Toxic neuropathy
-
Upload
apple-samsung -
Category
Health & Medicine
-
view
437 -
download
2
description
Transcript of Toxic neuropathy
- 1. Toxic neuropathy Tossif Ghodiwala Peoples Friendship University of Russia
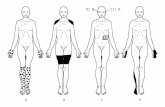
2. Neither clinical nor laboratory evaluation can distinguish occupational neuropathies from neuropathies due to other causes. Ref: Occupational Peripheral Neuropathies (MARCELLO LOTTI, MD; CHARLES E. BECKER, MD, and MICHAEL J. AMINOFF, MD, San Francisco) 3. Peripheral neuropathies can be divided into: Those which are bilaterally symmetrical polyneuropathies (for example, most neurotoxins) Those which are focalmononeuropathies Multiple mononeuropathies (vasculitidies, multifocal motor). 4. Other subdivisions are based on the predominant site of dysfunction: Axonsaxonopathies (organophosphates) Nerve cell bodiesneuronopathies (pyridoxine) Schwann cells and/or their myelin sheaths demyelinating neuropathies (acute arsenic poisoning). 5. There are also different types of peripheral nerve fibres: motor, sensory, and autonomic. Sensory fibres are divided into at least three groups anatomically, physiologically, and functionally: A (or A)large diameter, myelinated, fast conducting; mediating vibration, position, and touch sensations Asmall diameter, myelinated, slow conducting; mediating cold sensation C fibresvery small diameter, unmyelinated, very slow conducting; mediating hot and pain 6. distal axonopathy is the most common form 7. Clinical 8. The clinical effect of a polyneuropathy depends on 1) what modalities involved 2) what fibers are effected 3) whether the injury is axonal or demyelinating. Adapted from http://www.neuroanatomy.wisc.edu/SClinic/Weakness/Weakness.htm 9. Loss of function - symptoms Disturbed function + symptoms Motor nerves Wasting Hypotonia Weakness Hyporeflexia Orthopedic deformity Fasiculations Cramps The clinical response to motor nerve injury 10. www.neuro.wustl.edu/neuromuscular/pics/people/patients/Hands/handatrophymnd3.jpg 11. Loss of function - symptoms Disordered function + symptoms Sensory Large Fiber Vibration Proprioception Hyporeflexia Sensory ataxia Paresthesias Sensory Small Fiber Pain Temperature Dysesthesias Allodynia The clinical response to sensory nerve injury 12. Loss of function - symptoms Disturbed function + symptoms Autonomic nerves Sweating Hypotension Urinary retention Impotence Vascular color changes Sweating Hypertension The clinical response to autonomic nerve injury 13. Axonal Demyelinating Mixed Sensory Sensory & Motor Motor Lead Nitrous oxide Acrylamide Alcohol (Ethanol) Allyl chloride Arsenic Cadmium Carbon disulfide Cobalt Colchicine Cyanide Ethylene oxide Lithium Methyl bromide Organophosph ates Botulism Lead Mercury Buckthorn Hexachlorophe ne Muzolimine Perhexiline Porcine brain Procainamide Tellurium Diethylene glycol Ethylene glycol Gold Hexacarbons n-Hexane Na+ Cyanate 14. Allyl chloride Toxicity Uses: Manufacture of epoxy resin & glycerin Atmospheric exposure Outbreaks in Chinese Neuropathy Distal Sensory > Motor Axonopathy; Distal Recovery: Months; Following toxin withdrawal Pathology Distal axonopathy Multifocal neurofilament accumulations CNS: Dorsolateral columns 15. Arsenic (inorganic)Toxicity Sources: Suicidal, Homicidal, Occupational, Environmental Mining Inorganic arsenic: Exposure to by-products of copper & lead smelting Ingestion of trivalent arsenic Suicide Homicide Food or water contamination: Endemic regions o Groundwater contamination o Locations: West Bengal, India; Bangladesh; Inner Mongolia o West Bengal, India 6 million people exposed to arsenic through drinking water 300,000 people manifest signs of chronic arsenicosis Contaminated opium: Punjab 16. Clinical syndromes: Dose related General: Garlic-like smell to breath & tissue fluids Massive overdose: Subacute neuropathy Early GI: Vomiting & Diarrhea; Probably 2 GI irritation Autonomic: Tachycardia & Hypotension; 2 GI fluid loss Neuropathy Onset Delayed: After 10 to 20 days Distal paresthesias & numbness Evolution Over 2 to 5 weeks Sensory > Motor Large fiber sensory modalities Systemic signs: Few Pathology: Distal axonal loss Demyelination Treatment: Chelation with BAL or penicillamine for months Recovery: Slow over years 17. Hexacarbons Toxic compounds n-Hexane n-butyl ketone 2,5-hexanedione Metabolism n-Hexane & n-butyl ketone metabolized to active agent: 2,5-hexanedione 2,5-HD half-life: 13--14 hours; Accumulation may occur during workweek Detection: Acid-hydrolyzed urinary levels of 2,5-HD Sampled at the end of a shift Correlate with workplace concentrations of n-hexane 18. Uses n-Hexane: Glues & Lacquers: Solvents Exposure: Glue sniffing; Gasoline sniffing; Occupational n-butyl ketone: Solvent Exposure routes Common: Airborne Occasional: Dermal; Latex gloves not effective protection Exposure limit: 50 ppm Epidemiology Young males: Glue sniffing; Gasoline sniffing Occupational: Auto mechanics; Printing plants; Sandal shops; Furniture factories Geography: Asia; Europe; US Neurotoxic effects of n-hexane may be