Typhoid fever
-
Upload
kivanc-kayhan -
Category
Health & Medicine
-
view
115 -
download
0
Transcript of Typhoid fever
• Antigenic structure of Salmonella
H( flagella ) antigens
O (somatic) antigens
Vi (Virulence) capsular
polysaccharide antigens
• Salmonella Typhi %90 or Salmonella paratyphi.
>Transmitted through the ingestion of food or drink(ice cream, shellfish) contaminated by the feces or urine of infected people,
>contact with an acute case of typhoid fever, Contact with a chronic asymptomatic carrier.
>The bacterium can withstand both drying and refrigeration.
>Salmonella bacteria can survive for days in groundwater or seawater and for months in contaminated eggs and frozen oysters
>The infectious dose varies between 103-106 organisms given orally
• Refrigeration and freezing could slow their growth.
• Pasteurizing and food irradiation kill Salmonella for commercially-produced food stuffs
• carry the bacteria in their bloodstream and intestinal tract>Symptoms usually develop 1–2 weeks(3-60 days) after exposure, and may be mild or severe. >H.pylori + patients are more susceptible
FIRST WEEK:
•Prolonged High fever (39.4 or 40 C) at least 3 days
•Malaise
•Headache
•Dry bronchitic cough
•Constipation (adults) or diarrhea (children)
•Rose-colored spots on the chest, abdomen, back (exanthema) appears with fever
•Enlarged spleen and liver
Ingestion of contaminated food or water, multiplies in lamina propria than passes to mesentheric Lymph nodes, than to bloodstream causes bacteremia
Salmonella typhi
Carried by white blood cells into the liver, spleen, and bone marrow
Multiply and reenter the bloodstream (Clinical illness)
Bacteria invade the gallbladder, biliary system, and the lymphatic tissue of the bowel and multiply in high numbers
Then pass into the intestinal tract (can be identified for diagnosis in cultures from the stool)
Typhoid ulcers can cause perforation and hemorrhage
How does the bacteria cause disease ?
SECOND WEEK:
• Continuing high fever
• Either diarrhea that has the color and consistency of pea soup, or severe constipation
• Considerable weight loss
• Extremely distended abdomen
THIRD WEEK:
• Lie motionless and exhausted with your eyes half-closed in what's known as the typhoid state
FOURTH WEEK:
• Improvement starts to seen
• Fever is likely to decrease, returns to normal in another week
• Intestinal bleeding or perforation(mostly last 20 cm segment of ileum, 2 or more) — may develop in the third week of illness. Sudden pain in lower right abdominal
• Shock, followed by the appearance of blood in your stool, severe abdominal pain, nausea, vomiting , %20 occult blood in stool, %3 melena
• %90 non-comp, %10 complicated (bloody stool, perforation)
• by week 5, recovered
• In the following 8 weeks, relapse in 5-10%
• %1-5 of cases stays as chronic(after one year of treatment having still positive urine or stool culture) carrier, stays in gall bladder.
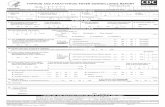
DIAGNOSIS: Leukopenia(leukocytosis is rare: bowel perforation)
• Left shift, Decreased eosinophils or absence of eosinophils, Mild inc. liverenzymes
>Body fluid or tissue culture - small sample of blood, stool, urine or bonemarrow(GOLD st.) ,
Blood cultures (60%-70%) Stools cultures (30%-70%) Bone marrow (75%-95%)
WIDAL test: Detection anti O and H antibodies in serum, not Vi antibodies!! 1 st week negative. Titers raise in 2nd week
• Carriers of typhoid bacilli possess antibody against the Vi antigen of S. typhi. (Vi tires seem to correlate better with the carrier state )
TREATMENT: Drinking fluids. This helps prevent the dehydration that results from a prolonged fever and diarrheaTEACH:
• Explain causes of salmonella infection
• Show the patient proper hand washing techniques
• Tell patient to cook foods thoroughly & refrigerate promptly
• Avoid cross-contamination of food
• Wash fruits & vegetables thoroughly
boil for one minute before drinking it.
Ask for drinks without ice, unless the ice is made from bottled or boiled water. Avoid Popsicles and flavored ices.
Eat food that have been thoroughly cooked and that are still hot and steaming.
Avoid raw vegetables and food that cannot be peeled like lettuce.
When eat raw fruit and vegetables that can be peeled, peel yourself. Don’t eat the peelings.
Avoid foods and beverages from street vendors.
