Uveitis for the non-ophthalmologistAnatomic classification of uveitis by primary site of...
Transcript of Uveitis for the non-ophthalmologistAnatomic classification of uveitis by primary site of...

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 1
Uveitis for the non-ophthalmologistBryn M Burkholder,1 Douglas A Jabs1,2
1Wilmer Eye Institute, Department of Ophthalmology, the Johns Hopkins University School of Medicine, Baltimore, MD, USA2Center for Clinical Trials and Evidence Synthesis, the Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, USACorrespondence to: BM Burkholder [email protected] this as: BMJ 2021;372:m4979 http://dx.doi.org/10.1136/bmj.m4979
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors.
IntroductionThe uveitides are a collection of more than 30 diseases characterized by inflammation inside the eye (table 1). They are distinct from and should not be confused with diseases of the ocular surface and sclera, which also may be affected by inflammation (eg, peripheral ulcerative keratitis, scleritis, etc), although these latter diseases may have an associated secondary intraocular inflammation (eg, keratouveitis or sclerouveitis). Although some of the uveitides are linked to a systemic infection or a rheumatologic disease, many, if not most, of the uveitides are eye limited, presumed to be immune mediated, and without any known systemic associations. The goal of the ophthalmologist is to identify the specific uveitic entity by medical history, clinical examination, ocular imaging, and supplemental laboratory testing, as indicated.
For patients with associated systemic disease or requiring systemic immunosuppression, management is optimized by collaboration between the ophthalmologist and rheumatologist and/or primary care physician. In this review, we provide an overview of the uveitides for the non-ophthalmologist clinician, including the clinical findings and diagnosis of the uveitides, and the treatment of the non-infectious uveitides, particularly through use of systemic therapy, including immunosuppressive drug therapy.
EpidemiologyWorldwide the uveitides are a major cause of visual impairment. They account for 10-15% of blindness in
developed countries3 4 and collectively are the fifth or sixth leading cause of blindness worldwide.5 6 The prevalence of uveitis in the United States is estimated as 115-133 per 100 000.7-10 Unlike the other common causes of visual impairment, such as cataract, age related macular degeneration, and glaucoma, the uveitides affect all age groups, including children, have the potential to result in visual impairment over a longer portion of the patient’s lifetime, and have a much greater impact on years of potential vision lost.11 Early diagnosis and proper treatment can prevent blindness and long term disability.12 13
Clinical featuresThe uveitides have multiple distinct presentations. Uveitis can be classified across several dimensions,
ABSTRACT
The uveitides are a heterogeneous group of diseases characterized by inflammation inside the eye. The uveitides are classified as infectious or non-infectious. The non-infectious uveitides, which are presumed to be immune mediated, can be further divided into those that are associated with a known systemic disease and those that are eye limited,—ie, not associated with a systemic disease. The ophthalmologist identifies the specific uveitic entity by medical history, clinical examination, and ocular imaging, as well as supplemental laboratory testing, if indicated. Treatment of the infectious uveitides is tailored to the particular infectious organism and may include regional and/or systemic medication. First line treatment for non-infectious uveitides is corticosteroids that can be administered topically, as regional injections or surgical implants, or systemically. Systemic immunosuppressive therapy is used in patients with severe disease who cannot tolerate corticosteroids, require chronic corticosteroids at >7.5 mg/day prednisone, or in whom the disease is known to respond better to immunosuppression. Management of many of these diseases is optimized by coordination between the ophthalmologist and rheumatologist or internist.
SOURCES AND SELECTION CRITERIA
We reviewed the literature from 1980 to the present, using the search term “uveitis” in the PubMed database, and identified relevant, peer reviewed sources, with an emphasis on large, randomized controlled trials and systematic reviews. We primarily included articles published in the last 20 years but included older sources if they contained data of significance. We included smaller trials or retrospective studies when better evidence was not available. We also included consensus guidelines from expert panels of uveitis specialists.
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
2 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
including disease course, laterality, primary anatomic location of inflammation, morphologic features, and the host, including the presence or absence of an associated systemic disease.2
In 2005, the Standardization of Uveitis Nomenclature (SUN) Working Group developed a classification scheme that structures the way clinicians and researchers describe uveitis and grade its severity (table 1).1 Anatomically, uveitis is classified by the primary site of inflammation.14 Anterior uveitis, also termed iritis or iridocyclitis, is inflammation primarily in the anterior chamber of the eye. Intermediate uveitis describes inflammation primarily in the vitreous cavity. Posterior uveitis is inflammation in the retina, choroid, or retinal blood vessels. Of note, retinal edema and optic nerve edema may be structural complications of inflammation elsewhere in the eye and do not, in isolation, constitute “posterior uveitis.” Panuveitis describes inflammation involving anterior chamber, vitreous, and retina or choroid without a predominance of any one anatomic class. In general, eyes with posterior or panuveitis have a worse prognosis, given that inflammation may cause irreversible damage to structures critical to vision, including the macula and optic nerve.4 5
Symptoms may vary greatly, even for patients with the same anatomic type of inflammation. For example, anterior chamber inflammation may cause a red, painful eye, spondyloarthritis/HLA B27 associated uveitis being a classic example. Other anterior uveitides may have no associated pain or conjunctival injection, such as juvenile idiopathic arthritis (JIA) associated chronic anterior uveitis.15 16 Similarly, the presence of symptoms does not necessarily indicate active disease. A patient with inactive disease may still have decreased vision from complications of their disease (eg, band keratopathy or chorioretinal scarring) and/or side effects of their treatment (eg, cataracts or glaucoma). In many cases, clinical examination, ocular imaging, or both are necessary to determine disease activity.
ExaminationOn ophthalmic examination with a slit lamp, it is possible to see and quantify or grade leukocytes in the anterior chamber and anterior vitreous. Other signs of anterior chamber inflammation include perilimbal injection, collections of inflammatory cells on the corneal endothelium (known as “keratic precipitates,” fig 1a), and iris nodules (fig 1b). Iris atrophy (fig 1c) is common in unilateral anterior chamber inflammation associated with the herpes simplex (HSV) and varicella zoster (VZV) viruses.17
On fundus examination, optic disc edema may be present (fig 2a) as a primary manifestation of optic nerve inflammation, or as a secondary structural complication of inflammation elsewhere in the eye. Macular edema, the most common cause of vision loss in uveitis, is caused by fluid leakage into the macula and is detected by either clinical examination or imaging (discussed below).18
Inflammation of retinal blood vessels may appear as vascular sheathing (fig 2b) or as occlusive retinal vasculitis with associated retinal hemorrhages, cotton wool spots, and non-perfusion of the retina (fig 2c). Retinitis is almost always due to infection, such as with viruses—eg, cytomegalovirus (CMV) (fig 3a), HSV, or VZV (fig 3b), or parasites—eg, toxoplasmosis (fig 3c), although Behçet disease may also present this way.2
Ocular nodules caused by granulomatous disease may be seen on the iris or in the choroid and may be the result of infections, such as tuberculosis, or non-infectious granulomatous disease, such as sarcoidosis (fig 4).
Disease course and severityDisease course, anatomic class, and laterality (unilateral, bilateral, or unilateral alternating [one eye at a time, but either eye may be affected]) are important considerations in both diagnosis and treatment. Uveitides may be acute (characterized by sudden onset and duration <3 months) and
Table 1 | Anatomic classification of uveitis and associated diseasesAnatomic class of uveitis Primary site of inflammation Systemic disease Infection No systemic diseaseAnterior uveitides Anterior chamber Spondyloarthritis/HLA B27 associated
anterior uveitis, juvenile idiopathic arthritis associated chronic anterior uveitis, sarcoidosis, Behçet disease
Herpes simplex virus anterior uveitis, varicella zoster virus anterior uveitis, cytomegalovirus anterior uveitis, syphilis
Fuchs heterochromic iridocyclitis (Fuchs uveitis syndrome)
Intermediate uveitides
Vitreous Multiple sclerosis associated intermediate uveitis, sarcoidosis, tubulointerstitial nephritis
Syphilis, Lyme disease Pars planitis, undifferentiated intermediate uveitis (intermediate uveitis, non-pars planitis type)
Posterior uveitides Retina and/or choroid Sarcoidosis Toxoplasmic retinitis, syphilis, tuberculosis, cytomegalovirus retinitis, acute retinal necrosis (herpes simplex virus or varicella zoster virus retinitis), Bartonella, Lyme disease
Acute posterior multifocal placoid pigment epitheliopathy, birdshot chorioretinopathy, multiple evanescent white dot syndrome, punctate inner choroiditis, relentless placoid choroiditis, serpiginous choroiditis, multifocal choroiditis and panuveitis*
Panuveitides Anterior chamber, vitreous, and retina or choroid (with no one site predominant)
Sarcoidosis, Behçet disease, Vogt-Koyanagi-Harada disease (separated into early stage and late stage)
Syphilis, Lyme disease Sympathetic ophthalmia
Anatomic classification of uveitis by primary site of inflammation, with examples of associated systemic diseases and infections for each type of uveitis.*Classified as “posterior uveitis” because primary site of inflammation is the choroid, with minimal anterior/vitreous inflammation.Adapted from the Standardization of Uveitis Nomenclature Working Group1 and Jabs and Busingye.2
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 3
monophasic; acute and recurrent; or chronic. As with the diagnosis of the arthritides, course, laterality, and anatomic class are helpful in narrowing the differential diagnosis. For example, patients with an acute, unilateral alternating, anterior uveitis have an ~80% chance of carrying the HLA-B27 allele, and if HLA-B27 positive, a ~60-80% chance of having an associated spondyloarthritis.19-22
The ophthalmologist determines whether uveitis is active or inactive based on clinical examination, supplemented with ocular imaging. Fluorescein angiography can show retinal vascular leakage and/or non-perfusion (fig 5a); indocyanine green angiography can show choroidal lesions (fig 5b); and fundus autofluorescence often can distinguish between active choroidal lesions and inactive scars (figs 5c, 5d). Similarly, the presence of structural complications of uveitis, shown on examination and/or imaging, may help to determine disease activity and severity and to guide treatment decisions. In this regard, optical coherence tomography (OCT) has proven to be highly useful in managing uveitic macular edema (fig 5e).
Diagnostic evaluation for associated systemic diseaseUveitides are either infectious (ie, caused by organisms in the eye) or non-infectious. The non-infectious uveitides, which are presumed to be immune mediated, can then be divided into those with and without associated systemic disease; those without an associated systemic disease may either be diagnosable as a specific uveitic entity (eg, birdshot chorioretinitis) or be “undifferentiated.”
A selected laboratory evaluation should be conducted based on the clinical features of uveitis, the patient’s medical history, and a focused review of systems. The goals of a laboratory evaluation are to diagnose an infection (where antimicrobial or antiviral therapy is indicated) or to diagnose an associated systemic disease that can affect the patient’s systemic health.2 Identifying an infectious cause of uveitis is important, because treating infectious uveitides require antimicrobials or antivirals, while non-infectious uveitides require corticosteroids and immunosuppressive therapy. Identifying an associated systemic disease is important because it may prevent future morbidity and influence choice of therapy that would treat both systemic and ocular disease.