intensified Use with other chemicals: Acetone, MEK, Isopropanol 19. Chronic low dose exposure: Neuropathy syndromeExposure: Gasoline sniffing , Shoemakers Onset Subacute or Slowly progressive: 2 months Sensory loss: Distal Paresthesias Weakness Distal > Proximal Legs > Arms Distribution Symmetric: Most common Mononeuritis multiplex: Rare; ? Due to nerve compressions Sensory Loss Distal; May progress to proximal involvement Hands & Feet Large & Small fiber modalities Paresthesias Distal Hands & Feet 20. Tendon reflexes: Absent or Preserved except at ankles Recovery: With delay after removal of toxin Progression ("coasting") for 1 to 4 months Improvement: Months to years Residual deficits in more severe cases Distal sensory loss & weakness Spasticity CNS Encephalopathy: Hallucinations Myelopathy: Occasional; Delayed onset; Spasticity Systemic disorders Weight loss Malaise & Anorexia Abdominal pain Electrodiagnostic SNAPs: Subclinical exposure to 2,5-hexanedione can reduce amplitudes 21. LaboratoryCSF: Normal Electrophysiology: Axonal loss + Features of demyelination Axonal loss: Small CMAPs Conduction block Partial; Non-focal (Graded); Distal (Forearm & Leg) Especially rapid onset cases exposed to high doses Glue sniffing more than chronic industrial exposure In progressive phase of disease Late: Disproportionate distal slowing of NCV CNS: Abnormal visual & auditory evoked potentials 22. Pathology Distal axonopathy Giant neurofilamentous swellings In PNS & CNS At proximal sides of nodes of Ranvier Distal, non-terminal regions of axons Progress proximally Consist of 10 nm neurofilaments May produce 2 demyelination: Thin myelin sheaths Axoplasmic transport may be impaired Nerve biopsies may be normal with mild disease Treatment: Removal from n-hexane exposure 23. Lead Epidemiology of lead toxicity Common in children: Especially black non-hispanic children (22%) Most common in homes built from 1920 to 1950 Identical twins often have concordant lead levels Lead neuropathy: Especially from industrial exposure Exposure: Most common with ingestion & inhalation Sources Ingestion: Paint; Moonshine whiskey; Rum processed in lead pipes; Asian folk medicines9 Occupational: Smelting; Battery manufacture; Demolition; Auto radiator; Silver refining 24. Neuropathy: Motor Exposure: Subacute to high environmental lead concentrations Patterns of weakness: Variable Childhood: Lower extremity Adults Arms (Wrist & Finger extensors) > Legs Distal > Proximal Asymmetric Recovery: Good with elimination of exposure, unless severe weakness Variants Severe exposure: May produce quadriplegia Chronic low level exposure: No weakness Older literature: Focal weakness o Wrist & finger extensors o Proximal shoulder o Hand intrinsic muscles o Peroneal muscles o Laryngeal paralysis 25. Associated disorders Pain: Abdominal; Headache; Joint General: Fatigue; Irritability Anemia Sickle cell disease Electrophysiology Motor Axon loss Mild cases: Prolonged distal latencies or Normal Sensory Vibratory thresholds: Increased Mild slowing of NCV Pathology Humans: Axonal degeneration Experimental animals Segmental demyelination Endoneurial edema Recovery: Slow improvement 26. Neuropathy: Sensory Chronic low level lead exposure: Often decades Distal; Legs > Arms; Symmetric Subclinical changes common CNS Encephalopathy in children: Lethargy; Ataxia; Dysarthria Severe: Cerebral edema; Seizures Chronic Intellect impaired in dose dependent fashion More severe: Exposure at 2 years; Long duration of exposure Systemic features GI: Constipation; Abdominal pain Renal failure Hypertension Gums: Blue discoloration 27. Basophilic stippling Lab Hematologic: Mild anemia Hypochromic & Microcytic Basophilic stippling of erythrocytes Always present with neuropathy Uric acid: Low CSF: Usually normal Urine Coproporphyrin: High Lead: High (> 0.2 mg/L); Related to intake Blood lead levels Usual test for lead exposure Symptoms usually with levels > 80 g/dL Not accurate indicator of degree of symptomatology or body burden Radiology Bones: Lead lines GI: Paint chips in GI tract with acute ingestion 28. Treatment Elimination of exposure Chelation: Children > 25 g/dL; Adults > 70 g/dL Penicillamine: Mild intoxication < 70 g/dL Succimer (DMSA) Ca-Na2 EDTA: Lead level > 70 g/dL BAL: Added with severe toxicity Dimerval (DMPS) 29. Work-out 30. Diagnosis Take a thorough medical history, including the patients occupational and environmental history, to consider all sources of exposure to all possible agents. List details of all jobs and specific tasks within these jobs, as well as when various symptoms and medical problems began for the patient. 