Gender Differences in Employed Job Search: Why Do Women Search
Why the differences?
-
Upload
truongtuong -
Category
Documents
-
view
218 -
download
1
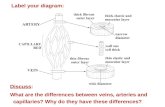
Transcript of Why the differences?

Laura M. Bruse Gehrig, MD Margaret M. Baker, MD Cordelia W. Carter, MD
Christy Hylden, MD Mary Lloyd Ireland, MD Anthony Johnson, MD
Elizabeth G. Matzkin, MD
The AAOS Women’s Health Issues Advisory Board (WHIAB) seeks to advocate, advance, and serve as a resource on sex and gender differences in musculoskeletal health.
Females suffer from injury/disease in different ways than males. Recognizing sex-related differences is critical to optimizing patient care.
www.aaos.org/women

Patellofemoral Pain Syndrome
Definition
Anterior or retropatellar knee pain with activities such as prolonged sitting, running, stair-climbing, squatting.10
General term with broad definition, often used when other knee pathology has been ruled out.
Common diagnosis, especially in young athletes.9
Sexual Dimorphism
Female athletes are more at risk than males of experiencing patellofemoral pathology.1,3,7,10
Proposed causes of this dimorphism include anatomic, hormonal, and neuromuscular factors:
Anatomic Differences in Q-Angles between the sexes is commonly referenced as a
possible reason for differences in knee pathology.7,8
Directional pull of quadriceps muscle may be impacted by Q-angle
However, there is no evidence that increasing Q-angle leads to increased risk of patellofemoral pain or other knee issues
There are sex-specific differences in distal femoral shape, such as the trochlear groove, that may contribute to mal-tracking and pain.6
Hormonal Increased laxity of joints may put more stress on the knee, leading to pain.8
Neuromuscular Hip muscle strengthening has been shown to improve knee pain in females.
Hip kinematic studies show females tend towards more internal rotation of the femur and greater hip adduction with running.2,5,8
During a squat, those with patellofemoral pain also tend to have more femoral internal rotation.
Knee kinematic studies have shown sexual dimorphism in muscle activation of both the kicking and the supporting lower extremities during a soccer kick.4
Treatment
Mainstay of treatment remains physical therapy, with hip strengthening becoming a bigger focus.2,5,7,9
Sometimes a role is found for surgery, but this is usually associated with more specific diagnoses such as patellar instability.
Prevalence and Incidence
The prevalence of Achilles tendon rupture is 6-37/ 100,0001.
Acute Achilles tendon rupture is more common in men.
The incidence of Achilles tendon rupture has increased over all age groups over a 33 year period in both young male persons (most common) and elderly females.2
The male: female ratio of 2.81:1.3
Etiology and Location
Nonacute pathology for rupture is more common in women, with the age in women slightly higher.
Whether degeneration or not, the requirement of eccentric contraction of sufficient force is still required.4
The most common location is 3-6 cm above the calcaneal insertion.
Sexual Dimorphism
Sex may affect outcomes after acute Achilles tendon rupture. Overall, male patients have better outcomes at 1 year compared to female patients, regardless of treatment method.5
A study in rats found that female sex hormones had an inhibitory effect on muscle fiber diameter. This proposed a possible protection to risk of rupture in women.6
Stiffness of tissue and lever arm length affects increase risk of injury in men. Men have higher joint stiffness and higher lever arm. This increases the strain on the tissues when stretched for a given change in joint angle.7
Moderate evidence that decreased tendon fibril size also increases the risk in women.
Limited evidence was found for other modifiable factors such as increased body weight, oral corticosteroid use.8
One important non-modifiable risk factor for women is increasing age.
Future
More studies are needed to further identify and determine the racial differences and what preventative measures might prevent Achilles tendon rupture acutely in young males and elderly females.
