Transcatheter Leadless Cardiac Pacing with Limited Venous ... · leadless cardiac pacemaker; PM =...
Transcript of Transcatheter Leadless Cardiac Pacing with Limited Venous ... · leadless cardiac pacemaker; PM =...

Title Transcatheter Leadless Cardiac Pacing with Limited VenousAccess
Author(s) Lau, CP; Lee, KLF
Citation Pacing and Clinical Electrophysiology, 2016, v. 39 n. 11, p. 1281-1284
Issued Date 2016
URL http://hdl.handle.net/10722/234697
Rights
This is the accepted version of the following article: Pacing andClinical Electrophysiology, 2016, v. 39 n. 11, p. 1281-1284, whichhas been published in final form athttp://onlinelibrary.wiley.com/wol1/doi/10.1111/pace.12895/abstract; This work is licensed under a Creative CommonsAttribution-NonCommercial-NoDerivatives 4.0 InternationalLicense.

PACE pace12895 Dispatch: May 29, 2016 CE: AFL
Journal MSP No. No. of pages: 4 PE: Izzat Ibrahim
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
UNCORRECTEDPROOF
CASE REPORT
Transcatheter Leadless Cardiac Pacing with LimitedVenous AccessCHU-PAK LAU, M.D., F.H.R.S.*,† and KATHY LAI-FUN LEE, M.B.B.S., F.A.C.C.*Q1
From the *Cardiology Division, Department of Medicine, Queen Mary Hospital, the University of Hong Kong, HongKong SAR, China; and †Research Center of Heart, Brain, Hormone and Healthy Ageing, Li Ka Shing Faculty ofMedicine, the University of Hong Kong, Hong Kong SAR, China
Entirely leadless cardiac pacemakers that are delivered transvenously required the use of large diameterdelivery sheath and femoral venous approach. The complexity of external femoral and iliac venousanatomy may limit their implantation. We describe a patient without subclavian venous access and aconventional pacemaker with a failed right ventricular lead, who had difficult iliac venous anatomy thatwas also compressed by an external endovascular abdominal aortic stent. Successful leadless pacing usinga MicraTM (Medtronic Inc) was accomplished with a strong support wire, hydrophilic delivery sheath andguided by venography. (PACE 2016; 00:1–4)
leadless cardiac pacing, heart block, aortic stent graft
IntroductionTranscatheter deployed entirely leadless car-
diac pacemaker (LPM) avoids the complicationsassociated with pacing leads and pacemakerpockets.1,2 Current LPMs require large diametersheaths that are introduced through the femoralveins. There is limited information on theimplantation of LPM in patients with limited ordifficult venous anatomy.
Patient and MethodAn 81-year-old woman with atrial fibrillation
and complete heart block had a DDDR pacemakerimplanted over her left infraclavicular area10 years ago. She had chronic renal failure forQ27 years, and hemodialysis (HD) using arteriove-nous fistulae on either arm, right subclavianand right internal jugular veins failed because oftortuosity and repeated infection. She was finallydialysed from a right femoral HD catheter. In 2010,she developed a leaking infrarenal abdominalaortic aneurysm and underwent an emergencyendovascular repair with aortic stent graft (EVAR:Enduran 26/13/145 + 16/24/80R and 16/24/120L)in the lower abdominal aorta straddling intothe two common iliac arteries. At the time ofpacemaker replacement in 2012, the ventricular
Address for reprints: Chu-Pak Lau, M.D., F.H.R.S., CardiacHealth Heart Centre, The University of Hong Kong, Suite1303, Central Building, 1 Pedder Street, Central, Hong Kong.Fax: 852-21795114; e-mail: [email protected]
Received February 2, 2016; revised May 3, 2016; accepted May17, 2016.
doi: 10.1111/pace.12895
lead had a threshold of 4 V at 0.4 ms. An attemptto introduce a new ventricular lead failed and aBoston Scientific AltruaTM was implanted usingthe original high threshold ventricular lead. Thedevice was programmed at 6.5 mV at 0.9 msand its battery became depleted in 2015. Leadextraction or an epicardial lead placement wasoffered but the patient declined both because ofrisk. A decision was made to use an LPM forpacemaker replacement.
After creation of a subcutaneous purse stringsuture in the left femoral venous site, the commonfemoral vein was punctured and a stiff supportwire was inserted and placed at the level of theright atrium. The support wire had a tortuouscourse in the left common iliac vein (LCIV)and the Medtronic 27F hydrophilic sheath anddilator failed to track across (Fig. 1A). A handinjection cine-angiogram was then performed withmultipurpose catheter tracked over this wire.The injection showed that the whole LCIV wasseverely compressed by the right and left iliacextensions of EVAR, and that the multipurposecatheter was in the lower tortuous patent channel(Fig. 1B). The wire was, therefore, repositioned tothe straighter patent upper channel. The sheathand dilator was then tracked over the wire butwas caught between the left and right commoniliac extensions of the EVAR stent in front, and thepelvic bone behind. Using a series of progressivelylarger dilators, the venous passage was dilated upto 27F size. With gentle but sustained pushingand pulling on the support wire (push and pulltechnique), the venous sheath and dilator finallyachieved a right atrial position, and crossed thetricuspid valve without problem or interference
©2016 Wiley Periodicals, Inc.
PACE, Vol. 00 2016 1

