Towards identifying optimal doses for alpha-2 adrenergic modulation of colonic and rectal motor and...
Transcript of Towards identifying optimal doses for alpha-2 adrenergic modulation of colonic and rectal motor and...

Towards identifying optimal doses for alpha-2 adrenergicmodulation of colonic and rectal motor and sensory function
A. MALCOLM*, M. CAMILLERI*, L. KOST*, D. D. BURTON*, S. L. FETT & ALAN R. ZINSMEISTER *Gastroenterology Research Unit, and Section of Biostatistics, Mayo Clinic and Mayo Foundation, Rochester, USA
Accepted for publication 14 December 1999
INTRODUCTION
Disorders of colorectal motor and sensory function are
thought to contribute to the symptoms of various
gastrointestinal diseases including functional bowel
disorders.1 Heightened sensitivity has been demonstrat-
ed in irritable bowel syndrome and reduced colonic
motility has been demonstrated in idiopathic constipa-
tion, pseudo-obstruction, neurological conditions such
as spinal cord injury, multiple sclerosis and Parkinson's
disease.1±6 Increased high amplitude colonic contrac-
tions are observed postprandially in irritable bowel
syndrome with predominant diarrhoea.7
Current therapy for these conditions is suboptimal;
future advances require mechanistic studies of the
neuromuscular apparatus of the colon. The adrenergic
nervous system provides extrinsic inhibitory control of
gut motility; visceral afferents synapse with dorsal horn
neurones and descending adrenergic and serotonergic
®bers in the spinal cord modulate dorsal horn neurones
which are the second order neurones in the 3-neurone
pathway mediating visceral sensation.8
Correction of colorectal motor or sensory dysfunction
may improve symptoms if selective therapies modulate
SUMMARY
Rationale: Visceral sensation and motility are important
in functional gut disorders and are partly controlled by
adrenergic innervation.
Objectives: To characterize the a2-adrenergic control of
motor and sensory function of descending colon and
rectum.
Methods: In 32 healthy volunteers, we assessed com-
pliance, fasting and postprandial tone, and sensations of
gas, urgency and pain during phasic distentions. Each
subject received one agent at clinically approved doses:
clonidine (0.05, 0.1, 0.2 or 0.3 mg p.o.); or the a2
antagonist yohimbine (0.0125 mg, 0.05 mg, 0.125 mg
or 0.2 mg intravenously and infusion over 2.5 h).
Results: Clonidine increased colonic and rectal compli-
ance, and reduced tone, pain, gas sensation and rectal
urgency. Clonidine showed large pairwise differences in
sensation and motility between 0.05 and 0.1 mg doses,
which did not interfere with the colon's motor response
to feeding. Conversely, yohimbine dose-dependently
altered the compliance curve, increased tone and
sensations of gas, pain and urgency. Drug effects in
the colon were more marked at low distensions;
a2 modulation of rectal sensation was observed at all
levels of distension.
Conclusions: a2-adrenergic mechanisms modulate colo-
rectal sensations and motility; at doses as low as
0.05 mg, clonidine reduced colorectal sensation while
the tone response to feeding was preserved. These
studies provide insight into the potential use of a2
agents in disease states.
Correspondence to: Dr M. Camilleri, Gastroenterology Research Unit, Al-
fred 2±435, Mayo Clinic, 200 First St. S.W., Rochester, MN 55905,
USA.E-mail: [email protected]
Aliment Pharmacol Ther 2000; 14: 783±793.
Ó 2000 Blackwell Science Ltd 783

functions without deleterious effects on others. We have
previously demonstrated that, among a variety of
adrenergic agents active on receptor subtypes, the
a2-adrenergic agents, administered at maximal
approved doses, affect colonic and rectal motor and
sensory function.9, 10 Thus, clonidine, an a2-adrenergic
agonist, induces colonic and rectal relaxation and
reduces conscious perception of balloon distention in
the colon and rectum.9, 10 On the other hand, yohim-
bine, an a2-adrenergic antagonist, has been shown to
cause contraction of the rectum and to increase the
perception of balloon distention in the rectum.10
In this study, our aims were to characterize dose-
related effects of clonidine and yohimbine on colonic
and rectal motor and sensory function in healthy
human volunteers; this goal was intended to indicate
the optimal doses of each of the drugs to be used in
future studies in disease states. A second speci®c goal
was to evaluate the doses of clonidine that relieve pain
or gas perception during experimental distentions, while
preserving the ability of the colon to contract or
increase tone following meal ingestion.
MATERIALS AND METHODS
Healthy volunteers
Thirty-two healthy volunteers, aged 19±44 years (14
males, 18 females; mean age 29 years), were recruited
by public advertisement. None had undergone previous
gastrointestinal surgery; all had negative responses on
the Bowel Disease Questionnaire and normal responses
on the Hospital Anxiety and Depression Inventory, and
a normal clinical and physical examination and
electrocardiogram (EKG).11, 12 Women of childbearing
potential were required to have a negative pregnancy
test. The protocol was approved by the Mayo Institu-
tional Review Board, and written informed consent was
given in all cases.