References: (1) Arendt EA. Dimorphism and patellofemoral disorders. Orthop Clin North Am. 2006 Oct;37(4):593-9. (2) Arendt E. Hip-strengthening exercises before functional exercises reduced pain in women with patellofemoral pain syndrome. J Bone Joint Surg Am. 2012 May 16;94(10):940. (3) Arendt EA. Musculoskeletal injuries of the knee: are females at greater risk? Minn Med. 2007 Jun;90(6):38-40. (4) Brophy RH, et al. Differences Between Sexes in Lower Extremity Alignment and Muscle Activation During Soccer Kick. J Bone Joint Surg Am, 2010 Sep 01;92(11):2050-2058. (5) Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Lattermann C, Uhl TL. Hip Strengthening Prior to Functional Exer-cises Reduces Pain Sooner Than Quadriceps Strengthening in Females with Patellofemoral Pain Syndrome: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2011 Aug;41(8):560-70. (6) Everhart JS. Creation of a simple distal femur morphology classification system. J Orthoop Res. 2015 Nov 17. (7) Gorman McNerney ML, Arendy EA. An-terior knee pain in the active and athletic adolescent. Curr Sports Med Rep. 2013 Nov-Dec;12(6):404-10. (8) Prins M, van der Wurff P. Females with patellofemoral pain syn-drome have weak hip muscles: A systematic review.The Australian J of Physio, 2009 Feb;vol55:9-15. (9) Rixe JA, et al. A review of the management of patellofemoral pain syndrome. Phys Sportsmed. 2013 Sep;41(3):19-28. (10) Witvrouw E, et al. Clinical classification of ptellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc, 2005 13:122-130.
Achilles Tendon Rupture
References: (1) Predictors of primary Achilles tendon ruptures. Claessen FM, de Vos RJ, Reijman M, Meuffels DE. Sports Med. 2014 Sep;44(9):1241-59. doi: 10.1007/s40279-014-0200-z. Review. PMID: 24929701 [PubMed - indexed for MEDLINE]. (2) Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Lantto I, Heikkinen J, Flinkkilä T, Ohtonen P, Leppilahti J.Scand J Med Sci Sports. 2015 Feb;25(1):e133-8. doi: 10.1111/sms.12253. Epub 2014 May 23. PMID: 24862178 [PubMed - indexed for MEDLINE] (3) Achilles tendon rupture in women. Vosseller JT, Ellis SJ, Levine DS, Kennedy JG, Elliott AJ, Deland JT, Roberts MM, O'Malley MJ. Foot Ankle Int. 2013 Jan;34(1):49-53. doi: 10.1177/1071100712460223. PMID: 23386761 [PubMed - indexed for MEDLINE] (4) Achilles tendon rupture in women. Vosseller JT, Ellis SJ, Levine DS, Kenne-dy JG, Elliott AJ, Deland JT, Roberts MM, O'Malley MJ. Foot Ankle Int. 2013 Jan;34(1):49-53. doi: 10.1177/1071100712460223. PMID: 23386761 [PubMed - indexed for MED-LINE]5. AAOS Now August 2014 Issue). (6) Achilles tendon rupture in women. Vosseller JT, Ellis SJ, Levine DS, Kennedy JG, Elliott AJ, Deland JT, Roberts MM, O'Malley MJ. Foot Ankle Int. 2013 Jan;34(1):49-53. doi: 10.1177/1071100712460223. PMID: 23386761 [PubMed - indexed for MEDLINE] (7) Gender differences in both active and passive parts of the plantar flexors series elastic component stiffness and geometrical parameters of the muscle-tendon complex. Fouré A, Cornu C, McNair PJ, Nordez A. J Orthop Res. 2012 May;30(5):707-12. doi: 10.1002/jor.21584. Epub 2011 Oct 27. PMID: 22034230 [PubMed - indexed for MEDLINE] Free Article (8) Predictors of primary Achilles ten-don ruptures. Claessen FM, de Vos RJ, Reijman M, Meuffels DE. Sports Med. 2014 Sep;44(9):1241-59. doi: 10.1007/s40279-014-0200-z. Review. PMID: 24929701 [PubMed - indexed for MEDLINE]

ACL Injuries and Management
Epidemiology
Highest Female:Male rate differences: Basketball and Team Handball1
Prevention and post ACLR
rehab programs: No sex differences2
Mechanisms of Injury: No
sex difference in noncontact mechanisms; difference in weight bearing pivot shift3
Intrinsic Risk Factors
Hormonal / Joint Laxity: Data are insufficient to make any conclusive statement regarding menstrual cycle of knee laxity and on the rate of ACL injury in females4
The COL5A1 Gene Is Associated With Increased Risk of ACL Tears in Females:5 Gene that encodes alpha1 chain of type 1 collagen ACL tears type 5 collagen Achilles tendon injuries. Hypermobility (excessive joint laxity) associated with increased incidents of musculoskeletal injury6
Notch Size: No Sex Differences; Smaller Notch and Ratios = Greater ACL Tear Rate
Tibial Plateau Geometry:
No Sex Differences7,8
Tibial Plateau Risk Model Medial and Lateral Slope and Medial Tibial Depth
Odds Ratio (Hashemi/Gibson): 1 mm ↓ MTP and 1° ↑ Posterior Slope: Females: 3.58 / Males: 4.18
Extrinsic Risk Factors