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
UNCORRECTEDPROOF
LAU AND LEE
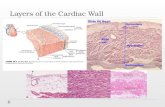
Figure 1. (A) Cine-angiogram in the anteroposterior view of the pelvis showing the placement of a support wirefrom the left femoral vein, through the left common iliac vein (LCIV) into the inferior vena cava. Shown also are theendovascular aortic repair stent graft (EVAR) with its right (R) and left iliac (L) extensions. The MicraTM deploymentsheath could not track over the wire because of venous tortuosity. (B) Hand-injection cine-angiogram in the sameposition using a 5F multipurpose (MP) catheter in the LCIV tracked over the support wire. The LCIV was severelycompressed by the iliac limbs of the EVAR. The MP catheter was in the tortuous lower patent channel of the LCIV,which was pacified with this injection, with its entry into the right common iliac vein (RCIV) and reflux of contrastto the inferior vena cava (IVC). An upper channel of the LCIV has a straighter course (arrows), and the MicraTM
deployment sheath was successfully tracked over the support wire subsequently placed in this channel.
by the right ventricular lead. A Medtronic MicraTM
TCP was then deployed over the sheath in the rightventricle. Again, hand injection from the sheathidentified it to be above the apex to minimizethe risk of ventricular perforation. There wasno mechanical interference with the implantedright ventricular lead. A threshold of 0.88 V at0.24 ms was achieved. The device was then de-ployed, sheath removed, and hemostasis achievedwith the subcutaneous purse string suture. Theold pacemaker was programmed to the minimumlower rate (30 beats/min) and output. The patientmade an uneventful recovery, and there wasno groin access complication. When seen at6 weeks and 3 months, the MicraTM TCP hada ventricular threshold of 0.63 V and 0.5 V at0.24 ms, respectively. There was satisfactory rateadaptation in the VVIR mode. There was noelectrical interference with the implanted deviceor pacemaker syndrome.
DiscussionCurrent LPMs are relatively large in diameter,
and require large diameter delivery sheaths fortranscatheter deployment (21F in St. Jude MedicalLCPTM, and 27F in Medtronic MicraTM TCP).These large sheaths are delivered from a femoral
venous approach. Because the right common iliacartery crosses in front of the LCIV, the vein isnaturally compressed and in some patients venousdrainage of the left leg may be compromised(May-Thurner syndrome).3 In this case, the venouspassage for the delivery sheath is compressed evenfurther by the rigid EVAR metal stent in boththe left and right common iliac arteries. A rightfemoral venous approach should be easier as thevein is not compressed in front, but is not possiblein this patient due to an indwelling HD catheter.By choosing the less obstructed upper venouschannel in the LCIV, and using sequentiallyupsized venous dilators, a stiff support wire, andpush and pull technique, the slippery hydrophilicsheath and dilator was successfully passed acrossthe compressed LCIV into the superior vena cava.
We did not find difficulty in physicalinterference of the delivery catheter and theindwelling ventricular lead across the tricuspidvalve. Passage across the tricuspid valve isfacilitated by deflectable sheath. With carefulpositioning and contrast injection, there is nophysical interference between the implanted rightventricular lead or the LPM. In a cadaveric study,4
up to 3 MicraTM TCP could be implanted inthe right ventricle without physical interference.
2 2016 PACE, Vol. 00