Experimental design
All subjects were admitted to the General Clinical
Research Center on the evening prior to the study for
bowel cleansing with 2 L of polyethylene glycol and
electrolyte solution (OCL, Abbott Laboratories, Chicago,
IL) and overnight fast. Left-sided colonoscopy was
performed without sedation; a 4-meter Te¯on-coated
guidewire (Microvasive, Hobbs Medical, Stafford
Springs, CT) was placed with its tip at the splenic
¯exure and the colon was de¯ated as the colonoscope
was withdrawn. The colonic tube assembly was intro-
duced into the colon over the guidewire and positioned
under ¯uoroscopic control with the polyethylene bal-
loon (9-cm long cylinder with a maximum volume of
600 mL [Hefty Baggies, Mobil Chemical Company,
Pittsford, NY]) in the mid-descending colon. A second
balloon was then inserted into the rectum. Respiratory
excursions were continually recorded from a pneumo-
graph belt positioned around the lower chest. Blood
pressure was recorded at 30-min intervals during the
entire study. Patients lay in the right lateral position
during the study to avoid pressure on the descending
colon and rectum from surrounding organs.
After a `dummy' distention (ramp to 20 mmHg with
steps of 4 mmHg, 30 s), which has previously been
shown to enhance reproducibility of colorectal compli-
ance tests, the barostat operating pressures were set
(2 mmHg above the point at which respiratory variation
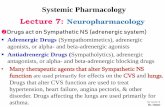
was noted).13 The entire experimental protocol is sum-
marized in Figure 1. After a 30-min wait, the levels of
sensory perception and compliance were measured,
followed by fasting tone (30-min period). The drug was
then administered, and post-drug tone (30 min), compli-
ance and perception were reassessed. Tone was assessed
for 30 min pre-meal and 1 h following a 1000 kcal
liquid, high-fat (50%) meal. Sensation and compliance
were again measured 1 h after the meal was ingested.
Colonic and rectal motor function
Tone of the colon was measured as in previous
studies.14
Figure 1. Experimental protocol.
784 A. MALCOLM et al.
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

Testing colonic and rectal compliance
Colonic and rectal compliance were assessed as the
volume response to 2 mmHg increments in intraballoon
pressures at 30-s intervals from 0 to 24 mmHg above
operating pressure. The rigid piston barostat used in this
study (Distender Series II, G & J Electronics, Toronto,
Canada) has almost zero intrinsic compliance.
Testing colonic and rectal sensation
Subjects received a standardized information sheet prior
to sensation testing; thereafter there was minimal inter-
action between subject and investigator. Sensation was
assessed by responses recorded on a visual analogue scale
during rapid phasic distentions of 8, 16 and 24 mmHg
above operating pressure performed in a randomized
order. Each distention lasted 60 s and was followed by a
rest period at the operating pressure, also lasting 60 s.
Ratings of sensory perception were assessed at a
standardized time, 30 s after the onset of the distention.
The subject was asked to record perception on three
100 mm visual analogue scales for the feeling of gas and
pain during colonic distensions, and for urgency, gas and
pain during rectal distensions. The visual analogue
scales were anchored at each end by the descriptions
`none' and `worst possible'. This approach to measuring
visceral perception has previously been shown to be
responsive to variations in stimulus, psychosensory
state, and pharmacological modulation.9, 10, 15
Clonidine and yohimbine administration
Clonidine was administered p.o. because it is > 99%
bioavailable, Tmax is around 60 min, and plasma
levels are high for at least 4 h after p.o. ingestion.
Yohimbine was administered as i.v. bolus and infu-
sion in order to maintain a constant plasma level,
because intravenous yohimbine has a short half life
(3±5 min). The doses used are over a range where
effect has been seen in previous studies, and in
addition an investigational drug permit was obtained
from the United States Food and Drug Administration
to also use yohimbine at a dose just above that which
has been used in previous gastrointestinal physiolog-
ical studies in order to obtain wider dose response
data. Table 1 shows the number of subjects in each
treatment arm and the doses of clonidine and
yohimbine given.
Data analysis
Colonic and rectal motor parameters. Barostat balloon
volume and pressure activity for colon and rectum
were sampled as analogue signals at 8 Hz and
converted to digital signal before being recorded on a
computer. A modi®ed VAX LAB ®ltering program
(Digital Equipment Corporation, Boston, MA) was used
to record and identify phasic activity. Phasic volume
peaks recorded by the barostat balloon occur at a
frequency of < 3 per minute;14 therefore, waveform
frequencies of > 6 cpm were ®ltered out by a computer
program to separate baseline balloon volume from
phasic volume events. Colonic and rectal tone are
assessed by the level of colonic or rectal barostat
balloon baseline volume.