Kinematics: Valgus Collapse and increased knee abduction moment9
205 female athletes, 9 ACL tears: Greater abduction moment predicted ACL injury p<.001
Biomechanical/Neuromuscular:10 Proximal Control
Mini Squat, Normal Subjects:
Surgical Management
Graft Choice: No sex difference; do not change based on cosmetic concerns
Pearls: For the smaller, shorter patient: Adjust femoral fixation; Use suspension or bioabsorbable devices; Avoid Iatrogenic ITB Syndrome
Outcomes
Graft Failure/Future Surgeries:11 Meta Analysis 13 studies – no sex differences in Graft Failure (8); Contralateral ACL Rate (3); Laxity Post OP (6)
Return to Play/Activity Level: Moon Study12
100 Soccer Athletes (55) Male (45) Female
Average age 24.2 years
7 year follow up 30% still playing
Females more likely to have ACL Surgery (%20 vs %5 p=.03)
Older athletes and females less likely to RTP p=0.37 2 Year F/U Females Lower Activity (OR=0.60)13
Development of Osteoarthritis:
Longer term Registry follow up needed14
Swedish ACL Registry:15
84 female soccer players ACL injuries
12 year follow up
42% Symptomatic Knee OA
75% Symptoms affected QOL No difference if underwent ACLR compared to those who had not
Male Female
Pelvis Level Contralateral Drop
Hip No Rotation Internal Rotation and Adduction
Knee 0o Varus/Valgus Valgus
Tibia Neutral External Rotation
Foot Flat Pronation
Back Flat Lordotic
Pelvis Neutral Anterior Tilt
References: (1) Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, Georgoulis T, Hewett T, Johnson4 R, Krosshaug T, Mandelbaum B, Micheli L, Myklebust G, Roos E, Roos H, Schamasch P, Shultz S, Werner S, Wojtys E, Engebretsen L. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts state-ment. Br J Sports Med 2008;42:394-412; (2) Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE Jr, Hannafin JA, Hewett TE, Hus-ton LJ, Ireland ML,Johnson RJ, Lephart S, Mandelbaum BR, Mann BJ, Marks PH, Marshall SW, Myklebust G, Noyes FR, Powers C, Shields C Jr, Shultz SJ, Silvers H, Slauterbeck J, Taylor DC, Teitz CC, Wojtys EM, Yu B. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006 Sep;34(9):1512-32. (3) Ireland M. Anterior Cruciate Ligament Injury in Female Athletes: Epidemiology. JournalofAthleticTraining1999;34(2):150-154 (4) Sutton K, Bullock J. Ante-rior Cruciate Ligament Rupture: Differences Between Males and Females. The Journal of the American Academy of Orthopaedic Surgeons 01/2013; 21(1):41-50. (5) Posthumus M, September A, O’Cuinneagain D, Merwe W, Schwellnus M, Collins M. The COL5A1 Gene Is Associated With Increased Risk of Anterior Cruciate Ligament Ruptures in Female Partici-pants. Am J Sports Med NOV;37(11) 2234-40 (6) Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg. 2011 Aug;19(8):463-71. (7) Gibson G, Hashemi J, Mansouri H, Slauterbeck J, Beynnon V. On the Horizon from ORS. Journal of the American Academy of Orthopaedic Surgeons. 2010 OCT 18(10):638-641 (8) Hashemi J, Chandrashekar N, Mansouri H, et al: Shallow medial tibial plateau and steep medial and lateral tibial slopes: New risk factors for anterior cruciate ligament injuries. Am J Sports Med 2013;38(1):54-62 (9) Hewett TE, Myer GD, Ford KR, et al: Biomechanical measures of neuromuscular control and valgus loading of the knee predict Anterior Cruciate Ligament injury risk in female athletes: A prospective study. AM J Sports Med 2005;33(4):492-501. (10) Ireland M, Durbin T, Bolgla L. Gender Differ-ences in Core Strength and Lower Extremity Function During the Single-Leg Squat test. IN: ACL Injuries in the Female Athlete: Causes, Impacts, and Conditioning Programs. Noyes FR, Barber-Westin SD Berlin Heidelberg, 2012.:203-219 (11) Ryan J, Magnussen R, Cox C, Hurbanek J, Flanigan D, Kaeding C. ACLR: Do Outcomes Differ by Sex? Journal of Bone and Joint Surgery 2014;96:507 (12) Brophy R, Schmitz L, Wright R, Dunn W, Parker R, Andrish J, McCarty E, Spindler K. Return to Play and future ACL Injury Risk After ACLR in Soccer Athletes from the Multicenter Orthopaedic Outcomes Network (MOON) Group. The AM J Sports Med NOV 2012;40(11) 2517-2522 (13) Dunn W, Spindler K. Predictors of Activity Level 2 Years After ACLR. The American Journal of Sports Medicine 2010 ;38(10):2040-2050. (14) O’Connor M. Sex Differences in Osteoarthritis of the Hip an Knee. Journal of the American Academy of Orthopaedic Surgeons. 2007 15:22-25 (15) Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in fe-male soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 2004;50:3145-3152.

