VCU DEATH AND COMPLICATIONS CONFERENCE. Brief Overview Surgery: Open distal gastrectomy with BII ...
-
Upload
charity-gibbs -
Category
Documents
-
view
221 -
download
1
Transcript of VCU DEATH AND COMPLICATIONS CONFERENCE. Brief Overview Surgery: Open distal gastrectomy with BII ...
Brief Overview
Surgery: Open distal gastrectomy with BII
Attending: Dr. Kaplan Resident: Jeffrey Stromberg Complication: Efferent loop obstruction,
cardiac arrest
HPI
67 year old F presented for treatment of gastric cancer. Initially presented at OSH 1 month prior for work up of N/V and abd pain. During EGD which revealed ulcerated antral mass consistent with mucinous adenocarcinoma, had a cardiac event which lead to type II 2nd degree heart block and pacemaker placement.
PMHx: breast cancer s/p segmental mastectomy 2001, HTN, hypercholesterolemia, diabetes, GERD
Medications: Albuterol, omeprazole, HCTZ, metoprolol, pravastatin, metformin, coumadin/Lovenox bridge
Exam: Unremarkable
Surgery
Supraumbilical midline incision No gross evidence of metastatic disease Palpable firm nodular mass in antrum Omentectomy and lesser omentum divided. 1st portion duodenum divided GIA stapler. Gastric body
divided with GIA stapler. Jejunum 40cm distal to ligament of Treitz used to make
antecolic retrogastric stapled gastrojejunostomy. Jejunum lined up and secured to retrogastric body with stay
sutures. Gastrotomy and eneterotomy made. Antimesenteric stapled anastomosis. TA stapler used to close defects.
TA staple line imbricated with silk
PostOp Course
POD1 NG pulled and advanced to sips Rapid return of bowel function but unable to
ever advance diet beyond clears due to persistent nausea and 1-2 episodes bilious emesis every other day.
On POD10 had 1L bilious emesis. Refused NG placement
POD11 PICC placed and GI consulted for EGD for suspected efferent limb syndrome
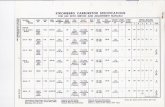
POD11 UGI performed after 3L emesis:
EGD
Great difficulty finding efferent limb but once identified was patent. Noted to be edematous and angulated.
Prior to dilation her abdomen was noted to be distended and she became tachycardic up to 150s. Was given nitropaste
Balloon dilation of efferent limb entry with 15mm balloon
At conclusion of procedure, became dyspneic and hypoxic. Rapid response called and then intubated. CXR as follows:
Subsequently went into PEA arrest. During ACLS her abdomen was needle decompressed.
Return of pulses Admitted to ICU for arctic protocol After conclusion of arctic protocol CT
head noted evidence of ischemic stroke in basal ganglia and occipital lobes.
CT abdomen at time of CT head as follows:
Retrospective analysis
Was the complication preventable Yes
Would avoiding the complication change the outcome? Would not have required EGD which lead to the
perforation and subsequent arrest. What factors contributed to the complication?
Failure to recognize pneumoperitoneum Failure to stop the procedure earlier Possible technical factors such as excessively large
bites with imbrication sutures, too large a bite with TA stapler
Postgastrectomy Syndrome
Gastric outlet obstruction Alkaline reflux gastritis Gastroparesis Roux limb syndrome Afferent loop syndrome Efferent loop syndrome Dumping syndrome
Alkaline Reflux Gastritis
Caused by reflux of intestinal contents into stomach
Symptoms typically arise late (1 year postop). Burning epigastric pain, nausea, emesis, pain aggravated by meals, pain unrelieved by emesis
Most common in BII, occasionally in B1, rare in Roux-en-Y
Work up can include EGD, Bernstein test, scintigraphy
Treatment – Braun anastomosis (historical only), antiperistaltic interpositions, conversion to Roux-en-Y (board answer)
Gastroparesis
Occurs in early postop period N/V, early satiety, bloating, abdominal pain High risk in diabetics or those who had chronic
preop gastric outlet/duodenal obstruction Diagnose with nuclear emptying study. Other
useful studies include UGI Mechanical causes include hematoma,
kinking, anastomotic leak, anastomotic edema Treat with NG decompression, TPN/tube feeds,
prokinetics (Reglan, erythromycin)
Dumping Syndrome
Caused by hyperosmolar load to intestines with subsequent hypoglycemia Postprandial weakness, dizziness,
palpitations, diaphoresis, cramping, explosive diarrhea
Surgical treatment involves delaying gastric emptying (vagotomy) and conversion to roux-en-y
Afferent limb syndrome
Only after BII Typically afferent limb too long (>40cm) Present with intermittent RUQ or epigastric
pain relieved by bilious emesis (no food particles). May have hyperamylasemia Acute setting requires prompt diagnosis to
prevent stump blowout UGI and EGD ideal tests
Treatment is surgical as causes include internal herniation, volvulus, kinking, anastomotic stenosis, adhesions.
Efferent Limb Syndrome
Similar symptoms of afferent limb syndrome – crampy pain associated with bilious emesis
Causes are the same
Tension Pneumoperitoneum
Creates hyperacute abdominal compartment syndrome Decreased preload, decreases splanchnic blood flow,
decreased ventilation, decreased cardiac output Causes
Colonoscopy, endoscopy, percutaneous endoscopic gastrostomy, CPR, mechanical ventilation in patients with pleural-peritoneal shunts
Signs Tachycardia, abdominal distension, diffuse tympany,
hypotension, obtundation, decreased minute ventilation, increased peak pressures
Treatment Emergent needle paracentesis and then +/- surgery