Colonic and rectal compliance. The volume±pressure
relationships de®ning colonic or rectal compliance are
Table 1. Participant characteristics
Drug Dose
Gender
number (M:F) Age Anxiety* Depression*
Clonidine 0.05 mg 3 1:2 31.0 � 4.9 2.7 � )1.2 2.7 � )1.2
Clonidine 0.1 mg 5 1:4 27.8 � 3.7 3.8 � )1.0 0.8 � )0.4
Clonidine 0.2 mg 5 2:3 25.8 � 2.7 1.1 � )0.5 0.4 � )0.2
Clonidine 0.3 mg 3 2:1 23.7 � 2.7 2.7 � )1.2 2.0 � )1.5
Yohimbine 0.0125 mg 3 1:2 36.7 � 4.9 2.7 � )0.3 1.0 � )0.6
Yohimbine 0.05 mg 5 3:2 27.4 � 3.0 4.8 � )0.7 3.2 � )0.8
Yohimbine 0.125 mg 5 3:2 30.8 � 4.2 3.2 � )1.3 2.0 � )0.8
Yohimbine 0.2 mg 3 1:2 31.0 � 6.5 4.3 � )0.9 3.0 � )0.6
Data are mean + S.E.M.
* Anxiety and depression ratings based on Hospital Anxiety and Depression Scale, where
scores < 7, 8±10 and > 10 represent normality, indeterminate and de®nite anxiety or
depression, respectively.
a2 -ADRENERGIC CONTROL OF HUMAN COLON 785
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

nonlinear and were analysed as in previous studies
using a power exponential model:9
Pvol � R� expfÿ�k� rP�bg
where rP is reciprocal pressure (1/pressure), Pvol is the
proportionate volume (vol/Vmax, Vmax is the maximum
volume in the compliance assessment) and R is the
estimated minimal proportionate volume. The summary
parameters estimated for this model of compliance,
k (slope) and b (overall shape of the curve), were used to
calculate Pr1/2, the pressure producing half maximum
volume on the pressure±volume curve.
Colonic and rectal sensation. Sensation scores for gas,
urgency and pain were analysed separately; an addi-
tional analyses used the aggregate (mean) of pain and
gas sensation scores in the colon and an aggregate
(mean) sensation of gas, urgency and pain scores for
analysis of rectal sensation.
Statistical analysis
We examined the pre-drug differences in tone, com-
pliance and sensation among the four dosage groups
for each drug using the Kruskal±Wallis test. Overall
drug effects were assessed by comparing pre-drug and
post-drug values using the Wilcoxon signed rank test.
In order to adjust for minor differences in baseline
response values, we adjusted for pre-drug values (and,
in the analysis of tone, for body mass index) by
incorporating these as covariates in the analysis of
dose level effects on post-drug and post-meal measure-
ments using an analysis of covariance. The analysis of
sensation scores was based on a (mixed-model)
repeated measures analysis incorporating pre-drug
sensation score, volumes corresponding to each speci®c
distention level, and the corresponding pressure and
order of distention. To facilitate individual pairwise
comparisons among dosage groups, the (adjusted for
baseline values) mean (and 95% con®dence intervals)
was computed for tone and sensation scores. The (least
squares estimated) mean values of the compliance
parameters (adjusted for baseline values) were used to
construct mean dosage group compliance curves to
graphically summarize drug effects on colonic and
rectal compliance. In situations where overall dose
effects were detected, the Tukey adjustment for mul-
tiple pairwise comparisons amongst speci®c doses was
used.
RESULTS
Patient characteristics
Demographic features and hospital anxiety and de-
pression ratings are summarized in Table 1. Post-drug
data could not be fully evaluated in three patients for
technical reasons (blocked pressure port in the baro-
stat, leak in the barostat balloon, or a kinked tube).
These three subjects were receiving yohimbine at
doses of 0.05 mg (n � 1), 0.125 mg (n � 1) and
0.2 mg (n � 1). Prior to the studies, the participants
who had been randomized to the yohimbine group
had higher depression scores (P � 0.03, 2-sample t-
test) and somewhat higher anxiety scores (P � 0.07,
2-sample t-test) compared to the participants in the
clonidine group; however, none of the scores were in
the range associated with clinically signi®cant affective
disorder.
Effects of a2-adrenergic agents on colonic and rectal tone
Clonidine (Figure 2). There were no differences in the
pre-drug balloon volumes (tone) among the different
dosage levels of clonidine. Post-drug, there was an
overall relaxation of colonic tone (P < 0.01) relative to
pre-drug (Wilcoxon signed rank test). Meal ingestion
resulted in a reduction in volume relative to pre-meal.
Clonidine relaxed rectal tone (P < 0.01, Wilcoxon
signed rank test) during fasting. The meal induced a
reduction in balloon volumes (increase in tone) in the
colon and rectum (P < 0.01 for both sites, Wilcoxon
signed rank test).
After adjusting for the pre-drug volume and body mass
index, as a means to compensate for differences in
colonic and rectal dimensions (since these were signi®-
cant covariates), there was a signi®cant overall dose-
related effect (P < 0.05) on the colon's tone (increase in
volume) following administration of the drug. The
largest pairwise difference in volumes for the colon
was between the 0.05 mg (mean 79 mL, 95% con®d-
ence interval 64, 97) and 0.1 mg (mean 124 mL, 95%
con®dence interval 107, 145) doses (P < 0.05, Tukey
adjustment).