Shoulder Instability and Ligamentous Laxity
Is There Sex Difference in Shoulder Instability?
NIH Revitalization Act of 1993: Requires all NIH-supported human subjects research include and analyze the impact on women & minorities
Multi-Directional Shoulder Instability (MDI) is thought to be more common in females:1 Females comprise <50% of the population reported in clinical series on MDI2
Traumatic Shoulder Dislocation data mixed results: Question whether females have inferior outcomes with arthroscopic Bankart stabilization3
Epidemiology of Shoulder Dislocation
Incidence in Shoulder Dislocations
Overall: 0.08-0.24/1000 person-years4
Military: 1.69/1000 person-years (Cadets: 4.35/1000 person-years5)
Male: 1.82 vs. Female 0.90
Males 2.6 times more likely to present to emergency department for shoulder dislocation relative to males6
White 1.78 > “Other” 1.59 > Black 1.41
Inverse relationship with age vs. direct relationship with activity level
Subluxation events >> dislocation events
Return to Play
Approximately 1:4 athletes will return and complete season after in-season anterior shoulder instability
Subluxation events 5.3x more likely to return to sport vs. dislocation events
Did not look at sex based differences
Sex-Based Differences in Anatomy
Glenoid Morphology Associated with Instability
Tall and Thin less stable than Short and Wide7
Increasing coraco-humeral distance proportional to instability risk
Glenoid Dimensions Vary by Race and Sex8
Females have significantly small glenoids (height and width) vs. males
Females have significantly higher inclination angles vs. males
Glenoid retroversion increased for Whites vs. Blacks
No significant difference for sex
Sex Differences in Range of Motion
Variations on study population size, design, and measuring techniques contribute to confusion and variation on body of knowledge
Females have greater ROM vs. Males in all planes of motion9
True in PROM & AROM (PROM > AROM)
Race, Occupation, Sports Participation no effect on shoulder ROM
Motions with greatest difference was abduction & external rotation
Dominant vs. Non-Dominant extremity range of motion
Sufficient magnitude to call into question of contra-lateral limb as internal reference point
Questions of statistical vs. clinical significance
Especially for abduction-external rotation for the dominant shoulder in athletic populations
Sex Differences in Ligamentous Laxity
Prevalence of generalized joint laxity between 8.8% and 64.6%10
45% of girls and 29% of boys have hypermobile fingers11
Suggestion of a association between hypermobility in girls and physical activity and body mass index
Association extends after puberty
No associations were seen in boys
Recurrent Shoulder Instability
Variety of injury and patient related factors may contribute to risk of recurrent shoulder instability12
Majority of literature support the risk is highest in young male athletic patients
Survival Analysis: Mean time of development of recurrent instability: 13.3 mos. Risk of recurrence peaks at 24 months
Uni-variate Analysis: Age, sex, GLL, sport & level of participation, return to contact sports all contributing factors
Multi-variate Analysis: Only male sex and young age group independently predictive of recurrent instability. Risk of recurrent instability lower for females of all age groups vs. age matched males
Sex Bias in Scoring Instruments
Overall health assessment + disease & site specific outcomes measures necessary
Instruments also need to measure patients’ perception of health status13
Instrument Bias
Outcomes may vary due to factors other than shoulder pain, impairment, or disability
Effect of demographics in scoring instruments TJA14
Evaluation of Constant-Murely, UCLA, ASES, SPADI, Oxford15
Significantly higher total normalized scores for men
Constant-Murely most susceptible to gender bias, especially on the strength subscale
Men scored 8.3 points higher than women (out of 25)
UCLA susceptible to gender bias for range of motion
Oxford susceptible to gender bias for pain subscale
Hand dominance had no significant effect (Role of Confirmation bias?)
