Tx: Half the deficit over the first 24 hours, then the ... · (10/19) Kim Lecture: Sodium Disorders...
Transcript of Tx: Half the deficit over the first 24 hours, then the ... · (10/19) Kim Lecture: Sodium Disorders...

§ Tx: Half the deficit over the first 24 hours, then the remainder over the next 24-72h o Goal: Maintain Urine Output 0.5-1mL/kg/hour. In replacement therapy, we do care about SNa, so if
hypernatremic, lets give D5W - Maintenance: [Looking at the future] Performed over a 24 hour period, and dosing is based on body weight (kg)
o Dx: Dehydration: Would give 45mL/kg/day, Dx: Euvolemia: Would give 35mL/kg/day - AE: Volume overload is common if infusion is not properly monitored
o à Monitor: Weight, SNa, Osmolarity, Physical Exams, Urine Output o ADR: Pulmonary edema (hear lungs crackling), peripheral edema, hyponatremia
Tx of Hypervolemia - Diuresis: Use loop diuretics (Furosemide), Aquaretic (Vasopressin Receptor Antagonists)
o Using a Loop? Monitor sodium, eyeball that hyponatremia. Aquaretic? No fear, doesn’t affect it - Dialysis: If the Kidneys are completely fried, do dialysis. But as we’ve learned, try to avoid this
o Emergent Dialysis: Indications? Toxicity, Hyperkalemia, Fluid Overload - AE: Dehydration, AKI, Hypotension, Hypernatremia
o à Monitor: Weight, labs (BUN/SCr), physical exam, urine output, vital signs (10/19) Kim Lecture: Sodium Disorders Sodium: The most abundant extracellular cation that helps redistribute water. It helps with neuromuscular functioning and plays a role in acid-base balance. Critical for Kidney function.
- Distribution: Very similar to water, 60-150mEq in addition to the intestinal secretions that are in homeostatic balance with the ECF, ICF, and Bone depots. Na cannot readily cross plasma membranes, pumps maintain the electrogradient. Na freely crosses PlasmaßàISF
- Excretion: Feces (10mEq), Renal (60-150mEq), Insensible (10mEq)
- Homeostasis: As we previously learned, the Kidney developed to help us retain sodium before the Big Mac. In the Nephron, 60-70% reabsorbed by proximal, 20-25% in Ascending Loop of Henle, 5-10% distal, and the remainder, a very small amount, in collecting duct as modulated by Aldosterone. [Goal: 135-145mEq/L]
Hyponatremia: (<135mEq/L), Symptoms worsen as ßNa - Sx: Mild cases may notice nausea and malaise, but it is
not until Moderate (~120) that headache, lethargy, restlessness, and disorientation become common. Severe deficiencies (<110) are characterized by seizure, coma, brain damage, and potentially death.
- Adaptation: The brain will adapt to chronic hyponatremia. Normally a tight regulator of all the ins and outs, it must release Na to address the excessive attraction of water. It will transport NaCl, K, and organic solutes (Glu, Taurine, Gln) extraceulluarly. As a result, Brain Osmolality ß, inducing water loss [Happens over hours/days]
- Specific Diagnosis: Hyponatremia (<135mEq/L) may be concomitant with Low, Iso, or High Osmolality General Tx of Hyponatremia Note: Electrolyte disorder is not a primary disorder, tx, then find underlying dx
- Acute/Severe: à Slam ‘em with hypertonic saline (3%). Moves sodium up fast with a lesser amount of fluid o Monitor every 2-4 hours, Once stable, find underlying etiology
- Other: NS. The 0.9% infusate has 154mEq/L, thus may not be too therapeutic to raise hyponatremia, compared to the 3% NaCl having 513. Find out how much of X you’ll need: DSNa/1L infusate = (InfusateNa-SNa)/(TBW+1)
- MAXIMUMS: 8mEq/L/24h is the max increase in serum sodium for a 24 hour period o Acute: Correct at 1-2mEq/L/hour (preferably 1mEq) for the first 48 hours in severe cases o Chronic: Correct at 0.5mEq/L/hour for time periods longer than 48 hours.