Yohimbine (Figure 2). There were no differences in the
pre-drug balloon volumes among the different dosage
levels of yohimbine. Overall, yohimbine resulted in
signi®cantly lower colonic and rectal balloon volumes
786 A. MALCOLM et al.
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

(increased tone) in the post-drug vs. pre-drug fasting
and post-meal vs. pre-meal periods (all P < 0.01,
Wilcoxon signed rank test). After adjusting for the
pre-drug volume (a signi®cant covariate), we observed a
tendency for dose-related effects on the post-drug
volume in the colon (P � 0.06).
Figure 2. Overall effects of several doses of clonidine and yohim-
bine on colonic and rectal tone. Note that clonidine increases
balloon volumes post-drug and pre-meal, consistent with reduced
tone; the meal results in an increase in tone (reduction in balloon
volume) in the colon and rectum. Conversely, yohimbine reduces
balloon volume, and meal ingestion results in a further reduction,
consistent with increased tone. Data show mean �95% con®dence
intervals; overall (doses), the post-drug and post-meal effects of
both drugs are statistically signi®cant.
Figure 3. Dose-related effects of clonidine on colonic compliance
post-drug (left) and post-meal (right). In the range tested, there
was a signi®cant difference between effects of 0.05 and 0.1 mg
clonidine on colonic compliance; no overall dose responsiveness
was noted post-drug or post-meal. Data show least square means,
incorporating pre-drug compliance curve parameter estimates at
each dose level.
a2 -ADRENERGIC CONTROL OF HUMAN COLON 787
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

Effects of a2-adrenergic agents on colonic
and rectal compliance
The ®t of the power exponential model across all studies
resulted in a median R2 of 0.992 (with 10th and 90th
percentiles of 0.972 and 0.999, respectively). No pre-
drug differences in compliance were detected in the
dosage levels for the two drugs.
Clonidine (Figure 3). Clonidine induced an overall
increase in colonic and rectal compliance as shown by
decreased j and Pr1/2. Speci®cally, clonidine had an
overall post- vs. pre-drug (pre-drug Pr1/2 � 16.1;
post-drug Pr1/2 � 11.6; P < 0.01) effect on rectal
compliance, but no dose effect was detected. The only
dose-related effect of clonidine identi®ed was a signi®-
cant dose effect on Pr1/2 estimates in the colon after the
meal (P < 0.05), adjusting for pre-drug compliance and
body mass index.
Yohimbine (Figure 4 [colon] and Figure 5 [rectum]).
Overall, yohimbine did not change compliance charac-
teristics, however we observed subtle dose-related
changes in the initial shape of the compliance curve
(b value) in the colon post-drug (P � 0.02) and in the
rectum post-drug (P � 0.05) and post-meal (P < 0.01).
Effects of a2-adrenergic agents on colonic
and rectal sensation
Clonidine (Tables 2 [overall] and 3 [dose-related effects]).
There were no differences in the pre-drug sensation
scores among the different dosage levels of clonidine. In
the colon, there were lower gas and aggregate gas and
pain scores post-clonidine in response to distention
with 8 mmHg (P < 0.01), but not at higher distention
levels. After adjusting for pre-drug sensation score,
volume, pressure, and order of distention, there was an
overall dose effect in the colon (Table 3) for aggregate
gas and pain post-drug (P � 0.01) and post-meal
(P � 0.04).
Figure 4. Dose-related effects of yohimbine on colonic compliance
post-drug (left) and post-meal (right). There were signi®cant dose-
related effects of yohimbine on the estimated b parameters of the
compliance curves (P � 0.02), but not on j or Pr1/2 parameters.
The ®gure shows curves constructed from least square means,
incorporating the pre-drug compliance curve parameter estimates
at each dose level.
788 A. MALCOLM et al.
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

In the rectum, pooling dose groups, clonidine signi®-
cantly decreased (Table 2) aggregate scores of gas,
urgency, and pain at all levels of distention (P < 0.05 for
8 and 24 mmHg; P < 0.01 at 16 mmHg). A borderline
signi®cant dose-related effect of clonidine was observed
in the rectum (Table 3) during the post-drug period for
gas scores (P � 0.06), but not for urgency or pain.
Yohimbine (Tables 4 [overall] and 5 [dose-related effects]).
Sensation scores during pre-drug assessment were
similar among the different yohimbine dosage groups
except for pain scores in the colon at 8 mmHg
distention (P � 0.03, unadjusted for multiple compar-
isons). Overall, the changes in colon sensation (pre vs.
post, Table 4) at each distention level indicated consis-
tently higher scores post-drug for both pain and gas,
and the aggregate (average score). Similar results
(Table 4) were observed in the rectum for gas, urgency,
pain, and the aggregate (average score). The speci®c
signi®cant changes are noted in Table 4.