Identifying infectious causes of uveitisAlthough the laboratory evaluation should be individualized, a syphilis test should be performed for all adolescents and adults with uveitis because syphilis is a treatable cause of uveitis that can present as any class of disease (fig 2a, 5d). Non-treponemal tests (eg, rapid plasma reagin) have an estimated 30% false negative rate, therefore a treponemal test should be first performed in all cases, utilizing the reverse screening algorithm from the Centers for Disease Control and Prevention.23 24
Fig 1 | Anterior segment findings in uveitis. (a) Granulomatous keratic precipitates on the inferior corneal endothelium. (b) Iris nodules (arrows). (c) Sectoral iris atrophy in herpetic anterior uveitis
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
4 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
Lyme disease is an uncommon cause of uveitis. Serologic Lyme disease testing is appropriate in Lyme endemic regions for intermediate uveitis and for patients exposed to Lyme disease. However, in non-endemic regions positive test results are more likely to be false, and routine testing is not recommended.25 26
Tuberculosis is a more common cause of uveitis globally, but regional variation is great, and tubercular uveitis is very uncommon in the US, accounting for only 0.2-0.5% of uveitis cases.27 The positive predictive value of routine tuberculosis testing for patients with uveitis in the US is low (in the range 1 to ~10%).28 Routine tuberculosis testing is therefore not recommended for patients with uveitis, except those who have lived or travelled in endemic regions and those with clinical presentations highly suggestive of tubercular uveitis (figs 6a, 6b). Additionally, tuberculosis testing is recommended in patients with possible exposure to tuberculosis who are starting immunosuppression for non-infectious uveitis, and in all patients, regardless of risk factors, who are starting treatment with a tumor necrosis factor-α (TNF-α) inhibitor.
Testing for selected infections using polymerase chain reaction (PCR) technology has proven to be useful. Either the aqueous or vitreous can be sampled. Diseases in which such sampling often is performed include herpetic anterior uveitis, herpetic retinitis, and toxoplasmic retinitis.29-36 Because of the low yield in routine testing, PCR for these infections should be used selectively based on clinical findings, where there is a limited differential.37-39 Of note, the ability to perform PCR testing on ocular fluid requires a laboratory capable of handling small volumes (eg, 0.1 mL) and may not be available in all locations.
Identifying non-infectious systemic disease associated with uveitisAs with testing for infectious causes of uveitis, laboratory testing for systemic disease associated with non-infectious uveitis should be based on the specific uveitic features.
HLA-B27 associated diseaseHLA-B27 associated spondyloarthritis is the most common systemic disease associated with adult anterior uveitis. It was reported in 18-32% of patients with anterior uveitis in Western countries, and in 6-13% of patients with anterior uveitis in Asia.40
When used in the appropriate clinical setting, HLA-B27 provides prognostic information; patients with spondyloarthritis/HLA-B27 associated anterior uveitis typically have recurrent acute, unilateral, or unilateral alternating episodes of anterior uveitis that often respond well to topical corticosteroid therapy.40 41
The average duration of an attack is around six weeks, and the average frequency of attacks is around one per year, although the interval between recurrences can be highly variable, even within the same patient.5 20 Because of the symptomatic nature
Fig 2 | Posterior segment findings in uveitis. (a) Optic disc swelling and hemorrhage in syphilitic uveitis (photograph courtesy of Matthew Star, MD). (b) Perivenular sheathing in sarcoidosis associated retinal vasculitis. (c) Fluorescein angiogram showing peripheral retinal non-perfusion in sarcoidosis associated retinal vasculitis
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 5
of attacks, short duration, and limited frequency, chronic, suppressive therapy typically is not needed. However, ~40% of patients will have at least one attack that requires more than topical corticosteroids (eg, a short course of oral prednisone), and ~5-10% of patients will develop a crescendo pattern resulting in chronic uveitis that requires chronic therapy.
HLA-B27 testing is also helpful in identifying patients who may have undiagnosed spondyloarthritis. In a large multicenter prospective study of patients with anterior uveitis, those who were HLA-B27 positive were more frequently diagnosed with axial (69.8% v 27.3%) and peripheral spondyloarthritis (21.9% v 11.1%) than those who were HLA-B27 negative.42 Several studies also have suggested that among patients with HLA-B27 associated anterior uveitis who have a spondyloarthritis, in approximately half, the spondyloarthritis will have been undiagnosed or misdiagnosed before the uveitis consultation.20 These results indicate that 30-50% of patients with acute anterior uveitis may have undiagnosed spondyloarthritis.43 Early diagnosis may facilitate appropriate treatment of the spondyloarthritis and prevent future morbidity.44
Patients with inflammatory bowel disease may have either of two distinct presentations of anterior uveitis; those who are HLA-B27 positive and have an axial spondyloarthritis typically have a recurrent acute anterior uveitis, whereas those who are HLA-B27 negative and have either no arthritis or the peripheral joint enteropathic arthritis may have a chronic unilateral or bilateral anterior uveitis.45 Although patients with psoriatic spondylitis may have an HLA-B27 associated recurrent acute anterior uveitis, some case series suggest that they are more likely to develop chronic anterior uveitis than are patients with ankylosing spondylitis or reactive arthritis.45 46
With the exceptions of HLA-B27 testing, and HLA-A29 in patients with suspected birdshot chorioretinitis (an eye limited disease), the utility of HLA testing as part of a uveitis diagnostic evaluation is limited.41
Antinuclear antibody associated diseaseAntinuclear antibody (ANA) testing has poor utility when used routinely in patients with uveitis. Systemic lupus erythematosus (SLE) is uncommonly associated with uveitis.27 47 In a meta-analysis including 53 315 adult patients with uveitis, the prevalence of SLE was estimated to be 0.47%, and the positive predictive value of routine ANA testing in patients with uveitis was estimated to be 2.9%.47 An earlier analysis, using a prevalence of 0.1% for lupus in patients with uveitis, calculated an even lower positive predictive value of 0.6%.27 ANA testing in adult patients has value only for those in whom there is a high pretest probability of SLE, either in patients with clinical features suggestive of lupus or in patients with an occlusive retinal vasculopathy suggesting anti-phospholipid antibody syndrome in the context of SLE.
Fig 3 Infectious retinitis. (a) Cytomegalovirus retinitis in a patient with acquired immunodeficiency syndrome. (b) Acute retinal necrosis associated with varicella zoster virus. (c) Focal retinitis associated with toxoplasma gondii infection
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
6 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
Juvenile idiopathic arthritisConversely, ANA testing is useful in children with chronic anterior uveitis, because JIA is the most common systemic disease associated with chronic anterior uveitis in childhood, and comprises 75% of all pediatric anterior uveitis cases.15 48 49 For children with JIA without uveitis, ANA testing is routinely performed as it identifies those at high risk for the development of an insidious onset, typically asymptomatic, and potentially blinding uveitis.
Chronic anterior uveitis occurs in 30% of children with JIA who are ANA positive, and the risk is similar for children with oligoarticular persistent, oligoarticular extended, and rheumatoid factor negative polyarthritis subsets.50 Because JIA associated uveitis is often asymptomatic until vision threatening complications occur, routine screening eye examinations are important, particularly for those at high risk,51-53 and screening algorithms have been developed based on the type of arthritis, ANA test results, age of the patient, and arthritis duration.
Early diagnosis and treatment, including immunosuppressive drug therapy as needed, markedly reduce the risk of vision loss in this patient population.54 Children with the enthesitis related arthritis subset of JIA, which is an HLA-B27 associated disease, develop a symptomatic recurrent acute anterior uveitis.
SarcoidosisSarcoidosis associated uveitis accounts for 5-10% of cases in large case series and may present with an acute or chronic anterior uveitis, intermediate uveitis, focal posterior uveitis (fig 4), retinal vascular sheathing (figs 2b,c), or a panuveitis.55 Therefore, nearly all patients with uveitis should be screened for sarcoidosis with radiographic imaging of the chest.56 57
Ophthalmic manifestations of sarcoidosis occur in 30-60% of patients with systemic sarcoidosis, with uveitis as the most common ocular manifestation.58
Definitive diagnosis is made by histologic confirmation on biopsy of an affected tissue. Conjunctival nodules, if present, may demonstrate granulomatous inflammation; frequently, however, there is no ocular pathology that is amenable to biopsy,
Previous studies have suggested that in patients with bilateral hilar adenopathy and uveitis, lung biopsy results nearly always confirm the diagnosis of sarcoidosis58; however, in patients with asymptomatic bilateral hilar adenopathy with normal pulmonary function tests, a lung biopsy is often not performed, because a definitive diagnosis is unlikely to change management.
Debate surrounds the best approach to chest imaging—chest radiograph or chest computed tomography (CT). Chest CT is more sensitive than chest radiography, but most cases are detected by chest radiograph. Many uveitis experts use the chest radiograph as a screening tool and reserve the chest CT scan for cases in which the chest radiograph is equivocal or atypical, or in which the suspicion for sarcoidosis is high.59 60 The serum angiotensin converting enzyme levels and lysozyme tests have very poor positive predictive values (in the ~10-20% range) and have limited utility as screening tests for sarcoidosis.2
“Eye limited” uveitisOne common misconception is that uveitis must be a manifestation of a specific underlying cause. In fact, many of the uveitides are presumed to be immune mediated and without a known association to any systemic disease.
Uveitis in patients with no associated infection or rheumatologic disease is classed as “eye limited.” Among these cases, some have clinical features that establish a specific diagnosis (eg, Fuchs heterochromic iridocyclitis or acute posterior multifocal placoid pigment epitheliopathy (fig 5c)). Identifying these morphologically distinct diseases provides information about management and prognosis.
If no identifiable infection, associated systemic disease, or specific ocular uveitic entity is present, we describe these cases as “undifferentiated” and add descriptors of course, laterality, and anatomic location (for example, “chronic, bilateral, panuveitis”).2
In the past, these cases were often described as idiopathic, a practice that leads to the following illogical conclusion: cases of chronic anterior uveitis in a child without JIA are “idiopathic,” whereas those with juvenile idiopathic arthritis are not idiopathic, when in reality both are idiopathic (ie, of unknown cause). Hence, we recommend using the term undifferentiated instead of idiopathic.
Treatment of non-infectious uveitidesThe treatment of non-infectious uveitis can be conceptualized as local therapy (including topical corticosteroids and regional injections or implants),
Fig 4 | Choroidal granuloma in a patient with sarcoidosis
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 7
systemic therapy (including oral corticosteroids, immunosuppressive drug therapy, and biologics), or a combination of the two approaches. In general, the primary anatomic site of the inflammation determines the initial approach to therapy.
Patients with anterior uveitides typically are treated with topical corticosteroids, patients with
posterior uveitides with systemic medications, and patients with panuveitis with topical corticosteroids and systemic medications. Some patients with intermediate uveitis can receive infrequent regional corticosteroid injections, but about one quarter will need systemic therapy.61 The predicted disease course determines the chronicity of therapy; patients
Fig 5 | Imaging in uveitis. (a) Fluorescein angiogram showing retinal vascular leakage in an eye with intermediate uveitis. (b) Indocyanine green angiogram showing the classic choroidal lesions seen in birdshot chorioretinitis. (c) Fundus autofluorescence showing chorioretinal lesions in acute posterior multifocal placoid pigment epitheliopathy. (d) Syphilitic posterior placoid chorioretinitis seen on fundus autofluorescence. (e) Fovea-involving macular edema, seen on optical coherence tomography, pre- and post-treatment
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
8 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
with acute or recurrent acute disease (eg, spondylitis/HLA-B27 associated anterior uveitis) are treated with a short course of treatment during an acute attack,
whereas those with chronic disease need chronic suppressive therapy.