- Goal: 130mEq/L Dx: Hypervolemic Hypotonic Hyponatremia –ECFÝ. Low Na & Low osmolarity? What’s going on! [TBWÝÝ, TBNaÝ]
- Cx: Hypervolemia (ÝECF) often due to CHF, Nephrotic Syndrome, Liver Failure, & Acute/Chronic Renal failure o Decreased ability to eliminate fluids will cause a hypotonic environment, only because TBWÝmore>Na
- Tx: Regardless of the severity of the case, the goal will be to decrease the TBW o Mild/Moderate: Restrict Sodium Intake. If the patient is stable and there are no lung symptoms, perhaps
just some leg edema, this should work. It will take days to show improvement

o Severe: Diuretic – Furosemide. If the patient is unstable. Will need to monitor sodium lab values § If sodium begins to dip, may need sodium supplementation
- AE: Furosemide is a sodium reabsorption inhibitor, so our sodium levels will likely go down Dx: Euvolemic Hypotonic Hyponatremia - ECF remains ~neutral, what causes Na to leave? [TBWsmallÝ, TBNa~]
- Cx: Hypothyroidism, Addison’s Disease, Excessive and Inappropriate ADH effects (SIADH) o ADH/AVP/Vasopressin will promote solute-free water reabsorption in the collecting ductà relative Na ß o Causes of SIADH? Often severe nausea and pain, CNS disorder, lung malignancy, Meds: Haldol, TCA,
SSRI, Carbamazepine, Desmopressin. o Treatment of Chronic SIADH: Demeclocycline is the preferred drug, inhibiting renal response to ADH
- Tx: Treatment options depend on the severity of the condition and the symptoms present o Mild/Moderate: Fluid Restriction. If symptomatic – use an Aquaretic/Diuretic o Severe Sx: Furosemide + Hypertonic Solution (3%)
Dx: Hypovolemic Hypotonic Hyponatremia - ECFß. Now we have Sodium AND water loss, how? [TBWß, TBNaßß] - Cx: Renal: Excess Diuretic Use, Cerebral salt wasting, adrenal insuff, Non-renal: Bleeding, barfing, on-fire - Tx: D/C the offending diuretic. Improvement? Good. Still Symptomatic? à NaCl dosing (3-4xdaily). AE of
NaCl may be nausea, which we know to increase ADH release causing further diuresis. daaaaaaaaamn o Severe Cases: 3% NaCl
SPECIAL Cases of Hyponatremia - Dx: Central Pontine Myelinolysis (CPM); “Osmotic Demyelination”, first described by Adams in 1959, boozers
o Patho: Characterized by loss of oligodendrocytes and myelin in the pons/pontine (part of brainstem). This can occur when chronic cerebral adaptation to hyponatremia is exposed to a hypertonic fluid, sucking water from the brain and inducing demyelination
o Cx: Severe Hypo (<120mEq/L), Chronic Hypo (>48 hours), Excessive Hypo Correction (>12mEq/L/day) o At Risk Populations: Hepatic Fever, Hypokalemia, Malnutrition
- Dx: Hypertonic Hyponatremia- It’s not all sodium’s fault! o Cx: Hypertonicity is often related to Hyperglycemia or the use of mannitol. This is an exaggerated effect
§ Every 100mg/dL Serum Glucose = ß 1.7mEq/L of Na - Dx: “Pseudohyponatremia” Isotonic Hyponatremia- This can happen! But incredibly rare
o Cx: Hyperlipidemia and Hyperproteinuria DRUG CLASS: Aquaretics/ADH Inhibitors: Also referred to as –vaptans or Vasopressin Receptor Antagonists
- While this drug class may have 4 names to describe it, there are only 2 drugs that are available. Including: o Conivaptan (Vaprisol), and Tolvaptan (Samsca)
- MoA: Potent class of compounds that promote free water loss. Therefore, they do not lead to hyponatremia - AE: Hypotension is the main concern, even at low doses
Hypernatremia - Sx: Clinical manifestations increase at higher Na. Including muscle weakness, restlessness, N/V, confusion, coma
General Tx of Hypernatremia: Use infusate with [Na] < SNa. The Goal: SNa in Hypernatremia is 150mEq/L - Option 1: Choose an infusate, Calculate how much: DSNa/1L infusate = (InfusateNa-SNa)/(TBW+1) - Option 2: “easier quicker way” – Calculate Free Water Deficit, Replace that with low-Na Infusate
o à ADMINISTER either option 50% in first 24 hours, then the rest in 24 (acute) to 72 (chronic) hours o Deficit = Normal TBW – Current TBW Current TBW = (Goal Na / Actual Na) * nTBW
- Maximums: The Goal SNa = 150mEq/L, with a maximum daily decrease of SNa of 10mEq/L/24 hours o Acute (<48 hours) Severe cases: 1-2mEq/L/hour, with a starting target of 1mEq/L o Chronic (>48 hours) Mild: 0.5mEq/L/hour
- Hypervolemia Hypernatremia: ECFÝ, TBWÝ, TBNaÝÝ o Cx: Commonly Iatrogenic (caused by medical treatment)–like watering the grass and leaving the hose on,
