Using Analytical Models to Site Medical Distribution Centers€¦ · an Emergency event, what is...
Transcript of Using Analytical Models to Site Medical Distribution Centers€¦ · an Emergency event, what is...
Using Analytical Models to Site Medical Distribution Centers
Nicholas A. Jackson and Julie KanzlerArlington County and City of Alexandria, VA
Medical Distribution Centers Model
Presentation Outline
• City of Alexandria– GIS and stakeholders– Project and model
• Arlington County– Project and model– Application and joint effort
Medical Distribution Centers Model
The Big Picture
When we fail to make Spatial Analysis part of the pre-event planning strategy, we can overlook critical selection criteria, such as the population each center might serve and its relative accessibility.
Under the City's default strategy, which uses schools as Emergency Medical Distribution Centers, portions of the City are effectively "cut off" from pedestrian access. To develop a better alternative, we generated a city-wide boolean raster model of pedestrian barriers ("Walking Accessibility Surface") and optimized allocations to centers based on walking accessibility, evenness of allocation, and landmark quality.
Medical Distribution Centers Model
City Readiness Initiative
• Originated from CDC City Readiness Initiative– Aids state and local officials in developing plans that
support mass dispensing drugs to 100% of the identified population within 48 hours of a decision to do so.
– Provides funding to states, whose CRI jurisdictions cover 500 counties. This means that 56% of the US population lives within a CRI jurisdiction.
– Awarded Metropolitan Statistical Areas (MSA) close to $60 million in aid for 2006-2007
– For more detailed information: http://www.bt.cdc.gov/planning/guidance05/pdf/appendix3.pdf
• Transportation Modes for Citizens– Walking only
• Between 1 and 1½ Mile Walking Distance
Medical Distribution Centers Model
Evolution
• Both jurisdictions received this project as a basic “buffer analysis”– Stakeholders in each City’s Health Department
identified the need for a GIS role in the decision-making, but didn’t know the best way to answer the question at hand: how do we best choose and evaluate which sites we choose for emergency medical distribution centers?
• Alexandria developed the model, and Arlington became interested in participating through a presentation among regional health departments
Medical Distribution Centers Model
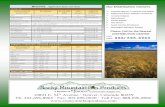
The Starting point - Schools
Mean Walking Distance (ft)
1000
2000
3000
4000
5000
6000
7000
8000
051015202530354045
No. of Facilities
% Households outside 1 mi Walking Distance from Selected Facility
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
051015202530354045No. of Facilities
Medical Distribution Centers Model
The Question
• Assuming that the population is on foot during an Emergency event, what is the optimal location and number of Medical Distribution Centers?– Whether the emergency event is an Anthrax Plume
or the Aftermath of a Hurricane, Medical supplies and services (e.g., Vaccines, Medications, Supplies, and Basic Triage) need to be distributed efficiently and equitably during and after it. This is why we need to make Spatial Analysis part of the pre-event planning strategy.
Medical Distribution Centers Model
Walking v. “as the crow flies”
• E.g., people tend to avoid crossing into private residential property– We still need
references for these assumptions
Medical Distribution Centers Model
Tools & Inputs
• Tools– ArcGIS ModelBuilder– ArcGIS Spatial Analyst
• Inputs– Boolean raster surface based on 100-scale
planimetric data (our “Walking Accessibility Surface”)
• Paved areas and roads, sidewalks and crosswalks, building footprints, rail lines, parcels, even fences
• Rasterize and classify barriers based objective rules
– Housing Unit data• A proxy for family count
– Assumption: one person from each family to user the center
• Rasterize into housing unit density
COSTALLOCAT ION
GRIDAllo catio n
GRIDDis ta nce
GRID Co stBack link
ZST AT houunits fo r e a ch
a llo ca tio n
DBF co s t suma llo c zo nes
JOIN
LAYER fac il i tie sjo in 1
MFL 1
LAYERse lec tio n
ZST ATdis tma sk
ve ctor a lloc
DBF Allo cZone zs ta t
JOIN vec to rzs tat
LAYERfa c il i tie s
COPYFEAT URES 2
FEAT UR ES SelFa c il i ties A lloc
SOMAExc lude
Build ing s
GRIDd is tmask
Ra ster toPo lyg on
FEAT URESAllo catio n
COPY
GR IDd istOut
SELECTMod e ledFac il itie s
FEAT UR ESSe le cte d
SQL Se le c tion o fFac il ie s by ID
MFL 2
LAYERfa c il i tie s
ZST ATc itywid e
