Urinary tract infection (UTI):
-
Upload
nissim-franklin -
Category
Documents
-
view
51 -
download
0
description
Transcript of Urinary tract infection (UTI):
Urinary tract infection (UTI):
Urinary tract infection (UTI) can be divided into the following:
1- Upper UTI: Pyelonephritis and Ureteritis.
2- Lower UTI: Cystitis, Urethritis, and Prostatitis in men.
Urinary tract infection is more common in females due to the following factors:
1-The short urethra, and proximity of the urethral opening to the anus.
2-Lack of antibacterial prostatic secretions.
3-Facilitation of bacterial migration by sexual intercourse.
Other risk factors for UTI:
1- Poor personal hygiene.
2-The insertion of contaminated catheters.
Physical and chemical barriers that protect human urinary tracts:
Human urinary tracts are protected from infectious microbes by :1-The frequent flushing action of urination.
2- The acidity of urine ( pH from 4.5 to 8 ).
3- The prostatic secretions (lysozyme and IgA).
Factors that play a role in establishment of UTI:
1-The microbial virulence.
2-The pathogenic dose.
3-The antibiotic resistance ability (Hospital-dwelling bacteria).
4-The immune system (weakness of Humoral immunity in urinary
tracts).
Pyelonephritis:
Pyelonephritis: (Pyelum: Renal pelvis, Nephro: kidney) : is an urinary tract infection that has reached the pelvis of the kidney. Severe cases of pyelonephritis leads to pyonephrosis (accumulation of Pus in kidney pelvis).
Etiology of Pyelonephritis: 1- Escherichia coli. 2- Staphylococcus saprophyticus.
3- Other genera of Enterobacteriaceae : Klebsiella, Enterobacter, Proteus, and Serratia.
4- Pseudomonas aeruginosa ( Hospital-acquired infection).5- Enterococcus faecalis ( Hospital-acquired infection).
a
Escherichia coli: E.coli:- The most common cause of UTI ( 70-95%).- Complicated UTI (Pyelonephritis) mainly caused by nonuropathogenic strains of E.coli.- Source of bacteria: Fecal contamination.
Staphylococcus saprophyticus: - It considered as a second causative agent of UTI (5-20%). - Frequent cause of urinary bladder infection in female due to its occurrence as part of normal vaginal flora.
Others microbes : Enterobacteriaceae: -Species of Enterobacteriaceae form the other percentage of infection.
Microbial Pathogenesis :
Pyelonephritis is established according to the following arranged Consequences: 1-The bacterial lower urinary tract infection.2-PMNs influx from lower urinary bladder to ureter and kidney. 3-Reflux of infected urine up the ureters into the renal pelvis due to: A-Congenital abnormality ( short intravesical ureter). B- Obstruction of ureters ( ureter stone or carcinoma).- If PMN cell proliferation occurs in Renal Pelvis; Pyelonephritis will be established.
n
3- Bacterial entry through the papillae into the renal parenchyma. 4- adhesion of microbes to interstitial tissue surrounding the tubules in kidney medulla. 5- Activation of PMN cells, infiltration of interstitial tissue by B, and T -lymphocytes, and eosinophils, proliferation of cells, inflammation .6- Tubulointerstitial nephritis.
Tubulointerstitial nephritis ( TIN):Types:1-Acute TIN: - involves an inflammatory infiltrate and edema affecting the renal interstitium that often develops over days to months. - Over 95% of cases result from infection or an allergic drug reaction.
- interstitium abscesses : necrosis contains neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils). -Tubules are damaged by exudate and may contain neutrophil casts. - In the early stages, the glomerulus and vessels are normal.
n
2- Chronic TIN: - Gradual interstitial infiltration and fibrosis, tubular atrophy and dysfunction, and a gradual deterioration of renal function, usually over years. - Glomerular involvement is much more common in CTIN than in ATIN. - Causes: immunologically mediated disorders, infections, obstructive nephropathy, and drug interaction.
-A perinephric abscess (infection around the kidney) and/or pyonephrosis may be developed in chronic pyelonephritis (chronic TIN).
n
Chronic TIN:
Normal, and Destroyed Glomeruli with cellular infiltration.
Fibrosis, cellular infiltration, tubules could be absent or atrophied.
Signs and Symptoms of Pyelonephritis:
The symptoms of acute bacterial pyelonephritis are summarized as :1- High fever ( Pyrogenic infection) , flank pain, and pain in the joints and muscles including flank pain.
2- Burning sensation during urination (dysuria: Difficult and painful urination) , and increased frequency of urination (polyuria).
3- Pyuria (pus in urine; pyogenic infection).
4- As the kidney becomes more inflamed, pain, loss of appetite, and headache could be present.
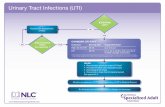
Diagnosis of Urinary tract infection:
Urine analysis:1- Physical properties: -Appearance: turbidity or milky: suggested pus in urine or others. -Color: white color: Pus in urine: Pyuria :infection?
Red color: RBCs in urine: (Hematuria): kidney stones, infections , or tumors?
n
2-Chemical properties: -Glucose in urine: (Glycosuria) : In Diabetes mellitus patients. : considered as a risk factor for bacterial infection; because bacteria utilize glucose during binary fission. -Nitrite in urine: (Nitrituria): : indicates the presence of Coliform bacteria in urine. : Note: Enterobacteriaceae species reduce Nitrate to Nitrite.
n
Protein in urine: Proteinuria: Albuminuria: - In Pyelonephritis, and lower UTI: Proteinuria (trace from pus or bacterial origin) and Pyuria. - In interstitial nephritis and Glomerulonephritis: Proteinuria , Hematuria, lower number of Pus in urine.
3-Microscopic properties: -WBCs: Normal : 2-3 /HPF. -RBCs: Normal : 3-4 cells/HPF. - Casts: A- Granular and fatty cast: in tubulointerstitial nephritis, glomerular disease.
B- Hemoglobin and RBCs cast: Acute Glomerulonephritis due to immune system response. C- WBCs cast: acute pyelonephritis, acute tubulointerstitial nephritis due to infection.
Glomerulonephritis: GN:GN: is the inflammation of the Glomeruli of the nephron. Causes:1- Insoluble antigen: trapped in the glomerulus; antibodies attack the structural components of the kidney and antigen.
2- Soluble antigen: in blood stream: antibodies react with soluble antigen: Immune- complexes formation: precipitation in glomeruli. Both antigen-antibodies reactions cause GN or TIN.
Types of soluble antigen:
1- Exogenous: A-Drugs, toxoid, or serum. B-Infectious agent antigen: - Post-Streptococcal glomerulonephritis: Anti-Streptolysin-O- Ag complexes. -Other infections: Bacterial: Staphylococci, Streptococcus pneumoniae, Klebsella, Yersinia enterocolitica, Treponema, Salmonella. Parasites: Malaria, Schistosoma, and Toxoplasma. Viral : Hepatitis, and E.B.V. Fungal: Candidiasis. 2- Endogenous: Self antigen.





















![7 Catheter-associated Urinary Tract Infection (CAUTI) · UTI Urinary Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-Associated Urinary Tract](https://static.fdocuments.in/doc/165x107/5c40b88393f3c338af353b7f/7-catheter-associated-urinary-tract-infection-cauti-uti-urinary-tract-infection.jpg)