After adjusting for the signi®cant covariates (pre-drug
sensation scores, the individual volumes corresponding
to each speci®c distention level, the speci®c pressure,
and the order of distention), we observed signi®cant
dose-related increases in colonic sensation of gas
(P < 0.01), pain (P < 0.01), and the aggregate (aver-
age score [P � 0.06] with yohimbine). These were
especially evident in the post-meal period (P < 0.01 for
gas, P < 0.005 for pain, P < 0.005 for average gas and
pain, respectively). Higher doses of yohimbine tended to
increase the sensation scores (Table 5) in both the colon
and the rectum, in particular post-drug and post-meal
rectal urgency.
DISCUSSION
This study shows that the a2-adrenergic system alters
motor and sensory function of the human colon and
rectum in healthy individuals. These studies also
indicate threshold levels for the dose-related effects on
some of the motor and sensory functions of the colon
and rectum. With clonidine, it appears that a signi®cant
dose-related pairwise difference is observed between the
0.05 and 0.1 mg doses. These dose-related effects of
clonidine on perception scores are not associated with
major differences in the relaxation of the colon, nor on
the ability of the colon to increase tone postprandially.
Therefore, we would consider a dose of 0.05 mg optimal
for ongoing studies of clonidine, given this dose has the
lesser potential to cause haemodynamic side-effects in
patients.
Clonidine lowered gas and pain sensation in the colon
at low levels of distension during fasting and postpran-
Figure 5. Dose-related effects of yohimbine on rectal compliance
post-drug (left) and post-meal (right). Yohimbine dose-relatedly
altered the b parameter of the rectal compliance curves post-drug
(P � 0.05) and post-meal (P < 0.01). There were no effects on jor Pr1/2. Data show least square means, incorporating the pre-
drug compliance curve parameter estimates at each dose level.
a2 -ADRENERGIC CONTROL OF HUMAN COLON 789
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

dially. These data expand on the previous observations
from our lab showing that 0.3 mg clonidine p.o.
reduced pain sensation during colonic distention, but
failed to signi®cantly alter gas sensation.9 The current
experiments explored a broader range of distentions and
a wider dosage range. The current data suggest that the
sensory effect of clonidine is not restricted to pain since
clonidine dose-dependently reduced aggregate colonic
sensation. Moreover, clonidine reduced rectal sensations
of urgency, gas and pain at all levels of rectal disten-
sion. These observations con®rm the importance of
a2-adrenergic mechanisms in the control of colorectal
sensation and suggest a potential role for clonidine in
the treatment of hypersensitivity or hypercontractile
states in the colorectum, such as in patients with
diarrhoea-predominant irritable bowel syndrome or
colonic autonomic neuropathy. These conditions are,
respectively, associated with rectal hypersensitivity and
with increased prevalence of high amplitude propagated
colonic contractions in the post-meal period which
induce rectal urgency and diarrhoea.3, 7
The effects of yohimbine, which induced higher gas
and pain scores in the colon, and gas, pain and
urgency scores in the rectum during all three levels of
8 mmHg 16 mmHg 24 mmHg
Colon
Gas 1.5 (0.5, 2.4)** 0.2 ()0.3, 0.8) )0.1 ()0.8, 0.6)
Pain 0.3 (0.0, 0.6) 0.2 ()0.6, 0.9) 0.5 ()0.3, 1.2)
Aggregate (gas and pain) 0.9 (0.3, 1.4)** 0.2 ()0.3, 0.7) 0.2 ()0.2, 0.6)
Rectum
Gas 0.9 ()0.5, 2.4) 0.8 (0.0, 1.7) 0.4 ()0.5, 1.3)
Urgency 0.8 (0.0, 1.6) 1.2 (0.5, 1.9)** 0.5 ()0.4, 1.4) Pain 0.3 ()0.1, 0.7) 0.7 ()0.1, 1.5) 0.8 ()0.3, 1.8)
Aggregate (gas, urgency, pain) 0.7 (0.0, 1.4)* 0.9 (0.3, 1.5)** 0.6 ()0.1, 1.2)*
* P < 0.05; ** P < 0.01; P < 0.1, from Wilcoxon signed rank test (pre-drug vs. post-drug),
unadjusted for multiple comparisons. Positive values indicate clonidine reduced sensation
scores.
