Water balance, infusions
description
Transcript of Water balance, infusions

MUDr. Štefan Trenkler, PhD.I. KAIM UPJS LF a UNLP Košice
Water balance, infusions
Košice 2012

Distribution of body fluids and the Na & K concentrations in the body water
compartments
Lobo DN: Physiological Aspects of Fluid and Electrolyte Balance, 2002 42 l = 28 + 14 (3,5 + 10,5) litres

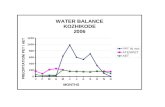
DAILY WATER BALANCE IN ADULTS WATER INTAKE
Water intake in form of fluids (volumes of drinks including soups)
1000-1500 ml
Water intake in form of semi-solid and solid foods
700 ml
Water of oxidation 300 ml Total daily water intake 2000-2500 ml WATER OUTPUT
water loss in urine 1000-1500 ml water loss through skin 500 ml
water loss through lungs 400 ml water loss in stools 100 ml
Total daily output 2000-2500 ml

Fluid balance

ADDITIONS TO MINIMUM WATER REQUIREMENT, DEPENDING ON CLINICAL SITUATION IN ADULTS
(osmotic free water)
- temperature elevation by 1 oC - moderate sweating - marked sweating, high fever - hyperventilation - hyperventilation in very dry surroundings - exposed wound surfaces and body cavities
(operation lasting up to 5 hours)
100-300 ml 500 ml
1000-1500 ml 500 ml
1000-1500 ml 500-3000 ml

Water, electrolytes homeostasis
• Adequate volume of circulating plasma = normal tissue perfusion
• ECF volume ~ total body Na+ content• Kidney – filtration, reabsorbtion of
water, Na+
• Hormones – renin, aldosteron, ADH; ANP
• Potassium

Na+: 1,5 mmol/kg/dK+: 1 mmol/kg/d

Homeostasis disturbances
• Water – hyper and dehydratation• Osmolality (Na) – hyper a
hypoosmolality• Oncotic disturbances • Ions disturbances• ABG disturbances

Osmotic pressure
Osmotic pressure is force per area that prevents water from passing through membrane!

Osmotic pressure (e.g. erytrocyte)

LABORATORY FINDINGS IN DISORDERS OF WATER BALANCE Disorder Na
mmol/l MCHC
g/l Protein
g/l Hb
mmol/l Hct %
RCC T/l
MCV fl
Normal range 135-145 320-360M 300-340F
65-80 8,7-11,2M
7,4-9,9F
40-48M 36-42F
4,5-6,1M 4,1-5,3F
82-93
Hypotonic dehydration
Isotonic dehydration
n n n
Hypertonic dehydration
Hypotonic overhydration
Isotonic overhydration
n n n
Hypertonic overhydration
If isotonic dehydration is caused by blood loss, total protein, RCC, Hb and Hct are normal or low. If isotonic dehydration is caused by plasma loss, total protein is normal or low. MCHC = mean (erythrocyte) cellular haemoglobin concentration, Hb = haemoglobin, Hct = haematocrit, RCC = red cell count, MCV = mean (erythrocyte) cellular volume,

Fluid inputMaintaining the IC and EC fluid volume
1. Basic requirements (30 ml/kg/d)(1000 ml NS 0.9%; 2000 ml free water (Glu); 60 mmol KCl)
2. Pre-existing deficit (signs of dehydratation/hypovolemia - assessment)
3. Additional losses

Hydratation status, intravascular volume assessment
• History• Physical examination (P, BP, RR, CR,
MM, diuresis)• Tests results (Na, K, osmolality, HTC,
urea)• Patient response to the fluid
administration (physiological parameters)(10 – 20 ml NS 0.9%/kg)

Hypovolemia (fluid depletion)
• Hypotension MAP<65 mm Hg, tachykardia
Diuresis body weight• MAC (MLAC) CVP PAWP LVEDP (TEE)

Distribution of infused fluids in the body water compartments
Lobo DN: Physiological Aspects of Fluid and Electrolyte Balance, 2002

Crystalloids composition
[mmol/l] K Na Cl Ca HPO4 HCO3 Mg kJ kcal inéF1/1 154 154F1/2 77 77 428 103 G 25 gRinger 4 147 156 2,3Ringer L 5,4 130 112 1,8 Lt 27Hartmann 5,4 130 112 1,8 2 Lt 30Darrow 36 120 104 Lt 52Plasmalyte 4 140 98G 5% 855 205 G 50 gG 10% 1710 410 G 100 gArgininCl 21% 1000NaHCO3 8,4% 1000 1000

Colloids
Natural
• Plasma 5 % (frozen)
• Albumin 4,5 %, 20 %
Synthetic
Gelatine Dextran 40, 70 Hydroxyetylstarch
– HAES, Voluven,

Crystalloids vs colloids
• No differences in clinical outcome• More oedema with crystalloids• More rapid replacement with colloids
(permeability)• Risk vs benefit; cost• Newer (better) HEAS?• Mixture of C&C

Fluid replacement
Loss of 1 liter of blood:
Replacement: 1 l of blood or 1 l of colloid (IV)
or 4 l of crystalloid (EC)
or 12 l of glucose (IV + EC + IC)
Distribution volumes of fluids!
Speed of loosesReplace what is lostVolume vs haemoglobinOral/GI route has preference!!!

Guidelines for transfusion of red cells
AAGBI 2001
• Normally patients should not be not transfused if the haemoglobin concentration is >100 g/l.
• A strong indication for transfusion is a haemoglobin concentration <70 g/l.
• Transfusion will become essential when the haemoglobin concentration decreases to 50 g/l.
• A haemoglobin concentration between 80 and 100 g/l is a safe level even for those patients with significant cardiorespiratory disease.
• Symptomatic patients should be transfused

Transfusion trigger
• HB (g/L) Clinical situation
• 100 Acute coronary syndrome• 90 Stabile heart failure• 80 Aged, vascular surgery, sepsis• 70 All other patients

Blood transfusions
• In the meantime – complex decision; prudent and conservative management, based on: - awareness of risks - individual haemoglobin level (70-100 g/L) - clinical judgement based on the sound understanding of the normal and pathological physiology - normovolaemia
• Unit-by-unit basis (1 u ~ 15 g/l), re-evaluation• Departmental/hospital guidelines; regular audit• Haemovigilance system

Fluid regime
1. Preoperative deficits2. Maintenance fluids3. Blood loss4. Losses to the third space

Situation
• Blood volume: • 70 ml x 80 kg = 5600 ml
• Blood loss:• 20% ~ 25-30 g/l = 90 g/l

• End