Specific uveitic diseases may be more or less likely to require systemic therapy. For example, in patients with JIA associated chronic anterior uveitis, the use of immunosuppression reduces the risk of vision loss by ~40%, as shown in retrospective cohort studies.16 54 Similarly, specific medications are also more effective for certain type of uveitis; patients with Behçet disease and an occlusive retinal vasculitis appear to respond well to antiTNF monoclonal antibody therapy.62-64 Studies have shown that the presence of even low levels of inflammation in patients with uveitis increase the risk of visual impairment and blindness by twofold to threefold; therefore the goal of therapy is complete suppression of inflammation, while minimizing systemic and ocular side effects.54 65-67
Corticosteroid treatment Topical corticosteroidsCorticosteroids in their various forms typically are first line treatment for non-infectious uveitis. Even in those diseases where immunosuppression is indicated, corticosteroids are part of the initial regimen. Anterior chamber inflammation is amenable to treatment with corticosteroid eye drops; however, they have poor penetration to the more posterior structures of the eye and are thus poorly suited to treat intermediate and posterior uveitis. Topical corticosteroid potency for treating anterior uveitis is dependent on the corticosteroid, the preparation (salt), and the concentration, all of which influence the penetrance into the anterior chamber.
Of the older topical corticosteroid preparations, prednisolone acetate 1% had the best potency for anterior uveitis and remains a standard therapy.68 Loteprednol is slightly less effective for uveitis, but is less likely to raise the intraocular pressure, and often is used when there is an intraocular pressure rise with topical corticosteroids. Difluprednate is twice as potent as prednisolone acetate 1%, allowing less frequent use and improved adherence to treatment69 but has been associated with marked and sometimes unpredictable elevations in intraocular pressure, particularly in children.70 71
Adverse effectsAs with corticosteroids in any form, the main risks associated with topical corticosteroid use are cataract and elevated intraocular pressure, which can lead to glaucoma. Cataract in children carries the additional risk of amblyopia, or permanent vision impairment from lack of stimuli to the visual pathways in the developing brain.
Untreated inflammation itself can cause cataract and glaucoma, as well as additional irreversible complications. In studies of JIA associated chronic anterior uveitis, active uveitis was a stronger risk factor for cataract than topical corticosteroid use, and in a long term study of a large uveitis cohort, active uveitis was a strong risk factor for subsequent
Fig 6 | Clinical presentations of tubercular uveitis. (a) Active serpiginous chorioretinitis. (b) Retinal vasculitis
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 9
intraocular pressure elevation.16 54 72 73 The use of topical prednisolone acetate 1% three times a day has a minimal risk of cataract formation, and prednisone at a dose of ≤7.5 mg/day does not increase the risks of cataract formation and intraocular pressure elevation, according to a retrospective cohort study.72
Thus, prioritizing treating inflammation using the necessary quantity of corticosteroids, minimizing long term corticosteroid use with immunosuppression, and managing any ocular complications of corticosteroid use is now the preferred treatment paradigm.
Corticosteroid injections and implantsCorticosteroids can be given into or around the eye with an injection. A periocular depot of triamcinolone acetonide (Kenalog40), injected into the orbital floor or adjacent to the posterior globe, under the Tenon’s layer, is a safe and effective treatment for uveitis and uveitic macular edema.74-79 A single injection may be sufficient to control inflammation for three months or more, and one or two repeated injections, spaced >4 weeks apart, may have additional value.78
Corticosteroids can be delivered to the vitreous cavity, in the form of injection or implant. Intravitreal triamcinolone acetonide (Triescence) is used to treat non-infectious intermediate, posterior, and panuveitis, as well as uveitic macular edema.80-82 Corticosteroid implants, available in both short acting and long acting forms, are injected into the vitreous cavity and provide sustained release of corticosteroid over time. The dexamethasone implant (Ozurdex) is a biodegradable implant that releases dexamethasone for up to six months (table 2).92-94 A randomized controlled trial of the dexamethasone implant in eyes with uveitis showed reduced inflammation and visual acuity.94
A large, multicenter randomized clinical trial studied the comparative effectiveness of the three modalities of regional corticosteroid injections for uveitic macular edema—periocular triamcinolone acetonide, intravitreal triamcinolone acetonide, and the intravitreal dexamethasone implant (table 2).85 All three treatment approaches were effective; however, intravitreal corticosteroids were superior to periocular triamcinolone. Intravitreal triamcinolone and intravitreal dexamethasone implant had similar effectiveness and duration of effect, and all three approaches had similar and low rates of elevation of intraocular pressure.
Injection of triamcinolone into the suprachoroidal space has emerged as an alternative technique that may offer more targeted delivery of corticosteroid to the macula and posterior segment, potentially reducing corticosteroid induced cataract and elevation of intraocular pressure. A randomized controlled trial of patients with uveitic macular edema showed a clinically significant improvement in vision in eyes treated with suprachoroidal triamcinolone compared with sham injection (table 2).86 The relative merits of this approach and its role in the management of patients with uveitis needs to
be defined, preferably by comparative effectiveness trials.
Longer acting corticosteroid implants have also been available since the advent of the non-erodible fluocinolone acetonide 0.59 mg implant (Retisert), which was approved by the Food and Drug Administration (FDA) for the treatment of non-infectious intermediate, posterior, and panuveitides in 2005.95 96 The implant is sutured to the sclera, inside the vitreous cavity, and releases corticosteroid for up to three years with minimal systemic absorption. The implant may be replaced, if needed, to create space for additional implants. Consistent with the dose and duration of corticosteroid released by the fluocinolone acetonide implant, high rates of cataract and elevated intraocular pressure were recorded; nearly all eyes that had not had cataract surgery before placement of the implant developed a cataract and needed cataract surgery within three years of placement.96 Seventy eight per cent required intraocular pressure lowering medications, and 40% required glaucoma surgery to control eye pressure.
The Multicenter Uveitis Steroid Treatment (MUST) trial was a multicenter randomized clinical trial that compared systemic therapy with oral corticosteroids and immunosuppression to the fluocinolone acetonide implant for the treatment of non-infectious intermediate, posterior, and panuveitides.97 Patients in the MUST trial were followed for >7 years.11 91 98 Patients in the implant group underwent re-implantation of second and even third implants when the uveitis relapsed. Although both treatment approaches improved vision similarly, and successfully controlled inflammation for the first five years, eyes with implants had slightly better control of the inflammation; however, this effect disappeared after five years, and at seven years, eyes in the systemic treatment group had significantly better visual acuity than those in the implant group, with a near doubling of the risk of blindness in the implant group (table 2).91
Ocular adverse effects were more common in the implant group. Specifically, the risk of glaucoma was around threefold higher in the implant group.91
99 Systemic therapy was well tolerated, with no significant differences between the MUST trial implant and systemic groups in terms of systemic adverse events, with the exception of a greater use of antibiotics in the systemic treatment group, which reflects good medical care in patients on immunosuppression. These results highlight the relative safety of systemic corticosteroids and immunosuppression when used correctly and suggest a potential role for the fluocinolone acetonide implant when systemic therapy cannot control the inflammation or be tolerated.
More recently, long acting, injectable fluocinolone acetonide 0.18 mg and 0.19 mg inserts (FAi) (Yutiq and Iluvien, respectively) have been developed. Yutiq was FDA approved for the treatment of non-infectious intermediate, posterior, and panuveitides in 2018; Iluvien had been approved for the same indication by
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
10 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
the European Medicines Agency two years earlier.100 Similar to the dexamethasone implant described previously, the FAi inserts are injected into the vitreous cavity; however, unlike the dexamethasone implant, they are smaller, non-erodible, and release corticosteroid for around three years.
Results from a randomized controlled study of FAi compared with sham injection showed that the FAi controls inflammation, reduces the need for adjuvant therapy, and is reasonably safe to administer in a clinic setting (table 2).84 101 However, the FAi appears to be less effective than the fluocinolone acetonide implant; the FAi relapse rate at one year was 38%, whereas the fluocinolone acetonide implant rate was 4%.84 96 For both implants, cataract surgery was nearly universal, but the FAi may have a lower risk of elevated intraocular pressure. To date, there are no randomized trials comparing injectable FAi with surgically implanted fluocinolone acetonide implants.
Systemic corticosteroidsSystemic corticosteroids are used to treat severe inflammation and/or inflammation in the more posterior parts of the eye (eg, intermediate, posterior, and panuveitis). As with the treatment of rheumatologic diseases, our initial approach is to give prednisone 1 mg/kg/day, up to a maximum 60 mg/day.102 103 If an adequate response is achieved, we typically begin to taper the prednisone after
2-4 weeks. The goal of therapy is to achieve total suppression of inflammation at a prednisone dose of ≤7.5 mg/day, which has been shown to be relatively well tolerated over years with a low risk of systemic side effects.104 105
For particularly severe, vision threatening disease, high dose intravenous corticosteroids are effective and safe for short term treatment of ocular inflammation.106 107
Although the MUST trial showed the superior efficacy of systemic therapy to relapse driven regional therapy, patients on systemic therapy with uveitic macular edema may benefit from a limited number of adjunctive regional corticosteroid injections. The MUST trial reported that, among patients with uveitic macular edema treated with systemic therapy, 62% needed at least one short acting regional corticosteroid injection, but that the median number over a two year period was 1.108
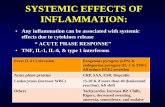
Systemic corticosteroid sparing therapyFor patients requiring unacceptably high doses of corticosteroids to control their uveitis or for those in whom the disease is known to require immunosuppression for control, corticosteroid sparing therapy with immunosuppressive medication is indicated.65 103 109 Several medications—including antimetabolites, calcineurin inhibitors, alkylating agents, and biologics—have been used successfully to treat non-infectious uveitides (table 3).
Table 2 | Selected clinical trials in uveitisTrial Year Participants No Treatment groups Follow-up Primary resultsRegional therapy trialsHURON83 2011 NIIPPU 229 Intravitreal dexamethasone
implant (IDI) 0.7 mg v IDI 0.35 mg v sham injection
26 weeks IDI effective for uveitis. Grade 0 vitreous haze in 47% v 36% v 12% (0.7 mg IDI v 0.35 mg IDI v sham); P<0.001
Fluocinolone acetonide insert (FAi)84
2019 NIIPPU 129 Intravitreal FAi 0.18 mg v sham injection
12 months FAi effective for uveitis. Uveitis relapse in 38% v 98% at 1 year (FAi v sham); P<0.001
POINT85 2019 Uveitic macular edema
192 Periocular triamcinolone acetonide (TA) 40 mg v intravitreal TA 4 mg v IDI 0.7 mg
24 weeks Periocular TA inferior to intravitreal TA and IDI for improvement macular edema and visual acuity. Mean reduction in macular thickness on OCT 23% with periocular TA v 39% with intravitreal TA (P<0.001) v 46% with IDI (P<0.001). Intravitreal TA and IDI not different (ratio of reductions 0.88; 99% CI 0.71 to 1.08).