DBF Citywid ezs ta t
FEAT URESUnive rse o f
Fac il i tie s
SOMAremo ve b ld gs
GRID CostSurfa ce
FEAT URESUniverse o fBuild ings
T EST dis t > 1mi
GRID outs id e1 mi
ZST AT ho uunits o utsid e1 mi p er a llo c
DBF o uts id e 1mi a llo c zo ne
MFL 3
LAYER fa c il i tiesjo in 4
ZST AT ho uunits outs id e1 mi c itywid e
DBF Allo cZone zs ta t
SOMABo o lea n
Bld gs
GRID B ldgFo otp rints
Ma p Alg eb raExp re ss ion
GRID ho us ing unitd ens ity
GRIDBarriers
GRIDco nstant
COPYSe lec tio n
FEAT URESSele c te d
Summa rySta tis tics (2)
DBFsumma ry o f
JOIN HOA
LAYERfa c il i tie s
COPYFEAT U RES 3
FEAT URESfa c il i tie s jo ine d
SummarySta tis tics
D BFsumma ry
MFL 4
LAYER fa c il i tie sjo ined to a llo c
Medical Distribution Centers Model
The optimization
• How does the optimization work? – It starts with a 40-facility universe of potential sites for
use as Emergency Medical Distribution Centers. To select the optimal number and configuration of these sites, we developed a model to iterate through siting alternatives and successively drop the lowest performer.
• What makes one configuration of Emergency Medical Distribution Centers better than another?– We assess the differences and optimize based on
four metrics
Medical Distribution Centers Model
Metrics
• (m4) Percentage of households outsidemaximum walking distance (1 mile) to the nearest site (ensures centers are located where the people are)
• (m3) Mean Walking Distance from any given location in the city to the nearest facility
• (m2) Evenness of the Population Allocated to each site (assuming individuals will tend to walk to the closest facility)
• (m1) Aggregate Landmark Quality of the selected sites (e.g., a neighborhood school is more readily located than a church)
Medical Distribution Centers Model
Key Assumptions
• Barriers to movement on foot include physical impediments such as fences, buildings, and water, and social boundaries such as private residential property lines
• Individuals will tend to walk freely over all other unfenced property, private or public
• Underpasses and overpasses provide the only bypasses for pedestrian access through major highways
Medical Distribution Centers Model
Results
• Results
Mean Walking Distance (ft)
1000
2000
3000
4000
5000
6000
7000
8000
051015202530354045
No. of Facilities
% Households outside 1 mi Walking Distance from Selected Facility
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
051015202530354045No. of Facilities
Medical Distribution Centers Model
Results
• Metrics – Before and After optimization– Baseline = “schools only” scenario
Landmark Quality(ave. landmark rank*)
1
2.35
0
0.5
1
1.5
2
2.5
Schools Optimized
Allocation Evenness (hhld std. dev)
2404
1562
0
500
1000
1500
2000
2500
3000
Schools Optimized
% Households outside 1 mi
6.51%
0.30%
0%
1%
2%
3%
4%
5%
6%
7%
Schools Optimized
Mean Walking Distance (ft)
3231
2678
0
500
1000
1500
2000
2500
3000
3500
Schools Optimized
(m4)(m3)
(m2)
(m1)
Medical Distribution Centers Model
Results by Iteration
Mean Walking Distance (ft)
1000
2000
3000
4000
5000
6000
7000
8000
051015202530354045
No. of Facilities
% Households outside 1 mi Walking Distance from Selected Facility
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
50%
051015202530354045No. of Facilities
(m4) (m3)
Medical Distribution Centers Model
Arlington’s Medication Model-Overview
•Based on the Alexandria Model•Model Scenario from the County’s Health
Planner and the CDC City Readiness Initiative •Initially Two Models: 1 mile and 1½ mile walking
distance•Model relied heavily on Human Input
Medical Distribution Centers Model
Arlington Project Scenario
• Emergency Centers– Medication Centers (MC)
• Deliver medicine in first 48 hours• Medication Center’s should be less than a 1½ mile walk for Head
of House Hold one way
• Medication Center Staffing– ~20 staff/MC– Estimated 1 Head of House Hold Processed, from start to finish,
in 5 Minutes• Phase Approach for Opening MC’s
– Two Phases (Phase 1: 1½ Miles Model; Phase 2: 1 Mile Model)– Phase 1 only covered in this presentation
• Arlington Demographics– 2000 Census: 86,352 House Holds (HH)– 2008 Estimates: 96,069 House Holds (HH)
Medical Distribution Centers Model
Medication Center Selection Criteria
• Medication Centers– Elementary School only model would not provide the
coverage that is needed.– Medication Centers were selected primarily by the County’s
Health Planner-• Community Centers were identified as prime locations due to the
fact that they are County Property and there is no need for a legal agreement between the County and the Owner of the facility.
