Therapeutic Hypothermia presentation
-
Upload
phoebe-gulling -
Category
Documents
-
view
27 -
download
0
Transcript of Therapeutic Hypothermia presentation

Therapeutic Hypothermia: CAN WE FEED?
By: Phoebe Gulling

Objectives• Become familiar with terminology surrounding the use of
therapeutic hypothermia following cardiac arrest• Become familiar with inclusion/exclusion criteria and
typical protocol• Learn about the role of the medical team and RD• Learn about metabolic changes which occur during
hypothermic state• Learn about various studies surrounding the discussion of
whether or not to feed a patient during a hypothermic state

Terminology• Therapeutic Hypothermia: cooling the body to 32°C -
34°C for 24 hours following cardiac arrest to limit effects of ischemic brain damage like cerebral hypoxia and reperfusion.
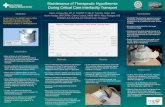
• Induction phase: period of rapid cooling• Maintenance phase: maintenance of target temperature
for 24 hours• Rewarming phase: should occur slowly (0.25-0.5 °C per
hour)
Collins, 2008; Polderman, 2009

Patient Prognosis – Mass (2002)• 55% of hypothermia
group w/ favorable outcome• 39% of normothermia
group w/ favorable outcome• 14% lower death rate 6-
months post-cardiac arrest in hypothermia group
Massachusetts Medical Society, 2002

Inclusion Criteria• In or out of hospital VF, asystole, or PEA cardiac arrest• Requiring CPR and with ROSC• Comatose: defined by GCS <8• Endotracheal intubation w/ mechanical ventilation• Rapid initiation of hypothermia (w/in 6 hours of ROSC)• Hemodynamic stability• Adults >18 years
Massachusetts General Hospital, 2014

Typical Protocol• Initiate cooling ASAP• Use of cooling pads• Set target temperature goal of 33°C
• Maintain hypothermia for 24 hours • Begin rewarming at 24th hour• Rate of less than 0.5°C per hour
• Monitor• Arterial line placed for BP monitoring• Continuous temperature monitor
• Medication for sedation and to prevent shiveringMassachusetts General Hospital, 2014

www.bostonglobe.com

Supportive Care• Medications• Sedatives• Analgesia• Paralytics
• Hemodynamics• MAP of >90mmHg
• Monitor for dysrhythmias
• Prevent infection • Monitor labs for
electrolyte abnormalities• Replete as needed
• Monitor arterial blood gases• Maintain skin integrity• Continuous EEG
monitoringMassachusetts General Hospital, 2014

Dietitian’s Role for Acute Care• Clinical guidelines identify critically ill patients at risk of
malnutrition• Inadequate oral intake• Poor GI absorption• Increased nutritional requirements
• 25-30 kcal/kg recommended• Early enteral feeing to prevent malnutrition• Enhanced wound healing• Reduced incidence of infection• Maintenance of GIT function
Williams, 2014

CAN WE FEED?• Critical illness severity• Age• Nutrition risk screening•Wait for resuscitation• Energy requirements• Formula selection• Enteral access• Efficacy• Determination of tolerance
?Miller, 2011

Recommendations for
feeding during therapeutic
hypothermia are unclear

Metabolic Changes
Polderman, 2009

Metabolic Changes• Hypothermia-induced decreased metabolic rate• Decreased electrolytes during induction• Increased renal excretion• Intracellular shift
• Increased K+ during rewarming• Hyperglycemia during induction• Decreased insulin sensitivity and reduced insulin secretion
• Increased synthesis of glycerol, FFA, ketonic acids, and lactate• Mild metabolic acidosis
Polderman, 2009

Management• More insulin required in induction phase• Decreased requirement in rewarming phase• Maintain glucose <180 mg/dL
• Mg supplementation during induction phase• Repletion of electrolytes during induction• DO NOT replete K+ during rewarming phase
Polderman, 2009

CAN WE FEED?Are enteral feedings tolerated in this
population?

Tolerance• Critically ill at risk for malnutrition• Increased metabolic rate
• Research unclear• Delayed gastric emptying in 70% of mechanically
ventilated• Ileus in 50-80% of critically ill• Gut dysfunction in 60% of outside hospital cardiac
arrest pts.Williams, 2014

Study Highlight – Smith (2011)• Retrospective observational study• Recorded total enteral feed input, total volume gastric
aspirate, and number of vomiting episodes over 72 hours• Absorption of feeds increased w/ temperature• Positive feed balance in 78% of patients during hypothermia
Smith, 2011

Study Highlight – Williams (2014)• Single-center longitudinal cohort analysis• Recorded enteral feeding, vomiting events, and
aspirate volume
Williams, 2014

Study Highlight – Williams (2014)
• Cooling: 83% tolerated some feeds • Significant number intolerant
• Rewarming: 83% tolerated some feeds• Vomiting in 19%
• Normothermia: 91% tolerated • -Almost 100% of feeds
• Recommended reduced rate when 32-34 °C• “Trickle feeds”
Williams, 2014

Conclusion• Therapeutic hypothermia associated with favorable
outcomes• Research unclear • Lower death rate with early enteral feeds• Greater volume of feeds tolerated w/ temperature
increase• Trickle feeds (<10 ml/h) may be tolerated during
cooling• More research needed
• Must continue to monitor for signs/symptoms of intolerance

References• Collins TJ, Samworth PJ. Therapeutic Hypothermic Following Cardiac Arrest: A Review of Evidence. Nursing in
Critical Care. 2008;13(3):144-151.• Massachusetts General Hospital: Critical Care. Therapeutic Hypothermia After Cardiac Arrest: General Guideline.
Updated: March 12, 2014. Retrieved: April 15, 2016. Available at: https://www2.massgeneral.org/stopstroke/pdfs/HypothermiaProtocol.pdf.
• Miller KR, Kiraly LN, Lowen CC, Martindale RG, McClave SA. “CAN WE FEED?” A Mnemonic to Merge Nutrition and Intensive Care Assessment of the Critically Ill Patient. JPEN J Parenter Enteral Nutr. 2011;35(5):643-659.
• Smith C, Nolan J, Williams M. Enteral Feed Absorption During Therapeutic Hypothermia Following Out-of-Hospital Cardiac Arrest. Critical Care. 2011;15(Suppl 1):P377.
• Williams M-L, Nolan JP. Is enteral feeding tolerated during therapeutic hypothermia? Resuscitation. 2014; 85: 1469-1472.
• Lee HK, Lee H, No JM, et al. Factors influencing outcome in patients with cardiac arrest in the ICU. Acta Anasthesiol Scand. 2013; 57: 784-792.
• Massachusetts Medical Society. The Hypothermia After Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346 (8): 549-556.
• Polderman KH, Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009; 37(3): 1101-1120.
• Oshima T, Furukawa Y, Kobayashi M, Sato Y, Nihei A, Oda S. Fulfilling Caloric Demands According to Indirect Calorimetry May be Beneficial for Post Cardiac Arrest Patients Under therapeutic Hypothermia. Resuscitation. 2015;88:81-85.
• Beer R, Fischer M, Dietmann A, Pfausler B, Schmutzhard E. Hypothermia and Nutrition: at Present More Questions Than Answers? Critical Care. 2012;16(Suppl 2):A28.

THANK YOU!