PEACHTREE86 2020 Uveitic macular edema
160 Suprachoroidal triamcinolone acetonide 4 mg v sham injection
24 weeks Suprachoroidal TA effective for uveitic macular edema. ≥15 letter improvement in best corrected visual acuity in 47% v 16% with sham; P<0.001
Systemic therapy trialsVISUAL I87 2016 Active NIIPPU 217 Adalimumab 40 mg q2 weeks
v placebo85 weeks Adalimumab effective for uveitis. HR for relapse uveitis=0.50;
95% CI 0.36 to 0.70; P<0.001VISUAL II88 2016 Inactive NIIPPU 226 Adalimumab 40 mg q2 weeks
v placebo20 months Adalimumab effective for uveitis. HR for relapse uveitis=0.57;
95% CI 0.39 to 0.84; P=0.004.SYCAMORE89 2017 JIA associated
uveitis on methotrexate
90 Adalimumab v placebo 2 years Adalimumab effective 2nd drug for JIA associated uveitis. HR for relapse uveitis=0.25, 95% CI 0.12 to 0.49; P<0.001
FAST90 2019 NIIPPU 194 Methotrexate 25 mg/week v mycophenolate 3 g/day
12 months Methotrexate non-inferior to mycophenolate for corticosteroid sparing. OR for treatment success (methotrexate v mycophenolate)=1.5; 95% CI 0.81 to 2.81; P=0.20
Regional versus systemic therapy trialsMUST91 2017 NIIPPU 255 Intravitreal fluocinolone
acetonide implant (FAI) 0.59 mg v systemic therapy with oral corticosteroids and immunosuppression
7 years Systemic therapy superior for visual acuity at 7 years; difference in mean improvement in visual acuity (systemic therapy v FAI) 7 letters; 95% CI 2 to 12; P<0.001. OR for blindness (FAI v systemic therapy)=1.81; P=0.04. Greater use antibiotics with systemic therapy (72% v 57%; P=0.015), but no other significant differences in systemic side effects between FAI and systemic therapy
No=number of participants. NIIPPU=non-infectious intermediate, posterior, or panuveitis. OCT=optical coherence tomography. OR=odds ratio. HR=hazard ratio. CI=confidence interval.
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 11
The Systemic Immunosuppressive Therapy for Eye Diseases (SITE) cohort study, a large retrospective study of 9250 patients with ocular inflammation, provides information on the long term outcomes of systemic therapy of eye diseases, including corticosteroids, alkylating agents, and non-alkylating agents.110-114 The study showed that treatment with non-alkylating agents was associated with control of inflammation in 52-73% of patients, depending on the drug. Successful corticosteroid sparing effect (prednisone <10 mg/day) was achieved in 36-58%; however, sustained, drug free remission was uncommon (<0.10 /person year) with non-alkylating agent therapy. In contrast, treatment with alkylating agents was associated with remission in 64-91% of patients, but current use of alkylating agents is limited by the risk of serious side effects and the availability of alternatives.114-117
Corticosteroid sparing medicationThe antimetabolites methotrexate and mycophenolate mofetil are the two most widely used immunosuppressive medications for the treatment of uveitis.65 111 112 118 Our standard treatment approach is to start methotrexate at 15 mg/week and escalate to 25 mg/week in a single step, if 15 mg/week is insufficiently effective. This approach has been used as most patients who respond to methotrexate respond to 15 mg/week. Mycophenolate is initiated at 2 g/day and escalated to 3 g/day as needed.
A retrospective analysis of the SITE cohort suggested that mycophenolate and methotrexate are similarly effective for long term (9 months and beyond) use, but that mycophenolate achieves corticosteroid sparing success faster than methotrexate.90 However, methotrexate was given in a dose escalation as needed approach in this cohort.119 The First-Line Antimetabolites for Steroid-Sparing Treatment (FAST) trial randomized patients with intermediate, posterior, and panuveitides to an initial lower dose of either mycophenolate or methotrexate for two weeks and then, if tolerated, increased to the maximum dose (table 2).120 The study found that methotrexate was non-inferior to mycophenolate (ie, mycophenolate was not superior to methotrexate), suggesting that, at maximum doses, both drugs are similarly effective.
Azathioprine, a less commonly used (in the US) antimetabolite for uveitis, appears to be similarly
successful in achieving corticosteroid sparing success to mycophenolate in retrospective studies.110 However, azathioprine had a higher rate of treatment related side effects, compared with other anti-metabolites,121 and a greater proportion of patients (24% in one study) discontinued the medication because of them.110 Nevertheless, azathioprine is less expensive than mycophenolate, and is more widely used outside the US.
Although single agent antimetabolite therapy often is effective, ~20% to 25% of cases will need a second agent to control inflammation122; an antimetabolite and a calcineurin inhibitor are frequently paired together in this setting.65 Of the calcineurin inhibitors, ciclosporin and tacrolimus are most widely used in the treatment of uveitis. Both medications appear to be similarly effective, but tacrolimus is better tolerated.123 Ciclosporin in particular is less well tolerated with increasing age.113 124 The dose of ciclosporin is 2 mg/kg twice a day; tacrolimus is initiated at 1 mg twice a day, and the dose escalated every two to four weeks until a therapeutic blood level is attained (maximum dose 3 mg twice a day).65
Alkylating agents cyclophosphamide and chlorambucil are effective in the treatment of uveitis but used less frequently because of their potential toxicity.65 103 115 Unlike the non-alkylating agents, they are substantially more likely to induce drug-free remissions. In the SITE cohort, patients treated with cyclophosphamide had a 64% remission rate at two years. Two year remission rates were even higher (91%) in a study of patients being treated with cyclophosphamide for ocular mucous membrane pemphigoid, which is also an immune mediated ocular inflammatory disease.117 The relapse rate is considerably lower than that of non-alkylating agents.114 With the advent of newer alternatives for the management of uveitides, use of alkylating agent therapy has declined, and it is now used rarely.
Emerging treatmentsBiologicsThe advent of biologic medications has provided new therapeutic avenues for treating non-infectious uveitis. The tumor necrosis factor-α (TNF-α) α inhibitors—in particular, adalimumab and infliximab—are the most commonly used biologic agents in these patients.
Table 3 | Immunosuppressive medications for the uveitidesClass Generic name Trade name Suggested initial dose Typical maximum doseAntimetabolite Azathioprine, methotrexate,
mycophenolateImuran, Rheumatrex, etc Cellcept
2 mg/kg/day 15 mg/week 1 g BID
3 mg/kg/day 25 mg/week 1.5 g BID
Calcineurin inhibitor Ciclosporin, tacrolimus Neoral, etc Prograf
2 mg/kg BID 1 mg BID
2 mg/kg BID 3 mg BID
Alkylating agent Cyclophosphamide, chlorambucil Cytoxan, Leukeran 2 mg/kg/day 0.1 mg/kg/day
250 mg/day 0.2 mg/kg/day
Biologic Adalimumab, infliximab Humira, Remicade, etc 40 mg/2 week* 5 mg/kg/4 week*
40 mg/week 10 mg/kg/4 week
BID=twice per day.*After loading dose.Adapted from Jabs65
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
12 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
Adalimumab is FDA approved for the treatment of non-infectious uveitides. The results of two randomized placebo controlled trials, VISUAL I87 and VISUAL II,88 showed the safety and efficacy of adalimumab in patients with active and suppressed non-infectious intermediate, posterior, and pan-uveitides, respectively (table 2). In both studies, treatment with adalimumab was associated with reduced inflammation and lower risk of uveitis relapse and vision loss through 52 weeks. The open label extension study, VISUAL-III, showed similar results through 78 weeks, and suggested a high rate of corticosteroid sparing success.125
Adalimumab was effective in a randomized placebo controlled study of patients with JIA associated chronic anterior uveitis on a stable dose of methotrexate (table 2).89 126 127 Adalimumab has been reported to reduce attacks of recurrent uveitis in patients being treated with adalimumab for spondylitis.128 The efficacy of adalimumab versus conventional immunosuppressive therapy currently is unknown. For adult uveitis patients, adalimumab is typically given as a loading dose of 80 mg, followed one week later by a maintenance dose of 40 mg, which is then repeated every two weeks.129 For patients on the standard dose of adalimumab who have improved but have persistent inflammation, an increase to weekly dosing has been tried by some investigators with some apparent success, but has not been proven successful in a clinical trial.130 131
Compared with adalimumab, infliximab appeared to have similar efficacy in a retrospective study of uveitis patients.132 Infliximab is well tolerated and effective, with uncontrolled case series suggesting corticosteroid sparing success in ~80%.129 133 Although infliximab is approved with a wide dose range (3-10 mg/kg every four to eight weeks), retrospective data suggest that doses ≥5 mg/kg every four weeks are needed to control uveitis.103 129 133
Anti-TNF therapy appears to be particularly effective for Behçet disease uveitis, and as a second line agent in JIA associated chronic anterior uveitis.62 64 109 129 134 135 Recommendations from an expert panel of uveitis specialists suggested anti-TNF monoclonal antibody therapy (eg, infliximab or adalimumab) as first line therapy for Behçet disease uveitis and as second line therapy for JIA associated uveitis.129
Some experts recommend concurrent use of a conventional immunosuppressive agent, such as methotrexate or mycophenolate, with infliximab to reduce the risk of anti-infliximab antibodies. This practice has been shown to reduce the formation of antibodies, prolong efficacy of treatment, and prevent infusion reactions in patients receiving infliximab for Crohn’s disease.136
Other TNF-α inhibitors have been used with varying success in the treatment of uveitis in retrospective case series. Data suggest that etanercept has substantially lower efficacy in treating uveitis than adalimumab or infliximab, and its use for uveitis generally is not recommended.129 137-141 Golimumab
appears to reduce risk of uveitis in patients with ankylosing spondylitis but has not been widely studied.142
As of 2020, the data on other biologics for uveitis are fewer; however, preliminary case series of tocilizumab, an interleukin (IL)-6 receptor antagonist, have suggested that it may be effective in treating uveitis, including uveitic macular edema.143-145 Abatacept, a co-stimulation inhibitor, has not shown particular promise in early studies for JIA associated uveitis. One small study showed a sustained treatment response in less than 15% of patients with JIA associated uveitis,146 and a slightly larger study reported 49% success over a year.147 The combined results of three clinical trials for secukinumab, an IL-17A antagonist, did not show benefit in treating uveitis, despite secukinumab being very effective for psoriasis, psoriatic arthritis, and ankylosing spondylitis.148
Long term safety of systemic therapySeven year data from the MUST trial show that, with appropriate management, systemic therapy with corticosteroids and immunosuppressive medication is well tolerated.91 97 98 149 The question of long term safety was also addressed by the SITE study, which found no increased risk of mortality or cancer related mortality with corticosteroids, antimetabolites, or calcineurin inhibitors in this patient population. Although alkylating agent therapy carried no increased risk of mortality, there was a borderline significant suggestion of an increased risk of cancer related mortality.150-152
An Australian study published in 2015 reported an increased risk of non-melanotic skin cancer among patients with ocular inflammation treated with immunosuppression; however, the study included both alkylating and non-alkylating agents together.153 Moreover, given the relatively higher incidence of non-melanotic skin cancer in Australia, this study’s results may not be representative of skin cancer risk in the general population. Nevertheless, it would seem prudent to recommend the use of sunscreen and routine skin examinations in patients with uveitis on immunosuppressive drug therapy.