Conclusions
Based on currently available literature, females seem to have lower rates of traumatic instability and recurrent instability
Females have higher rates of generalized ligamentous laxity
Few studies methodologically based to look for sex-based differences in shoulder instability
Few studies sufficiently powered to look for sex-based differences in shoulder instability
Gender bias in current outcomes measures identified
Role of confirmation bias unknown
References: (1) Wolf JM. JAAOS 23(6):339-347, 2015. (2) Gartsman GM. Arthroscopy 17(3):236-243, 2001. (3) Kaipel M. Orthopedics 33(3), 2010. (4) Owens BD. JBJS 91A(4):791-796, 2009. (5) Owens BD. AJSM 35(7): 1168-1173, 2007. (6) Zaccilli. JBJS 92A(3): 542-549, 2010. (7) Ow-ens BD. AJSM 42(11):2591-2596, 2014. (8) Churchill RS. JSES 10:327-332, 2001. (9) Barnes CJ. JSES 10:242-246, 2001. (10) Vougiouka O, Eur J Pediatr 2000;159:628, 2000; Lamari NM, Sao Paulo Med J 2005;123: 119–23, 2005. (11) Clinch J, Arthritis & Rheumatism 63(9):2819-2827, 2011. (12) Robinson CM. JBSA-A 88(11): 2326-2336, 2006. (13) Beaton DE. JBJS 78A(6):882-890, 1996. (14) Brinkler MR. Arthroplasty 11(7):820-830, 1996 & JBJS 79A(6):858-865, 1997. (15) Brinker MR. JSES 11:463-469, 2002.

Concussion
Overview
Concussion: a complex pathophysiological process affecting the brain, induced by biomechanical forces.1
Incidence in US increasing. Approx. 1.6 - 3.8 million concussions each year.2
5 percent of high school athletes will sustain a concussion each year.
Why look at sex?
Recent literature suggests a sex-related difference
Several studies indicate that in sports like soccer and basketball, females report more concussions than males.3,4,5,6
Female athletes may sustain more severe concussions with greater cognitive deficits and a longer recovery period.7,8,9
Why the differences? Biomechanical differences: Women have less head-
neck mass, resulting in greater reactive forces and 50% more acceleration during head trauma.10,11
Hormonal differences: Several studies have looked at adverse effects of estrogen on the brain after mTBI (mild traumatic brain injury).12
Patients with high levels of progesterone had worse outcomes after a mTBI.
Conclusions
Literature suggests potential sex differences, but there is conflicting data.13,14
The disparity can be attributed to:
Different populations
Reporting bias (retrospective studies)
Male athletes may be more likely not to report a concussion15
Team physicians should have a high index of suspicion for concussion with any head trauma sustained, regardless of sex.
Further research on concussions to determine the differences in incidence, symptom presentation and return to play criteria in men and women is still necessary.
Table 1. Studies that found a sex-related difference in concussion incidence
Primary Author
Year of Publication
Study Design Patients studied Evaluation tools Findings
Marar 2012 Descriptive
epidemiologic 1,936 high school
athletes Reported concussions
Females sustained twice as many concussions than males in soccer, females
sustained 30% more concussions in volleyball
Lincoln 2011 Descriptive
epidemiologic 158,430 high school
athletes Electronic medical
record keeping Females had double the risk of concussions
than male athletes
Gessel 2007 Descriptive
epidemiologic 100 high schools, 180
colleges
Reported concussions, electronic medical
record keeping
In high school sports played by both sexes, females sustained a higher rate of
concussions
Covassin 2003 Cohort study 882 collegiate
athletes reporting a concussion
NCAA Injury Surveillance System
Female basketball players had an increased risk for concussion. Females sustained a
higher percentage of concussions than male athletes in games
References: 1) McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, et al. Consensus statement on concussion in sport: the 4th Inter-
national Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 2013;47(5):250-8. 2) Thurman DJ, Branche CM, Sniezek JE. The epidemiology of sports-related traumatic brain injuries in the United States: recent develop-
ments. J Head Trauma Rehabil 1998;13(2):1-8. 3) Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train
2007;42(4):495-503. 4) Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J
Sports Med 2012;40(4):747-55. 5) Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-
year study. Am J Sports Med 2011;39(5):958-63. 6) Covassin T, Swanik CB, Sachs ML. Sex Differences and the Incidence of Concussions Among Collegiate Athletes. J Athl Train 2003;38(3):238-
44. 7) Broshek DK, Kaushik T, Freeman JR, Erlanger D, Webbe F, Barth JT. Sex differences in outcome following sports-related concussion. J Neuro-
surg 2005;102(5):856-63. 8) Colvin AC, Mullen J, Lovell MR, West RV, Collins MW, Groh M. The role of concussion history and gender in recovery from soccer-related