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
UNCORRECTEDPROOF
LEADLESS PACING IMPLANTATION
Figure 2. Chest and upper abdomen x-ray showing four implanted devices in the patient.EVAR = endovascular aortic repair stent graft; HD = hemodialysis catheter; LPM = entirelyleadless cardiac pacemaker; PM = conventional permanent pacemaker. Q3
There was no physical or electrical interference inour patient both during supine or standing whenshe was ambulant. An implanted pacemaker isan exclusion criteria in the published MicraTM
TCP trial.2 However, this patient demonstratesthat LPM may avoid multiple ventricular leadsacross the tricuspid valve in patients whoseright ventricular lead has failed and who arenot candidates for lead extraction. Upper limbvenography may still review patent subclavianveins and enable a repeat transvenous pacing.However, our patient, with her multiple venousfailures was reluctant to any further approach fromthe upper chest. Indeed, LPM has been reportedas an alternative to conventional pacing in apatient with recurrent pocket infection of bothsides of the chest, using the St. Jude MedicalLCPTM LPM.5 In another case, MicraTM TCP wasused in a patient with persistent left superior venacava and right subclavian vein that drained to the
abnormal superior vena cava in whom the pacingsystem was infected.6 Our patient with multiplecomorbidities and requiring anticoagulation madeleadless pacing a good alternative.7
ConclusionThe case exemplifies the following. (1)
Implantation of LPM is an alternative in patientswho do not have subclavian venous access for per-manent VVI pacemaker. (2) Contrast venography isuseful to identify the best possible venous passagefor the LPM, and for its positioning in the rightventricle. (3) In patients with EVAR, passage oflarge bore catheters required for deployment ofLPM may be difficult but achievable, althoughdownsizing of LPM and delivery sheath andcatheters will be useful, and (4) LPM is an optionto avoid multiple right ventricular leads across thetricuspid valve in case of right ventricular leadfailure.
PACE, Vol. 00 2016 3

1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
UNCORRECTEDPROOF
LAU AND LEE
References1. Reddy VY, Exner DV, Cantillon DJ, Doshi R, Bunch TJ, Tomassoni GF,
Friedman PA, et al. LEADLESS II Study Investigators. Percutaneousimplantation of an entirely intracardiac leadless pacemaker. N EnglJ Med 2015; 373:1125–1135.
2. Reynolds D, Duray GZ, Omar R, Soejima K, Neuzil P, Zhang S,Narasimhan C, et al. Micra Transcatheter Pacing Study Group. Aleadless intracardiac transcatheter pacing system. N Engl J Med 2015.[Epub ahead of print].Q4
3. May R, Thurner J. The cause of the predominantly sinistraloccurrence of thrombosis of the pelvic veins. Angiology 1957; 8:419–427.
4. Omdahl P, Eggen MD, Bonner MD, Wika K, Iaizzo AP. Rightventricular anatomy can accommodate multiple transcatheterpacemakers. Pacing Clin Electrophysiol 2015 (doi: 10.1111/pace.12804).
5. Tjong FV, Kooiman KM, de Groot JR, Knops RE. A leadless solution.Europace 2015; 17:800. Q5
6. Garweg C, Ector J, Willems R. Leadless cardiac pacemaker asalternative in case of congenital vascular abnormality and pocketinfection. Europace 2016. (pii: euw023).
7. Fisher JD. Leadless pacemakers: Putting them in and taking them out.Pacing Clin Electrophysiol 2015; 38:1247.
4 2016 PACE, Vol. 00