Table 2. Overall effect of clonidine on
change in sensation (VAS, cm) in colon and
rectum during isobaric distentions. Mean
differences (pre-post-drug) and (95% con-
®dence interval)
Table 3. Dose-related effect of clonidine on sensation (VAS, cm) in colon and rectum (mean, 95% con®dence interval)
0.05 mg 0.1 mg 0.2 mg 0.3 mg
Post-drug effect of clonidine on sensation during fasting
Colon
Gas 1.9 (1, 2.8) 1.6 (0.9, 2.4) 1.5 (0.7, 2.2) 0.5 (0, 1.4)
Pain 0.2 (0, 0.6) 0.3 (0, 0.7) 0.5 (0.1, 0.8) 0.3 (0, 0.8)
Aggregate (gas and pain)* 1.6 (1.1, 2.2) 1.0 (0.5, 1.4) 0.8 (0.4, 1.2) 0.2 (0, 0.7)
Rectum
Gas 2.7 (1.6, 3.8) 1.3 (0.4, 2.1) 2.2 (1.3, 3.1) 1.1 (0, 2.2)
Urgency 4.9 (3.8, 6.0) 4.4 (3.5, 5.2) 4.8 (4.0, 5.6) 3.8 (2.7, 4.9)
Pain 0.7 (0.3, 1.0) 0.8 (0.5, 1.1) 0.5 (0.2, 0.9) 0.6 (0.2, 0.9)
Aggregate (gas, urgency, pain) 2.9 (2.2, 3.7) 2.2 (1.6, 2.7) 2.3 (1.7, 2.8) 2.0 (1.2, 2.7)
Post-meal effect of clonidine on sensation
Colon
Gas 0.9 (0, 2.1) 2.0 (1.0, 3.0) 1.6 (0.6, 2.5) 0.2 (0, 1.4)
Pain 0.4 (0, 0.7) 0.3 (0, 0.6) 0.3 (0, 0.6) 0.3 (0, 0.7)
Aggregate (gas and pain)* 0.3 (0, 1.0) 1.4 (0.9, 2.0) 0.8 (0.3, 1.4) 0.3 (0, 1.1)
Rectum
Gas 2.6 (1.5, 3.7) 1.2 (0.4, 2.1) 1.5 (0.6, 2.3) 1.1 (0, 2.3)
Urgency 5.3 (3.6, 7.0) 4.9 (3.6, 6.3) 4.2 (2.9, 5.5) 4.5 (2.8, 6.3)
Pain 0.5 (0, 1.0) 0.6 (0.1, 1.1) 0.6 (0.1, 1.1) 0.5 (0, 1.0)
Aggregate (gas, urgency, pain) 2.6 (1.9, 3.2) 2.2 (1.7, 2.7) 2.2 (1.6, 2.7) 2.3 (1.6, 3.0)
* P < 0.05; P < 0.1; overall test for dose effects from repeated measures analysis (see text).
790 A. MALCOLM et al.
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

distention, also argue strongly for the role of the
a2-adrenergic system in control of colorectal sensation.
The therapeutic potential of a2-adrenergic antagonists
in increasing colonic tone is probably greater than the
observed effects on sensation. The results of the
compliance curve changes with yohimbine are consis-
tent with the increases in baseline tone, since the bparameter, a measure of the initial shape of the
pressure±volume curve, was altered, not the (k slope)
or Pr1/2. The latter appears to re¯ect the elastic
properties of the smooth muscle hollow organs and
these are unaltered by yohimbine. These effects of
yohimbine on tone need to be further evaluated in the
context of acute or chronic colonic pseudo-obstruction
or megacolon. Yohimbine could also be used poten-
tially as a pharmacological model for colorectal
hypersensitivity. Given the dose±response relationship
seen and the lack of haemodynamic side-effects, the
Table 5. Dose-related effect of yohimbine on sensation (VAS, cm) in colon and rectum (mean, 95% con®dence interval)
0.0125 mg 0.05 mg 0.125 mg 0.2 mg
Effect of yohimbine on sensation during fasting
Colon
Gas** 2.3 (1.7, 3.0) 3.5 (3.0, 4.0) 3.1 (2.7, 3.6) 4.2 (3.6, 4.8)
Pain** 0.8 (0.1, 1.6) 1.0 (0.4, 1.6) 2.8 (2.2, 3.4) 1.8 (1.1, 2.6)
Aggregate (gas + pain) 1.8 (1.0, 2.5) 2.3 (1.8, 2.8) 2.9 (2.4, 3.5) 2.9 (2.2, 3.5)
Rectum
Gas 2.9 (0.4, 5.5) 4.1 (2.2, 6.0) 3.0 (1.2, 4.9) 4.6 (2.2, 7.0)
Urgency** 5.9 (5.3, 6.6) 7.4 (6.9, 7.9) 6.8 (6.3, 7.3) 6.9 (6.3, 7.5)
Pain* 1.1 (0, 2.6) 2.8 (1.6, 3.9) 2.2 (1.1, 3.4) 4.5 (3.1, 6.0)
Aggregate (gas, urgency, pain) 3.6 (2.5, 4.6) 4.7 (4.0, 5.5) 4.1 (3.3, 4.8) 5.1 (4.2, 6.1)
Effect of yohimbine on sensation postprandially
Colon
Gas** 0.9 (0, 2.8) 4.7 (3.0, 6.4) 2.5 (1.0, 4.0) 6.8 (4.4, 9.1)
Pain** 0 (0, 1.4) 2.3 (1.1, 3.5) 1.5 (0.3, 2.6) 5.7 (3.7, 7.7)
Aggregate (gas and pain)** 1.2 (0, 2.8) 3.3 (1.9, 4.6) 1.7 (0.5, 3.0) 6.4 (4.4, 8.3)
Rectum
Gas 3.2 (0, 6.6) 4.2 (1.5, 6.8) 3.4 (0.8, 6.0) 5.3 (1.9, 8.6)
Urgency* 3.9 (2.2, 5.6) 7.5 (6.2, 8.8) 6.8 (5.6, 8.1) 6.9 (5.4, 8.5)
Pain 1.0 (0, 2.2) 1.8 (0.9, 2.7) 2.6 (1.8, 3.5) 2.7 (1.6, 3.9)
Aggregate (gas, urgency, pain) 2.2 (0.5, 3.9) 5.1 (3.7, 6.4) 4.1 (2.7, 5.4) 4.9 (3.3, 6.6)
*P < 0.05; **P < 0.01; P < 0.1, Overall test for dose effects from the repeated measures analysis (see text).