concussion. Am J Sports Med 2009;37(9):1699-704. 9) Preiss-Farzanegan SJ, Chapman B, Wong TM, Wu J, Bazarian JJ. The relationship between gender and postconcussion symptoms after sport
-related mild traumatic brain injury. PM R 2009;1(3):245-53. 10) Mansell J, Tierney RT, Sitler MR, Swanik KA, Stearne D. Resistance training and head-neck segment dynamic stabilization in male and fe-
male collegiate soccer players. J Athl Train 2005;40(4):310-9. 11) Tierney RT, Sitler MR, Swanik CB, Swanik KA, Higgins M, Torg J. Gender differences in head-neck segment dynamic stabilization during head
acceleration. Med Sci Sports Exerc 2005;37(2):272-9. 12) Wunderle K, Hoeger KM, Wasserman E, Bazarian JJ. Menstrual phase as predictor of outcome after mild traumatic brain injury in women. J
Head Trauma Rehabil 2014;29(5):E1-8. 13) Covassin T, Swanik CB, Sachs M, Kendrick Z, Schatz P, Zillmer E, et al. Sex differences in baseline neuropsychological function and concus-
sion symptoms of collegiate athletes. Br J Sports Med 2006;40(11):923-7; discussion 7. 14) Zuckerman SL, Solomon GS, Forbes JA, Haase RF, Sills AK, Lovell MR. Response to acute concussive injury in soccer players: is gender a
modifying factor? J Neurosurg Pediatr 2012;10(6):504-10. 15) Granito V CJ. Psychological response to athletic injury: Sex Differences. J Sport Behav 2002;25:243-59.

Stress Fracture Risk in Athletes Definition
Stress fractures are overuse injuries that occur with submaximal repetitive impact,
usually in weight-bearing bones. Stress fractures are common and may represent up to 10% of all sports injuries. Stress fractures can develop when muscle fatigue does not allow normal dissipation of energy at impact, causing excess forces on bone. Typically, bone is able to remodel and adapt to gradual increasing loads. If the repetitive load is increased more rapidly than bone is capable of responding, areas of bony resorption may lead to micro-damage. If overuse continues without interval
healing, a stress fracture occurs. In addition, if bone is not normal (low bone mineral density or osteopenia is present) stress fractures can occur at a lower threshold.
Incidence Female athletes, dancers, and military recruits are at increased risk for developing stress fractures. Compared to their male counterparts, females’ risk for stress fracture may be increased by as much as 1.5-12 times1.
Multifactorial Etiology
Stress fractures can occur in normal bone that is subject to increased repetitive loading without adequate time for repair and remodeling.
Change in Training /Change in Shoes: An increase in the time or distance of training, or change in running training (running on hard surfaces >2/3 of the time), increases occurrences of stress fractures.
Biomechanical Factors: Female pelvi are typically wider, with increased valgus at the femoral neck and knees.
Estrogen: When females develop amenorrhea or oligomenorrhea, decreased estrogen leads to decreased bone mass, predisposing stress fractures.
Disordered Eating: Females involved in appearance sports/activities that are judged subjectively (gymnasts, dancers, cheerleaders, figure skaters) have a high incidence of disordered eating.
Energy Deficit: Endurance runners and triathletes may strictly limit caloric and nutritional intake, leading to a relative energy deficit.
The interrelationship of disordered eating/energy deficit plus menstrual abnormalities plus bone loss is called the Female Athlete Triad. The Triad is a major risk factor for stress fractures, including recurrent and non–healing stress fractures2.
Clinical Presentation History: Runners account for the majority of stress fracture cases,
presenting with a sudden increase in training distance, intensity, duration, speed, a change in running surface, or change in shoe wear with weeks to months of pain described as a deep ache. It is not associated with night or rest pain. A unicortical incomplete stress fracture may become complete if the patient tries to “run through the pain.”
This scenario is often seen with stress fractures of the anterior tibia, tarsal navicular, base of the fifth metatarsal, and on the superior tension side of the femoral neck.
Taking a careful history of any training change as above, as well as a thorough history of menstrual and nutritional status is critical. Females with disordered eating may not be particularly forthcoming about these behaviors, so gaining the confidence of the athlete along with her parents, coaches and trainers can be helpful.
Physical Exam: Examination should include stance, gait, and mechanical bony alignment. The “Hop Test” may reproduce pain at the stress fracture site. Point tenderness and local swelling and/or periosteal thickening may be palpable. Bone percussion may reproduce pain at the fracture site. Height, weight, and BMI should be documented. Low BMI has been correlated with low bone mineral density and relative caloric deficit3.