such as using 3% NaCl, Excessive Na ingestion, Antibiotic containing Na, Hypertonic Dialysis § Hyperaldosteronism, and Cushing’s syndrome are some rare causes
o Tx: D/C the offending NaCl or Drug containing Sodium. If it is the dialysate- change the fluid § Use a diuretic to eliminate Na/H2O excess, and replace the free water deficit
- Euvolemia Hypernatremia: ECF~, TBWß, TBNa~ [Recall, TBNa~ usually related to odd ADH activity] o Cx: Renal Loss (Diabetes Insipidus), Non-renal loss (Fever, Hyperventilation) o Diabetes Insipidus: There are two types, each related to odd ADH activity. Central and Nephrogenic
§ CDI: Decreased release of ADH Risk: Brain Damage § NDI: Kidney exhibits decreased responsiveness to ADH Risk: Kidney Damage/problem
o Tx: Options depend on the severity of the condition

§ Mild/Moderate: Replace free water deficit PO or IV (Calculate Free water deficit) § Severe: Bring sodium down fast, replace the free water deficit with 0.45%NaCl/D5W
• CDI? Give Desmopressin or Vasopressin • Kidneys not responding? NDI? Give HCTZ, Amiloride, or Indomethacin
o HCTZ may cause a paradoxical effect of decreased urine output! - Hypovolemia Hypernatremia: ECFß, TBWßß, TBNaß
o Cx: Almost always excess diuresis. Renal (Diuresis, Loop drugs, AKI), Non-Renal (D,V, Sweating) o Monitoring: If there is volume loss, check vitals for a decrease in BP with reflective Tachycardia
§ Hypovolemic shock consists of tachycardia, mental status changes, and lethargy. o Tx: BPß, PÝ? à Slam ‘em with NS wide open, then follow up with replacement
§ Mild/Moderate: Replace free water deficit PO or IV § Severe à Resuscitation, 500-1000mL 0.9% NaCl over 30-60mins § Hypovolemic Shock à Resuscitate 500-1000mL NS over 30-60mins, Replace free water deficit
with 1/2NS or D5W IV SPECIAL Cases of Hypernatremia:
- Cerebral Edema – Hypernatremia’s fabled condition o Sodium acts as the effective solute to pull in more water o A rapid decrease in plasma sodium concentration results in herniation, 3 potential directions
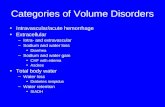
Hyponatremia INDICATION
Hypervolemic Hypotonic Low Osmolarity
Euvolemic Hypotonic ~~Isotonic
Hypovolemic Hypotonic High Osmolarity
LAB PARAMETERS
ECFÝ, TBWÝÝ, TBNaÝ ECF~, TBW~Ý, TBNa~ ECFß, TBWß, TBNaßß
CAUSE (Cx) Often CHF, Nephrotic Syndrome, Liver Failure, Acute/Chronic Renal Failure
Hypothyroidism, Addison’s Disease, Excessive and Inappropriate ADH (SIADH). SIADH may be the result of severe nausea±pain, or med-induced (Carbamazepine, SSRI)
Renal: Excess Diuretic use, Cerebral salt wasting, adrenal insufficiency Non-Renal: Blood loss, Vomiting, Burns
TREATMENT (Tx)
Mild/Moderate: Restrict Sodium intake. Will take days to show improvement Severe: Furosemide/Diuretic. Monitor Sodium lab values. If it begins to dip, may need to supplement Na
Mild/Moderate: Fluid Restriction. Symptomatic: Aquaretic/Diuretic Severe: Furosemide + 3% NaCl Chronic SIADHà Demeclocycline (inhibits renal response to ADH)
D/C the offending diuretic! Symptomatic after d/c? à PO NaCl (3-4xdaily) Severe: 3% NaCl
Comment This condition is related to the reduced ability to eliminate fluids.
In SIADH, ADH/Vasopressin promotes solute-free water reabsorption, causing relative Naß
PO NaCl may induce nausea, look to the left, that may induce SIADH!!
Hypernatremia INDICATION
Hypervolemic
Euvolemic
Hypovolemic
LAB PARAMETERS
ECFÝ, TBWÝ, TBNaÝÝ ECF~, TBWß, TBNa~ ECFß, TBWßß, TBNaß
CAUSE (Cx) Most commonly Iatrogenic – such as excess 3% NaCl use, Excess Na ingestion, Antibiotic-Na, Hypertonic Dialysis Hyperaldosteronism, Cushing’s
Renal: Diabetes Insipidus - CDI: Less ADH - NDI: Kidney doesn’t respond
to ADH Non-Renal: Fever, Hyperventilation
Almost always excess diuresis Renal: Osmotic diuresis, loops, AKI Non-Renal: N, V, Sweat, Fistula, Burn
TREATMENT (Tx)
D/C The offending NaCl! If it is the dialysate - D the fluid Use Diuretic to eliminate Na/H2O AND replace the free water deficit
Mild/Moderate: Replace free water deficit PO or IV Severe: Bring Sodium down fast! 1/2NS/D5W CDI: Desmopressin, Vasopressin NDI: HCTZ, Amiloride, indomet
Mild/Moderate: Replace free water deficit PO or IV Hypovolemic Shock: Resuscitate w/ 500-1000mL NS over 30-60mins, then replace free water deficit w/ 1/2NS or D5W
Comment Volume increase AND Na Increase, so we must be receiving Na!
CDI: Risk of Brain damage NDI: Risk of Kidney Damage
*Whenever there is Volume loss, monitor BP and P for hypovolemic shock