The long term risks associated with biologic agents in patients with uveitis are less clear, owing to the more limited amount of data available. The data from the SITE cohort were too few and the models too unstable to conclusively evaluate the risks or mortality and cancer related mortality in patients with eye disease treated with anti-TNF therapy.150 Large registries of patients with rheumatoid arthritis suggest only an increased risk of non-melanoma skin cancer.154 155 The risk of infection is increased, including with tuberculosis, with anti-TNF therapy156; hence, screening for tuberculosis, as well as hepatitis, before beginning anti-TNF therapy is recommended. Additionally, because anti-TNF therapy worsens multiple sclerosis, patients with intermediate uveitis, which is associated with a higher risk of multiple sclerosis, should be screened
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 13
with magnetic resonance imaging of the brain before initiating therapy with an anti-TNF agent.61 129 157
Treatment durationThe decision to discontinue therapy may be based on several different factors, including disease course and severity, risks associated with recurrence, and the patient’s tolerance for the current therapy. When a patient with uveitis also has associated systemic disease, their ophthalmologist and rheumatologist or internist should be involved in the decision about if and when to discontinue therapy.
As previously discussed, achieving a sustained, drug-free remission in patients with uveitis treated with non-alkylating agents is uncommon. Data from a cohort of patients with JIA associated chronic anterior uveitis indicate that median time to a sustained, drug-free remission was about 10 years in patients with mild disease, and that less than 25% of patients with severe disease achieved remission even after 20 years.52 However, another study of patients with JIA associated chronic anterior uveitis showed that the risk of relapse is lower in patients treated with methotrexate for more than three years and in those who had inactive disease for more than two years.158 This paradigm has been adopted for the use of immunosuppression in the uveitides and, for a patient who is tolerating therapy well, it is our practice to treat with non-alkylating immunosuppressive therapy for at least two years after corticosteroids have been discontinued before considering tapering immunosuppression. Given concerns for toxicity and malignancy risk associated with alkylating agents, if used at all, the target duration is one year after achieving disease quiescence and discontinuing prednisone, with a goal of limiting total duration of therapy to fewer than 18-24 months.103 159
GuidelinesThree sets of published guidelines are available, written by expert panels of uveitis specialists, for the use of systemic medications in patients with non-infectious uveitis.103 109 129 The first set of guidelines was published before widespread use of biologics in the treatment of uveitis103; the second set focused specifically on the use of biologics.129 The most recent set of guidelines answered 10 specific questions, including those about the timing of treatment escalation and discontinuation.109 All of the guidelines advocate for early and aggressive use of corticosteroid sparing therapy in patients with severe, non-infectious uveitis. Additionally, as discussed above, they recommend the use of anti-TNF therapy early in the course of Behçet associated uveitis and as second line therapy for chronic JIA associated uveitis.
ConclusionThe uveitides are a collection of more than 30 distinct diseases, and the goal of the uveitis evaluation is the identification of the specific disease. Some uveitides are associated with infection or systemic
disease; others are presumed to be immune mediated and limited to the eyes. The diagnosis of uveitis involves the intersection of clinical findings (both ocular and systemic) and focused laboratory testing. Treatment of the non-infectious uveitides involves both corticosteroids and, when indicated, immunosuppressive drug therapy. For patients with uveitis and associated systemic disease, collaboration of the ophthalmologist and rheumatologist facilitates treatment of both ocular and systemic disease and may prevent vision loss and other morbidity.Grant support: Supported in part by grant R01 EY026593 from the National Eye Institute, the National Institutes of Health, Bethesda, MD, US.Contributorship statement: Both DAJ and BMB performed the literature search, wrote the article, and participated in its revisions. DAJ is the guarantor.Patient involvement: No patients were involved were directly involved in the creation of this article.Competing interests The BMJ has judged that there are no disqualifying financial ties to commercial companies. The authors declare the following other interests: none.Further details of The BMJ policy on financial interests are here: https://www.bmj.com/about-bmj/resources-authors/forms-policies-and-checklists/declaration-competing-interestsProvenance and peer review: commissioned; externally peer reviewed.
1 Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 2005;140:509-16. doi:10.1016/j.ajo.2005.03.057
2 Jabs DA, Busingye J. Approach to the diagnosis of the uveitides. Am J Ophthalmol 2013;156:228-36. doi:10.1016/j.ajo.2013.03.027
3 Nussenblatt RB. The natural history of uveitis. Int Ophthalmol 1990;14:303-8.
4 Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, Murray PI. Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol 2004;88:1159-62. doi:10.1136/bjo.2003.037226
5 Rothova A, Suttorp-van Schulten MS, Frits Treffers W, Kijlstra A. Causes and frequency of blindness in patients with intraocular inflammatory disease. Br J Ophthalmol 1996;80:332-6. doi:10.1136/bjo.80.4.332
6 Suttorp-Schulten MS, Rothova A. The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol 1996;80:844-8. doi:10.1136/bjo.80.9.844
7 Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology 2004;111:491-500, discussion 500. doi:10.1016/j.ophtha.2003.06.014
8 Thorne JE, Suhler E, Skup M, et al. Prevalence of noninfectious uveitis in the United States: a claims-based analysis. JAMA Ophthalmol 2016;134:1237-45. doi:10.1001/jamaophthalmol.2016.3229
QUESTIONS FOR FUTURE RESEARCH• What is the role of molecular techniques such
as metagenomic deep sequencing in pathogen discovery in patients with undifferentiated uveitides?
• What is the comparative effectiveness of adalimumab versus conventional immunosuppressive agents as corticosteroid sparing treatments for non-infectious uveitides?
• What is the comparative effectiveness of long acting injectable (eg, Yutiq) versus implanted (Retisert) corticosteroid for the treatment of non-infectious uveitides?
• What is the comparative efficacy of intravitreal versus suprachoroidal corticosteroid, and what are the relative risks of cataract and glaucoma?
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
14 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
9 Jabs DA. Prevalence of the Uveitides in the United States. JAMA Ophthalmol 2016;134:1245-6. doi:10.1001/jamaophthalmol.2016.3289
10 Jabs DA. Epidemiology of uveitis. Ophthalmic Epidemiol 2008;15:283-4. doi:10.1080/09286580802478724
11 Thorne JE, Skup M, Tundia N, et al. Direct and indirect resource use, healthcare costs and work force absence in patients with non-infectious intermediate, posterior or panuveitis. Acta Ophthalmol 2016;94:e331-9. doi:10.1111/aos.12987
12 Dana MR, Merayo-Lloves J, Schaumberg DA, Foster CS. Prognosticators for visual outcome in sarcoid uveitis. Ophthalmology 1996;103:1846-53. doi:10.1016/S0161-6420(96)30417-X
13 Durrani OM, Meads CA, Murray PI. Uveitis: a potentially blinding disease. Ophthalmologica 2004;218:223-36. doi:10.1159/000078612
14 Bloch-Michel E, Nussenblatt RB. International Uveitis Study Group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol 1987;103:234-5. doi:10.1016/S0002-9394(14)74235-7
15 Foster CS. Diagnosis and treatment of juvenile idiopathic arthritis-associated uveitis. Curr Opin Ophthalmol 2003;14:395-8. doi:10.1097/00055735-200312000-00013
16 Thorne JE, Woreta F, Kedhar SR, Dunn JP, Jabs DA. Juvenile idiopathic arthritis-associated uveitis: incidence of ocular complications and visual acuity loss. Am J Ophthalmol 2007;143:840-6. doi:10.1016/j.ajo.2007.01.033
17 Van der Lelij A, Ooijman FM, Kijlstra A, Rothova A. Anterior uveitis with sectoral iris atrophy in the absence of keratitis: a distinct clinical entity among herpetic eye diseases. Ophthalmology 2000;107:1164-70. doi:10.1016/S0161-6420(00)00115-9
18 Lardenoye CW, van Kooij B, Rothova A. Impact of macular edema on visual acuity in uveitis. Ophthalmology 2006;113:1446-9. doi:10.1016/j.ophtha.2006.03.027
19 Rosenbaum JT. Characterization of uveitis associated with spondyloarthritis. J Rheumatol 1989;16:792-6.
20 Tay-Kearney ML, Schwam BL, Lowder C, et al. Clinical features and associated systemic diseases of HLA-B27 uveitis. Am J Ophthalmol 1996;121:47-56. doi:10.1016/S0002-9394(14)70533-1
21 Linssen A, Meenken C. Outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis. Am J Ophthalmol 1995;120:351-61. doi:10.1016/S0002-9394(14)72165-8
22 Monnet D, Breban M, Hudry C, Dougados M, Brézin AP. Ophthalmic findings and frequency of extraocular manifestations in patients with HLA-B27 uveitis: a study of 175 cases. Ophthalmology 2004;111:802-9. doi:10.1016/j.ophtha.2003.07.011
23 Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology 1990;97:1281-7. doi:10.1016/S0161-6420(90)32419-3
24 Centers for Disease Control and Prevention (CDC). Syphilis testing algorithms using treponemal tests for initial screening--four laboratories, New York City, 2005-2006. MMWR Morb Mortal Wkly Rep 2008;57:872-5.
25 Caplash S, Gangaputra S, Kesav N, et al. Usefulness of routine Lyme screening in patients with uveitis. Ophthalmology 2019;126:1726-8. doi:10.1016/j.ophtha.2019.06.014
26 Rifkin LM, Vadboncoeur J, Minkus CC, et al. The utility of Lyme testing in the workup of ocular inflammation. Ocul Immunol Inflamm 2019;2:1-5. doi:10.1080/09273948.2019.1657904
27 Rosenbaum JT, Wernick R. The utility of routine screening of patients with uveitis for systemic lupus erythematosus or tuberculosis. A Bayesian analysis. Arch Ophthalmol 1990;108:1291-3. doi:10.1001/archopht.1990.01070110107034
28 Albini TA, Karakousis PC, Rao NA. Interferon-gamma release assays in the diagnosis of tuberculous uveitis. Am J Ophthalmol 2008;146:486-8. doi:10.1016/j.ajo.2008.06.021
29 Schoenberger SD, Kim SJ, Thorne JE, et al. Diagnosis and treatment of acute retinal necrosis: a report by the American Academy of Ophthalmology. Ophthalmology 2017;124:382-92. doi:10.1016/j.ophtha.2016.11.007
30 Taravati P, Lam D, Van Gelder RN. Role of molecular diagnostics in ocular microbiology. Curr Ophthalmol Rep 2013;1. doi:10.1007/s40135-013-0025-1.