Table 4. Overall effect of yohimbine on
change in sensation (VAS, cm) in colon and
rectum during isobaric distentions
Mean differences (pre-post-drug) and (95% con®dence interval)
8 mmHg 16 mmHg 24 mmHg
Colon
Gas )0.5 ()1.1, 0.2) )1.4 ()2.3, )0.5)** )1.0 ()1.9, )0.1) Pain )0.6 ()1.3, 0.1) )0.8 ()1.6, 0.1)* )0.8 ()1.5, 0.0)*
Aggregate
(gas and pain)
)0.6 ()1.1, 0.0)* )1.1 ()1.7, )0.5)** )0.9 ()1.4, )0.3)**
Rectum
Gas )1.1 ()2.2, 0.0) )0.2 ()1.3, 0.9) )1.6 ()2.7, )0.5)**
Urgency )1.0 ()1.7, )0.3)** )0.4 ()1.1, 0.3) )0.7 ()1.2, )0.3)**
Pain )0.6 ()1.2, 0.0)* )1.9 ()3.0, )0.9)** )1.4 ()2.3, )0.5)**
Aggregate
(gas, urgency, pain)
)0.9 ()1.4, )0.4)** )0.8 ()1.2, )0.4)** )1.2 ()1.8, )0.6)**
*P < 0.05; **P < 0.01; P < 0.1, from Wilcoxon signed rank test (pre-drug vs. post-drug),
unadjusted for multiple comparisons. Negative values indicate yohimbine aggravated
(increased) score of sensation.
a2 -ADRENERGIC CONTROL OF HUMAN COLON 791
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

higher doses of yohimbine may be considered in future
studies.
The current studies do not provide suf®cient detail to
de®ne the ED50 for clonidine or yohimbine's effects on
colonic or rectal motor and sensory functions or
induction of megacolon or pseudo-obstruction in view
of the normal meal response. It is unclear whether the
differences in clonidine's effects on descending colonic
and rectal tone imply differences in a2-adrenergic
control of the two regions. Since yohimbine's dose-
related effects were very similar in the two regions, the
hypothesis of differential regional control by a2-adren-
ergic neurones seems unlikely.
The increase in sensory perception with increasing
dose of yohimbine suggests that, at levels that would
increase colonic tone, it is likely that yohimbine would
increase perception of colonic stimuli. Nevertheless, it is
conceivable that yohimbine might have a therapeutic
potential, as in acute post-operative ileus or acute
colonic pseudo-obstruction, when reversal of colonic
relaxation or distention is clinically indicated. Such a
pharmacologic approach could be advantageous, since
it may avoid the need for colonic decompression by
colonoscopy. The increase in rectal sensation observed
with yohimbine is also worthy of further study in
conditions associated with rectal sensory de®cits such as
in patients with diabetes mellitus and faecal incontin-
ence unassociated with external anal sphincter dener-
vation.16, 17
In fact, the effects of a2-adrenergic agents on colonic
motor and sensory function need to be further explored
in the context of neurological disorders which may
affect extrinsic afferent and efferent supply to the colon
and rectum. Such diseases include Parkinsonism
[especially those variants associated with autonomic
dysfunction such as Parkinson's plus or multiple
system atrophy (Shy±Drager's syndrome)], multiple
sclerosis, and diabetic autonomic neuropathy.18±20
The role of sympathetic adrenergic dysfunction in
non-neurologic disorders is currently unclear, though
other authors have suggested that sympathetic dys-
function is associated with diarrhoea-predominant
irritable bowel syndrome or slow transit constipa-
tion.21, 22
In summary, these in-depth studies indicate a poten-
tially important, hitherto disregarded and clinically
unexploited mechanism which may signi®cantly alter
the functions of the human colon and rectum. Our
data argue strongly for the continuation of the in-
depth study of the a2-adrenergic mechanism, its role in
colorectal diseases, and its potential as a modulator of
colorectal sensory and motor functions. Such studies
may lead to signi®cant advances in therapy with
agents that are already approved for use in humans
and that have known and generally acceptable toxicity
pro®les.
ACKNOWLEDGEMENTS
Dr Malcolm was funded by the Mayo-Janssen Advanced
Fellowship in GI Motility; Dr Camilleri is funded by NIH
grants 1RO1-DK54681±01 and 1K24±02638±01. This
study was also supported in part by NIH General
Clinical Research Center grant #RR00585 (Physiology
Core).
We thank Mrs. Cindy Stanislav for typing this
manuscript.
This work was presented at the Annual Meeting of the
American Gastroenterological Association in May,
1997 (Gastroenterology 1997; 112: A780).