31. Quantitative sensory testing in the diagnosis of neuropathy includes the following: Vibration threshold Thermal threshold Portable motor and sensory latency Current perception threshold (CPT) 32. Other studies that help to prove the presence of neuropathy include the following: Intraepidermal nerve fiber density (IENF) Sympathetic skin reflex Electromyography (EMG) Nerve conduction 33. Laboratory studies in patients with neuropathy can include the following: Glucose tolerance Serum, urine, or blood Vitamin B-12 Monoclonal gammopathy of unknown significance Axonal neuropathy Cryoglobins and hepatitis C evaluation Immunofixation (for paraneoplastic neuropathy) Cerebrospinal fluid (CSF) protein level: Usually normal in toxic neuropathy 34. Management 35. Medical Care Advise removal from occupational or environmental exposure. Advise discontinuation of medication or recreational drug habit. Also provide information regarding how alcohols affect those with exposures. Preventive care and supportive care should include consideration of life stressors, diet, and overall behavior modifications. 36. Treatment options also include the following: Nonpharmacologic options include cool soaks, heat, massage, elevation or lowering of the limbs, shoe tightness, and/or exercise. Pharmacological options include tricyclic antidepressants, anticonvulsants, opiates, or topical capsaicin cream. Other options include intravenous gamma globulin, aldose reductase inhibitors, nerve growth factor, antitumor necrosis factor-; these are mainly research ideas. Three that may be helpful presently include lipoic acid, evening primrose, and vitamin E. 37. Alpha lipoic acid is well reviewed by Halat and Dennehy. Thiolic acid is a free radical scavenger and chelator. It is approved for use in Germany for neuropathy. The best studies suggest parenteral use followed by oral use relieves symptoms and improves nerve blood flow. Oral preparations are available in United States. Two studies suggest increased nerve conduction (600/1200 mg for 2 y, oral) and reduced symptoms (1800 mg/d for 3 wk, oral). The mechanism of action includes chelation and, thus, a concern for mineral shortage exists. Monitoring iron levels is suggested, and persons with 38. Evening primrose is also well summarized by Halat and Dennehy.[58] It includes omega 6 essential fatty acids: gamma linoleic acid (GLA) and linoleic acid. It is an essential component of myelin and the neuronal cell membrane. Dosages ranging from 360-480 mg/d for 6 months to 1 year improved nerve function measurements. It has mild side effects including inhibition of platelet aggregation. Concern also exists for those with seizure disorders. 39. Vitamin E is discussed in the article Argyriou et al.[59] Vitamin E has been administered to patients on chemotherapy for prevention of neuropathy at doses of 600 mg/d during treatment and then for 3 months after treatment. A reduced peripheral neuropathy score has been noted. A neuroprotective effect has been described 40. Consultations Occupational therapist Environmental medicine specialist 41. Diet Although diet does not play a specific role in reparation of the PNS, a balanced diet is important for various reasons related to general health. Since various B vitamins have been implicated in the development of neuropathies, some physicians suggest supplementation. 42. Further Outpatient Care Consistent follow-up care with a neurologist is necessary to monitor the progress of neurological findings. Follow-up with an occupational medicine specialist may be important to assist with return to work and reduction of exposure. This clinician may be able to work with the company supervisors or management to improve the work environment. This may occur if the company chooses to substitute the neuropathy- causing agent with a less-toxic agent in the workplace, to change the schedules of workers so that their exposure is less during a period of time, or to promote safer personal protective equipment. Communication between health care provider and management is essential for this individual's health as well as his or her status for disability or ability return 43. Prognosis Each patient's prognosis depends on the severity of the neuropathy when exposure is ceased or reduced to levels that will not affect health negatively. 44. Patient Education Inform patients about aspects of dose, diet, and nutrition that may increase risk of toxicity when taking a medication. Since many solvents are metabolized in the liver, concomitant use of medications with similar metabolism may lead to increased toxicity. Workers, by law, need to be informed of chemicals in the workplace and their potential health hazards. Material safety data sheets (MSDS), per order of Occupational Safety and Health Administration (OSHA), are available to all workers in the workplace. The Emergency Planning and Community Right to Know Act (EPCRA) requires that facilities using, storing, or manufacturing hazardous chemicals make public inventory and report every release to public officials and health personnel. These facilities must cooperate with health personnel who are treating victims of exposure.






![VITAMIN E AMELIORATES THE TOXIC EFFECT OF AMIODARONE ON THYROID GLAND ... · peripheral neuropathy and thyroid dysfunction[4,5,6,7]. Recently, bilateral vestibulopathy was described](https://static.fdocuments.in/doc/165x107/5e77c33b15630f2b0e6f2b60/vitamin-e-ameliorates-the-toxic-effect-of-amiodarone-on-thyroid-gland-peripheral.jpg)