, K., et al. (1996) Molecular cloning and expression of cDNA for murine galactocerebrosidase and mutation analysis of the twitcher mouse, a model of Krabbe's disease. J. Neurochem. 66, 1118–1124
28. Gal, A. E., Brady, R. O., Pentchev, P. G., Furbish, F. S., Suzuki, K., Tanaka, H., and Schneider, E. L. (1977) A practical chromogenic procedure for the diagnosis of Krabbe's disease. Clin. Chim. Acta 77, 53–59
29. Sheenan, D. C., and Hrapchak, B. B. (1980) Theory and Practice of Histology, Lipshaw, Detroit.
30. Kobayashi, T., Yamanaka, T., Jacobs, J. M., Teixeira, F., and Suzuki, K. (1980) The Twitcher mouse: an enzymatically authentic model of human globoid cell leukodystrophy (Krabbe disease). Brain Res. 202, 479–483
31. Duchen, L. W., Eicher, E. M., Jacobs, J. M., Scaravilli, F., and Teixeira, F. (1980) Hereditary leukodystrophy in the mouse: the new mutant twitcher. Brain 103, 695–710
32. Olmstead, C. E. (1987) Neurological and neurobehavioral development of the mutant 'twitcher' mouse. Behav. Brain Res. 25, 143–153
33. Matsuda, J., Vanier, M. T., Saito, Y., and Suzuki, K. (2001) Dramatic phenotypic improvement during pregnancy in a genetic leukodystrophy: estrogen appears to be a critical factor. Hum. Mol. Genet. 10, 2709–2715
34. Shen, J. S., Watabe, K., Ohashi, T., and Eto, Y. (2001) Intraventricular administration of recombinant adenovirus to neonatal twitcher mouse leads to clinicopathological improvements. Gene Ther. 8, 1081–1087
35. Matsumoto, A., Vanier, M. T., Oya, y., Kelly, D., Popko, B., Wenger, D. A., Suzuki, K, and Suzuki, K. (1997) Transgenic introduction of human galactosylceramidase into twitcher mouse: significant phenotype improvement with a minimal expression. Dev. Brain Dysfunct. 10, 142–154
Page 11 of 17(page number not for citation purposes)

36. Yeager, A. M., Brennan, S., Tiffany, C., Moser, H. W., and Santos, G. W. (1984) Prolonged survival and remyelination after hematopoietic cell transplantation in the twitcher mouse. Science 225, 1052–1054
37. Hoogerbrugge, P. M., Poorthuis, B. J., Romme, A. E., van de Kamp, J. J., Wagemaker, G., and van Bekkum, D. W. (1988) Effect of bone marrow transplantation on enzyme levels and clinical course in the neurologically affected twitcher mouse. J. Clin. Invest. 81, 1790–1794
38. Hoogerbrugge, P. M., Suzuki, K., Poorthuis, B. J., Kobayashi, T., Wagemaker, G., and van Bekkum, D. W. (1988) Donor-derived cells in the central nervous system of twitcher mice after bone marrow transplantation. Science 239, 1035–1038
39. Suzuki, K. (1983) The twitcher mouse. A model of human globoid cell leukodystrophy (krabbe's disease). Am. J. Pathol. 111, 394–397
40. Jacobs, J. M., Scaravilli, F., and De Aranda, F. T. (1982) The pathogenesis of globoid cell leukodystrophy in peripheral nerve of the mouse mutant twitcher. J. Neurol. Sci. 55, 285–304
41. Suzuki, K. (1995) The twitcher mouse: a model for Krabbe disease and for experimental therapies. Brain Pathol. 5, 249–258
42. Suzuki, K., and Taniike, M. (1995) Murine model of genetic demyelinating disease: the twitcher mouse. Microsc. Res. Tech. 32, 204–214
43. Suzuki, K., Hoogerbrugge, P. M., Poorthuis, B. J., and Bekkum, D. W. (1988) The twitcher mouse. Central nervous system pathology after bone marrow transplantation. Lab. Invest. 58, 302–309
44. Krivit, W. (2004) Allogeneic stem cell transplantation for the treatment of lysosomal and peroxisomal metabolic diseases. Springer Semin. Immunopathol. 26, 119–132
45. Kondo, A., Nakano, T., and Suzuki, K. (1987) Blood-brain barrier permeability to horseradish peroxidase in twitcher and cuprizone-intoxicated mice. Brain Res. 425, 186–190
46. Pedchenko, T. V., and LeVine, S. M. (1999) IL-6 deficiency causes enhanced pathology in Twitcher (globoid cell leukodystrophy) mice. Exp. Neurol. 158, 459–468
47. Wu, Y. P., Matsuda, J., Kubota, A., and Suzuki, K. (2000) Infiltration of hematogenous lineage cells into the demyelinating central nervous system of twitcher mice. J. Neuropathol. Exp. Neurol. 59, 628–639
48. Sly, W. S., Kaplan, A., Achord, D. T., Brot, F. E., and Bell, C. E. (1978) Receptor-mediated uptake of lysosomal enzymes. Prog. Clin. Biol. Res. 23, 547–551
Received February 16, 2004; accepted April 17, 2005.
Page 12 of 17(page number not for citation purposes)