REFERENCES
1 Camilleri M, Ford MJ. Colonic sensorimotor physiology in
health and its alteration in constipation and diarrhoeal dis-
orders. Aliment Pharm Ther 1998; 12: 287±302.
2 Ritchie J. Pain from distension of the pelvic colon by in¯ating
a balloon in the irritable colon syndrome. Gut 1973; 14: 125±
32.
3 Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA. Altered
rectal perception is a biological marker of patients with irrit-
able bowel syndrome. Gastroenterology 1995; 109: 40±52.
4 Stivland T, Camilleri M, Vassallo M, et al. Scintigraphic mea-
surement of regional gut transit in idiopathic constipation.
Gastroenterology 1991; 101: 107±15.
5 O'Brien MD, Camilleri M, von der Ohe MR, et al. Motility and
tone of the left colon in constipation: a role in clinical practice?
Am J Gastroenterol 1996; 91: 2532±8.
6 Hutchinson R, Grif®ths C. Acute colonic pseudo-obstruction:
a pharmacological approach. Ann R Coll Surg Engl 1992; 74:
364±7.
7 Choi M-G, Camilleri M, O'Brien MD, Kammer PP, Hanson RB.
A pilot study of motility and tone of the left colon in patients
with diarrhea due to functional disorders and dysautonomia.
Am J Gastroenterol 1997; 92: 297±302.
8 Camilleri M, Saslow SB, Bharucha AE. Gastrointestinal sen-
sation: mechanisms and relation to functional gastrointestinal
disorders. In Camilleri M, ed. Gastroenterology Clinics of NA:
Gastrointestinal Motility in Clinical Practice, Vol 25. Phila-
delphia, USA: W.B. Saunders, 1996: 247±58.
9 Bharucha AE, Camilleri M, Zinsmeister AR, Hanson RB.
Adrenergic modulation of human colonic motor and sensory
function. Am J Physiol 1997; 273: G997±1006.
792 A. MALCOLM et al.
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793

10 Malcolm A, Phillips SF, Camilleri M, Hanson RB. Pharmaco-
logical modulation of rectal tone alters perception of distention
in humans. Am J Gastroenterol 1997; 92: 2073±9.
11 Talley NJ, Phillips SF, Wiltgen CM, Zinsmeister AR, Melton LJ.
III Assessment of functional gastrointestinal disease: the bowel
disease questionnaire. Mayo Clin Proc 1990; 65: 1456±79.
12 Zigmond AS, Snaith RP. The hospital anxiety and depression
scale. Acta Psychiatr Scand 1983; 67: 361±70.
13 Hammer HF, Phillips SF, Camilleri M, Hanson RB. Rectal
tone, distensibility, and perception: reproducibility and re-
sponse to different distensions. Am J Physiol 1998; 274:
G584±90.
14 Steadman CJ, Phillips SF, Camilleri M, Haddad AC, Hanson
RB. Variation of muscle tone in the human colon. Gast-
roenterology 1991; 101: 373±81.
15 Ford MJ, Camilleri M, Zinsmeister AR, Hanson RB. Psycho-
sensory modulation of colonic sensation in the human
transverse and sigmoid colon. Gastroenterology 1995; 109:
1772±80.
16 Wald A, Tunuguntla AK. Anorectal sensorimotor dysfunction
in fecal incontinence and diabetes mellitus. Modi®cation with
biofeedback therapy. N Engl J Med 1984; 310: 1282±7.
17 Schiller LR, Santa Ana CA, Schmulen AC, Hendler RS, Har-
ford WV, Fordtran JS. Pathogenesis of fecal incontinence in
diabetes mellitus: evidence for internal±anal±sphincter dys-
function. N Engl J Med 1982; 307: 1666±71.
18 Edwards LL, Quigley EM, Pfeiffer RF. Gastrointestinal dys-
function in Parkinson's disease: frequency and pathophysiol-
ogy. Neurology 1992; 42: 726±32.
19 Ashraf W, Pfeiffer RF, Quigley EM. Anorectal manometry in
the assessment of anorectal function in Parkinson's disease:
a comparison with chronic idiopathic constipation. Movement
Disorders 1994; 9: 655±63.
20 Caruana BJ, Wald A, Hinds JP, Eidelman BH. Anorectal sen-
sory and motor function in neurogenic fecal incontinence.
Comparison between multiple sclerosis and diabetes mellitus.
Gastroenterology 1991; 100: 465±70.
21 Aggarwal A, Cutts TF, Abell TL, et al. Predominant symptoms
in irritable bowel syndrome correlate with speci®c autonomic
nervous system abnormalities. Gastroenterology 1994; 106:
945±50.
22 Altomare D, Pilot MA, Scott M, et al. Detection of subclinical
autonomic neuropathy in constipated patients using a sweat
test. Gut 1992; 33: 1539±43.
a2 -ADRENERGIC CONTROL OF HUMAN COLON 793
Ó 2000 Blackwell Science Ltd, Aliment Pharmacol Ther 14, 783±793