Labs: Standard work-up should include a serum vitamin D level. Frequently, athletes in the northern hemisphere do not get adequate UV exposure to produce endogenous vitamin D, and are often nutritionally deficient. More detailed lab analysis may be required to workup endocrine abnormalities in athletes with amenorrhea/oligomenorrhea.
Imaging Radiographs: Plain radiographs
should be obtained, but are frequently negative especially in the first few weeks after stress fracture. After 3 or more weeks, faint endosteal bone formation may be present. A lucent line is relatively uncommon, but is of concern especially in the anterior tibial cortex where it may be a harbinger of impending complete fracture.
Nuclear Medicine: Technetium-99 triple phase bone scan is very sensitive for early detection of stress fracture. All 3 phases of the bone scan will show increased uptake. In pediatric patients with open physes, bone scan may not be as helpful since the physes will also show areas of increased uptake.
CT: For potential stress fractures of the tarsal navicular, calcaneus, or femoral neck, CT can be the most helpful imaging modality. CT can delineate stress fractures which have gone on to delayed or nonunion.
MRI: MRI is useful for early detection of stress fractures at all sites, with the added benefit of no ionizing radiation. A very early stress fracture may be noted as a finite area of bony edema.
DXA: Indicated for athletes who have sustained multiple stress fractures, and in those with a history of amenorrhea for 6 or more months, and for athletes with disordered eating4.
Treatment
Rest: The mainstay of treatment is allowing rest for adequate bony healing, then gradually resume activity after pain has abated.
Rehabilitation: Muscle strengthening and maintenance of aerobic conditioning is an important adjunct. Cross-training to a nonimpact activity such as swimming, biking, or rowing may be helpful.
Correct any caloric or nutritional deficit, especially with associated menstrual abnormalities. Oral contraceptives are not a first line treatment in cases of amenorrhea, since OCPs do not correct the underlying nutritional/caloric deficit. Most stress fractures will heal with standard nonoperative treatment. Due to some data on impaired fracture healing, avoiding NSAIDs is prudent.
Surgical Treatment: May be indicated for stress fractures including the superior femoral neck, tarsal navicular, base of the fifth metatarsal, and the anterior tibia.
In elite or professional athletes, semi-elective early surgical intervention for these problem fractures may be considered rather than lengthier nonoperative treatment regimens. For patients with Female Athlete Triad, a multidisciplinary team approach is critically important. This should include a dietitian, psychologist, athletic trainer, primary care physician, trainer, coaches, and family.
References: (1) Callahan, LR. “Stress Fractures in Women”, in “The Athletic Woman”, Clinics in Sports Medicine, volume 19 (2), 2000. (2) Matzkin, E et al. “Female Athlete Triad: Past, Present, and Future”, JAAOS, 2015; 23: 424–432. (3) McBryde, AM and Barfield WR. “Stress fractures” in “The Female Athlete”, Saunders, Philadelphia, pp. 299–316, 2002. (4) Hame, SL and Bader, DA. “The Female Athlete Triad and Stress Fractures” in “Women’s Sports Injuries”, AAOS Monograph no. 50, Rosemont, IL, 2013, 65–76.
Female Athletes at Risk:
Runners
Triathletes
Gymnasts
Dancers
Cheerleaders
Basketball players
Rowers
Military recruits
Common Stress Fractures and Associated Activity:
Tibia, fibula, medial malleolus, femoral neck, pelvis: Running
Metatarsals: Dancing, ballet, running, marching
Pars intra-articularis: Gymnastics, dancing
Tarsal navicular, calcaneus: Basketball
Ribs: Rowing, golf
Humerus: Overhead throwing sports
Bilateral tibial stress fractures on Tc-99 bone scan MRI of femoral neck stress fracture

Femoroacetabular Impingement Overview
Femoroacetabular Impingement (FAI) results from abnormal physical contact between the acetabulum and proximal femur and commonly presents as activity-related groin pain in adolescents and young adults
On physical examination, patients with symptomatic FAI demonstrate:
Decreased passive hip flexion and internal rotation
Pain with hip flexion, internal rotation and adduction
FAI is typically characterized by the location of the predominant morphologic abnormality. There are three major types of FAI:
Cam impingement (femoral-sided): Aspherical extension of the articular surface at the anterosuperior head-neck junction of the proximal femur results in loss of the normal offset. Direct contact between this “bump” and the anterosuperior acetabulum during repeated motion results in cartilage injury and labral tearing (Figure 1)
Pincer impingement (acetabular-sided): Overcoverage of the femoral head results from acetabular retroversion and/or coxa profunda; physiologic hip motion may over time result in repetitive contact between the acetabulum and proximal femur and ultimately in chondrolabral injury