• Elementary Schools were also identified as prime locations sincethey are also County Property, but they hold certain restrictions to the use of the building, and thus, they are secondary to Community Centers.
• Polling Places were considered as possible Medication Centers, but due to the fact that Arlington County does not own all the Polling Places in the county could make it difficult to open thefacility in an medical emergency event.
Medical Distribution Centers Model
Arlington Tools & Inputs Arlington
• Tools– ArcGIS Model Builder– ArcGIS Spatial Analyst– ArcGIS for Cartographic Products
• Inputs– Vector Point Data
• Point Locations of Potential Medication Centers
– Community Centers, Elementary Schools, and Voting Locations
– Raster Surface• Boolean Raster representing Open Space
and Barriers – Barriers were Represented as Buildings, Divided
Highways, Single Family Parcels, Federally Owned Land, State Owned Land, Water Features, and Railroad/Metro Tracks
– Household Data• An Estimate of how many households would
be served in each Medication Center• Based on Census 2000 data and Estimated
Demography data for 2008
Co n
barop t03a lta
Input trueraste r o r
Input fa lseras te r o r
ba rrie rs(2)
Co stAlloc a tion
AlloOp t3a lta
Dis tOp t03Al ta
Back Op t03a l ta
QDC_Location_Op t3_
Sing le OutputMap A lgeb ra
DsMs kOpt3Aa
T e st
D is tOut1_5MAa
Zona lSta tis tics as
T ab le
Allo c_Zone_Sta t_1_
Raste r toPo lyg on
Alloca tion_Area sOp t
Add Fie ld
Alloca tion_Area sOp t
Ca lcula teFie ld
Alloca tion_Area sOp t
Po lygo n toRaste r
HHDe nsityAl t
Census HH_Data_200
Zona lSta tis tics a s
T a b le (2)
Op t3_ZStatAlta
back g round
Zona lSta tis tics as
T ab le (3)
Cost_Sum_Alloc_Zo
Make Fea tureLa ye r
QDC_Location_Op t3_
Add Jo in
QDC_Location_Op t3_Lay e r (2)
Add Fie ld (2)
QDC_Location_Op t3
Ca lcula teFie ld (2)
QDC_Location_Op t3
Zo na lSta tis tics as
T ab le (4)
T b l_A lloc_Zone _ZSt
Zo na lSta tis tics as
T ab le (5)
Zona lSt_Alloca t1_Op t
Add J o in (2)
QDC_Location_Op t3_
Medical Distribution Centers Model
Arlington Model Differences
• Arlington County Medication Center Model– Arlington County’s Model is based on the Model
created by Alexandria– Major differences are the method of which we
selected our Medication Centers.• Arlington relied heavily on Human Input for the selection of
the Medication Center that would be used (Alexandria relied on a large collection of sites and used iteration to select Medication Centers)
• Arlington’s physical landscape is different from Alexandria’s, and thus, created a barrier to use the original Model from Alexandria
– Large number of parcels in the County are Zoned for Single Family Residential in the Northern Arlington, and Multiple Family Residential (i.e. Condos and Apartment Buildings)
Medical Distribution Centers Model
Arlington Model ResultsAverage & Maximum Walking Distance per QDC Phase 1A
Max
imum
Dis
tanc
e, 7
,457
Max
imum
Dis
tanc
e, 7
,482
Max
imum
Dis
tanc
e, 8
,635
Max
imum
Dis
tanc
e, 8
,174
Max
imum
Dis
tanc
e, 4
,724
Max
imum
Dis
tanc
e, 8
,222
Max
imum
Dis
tanc
e, 7
,272
Max
imum
Dis
tanc
e, 5
,924
Max
imum
Dis
tanc
e, 9
,465
Max
imum
Dis
tanc
e, 7
,218
Max
imum
Dis
tanc
e, 7
,294
Max
imum
Dis
tanc
e, 6
,449
Max
imum
Dis
tanc
e, 7
,953
Ave
rage
, 3,3
52
Ave
rage
, 3,1
89
Ave
rage
, 3,1
78
Ave
rage
, 4,0
19
Ave
rage
, 1,9
14
Ave
rage
, 3,6
98
Ave
rage
, 3,3
33
Ave
rage
, 2,8
59
Ave
rage
, 4,1
54
Ave
rage
, 2,8
70
Ave
rage
, 4,0
66
Ave
rage
, 2,9
73
Ave
rage
, 3,7
36
0
1,000
2,000
3,000
4,000
5,000
6,000
7,000
8,000
9,000
10,000
Mad
ison
Com
mun
ityC
ente
r
Auro
ra H
illsC
omm
unity
Cen
ter
Wal
ter R
eed
Com
mun
ity C
ente