31 Dworkin LL, Gibler TM, Van Gelder RN. Real-time quantitative polymerase chain reaction diagnosis of infectious posterior uveitis. Arch Ophthalmol 2002;120:1534-9. doi:10.1001/archopht.120.11.1534
32 Chee SP, Bacsal K, Jap A, Se-Thoe SY, Cheng CL, Tan BH. Clinical features of cytomegalovirus anterior uveitis in immunocompetent patients. Am J Ophthalmol 2008;145:834-40. doi:10.1016/j.ajo.2007.12.015
33 Harper TW, Miller D, Schiffman JC, Davis JL. Polymerase chain reaction analysis of aqueous and vitreous specimens in the diagnosis of posterior segment infectious uveitis. Am J Ophthalmol 2009;147:140-147.e2. doi:10.1016/j.ajo.2008.07.043
34 Rothova A, de Boer JH, Ten Dam-van Loon NH, et al. Usefulness of aqueous humor analysis for the diagnosis of posterior uveitis. Ophthalmology 2008;115:306-11. doi:10.1016/j.ophtha.2007.05.014
35 McCann JD, Margolis TP, Wong MG, et al. A sensitive and specific polymerase chain reaction-based assay for the diagnosis of cytomegalovirus retinitis. Am J Ophthalmol 1995;120:219-26. doi:10.1016/S0002-9394(14)72610-8
36 Montoya JG, Parmley S, Liesenfeld O, Jaffe GJ, Remington JS. Use of the polymerase chain reaction for diagnosis of ocular toxoplasmosis. Ophthalmology 1999;106:1554-63. doi:10.1016/S0161-6420(99)90453-0
37 Holland GN. Ocular toxoplasmosis: a global reassessment. Part I: epidemiology and course of disease. Am J Ophthalmol 2003;136:973-88. doi:10.1016/j.ajo.2003.09.040
38 Holland GN. Ocular toxoplasmosis: a global reassessment. Part II: disease manifestations and management. Am J Ophthalmol 2004;137:1-17. doi:10.1016/S0002-9394(03)01319-9
39 Anwar Z, Galor A, Albini TA, Miller D, Perez V, Davis JL. The diagnostic utility of anterior chamber paracentesis with polymerase chain reaction in anterior uveitis. Am J Ophthalmol 2013;155:781-6. doi:10.1016/j.ajo.2012.12.008
40 Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol 2005;50:364-88. doi:10.1016/j.survophthal.2005.04.003
41 Zamecki KJ, Jabs DA. HLA typing in uveitis: use and misuse. Am J Ophthalmol 2010;149:189-193.e2. doi:10.1016/j.ajo.2009.09.018
42 Juanola X, Loza Santamaría E, Cordero-Coma M, Group SW, SENTINEL Working Group. Description and prevalence of spondyloarthritis in patients with anterior uveitis: The SENTINEL Interdisciplinary Collaborative Project. Ophthalmology 2016;123:1632-6. doi:10.1016/j.ophtha.2016.03.010
43 Haroon M, O’Rourke M, Ramasamy P, Murphy CC, FitzGerald O. A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: the DUET (Dublin Uveitis Evaluation Tool). Ann Rheum Dis 2015;74:1990-5. doi:10.1136/annrheumdis-2014-205358
44 Seo MR, Baek HL, Yoon HH, et al. Delayed diagnosis is linked to worse outcomes and unfavourable treatment responses in patients with axial spondyloarthritis. Clin Rheumatol 2015;34:1397-405. doi:10.1007/s10067-014-2768-y
45 Rosenbaum JT. Uveitis in spondyloarthritis including psoriatic arthritis, ankylosing spondylitis, and inflammatory bowel disease. Clin Rheumatol 2015;34:999-1002. doi:10.1007/s10067-015-2960-8
46 Zeboulon N, Dougados M, Gossec L. Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis 2008;67:955-9. doi:10.1136/ard.2007.075754
47 Gallagher K, Viswanathan A, Okhravi N. Association of systemic lupus erythematosus with uveitis. JAMA Ophthalmol 2015;133:1190-3. doi:10.1001/jamaophthalmol.2015.2249
48 Kotaniemi K, Kautiainen H, Karma A, Aho K. Occurrence of uveitis in recently diagnosed juvenile chronic arthritis: a prospective study. Ophthalmology 2001;108:2071-5. doi:10.1016/S0161-6420(01)00773-4
49 Saurenmann RK, Levin AV, Feldman BM, et al. Prevalence, risk factors, and outcome of uveitis in juvenile idiopathic arthritis: a long-term followup study. Arthritis Rheum 2007;56:647-57. doi:10.1002/art.22381
50 Ravelli A, Felici E, Magni-Manzoni S, et al. Patients with antinuclear antibody-positive juvenile idiopathic arthritis constitute a homogeneous subgroup irrespective of the course of joint disease. Arthritis Rheum 2005;52:826-32. doi:10.1002/art.20945
51 Sherry DD, Mellins ED, Wedgwood RJ. Decreasing severity of chronic uveitis in children with pauciarticular arthritis. Am J Dis Child 1991;145:1026-8.
52 Edelsten C, Lee V, Bentley CR, Kanski JJ, Graham EM. An evaluation of baseline risk factors predicting severity in juvenile idiopathic arthritis associated uveitis and other chronic anterior uveitis in early childhood. Br J Ophthalmol 2002;86:51-6. doi:10.1136/bjo.86.1.51
53 Cassidy J, Kivlin J, Lindsley C, Nocton J, Section on Rheumatology, Section on Ophthalmology. Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics 2006;117:1843-5. doi:10.1542/peds.2006-0421
54 Gregory AC2nd, Kempen JH, Daniel E, et al, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Research Group. Risk factors for loss of visual acuity among patients with uveitis associated with juvenile idiopathic arthritis: the Systemic Immunosuppressive Therapy for Eye Diseases Study. Ophthalmology 2013;120:186-92. doi:10.1016/j.ophtha.2012.07.052
55 Jabs DA, Nguyen QD. Sarcoidosis. In: Ryan SJ, ed. Retina. 4th ed. Elsevier, 2006: 1793-80210.1016/B978-0-323-02598-0.50109-9.
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
the bmj | BMJ 2021;372:m4979 | doi: 10.1136/bmj.m4979 15
56 Jabs DA, Johns CJ. Ocular involvement in chronic sarcoidosis. Am J Ophthalmol 1986;102:297-301. doi:10.1016/0002-9394(86)90001-2
57 McCannel CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG, UCLA Community-Based Uveitis Study Group. Causes of uveitis in the general practice of ophthalmology. Am J Ophthalmol 1996;121:35-46. doi:10.1016/S0002-9394(14)70532-X
58 Herbort CP, Rao NA, Mochizuki M, members of Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop On Ocular Sarcoidosis (IWOS). Ocul Immunol Inflamm 2009;17:160-9. doi:10.1080/09273940902818861
59 Maña J, Teirstein AS, Mendelson DS, Padilla ML, DePalo LR. Excessive thoracic computed tomographic scanning in sarcoidosis. Thorax 1995;50:1264-6. doi:10.1136/thx.50.12.1264
60 Lynch JP3rd. Computed tomographic scanning in sarcoidosis. Semin Respir Crit Care Med 2003;24:393-418. doi:10.1055/s-2003-42375
61 Donaldson MJ, Pulido JS, Herman DC, Diehl N, Hodge D. Pars planitis: a 20-year study of incidence, clinical features, and outcomes. Am J Ophthalmol 2007;144:812-7. doi:10.1016/j.ajo.2007.08.023
62 Taylor SR, Singh J, Menezo V, Wakefield D, McCluskey P, Lightman S. Behçet disease: visual prognosis and factors influencing the development of visual loss. Am J Ophthalmol 2011;152:1059-66. doi:10.1016/j.ajo.2011.05.032
63 Al Rashidi S, Al Fawaz A, Kangave D, Abu El-Asrar AM. Long-term clinical outcomes in patients with refractory uveitis associated with Behçet disease treated with infliximab. Ocul Immunol Inflamm 2013;21:468-74. doi:10.3109/09273948.2013.779727
64 Takeuchi M, Kezuka T, Sugita S, et al. Evaluation of the long-term efficacy and safety of infliximab treatment for uveitis in Behçet disease: a multicenter study. Ophthalmology 2014;121:1877-84. doi:10.1016/j.ophtha.2014.04.042
65 Jabs DA. Immunosuppression for the Uveitides. Ophthalmology 2018;125:193-202. doi:10.1016/j.ophtha.2017.08.007
66 Kaçmaz RO, Kempen JH, Newcomb C, et al, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study Group. Ocular inflammation in Behçet disease: incidence of ocular complications and of loss of visual acuity. Am J Ophthalmol 2008;146:828-36. doi:10.1016/j.ajo.2008.06.019
67 Thorne JE, Wittenberg S, Jabs DA, et al. Multifocal choroiditis with panuveitis incidence of ocular complications and of loss of visual acuity. Ophthalmology 2006;113:2310-6. doi:10.1016/j.ophtha.2006.05.067
68 Samudre SS, Lattanzio FAJr, Williams PB, Sheppard JDJr. Comparison of topical steroids for acute anterior uveitis. J Ocul Pharmacol Ther 2004;20:533-47. doi:10.1089/jop.2004.20.533
69 Foster CS, Davanzo R, Flynn TE, McLeod K, Vogel R, Crockett RS. Durezol (Difluprednate Ophthalmic Emulsion 0.05%) compared with Pred Forte 1% ophthalmic suspension in the treatment of endogenous anterior uveitis. J Ocul Pharmacol Ther 2010;26:475-83. doi:10.1089/jop.2010.0059
70 Birnbaum AD, Jiang Y, Tessler HH, Goldstein DA. Elevation of intraocular pressure in patients with uveitis treated with topical difluprednate. Arch Ophthalmol 2011;129:667-8. doi:10.1001/archophthalmol.2011.82
71 Slabaugh MA, Herlihy E, Ongchin S, van Gelder RN. Efficacy and potential complications of difluprednate use for pediatric uveitis. Am J Ophthalmol 2012;153:932-8. doi:10.1016/j.ajo.2011.10.008
72 Thorne JE, Woreta FA, Dunn JP, Jabs DA. Risk of cataract development among children with juvenile idiopathic arthritis-related uveitis treated with topical corticosteroids. Ophthalmology 2010;117:1436-41. doi:10.1016/j.ophtha.2009.12.003
73 Stroh IG, Moradi A, Burkholder BM, Hornbeak DM, Leung TG, Thorne JE. Occurrence of and risk factors for ocular hypertension and secondary glaucoma in juvenile idiopathic arthritis-associated uveitis. Ocul Immunol Inflamm 2017;25:503-12. doi:10.3109/09273948.2016.1142573
74 Tanner V, Kanski JJ, Frith PA. Posterior sub-Tenon’s triamcinolone injections in the treatment of uveitis. Eye (Lond) 1998;12:679-85. doi:10.1038/eye.1998.168
75 Ferrante P, Ramsey A, Bunce C, Lightman S. Clinical trial to compare efficacy and side-effects of injection of posterior sub-Tenon triamcinolone versus orbital floor methylprednisolone in the management of posterior uveitis. Clin Exp Ophthalmol 2004;32:563-8. doi:10.1111/j.1442-9071.2004.00902.x
76 Helm CJ, Holland GN. The effects of posterior subtenon injection of triamcinolone acetonide in patients with intermediate uveitis. Am J Ophthalmol 1995;120:55-64. doi:10.1016/S0002-9394(14)73759-6
77 Leder HA, Jabs DA, Galor A, Dunn JP, Thorne JE. Periocular triamcinolone acetonide injections for cystoid macular edema complicating noninfectious uveitis. Am J Ophthalmol 2011;152:441-448.e2. doi:10.1016/j.ajo.2011.02.009
78 Salek SS, Leder HA, Butler NJ, Gan TJ, Dunn JP, Thorne JE. Periocular triamcinolone acetonide injections for control of intraocular inflammation associated with uveitis. Ocul Immunol Inflamm 2013;21:257-63. doi:10.3109/09273948.2013.767353
79 Sen HN, Vitale S, Gangaputra SS, et al. Periocular corticosteroid injections in uveitis: effects and complications. Ophthalmology 2014;121:2275-86. doi:10.1016/j.ophtha.2014.05.021
80 Young S, Larkin G, Branley M, Lightman S. Safety and efficacy of intravitreal triamcinolone for cystoid macular oedema in uveitis. Clin Exp Ophthalmol 2001;29:2-6. doi:10.1046/j.1442-9071.2001.00360.x
81 Androudi S, Letko E, Meniconi M, Papadaki T, Ahmed M, Foster CS. Safety and efficacy of intravitreal triamcinolone acetonide for uveitic macular edema. Ocul Immunol Inflamm 2005;13:205-12. doi:10.1080/09273940590933511
82 Antcliff RJ, Spalton DJ, Stanford MR, Graham EM, ffytche TJ, Marshall J. Intravitreal triamcinolone for uveitic cystoid macular edema: an optical coherence tomography study. Ophthalmology 2001;108:765-72. doi:10.1016/S0161-6420(00)00658-8
83 Lowder C, Belfort RJr, Lightman S, et al, Ozurdex HURON Study Group. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol 2011;129:545-53. doi:10.1001/archophthalmol.2010.339