Table 1 GALC ERT increases GALC substrate cleavage in homogenates from brain, kidney, and liver and reduces the brain psychosine level in the treated animalsa Twitcher (Saline) Twitcher (Galc) WT Brain GALC (% to WT) 0 ± 0.91 6.54 ± 1.79 100 ± 2.58 Kidney GALC (% to WT) 0 ± 0.68 16.05 ± 4.02 100 ± 11.19 Liver GALC (% to WT) 0 ± 10.32 634 ± 33.29 100 ± 16.09 Brain psychosine (ng/100 mg) 855 ± 23.43 705 ± 30.55 0 ± 0.68 aGALC substrate cleavage was measured similarly to that described previously (28). The values are presented as a percentage of that normally found in wild-type mice. For this assay, all tissues were taken from the same animals described in Figure 2 following sacrifice after the animals became moribund. For psychosine determinations, all comparisons were made at postnatal day 29 following an every other day dosing regimen (similar to Figures 3 and 4). Hemi-brains were homogenized in 1% formic acid in methanol, dried, resuspended in 78% methanol containing 0.1% formic acid, and analyzed on an API 365 LC/MS system (Applied Biosystems, Foster City, CA). Quantification of psychosine was calculated with reference to an internal standard, lactosylsphingosine, added before extraction. Numbers represent the mean ± SE from 3 mice.
Page 13 of 17(page number not for citation purposes)

Fig. 1
Figure 1. GALC enzyme replacement increases life span of twitcher mice. Recombinant mouse GALC was produced from stably transfected HEK 293 cells. Twitcher mice were injected intraperitoneally once per week at a concentration of 6 mg/kg in 0.9% saline beginning on postnatal day (PND) 10 or 20 as indicated. Both GALC-treated groups had a significantly longer life span than the control group (Mann-Whitney nonparametric analysis: PND 10 vs. control, P=0.0022; PND 20 vs. control, P=0.0097). Data points represent the day that the animal became moribund and had to be sacrificed.
Page 14 of 17(page number not for citation purposes)

Fig. 2
Figure 2. GALC enzyme replacement therapy significantly improves the early clinical phenotype apparent in twitcher mice. A) Analysis of body weight. Initially we were limited in the amount of recombinant enzyme available, and the experiment shown in Figure 1 is based on a weekly administration of GALC. All subsequent experiments were performed following administration of the recombinant enzyme every other day. Recombinant GALC was administered every other day at 6 mg/kg in 0.9% saline beginning at postnatal day (PND) 20. Values presented are the percent change in body weight that occurred in each animal relative to that animal’s weight at the beginning of the experiment (PND 20). Each point represents the mean ± SE from three mice. Twitcher mice normally show a significant failure to thrive in early life when compared with their wild-type littermates. GALC-treated animals, however, gained weight at a rate essentially indistinguishable from the unaffected wild-type mice until approximately PND 32, resulting in a 70% difference in weight between the treated and control twitcher mice at this age. B) Gait analysis performed at PND 40 showed marked improvement in GALC-treated animals as compared with saline-treated animals also analyzed at PND 40. Imprints from wild-type mice also completed at PND 40 are included as a comparison. Blue and red imprints are labeled the front and back paws, respectively.
Page 15 of 17(page number not for citation purposes)

Fig. 3
Figure 3. Immunohistochemical analysis of GALC in wild-type as well as both control and treated twitcher mice (×400 magnification). Twitcher mice were injected with GALC at 6 mg/kg every other day beginning at postnatal day (PND) 20. Saline-treated animals were injected with an equal volume of saline using the same dosing regimen. All mice were sacrificed by CO2 asphyxiation followed by perfusion with PBS at PND 29. Paraffin-embedded sections of kidney, liver, sciatic nerve, and brain were stained with an affinity purified GALC antibody (CL1475 1:500; brown color). Slides were counterstained with hematoxylin (blue color).
Page 16 of 17(page number not for citation purposes)

Fig. 4
Figure 4. GALC ERT results in increased levels of myelination and a decrease in globoid cells in the sciatic nerve in treated animals as determined by Luxol-Fast Blue (LFB)/periodic acid Schiff (PAS) staining (×400 magnification) (29). Twitcher mice were injected with GALC at 6 mg/kg every other day beginning at postnatal day (PND) 20. Saline-treated animals were injected with an equal volume of saline using the same dosing regimen. All mice were sacrificed by CO2 asphyxiation followed by perfusion with PBS at PND 29.
Page 17 of 17(page number not for citation purposes)