r
Swan
son
Mid
dle
Scho
ol
Fire
Sta
tion
10
Barr
ett E
lem
enta
rySc
hool
Key
Elem
enta
rySc
hool
Long
Bra
nch
Elem
enta
ry S
choo
l
Not
tingh
amEl
emen
tary
Sch
ool
Oak
ridge
Elem
enta
ry S
choo
l
Tayl
or E
lem
enta
rySc
hool
Abin
gdon
Elem
enta
ry S
choo
l
Barc
roft
Elem
enta
rySc
hool
QDC Location
Wal
king
Dis
tanc
e (f
eet)
Medical Distribution Centers Model
Arlington Model Results
Total House Holds Served (2008) per QDC Phase 1A2,
026
10,8
31
8,09
7
6,97
9
7,52
9
14,4
66
11,5
79
4,69
4
4,72
9
3,24
6 5,21
9 7,81
4
8,85
8
0
2,000
4,000
6,000
8,000
10,000
12,000
14,000
16,000
Mad
ison
Com
mun
ityC
ente
r
Auro
ra H
illsC
omm
unity
Cen
ter
Wal
ter R
eed
Com
mun
ity C
ente
r
Swan
son
Mid
dle
Scho
ol
Fire
Sta
tion
10
Barr
ett E
lem
enta
rySc
hool
Key
Elem
enta
rySc
hool
Long
Bra
nch
Elem
enta
ry S
choo
l
Not
tingh
amEl
emen
tary
Sch
ool
Oak
ridge
Elem
enta
ry S
choo
l
Tayl
or E
lem
enta
rySc
hool
Abin
gdon
Elem
enta
ry S
choo
l
Barc
roft
Elem
enta
rySc
hool
QDC Location
Hou
se H
olds
Ser
ved
Medical Distribution Centers Model
Arlington Model Results
Distance from QDCdistance in feet
0 - 984
985 - 1,771
1,772 - 2,509
2,510 - 3,198
3,199 - 3,887
3,888 - 4,576
4,577 - 5,265
5,266 - 5,904
5,905 - 6,495
6,496 - 7,134
7,135 - 7,920
7,921 - 12,547
Medical Distribution Centers Model
Key Similarities and Differences
• Similarities– Both adopted essentially the same raster cost
allocation model, built in ModelBuilder– Both used an extensive and detailed
cadastral/planimetric database to derive areas accessible by walking
• Differences– Alexandria identified a large universe of sites and
used model iteration to select an “optimal”distribution of sites
– Arlington used local knowledge and human inputs to identify sites and evaluate site distribution
Medical Distribution Centers Model
Model into Reality
• With many geospatial analysis projects, we rarely get the opportunity to witness their model being implemented in the real world.
• This coming Fall, Arlington County and the City of Alexandria will be conducting a joint cross jurisdictional public health exercise to test the validity of the Medication Center Models.
• The participants of this joint exercise will be asked to fill out a survey to identify certain key questions, such as:– The Beginning Location of their trip– Did they walk or utilize public transportation– Route taken to reach medication center– Was this an easy trip to make– Was the center easily found
• With the Survey we will be able to better model the real world in our GIS Models for the Future.
Medical Distribution Centers Model
Lessons Learned so Far
• For best optimization, identify a large universe of potential sites (but don’t forget that each site adds hours of run time)
• Start with good data (e.g., spatially explicit population data)
• Make performance a key concern – changing scenarios ideally should not induce days of computer crunching
• Gather literature to backup key assumptions
Medical Distribution Centers Model
Future Developments
• Update population data (2000 Census does not capture some of our new and growing population centers)
• Test the sensitivity of model assumptions to metric weighting and review the process– Performance is a big concern
• Refine assumptions on walking behavior through field testing and literature review– The “perceptual” component is difficult to capture
• Incorporate terrain and/or barrier gradient into the cost allocation analysis
Medical Distribution Centers Model
How is this being applied?
• Sometimes GIS people don’t get to see how their work is applied
• This fall, there is going to be an exercise to apply and test the selected sites