• enteric fever was endemic in Western Europe and North America and that rates decreased in parallel with the introduction of treatment of municipal water, pasteurization of dairy products, and the exclusion of human feces from food production
• The identification and treatment of S. Typhi carriers, particularly those involved with food production, has proven to be an important strategy for the control of typhoid fever in low-incidence settings.
• The disadvantages of using chloramphenicol include a relatively high rate of relapse (57%), long treatment courses (14 days) and the frequent development of a carrier state in adults.
• BEST TX is cipro, for pregnants use azitro, cefixime, ceftriaxone
• TMP-SMZ as effective as chloramphenicol in defervescenceand relapse rate.
• Patients treated adequately during the first week produced mortality reduction to zero and complications were infrequent
• Chronic carrier: asympt patient with pos stool, TMP-SMZ effective %60, 281-6 weeks. Cipro is effective %80, 2*750-4 weeks
• REASONS FOR THE USE OF QUINOLONES IN THE TREATMENT OF TYPHOID FEVER
• High rate of cure (>95%)
• • Early negative faecal excretion to Salmonella
• • Decrease in the relapse rate (near to 0% in most studies)
• • Avoid transitory and chronic S. typhi carriers
• Reduction of chronic carriage
• • Few side effects and good tolerance (only 2 tabs/day)
• Reduction of the treatment time to 10 days (even 7 days)
• A COMPARATIVE STUDY OF OFLOXACIN AND CEFIXIME IN CHILDREN
• • Ofloxacin (n=38) 10mg/kg/day x 5 days, or
• Cefixime (n=44) 20mg/kg/day x 7 days
• • Fever clearance: Ofloxacin 4.4 days
• Cefixime 8.5 days p<0.0001
• • Failure: Ofloxacin 1 case (no relapse)
• Cefixime 10 cases (1 relapse)
VACCINE
• a) an oral live-attenuated vaccine (Vivotif Berna vaccine, manufactured from the Ty21a strain of Salmonella typhi (2 ) by the Swiss Serum and Vaccine Institute); 3 DOSES FOR 5 YEARS %33-66
• b) a parenteral heat-phenol-inactivated vaccine that has been widely used for many years (Typhoid Vaccine, manufactured by Wyeth-Ayerst);
• c) a newly licensed capsular polysaccharide vaccine for parenteral use (Typhim Vi, manufactured by Pasteur Mérieux).
• fourth vaccine, an acetone-inactivated parenteral vaccine, is currently available only to the armed forces.
Misdiagnosis
• Paratyphoid fever- similar to typhoid fever but usually less severe.
• Paraenteric fever- a typhoid-like fever but not caused by Salmonella.
• Gastroenteritis- mild case of typhoid fever may be mistaken for gastroenteritis.
• Typhomalarial fever
• Brucellosis
• Tuberculosis
• Infective endocarditis
• Q fever
• Rickettsial infections
• Acute diarrhea (type of Diarrhea)
• Viral Hepatitis
• Lymphoma
• Adult Still's disease
• Malaria
Some common home remedies
• Take two grains of Un nab, Munnakka 4, Kuhbkalan 3 gm's. and Misri 10 gm's. grind all of them and mix in 100 ml. of water, preferably boiled and cooled. Strain the water and make the patient drink at four hourly interval.
• Take 4 basil leaves, saffron 7 shreds, 7 grains of black pepper. Grind them to a paste by adding water and form small tablets out of the whole lot. Take each tablet twice or thrice everyday with lukewarm milk. The fever would also subside and the patient would get the desired relief.
• 1 to 2 teaspoons of fresh juice of coriander leaves mixed in 1 cup buttermilk and taken 2-3 times a day.
• Mash a ripe banana along with 1 tablespoon honey and eat twice a day for a few days.
INFECTIOUS DIARRHEA
• Second leading cause of death in children under five years old
• Kills 1.5 million children every year (WHO)
• Leading cause of malnutrition in children under five years old (WHO)
• Kills 5-10 million people/year (WHO)
• Bacterial infections– through contaminated food or water; Campylobacter,
Salmonella, Shigella, Clostridium dificile and Escherichia coli (E. coli)
• Viral infections – including rotavirus, norovirus, cytomegalovirus, herpes simplex
virus, and viral hepatitis– Infection with the rotavirus is the most common cause of acute
diarrhea in children.
• Parasites – Parasites that cause diarrhea include Giardia lamblia,
Entamoeba histolytica, and Cryptosporidium
• Intestinal diseases• Inflammatory bowel disease, ulcerative colitis, Crohn’s disease,
and celiac disease• Food intolerances and sensitivities such as lactose, wheat