84 Jaffe GJ, Foster CS, Pavesio CE, Paggiarino DA, Riedel GE. Effect of an injectable fluocinolone acetonide insert on recurrence rates in chronic noninfectious uveitis affecting the posterior segment: twelve-month results. Ophthalmology 2019;126:601-10. doi:10.1016/j.ophtha.2018.10.033
85 Thorne JE, Sugar EA, Holbrook JT, et al, Multicenter Uveitis Steroid Treatment Trial Research Group. Periocular Triamcinolone vs. Intravitreal Triamcinolone vs. Intravitreal Dexamethasone Implant for the Treatment of Uveitic Macular Edema: The PeriOcular vs. INTravitreal corticosteroids for uveitic macular edema (POINT) Trial. Ophthalmology 2019;126:283-95. doi:10.1016/j.ophtha.2018.08.021
86 Yeh S, Khurana RN, Shah M, et al, PEACHTREE Study Investigators. Efficacy and safety of suprachoroidal CLS-TA for macular edema secondary to noninfectious uveitis: phase 3 randomized trial. Ophthalmology 2020;127:948-55. doi:10.1016/j.ophtha.2020.01.006
87 Jaffe GJ, Dick AD, Brézin AP, et al. Adalimumab in patients with active noninfectious uveitis. N Engl J Med 2016;375:932-43. doi:10.1056/NEJMoa1509852
88 Nguyen QD, Merrill PT, Jaffe GJ, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet 2016;388:1183-92. doi:10.1016/S0140-6736(16)31339-3
89 Ramanan AV, Dick AD, Jones AP, et al, SYCAMORE Study Group. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N Engl J Med 2017;376:1637-46. doi:10.1056/NEJMoa1614160
90 Gangaputra SS, Newcomb CW, Joffe MM, et al, SITE Cohort Research Group. Comparison between methotrexate and mycophenolate mofetil monotherapy for the control of noninfectious ocular inflammatory diseases. Am J Ophthalmol 2019;208:68-75. doi:10.1016/j.ajo.2019.07.008
91 Kempen JH, Altaweel MM, Holbrook JT, Sugar EA, Thorne JE, Jabs DAWriting Committee for the Multicenter Uveitis Steroid Treatment (MUST) Trial and Follow-up Study Research Group. Association between long-lasting intravitreous fluocinolone acetonide implant vs systemic anti-inflammatory therapy and visual acuity at 7 years among patients with intermediate, posterior, or panuveitis. JAMA 2017;317:1993-2005. doi:10.1001/jama.2017.5103
92 Chang-Lin JE, Attar M, Acheampong AA, et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci 2011;52:80-6. doi:10.1167/iovs.10-5285
93 Kuppermann BD, Blumenkranz MS, Haller JA, et al, Dexamethasone DDS Phase II Study Group. Randomized controlled study of an intravitreous dexamethasone drug delivery system in patients with persistent macular edema. Arch Ophthalmol 2007;125:309-17. doi:10.1001/archopht.125.3.309
94 Lowder C, Belfort RJr, Lightman S, et al, Ozurdex HURON Study Group. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol 2011;129:545-53. doi:10.1001/archophthalmol.2010.339
95 Jaffe GJ, Ben-Nun J, Guo H, Dunn JP, Ashton P. Fluocinolone acetonide sustained drug delivery device to treat severe uveitis. Ophthalmology 2000;107:2024-33. doi:10.1016/S0161-6420(00)00466-8
96 Callanan DG, Jaffe GJ, Martin DF, Pearson PA, Comstock TL. Treatment of posterior uveitis with a fluocinolone acetonide implant: three-year clinical trial results. Arch Ophthalmol 2008;126:1191-201. doi:10.1001/archopht.126.9.1191
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

STATE OF THE ART REVIEW
16 doi: 10.1136/bmj.m4979 | BMJ 2021;372:m4979 | the bmj
97 Kempen JH, Altaweel MM, Holbrook JT, et al, Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group. Randomized comparison of systemic anti-inflammatory therapy versus fluocinolone acetonide implant for intermediate, posterior, and panuveitis: the multicenter uveitis steroid treatment trial. Ophthalmology 2011;118:1916-26. doi:10.1016/j.ophtha.2011.07.027
98 Multicenter Uveitis Steroid Treatment (MUST) Trial Follow-up Study Research Group. Quality of life and risks associated with systemic anti-inflammatory therapy versus fluocinolone acetonide intraocular implant for intermediate uveitis, posterior uveitis, or panuveitis: fifty-four-month results of the multicenter uveitis steroid treatment trial and follow-up study. Ophthalmology 2015;122:1976-86. doi:10.1016/j.ophtha.2015.06.043
99 Friedman DS, Holbrook JT, Ansari H, et al, MUST Research Group. Risk of elevated intraocular pressure and glaucoma in patients with uveitis: results of the multicenter uveitis steroid treatment trial. Ophthalmology 2013;120:1571-9. doi:10.1016/j.ophtha.2013.01.025
100 Jaffe GJ, Lin P, Keenan RT, Ashton P, Skalak C, Stinnett SS. Injectable fluocinolone acetonide long-acting implant for noninfectious intermediate uveitis, posterior uveitis, and panuveitis: two-year results. Ophthalmology 2016;123:1940-8. doi:10.1016/j.ophtha.2016.05.025
101 Jaffe GJ, Pavesio CE, Study I, Study Investigators. Effect of a fluocinolone acetonide insert on recurrence rates in noninfectious intermediate, posterior, or panuveitis: three-year results. Ophthalmology 2020;127:1395-404. doi:10.1016/j.ophtha.2020.04.001
102 Jabs DA. Treatment of ocular inflammation. Ocul Immunol Inflamm 2004;12:163-8. doi:10.1080/09273940490883671
103 Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol 2000;130:492-513. doi:10.1016/S0002-9394(00)00659-0
104 Da Silva JA, Jacobs JW, Kirwan JR, et al. Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis 2006;65:285-93. doi:10.1136/ard.2005.038638
105 Hwang YG, Saag K. The safety of low-dose glucocorticoids in rheumatic diseases. Clin Exp Rheumatol 2011;29(Suppl 68):S104-12.
106 Charkoudian LD, Ying GS, Pujari SS, et al. High-dose intravenous corticosteroids for ocular inflammatory diseases. Ocul Immunol Inflamm 2012;20:91-9. doi:10.3109/09273948.2011.646382
107 Beck RW, Cleary PA, Anderson MMJr, et al, The Optic Neuritis Study Group. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. N Engl J Med 1992;326:581-8. doi:10.1056/NEJM199202273260901
108 Tomkins-Netzer O, Lightman S, Drye L, et al, Multicenter Uveitis Steroid Treatment Trial Research Group. Outcome of treatment of uveitic macular edema: The Multicenter Uveitis Steroid Treatment Trial 2-year results. Ophthalmology 2015;122:2351-9. doi:10.1016/j.ophtha.2015.07.036
109 Dick AD, Rosenbaum JT, Al-Dhibi HA, et al, Fundamentals of Care for Uveitis International Consensus Group. Guidance on noncorticosteroid systemic immunomodulatory therapy in noninfectious uveitis: Fundamentals of Care for UveitiS (FOCUS) Initiative. Ophthalmology 2018;125:757-73. doi:10.1016/j.ophtha.2017.11.017
110 Pasadhika S, Kempen JH, Newcomb CW, et al. Azathioprine for ocular inflammatory diseases. Am J Ophthalmol 2009;148:500-509.e2. doi:10.1016/j.ajo.2009.05.008
111 Gangaputra S, Newcomb CW, Liesegang TL, et al, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study. Methotrexate for ocular inflammatory diseases. Ophthalmology 2009;116:2188-98.e1. doi:10.1016/j.ophtha.2009.04.020
112 Daniel E, Thorne JE, Newcomb CW, et al. Mycophenolate mofetil for ocular inflammation. Am J Ophthalmol 2010;149:423-32.e1, 2. doi:10.1016/j.ajo.2009.09.026
113 Kaçmaz RO, Kempen JH, Newcomb C, et al. Cyclosporine for ocular inflammatory diseases. Ophthalmology 2010;117:576-84. doi:10.1016/j.ophtha.2009.08.010
114 Pujari SS, Kempen JH, Newcomb CW, et al. Cyclophosphamide for ocular inflammatory diseases. Ophthalmology 2010;117:356-65. doi:10.1016/j.ophtha.2009.06.060
115 Akpek EK, Jabs DA, Tessler HH, Joondeph BC, Foster CS. Successful treatment of serpiginous choroiditis with alkylating agents. Ophthalmology 2002;109:1506-13. doi:10.1016/S0161-6420(02)01097-7
116 Goldstein DA, Fontanilla FA, Kaul S, Sahin O, Tessler HH. Long-term follow-up of patients treated with short-term high-dose chlorambucil for sight-threatening ocular inflammation. Ophthalmology 2002;109:370-7. doi:10.1016/S0161-6420(01)00942-3
117 Thorne JE, Woreta FA, Jabs DA, Anhalt GJ. Treatment of ocular mucous membrane pemphigoid with immunosuppressive drug therapy. Ophthalmology 2008;115:2146-2152.e1. doi:10.1016/j.ophtha.2008.08.002
118 Rathinam SR, Babu M, Thundikandy R, et al. A randomized clinical trial comparing methotrexate and mycophenolate mofetil for noninfectious uveitis. Ophthalmology 2014;121:1863-70. doi:10.1016/j.ophtha.2014.04.023
119 Jabs DA. Antimetabolite therapy for uveitis: methotrexate or mycophenolate?JAMA Ophthalmol 2019;137:1449-51. doi:10.1001/jamaophthalmol.2019.3964
120 Rathinam SR, Gonzales JA, Thundikandy R, et al, FAST Research Group. Effect of corticosteroid-sparing treatment with mycophenolate mofetil vs methotrexate on inflammation in patients with uveitis: a randomized clinical trial. JAMA 2019;322:936-45. doi:10.1001/jama.2019.12618
121 Galor A, Jabs DA, Leder HA, et al. Comparison of antimetabolite drugs as corticosteroid-sparing therapy for noninfectious ocular inflammation. Ophthalmology 2008;115:1826-32. doi:10.1016/j.ophtha.2008.04.026
122 Goldberg NR, Lyu T, Moshier E, Godbold J, Jabs DA. Success with single-agent immunosuppression for multifocal choroidopathies. Am J Ophthalmol 2014;158:1310-7. doi:10.1016/j.ajo.2014.08.039
123 Murphy CC, Greiner K, Plskova J, et al. Cyclosporine vs tacrolimus therapy for posterior and intermediate uveitis. Arch Ophthalmol 2005;123:634-41. doi:10.1001/archopht.123.5.634
124 Nussenblatt RB, Palestine AG, Chan CC, Stevens GJr, Mellow SD, Green SB. Randomized, double-masked study of cyclosporine compared to prednisolone in the treatment of endogenous uveitis. Am J Ophthalmol 1991;112:138-46. doi:10.1016/S0002-9394(14)76692-9
125 Suhler EB, Adán A, Brézin AP, et al. Safety and efficacy of adalimumab in patients with noninfectious uveitis in an ongoing open-label study: VISUAL III. Ophthalmology 2018;125:1075-87. doi:10.1016/j.ophtha.2017.12.039
126 Ramanan AV, Dick AD, Benton D, et al, SYCAMORE Trial Management Group. A randomised controlled trial of the clinical effectiveness, safety and cost-effectiveness of adalimumab in combination with methotrexate for the treatment of juvenile idiopathic arthritis associated uveitis (SYCAMORE Trial). Trials 2014;15:14. doi:10.1186/1745-6215-15-14
127 Horton S, Jones AP, Guly CM, et al. Adalimumab in juvenile idiopathic arthritis-associated uveitis: 5-year follow-up of the Bristol participants of the SYCAMORE trial. Am J Ophthalmol 2019;207:170-4. doi:10.1016/j.ajo.2019.06.007
128 Rudwaleit M, Rødevand E, Holck P, et al. Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: results of a prospective open-label study. Ann Rheum Dis 2009;68:696-701. doi:10.1136/ard.2008.092585
129 Levy-Clarke G, Jabs DA, Read RW, Rosenbaum JT, Vitale A, Van Gelder RN. Expert panel recommendations for the use of anti-tumor necrosis factor biologic agents in patients with ocular inflammatory disorders. Ophthalmology 2014;121:785-96.e3. doi:10.1016/j.ophtha.2013.09.048
130 Lee J, Koreishi AF, Zumpf KB, Minkus CL, Goldstein DA. Success of weekly adalimumab in refractory ocular inflammatory disease. Ophthalmology 2020;127:1431-3. doi:10.1016/j.ophtha.2020.04.009
131 Liberman P, Berkenstock MK, Burkholder BM, Chaon BC, Thorne JE. Escalation to weekly adalimumab for the treatment of ocular inflammation. Ocul Immunol Inflamm 2020;1-5. doi:10.1080/09273948.2020.1749857.