Mixed impingement: Aspects of both cam and pincer lesions
Radiographic Incidence of FAI Traditionally, cam-type impingement was associated
with young athletic males and pincer impingement with females in their fourth decade of life. However, recent population-based studies have shown that:
Cam lesions are more common in males than females2,4
In one study, 19.6% of males and only 5.2% of females had radiographic cam deformity2
Radiographic pincer lesions are common in both males and females, occurring in more than 15% of all patients
Bilateral findings of FAI are more common in males than females4
Cam: M 24.7% versus F 6.3%
Pincer: M 21.7% versus F 9.7%
Clinical Presentation At time of presentation, males and
females report similar symptomatology, however, symptomatic males with cam-type impingement have higher alpha angles than symptomatic females
(Figure 2)6,7
Beaulé et al, J Orthop Res 20056
3D CT
M 73.3° versus F 58.7°
Hetsroni et al, Arthroscopy 20137
CT
M 63.6° versus F 47.8°
Symptomatic females have increased femoral and acetabular anteversion than symptomatic males
Hetsroni et al, Arthroscopy 20137
Acetabular version (M 13.9° versus F 17.3° P < .001)
Femoral anteversion (M12.1° versus F 14.4° P = .05)
Males are more likely than females to have symptomatic bilateral FAI requiring surgery
Klingenstein et al, AJSM 20138
Odds Ratio M:F = 1.7 (95% CI 1.16-2.54)
Females have lower preoperative hip function scores than males
Malviya et al, JBJS-Br 20129
Females with significantly lower modified Harris Hip Score
Females with significantly lower Hip Outcome Score
ADLs, sports domains
Treatment and Outcomes There is conflicting evidence for whether males or
females are more likely to have surgery for FAI:
Ng et al, AJSM 201010
FAI surgical patients: 62.7% M versus 37.3% F
Clohisy et al, Clin Orthop 201012
FAI surgical patients: 45% M versus 55% F
There are no studies to date describing and/or examining sex-based surgical techniques
Females demonstrate equal or greater improvements in clinical outcomes scores (e.g., modified HHS) 1 year following surgery, although their scores remain lower than those of males.
References: (1) Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clinical orthopaedics and related research. Dec 2003(417):112-120. (2) Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoar-thritis: a population-based survey. The Journal of bone and joint surgery. American volume. May 2010;92(5):1162-1169. (3) Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. Aug 2007;15(8):1041-1047. (4) Laborie LB, Leh-mann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. Aug 2011;260(2):494-502. (5) Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clinical orthopaedics and related research. Feb 2010;468(2):555-564. (6) Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. Nov 2005;23(6):1286-1292. (7) Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. Jan 2013;29(1):54-63. (8) Klingenstein GG, Zbeda RM, Bedi A, Magennis E, Kelly BT. Prevalence and preoperative demographic and radiographic predictors of bilateral femoroacetabular impingement. The American journal of sports medicine. Apr 2013;41(4):762-768. (9) Malviya A, Stafford GH, Villar RN. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. The Journal of bone and joint surgery. British volume. Apr 2012;94(4):466-470. (10) Ng VY, Arora N, Best TM, Pan X, Ellis TJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. The American journal of sports medicine. Nov 2010;38(11):2337-2345. (11) Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative system-atic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. Feb 2011;27(2):252-269. (12) Clohisy JC, Baca G, Beaule PE, et al. Descriptive epi-demiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. The American journal of sports medicine. Jun 2013;41(6):1348-1356. (13) Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. Jan 2013;29(1):46-53.
Figure 1 is a coronal image from a T2-weighted MRI arthrogram of the right hip in a skeletally immature male, demonstrating loss of femoral head-neck offset (cam lesion) and concomitant labral tearing.
Figure 2 demonstrates measurement of the alpha angle. First, a best-fit circle is drawn overlying the femoral head (a). A line is then drawn from the center of the femoral head down the central axis of the femoral neck (b). Finally, a line is drawn from the center of the femoral head to the point where the femoral head/neck bone becomes aspherical (i.e., is outside the circle). The alpha angle is formed by the intersection of the two lines.













![Development and Health Differences Inequalities Between Developing Countries [Date] Today I will: - Know the reasons why there are differences between.](https://static.fdocuments.in/doc/165x107/56649c945503460f9495079e/development-and-health-differences-inequalities-between-developing-countries.jpg)