132 Vallet H, Seve P, Biard L, et al, French Uveitis Network. Infliximab versus adalimumab in the treatment of refractory inflammatory uveitis: a multicenter study from the French uveitis network. Arthritis Rheumatol 2016;68:1522-30. doi:10.1002/art.39667
133 Kruh JN, Yang P, Suelves AM, Foster CS. Infliximab for the treatment of refractory noninfectious Uveitis: a study of 88 patients with long-term follow-up. Ophthalmology 2014;121:358-64. doi:10.1016/j.ophtha.2013.07.019
134 Díaz-Llopis M, Salom D, Garcia-de-Vicuña C, et al. Treatment of refractory uveitis with adalimumab: a prospective multicenter study of 131 patients. Ophthalmology 2012;119:1575-81. doi:10.1016/j.ophtha.2012.02.018
135 Braun J, Baraliakos X, Listing J, Sieper J. Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheum 2005;52:2447-51. doi:10.1002/art.21197
136 Baert F, Noman M, Vermeire S, et al. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N Engl J Med 2003;348:601-8. doi:10.1056/NEJMoa020888
137 Foster CS, Tufail F, Waheed NK, et al. Efficacy of etanercept in preventing relapse of uveitis controlled by methotrexate. Arch Ophthalmol 2003;121:437-40. doi:10.1001/archopht.121.4.437
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

No commercial reuse: See rights and reprints http://www.bmj.com/permissions Subscribe: http://www.bmj.com/subscribe
STATE OF THE ART REVIEW
138 Galor A, Perez VL, Hammel JP, Lowder CY. Differential effectiveness of etanercept and infliximab in the treatment of ocular inflammation. Ophthalmology 2006;113:2317-23. doi:10.1016/j.ophtha.2006.04.038
139 Reiff A. Long-term outcome of etanercept therapy in children with treatment-refractory uveitis. Arthritis Rheum 2003;48:2079-80. doi:10.1002/art.11155
140 Reiff A, Takei S, Sadeghi S, et al. Etanercept therapy in children with treatment-resistant uveitis. Arthritis Rheum 2001;44:1411-5. doi:10.1002/1529-0131(200106)44:6<1411::AID-ART235>3.0.CO;2-O
141 Smith JA, Thompson DJ, Whitcup SM, et al. A randomized, placebo-controlled, double-masked clinical trial of etanercept for the treatment of uveitis associated with juvenile idiopathic arthritis. Arthritis Rheum 2005;53:18-23. doi:10.1002/art.20904
142 van Bentum RE, Heslinga SC, Nurmohamed MT, et al. Reduced occurrence rate of acute anterior uveitis in ankylosing spondylitis treated with golimumab—the GO-EASY study. J Rheumatol 2019;46:153-9. doi:10.3899/jrheum.180312
143 Calvo-Río V, Santos-Gómez M, Calvo I, et al. Anti-interleukin-6 receptor tocilizumab for severe juvenile idiopathic arthritis-associated uveitis refractory to anti-tumor necrosis factor therapy: a multicenter study of twenty-five patients. Arthritis Rheumatol 2017;69:668-75. doi:10.1002/art.39940
144 Tappeiner C, Mesquida M, Adán A, et al. Evidence for tocilizumab as a treatment option in refractory uveitis associated with juvenile idiopathic arthritis. J Rheumatol 2016;43:2183-8. doi:10.3899/jrheum.160231
145 Vegas-Revenga N, Calvo-Río V, Mesquida M, et al. Anti-IL6-receptor tocilizumab in refractory and noninfectious uveitic cystoid macular edema: multicenter study of 25 patients. Am J Ophthalmol 2019;200:85-94. doi:10.1016/j.ajo.2018.12.019
146 Tappeiner C, Miserocchi E, Bodaghi B, et al. Abatacept in the treatment of severe, longstanding, and refractory uveitis associated with juvenile idiopathic arthritis. J Rheumatol 2015;42:706-11. doi:10.3899/jrheum.140410
147 Birolo C, Zannin ME, Arsenyeva S, et al. Comparable efficacy of abatacept used as first-line or second-line biological agent for severe juvenile idiopathic arthritis-related uveitis. J Rheumatol 2016;43:2068-73. doi:10.3899/jrheum.151389
148 Dick AD, Tugal-Tutkun I, Foster S, et al. Secukinumab in the treatment of noninfectious uveitis: results of three randomized, controlled clinical trials. Ophthalmology 2013;120:777-87. doi:10.1016/j.ophtha.2012.09.040
149 Kempen JH, Altaweel MM, Drye LT, et al, Multicenter Uveitis Steroid Treatment (MUST) Trial Research Group. Benefits of systemic anti-inflammatory therapy versus fluocinolone acetonide intraocular
implant for intermediate uveitis, posterior uveitis, and panuveitis: Fifty-four-month results of the multicenter uveitis steroid treatment (MUST) trial and follow-up study. Ophthalmology 2015;122:1967-75. doi:10.1016/j.ophtha.2015.06.042
150 Kempen JH, Daniel E, Dunn JP, et al. Overall and cancer related mortality among patients with ocular inflammation treated with immunosuppressive drugs: retrospective cohort study. BMJ 2009;339:b2480. doi:10.1136/bmj.b2480
151 Kempen JH, Gangaputra S, Daniel E, et al. Long-term risk of malignancy among patients treated with immunosuppressive agents for ocular inflammation: a critical assessment of the evidence. Am J Ophthalmol 2008;146:802-12.e1. doi:10.1016/j.ajo.2008.04.035
152 Khachatryan N, Kempen JH. Immunosuppressive therapy and cancer risk in ocular inflammation patients: fresh evidence and more questions. Ophthalmology 2015;122:219-21. doi:10.1016/j.ophtha.2014.11.023
153 Yates WB, Vajdic CM, Na R, McCluskey PJ, Wakefield D. Malignancy risk in patients with inflammatory eye disease treated with systemic immunosuppressive therapy: a tertiary referral cohort study. Ophthalmology 2015;122:265-73. doi:10.1016/j.ophtha.2014.08.024
154 Wolfe F, Michaud K. Biologic treatment of rheumatoid arthritis and the risk of malignancy: analyses from a large US observational study. Arthritis Rheum 2007;56:2886-95. doi:10.1002/art.22864
155 Wolfe F, Michaud K. The effect of methotrexate and anti-tumor necrosis factor therapy on the risk of lymphoma in rheumatoid arthritis in 19,562 patients during 89,710 person-years of observation. Arthritis Rheum 2007;56:1433-9. doi:10.1002/art.22579
156 Dixon WG, Symmons DP, Lunt M, Watson KD, Hyrich KL, Silman AJBritish Society for Rheumatology Biologics Register Control Centre Consortium, British Society for Rheumatology Biologics Register. Serious infection following anti-tumor necrosis factor alpha therapy in patients with rheumatoid arthritis: lessons from interpreting data from observational studies. Arthritis Rheum 2007;56:2896-904. doi:10.1002/art.22808
157 Petrushkin H, Kidd D, Pavesio C. Intermediate uveitis and multiple sclerosis: to scan or not to scan. Br J Ophthalmol 2015;99:1591-3. doi:10.1136/bjophthalmol-2015-307269
158 Kalinina Ayuso V, van de Winkel EL, Rothova A, de Boer JH. Relapse rate of uveitis post-methotrexate treatment in juvenile idiopathic arthritis. Am J Ophthalmol 2011;151:217-22. doi:10.1016/j.ajo.2010.08.021
159 Radis CD, Kahl LE, Baker GL, et al. Effects of cyclophosphamide on the development of malignancy and on long-term survival of patients with rheumatoid arthritis. A 20-year followup study. Arthritis Rheum 1995;38:1120-7. doi:10.1002/art.1780380815
on 21 July 2021 by guest. Protected by copyright.
http://ww
w.bm
j.com/
BM
J: first published as 10.1136/bmj.m
4979 on 3 February 2021. D
ownloaded from

![Role of systemic inflammation in cirrhosis: From pathogenesis to … · 2017. 5. 2. · including oxidative stress, systemic inflammation, and organ dysfunction[5]. Systemic inflammation](https://static.fdocuments.in/doc/165x107/612db72a1ecc515869425c9c/role-of-systemic-inflammation-in-cirrhosis-from-pathogenesis-to-2017-5-2-including.jpg)