The single sperm curling test, a modified hypo-osmotic swelling test, as a potential technique for...
-
Upload
ali-ahmadi -
Category
Documents
-
view
248 -
download
36
Transcript of The single sperm curling test, a modified hypo-osmotic swelling test, as a potential technique for...

FERTILITY AND STERILITY@ Vol. 68, No. 2, August 1997 Copyright o 1997 American Society for Reproductive Medicine Published by Elsevier Science Inc.
Printed on acid-free paper in U. S. A.
The single sperm curling test, a modified hypo-osmotic swelling test, as a potential technique for the selection of viable sperm for intracytoplasmic sperm injection*
Ali Ahmadi, MSc. Soon-Chye Ng, M.D.?
Department of Obstetrics and Gynaecology, National University of Singapore, Singapore
Objective: To develop a technique for the selection of viable sperm for intracytoplasmic sperm injection (ICSI), based on the phenomenon of sperm tail curling in a hypo-osmotic environment, through modification of the hypo-osmotic swelling test.
Design: Individual sperm were exposed to single sperm curling (SSC) medium and then injected into hamster oocytes to study the effect of SSC medium on fertilization.
Setting: All materials were collected from the National University Hospital in Singapore. Patient(s): Semen of proven donors and hamster oocytes with intact zonae were used. Intervention(s): ICSI and the SSC test. Main outcome measure(s): Sperm head decondensation and male pronucleus formation. Result(s): Sperm head decondensation and male pronucleus formation were present in 59.4%
and 42.4%, respectively, of the oocytes injected with sperm that had been exposed to SSC medium. These rates were 70% and 46.8%, respectively, when the sperm were washed thor- oughly after exposure to SSC medium. In the control group (sperm that were not exposed to SSC medium), these rates were 68.8% and 46.2%, respectively.
Conclusion(s): The SSC test is useful for the selection of viable sperm for ICSI. It allows the behavioral study of a single sperm in hypo-osmotic conditions. Thorough washing of the exposed sperm is important. This procedure would be of benefit especially in testicular biopsies or very severe cases of low sperm count in which only a few sperm are found among many other cells and artifact. (Fertil Sterila 1997;68:346-50. 0 1997 by American Society for Reproductive Medicine.)
Key Words: Hypo-osmotic swelling (HOS) test, ICSI, human sperm, hamster oocyte, sperm head decondensation, male pronucleus formation
The treatment of male infertility recently has un- dergone a major revolution with the development of intracytoplasmic sperm injection (ICSI). This tech- nique circumvents all natural barriers to sperm pen- etration and removes all biologic selection from the process, including binding of the sperm to the zona pellucida (ZP) and fusion of the sperm with the oolemma. Using this method, any type of sperm (e.g., whole sperm, sperm at various developmental
Received January 21,1997; revised and accepted April 23,1997. * Supported by Research Grant No. RP3940336 of the National
University of Singapore. t Reprint requests: Soon-Chye Ng, M.D., Department of Obstet-
rics and Gynaecology, National University of Singapore, Lower Kent Ridge Road, Singapore 119074, Singapore (FAX: +65-779- 4753; e-mail: [email protected]).
346
stages, heads or nuclei, immotile, dead, or grossly defective sperm) can be injected.
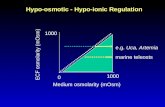
The hypo-osmotic swelling (HOS) test was intro- duced as a clinical means of measuring the func- tional integrity of the sperm membrane (1). This test is based on the semipermeability of the intact cell membrane, which allows the sperm to swell under hypo-osmotic conditions. On exposure of the sperm to hypo-osmotic conditions, an influx of water results in swelling of the cytoplasmic space and curling of the sperm tail fibers. The major problem in working with epididymal and testicular sperm is difficulty in differentiating live and dead sperm, because most of the sperm are immotile. The HOS test has been used by several researchers to differentiate live and dead sperm for ICSI (2, 3). In all procedures, approxi- mately 200,000 sperm were exposed to HOS medium
0015-0282/97/$17.00 PI1 SO0150282(97)00204-5

for 1 hour at 37°C. However, because most testicular samples have a low sperm count, performing the con- ventional HOS test is impossible. Moreover, diluting the sperm with HOS medium may result in the loss of sperm, leaving inadequate sperm for ICSI. In this investigation, we developed the single sperm curling @SC) test to aid in the selection of viable sperm in cases of very low sperm count. Before clinical appli- cation of the SSC test, we investigated its effect on fertilization in an animal model using a hamster ICSI assay (4).
The objective of this study was to modify the con- ventional HOS test to reveal the condition of individ- ual sperm in a hypo-osmotic environment and to allow the selection of viable sperm for ICSI in cases of very low sperm count by observing the phenome- non of tail curling under hypo-osmotic conditions. We evaluated sperm head decondensation and male pronucleus formation within hamster oocytes.
MATERIALS AND METHODS
Preparation of the Gametes
Frozen-thawed semen samples from proven do- nors were used for this study. The sperm were pro- cessed by the discontinuous Percoll gradient (Phar- macia Biotech, Uppsala, Sweden) (40%, 70%, and 90%) separation method. The semen samples were layered on top of the Percoll gradients. After centrif- ugation at 100 X g for 20 minutes, the whole column of sperm and the Percoll were discarded, and the pellet was washed three times with fresh medium at 350 x g for 5 minutes. The supernatant was re- moved and the pellet was introduced into fresh Earle’s balanced salt solution (EBSS) (GIBCO, Grand Island, NY). Incubation was carried out at 37°C and in 5% COP in air for 1 hour. Superovulation and recovery of the hamster oocyte has been de- scribed in detail elsewhere (5).
Single Sperm Curling Test
Single sperm curling medium was prepared by adding 0.5 mL of HEPES-buffered EBSS to 1 mL of mini-& water and adjusting the osmolarity to about 100 mOsmkg. A single sperm was aspirated tail- first into the microinjection pipette using the Na- rishige microinjector (M16; Narishige, Tokyo, Ja- pan). It then was exposed to SSC medium (5 PL) for 5 to 10 seconds. Immediately after contacting SSC medium, the tail began to coil. The sperm then was transferred into iso-osmotic HEPES-buffered me- dium (10 PL) and washed several times. The injec- tion pipette also was washed thoroughly by repeated aspiration of fresh medium to ensure removal of the solutions carried over from the SSC droplet. Finally,
thesperm was moved into a droplet of 10% polyvinyl- pyirolidone (PVP) d an rinsed several times until the tail almost straightened (ICSI-SSC washed group). In some experiments, the sperm was injected into the oocyte immediately after exposure to SSC me- dium without any further washing (ICSI-SSC un- washed group). In the control group, ICSI was per- formed as a standard procedure. In all control and experimental groups, the sperm tail was struck just before injection into the ooplasm. There was a sham control in which the oocyte was injected with SSC medium only (no sperm).
Microinjection Procedure
Microtools were made by drawing glass capillary tubes with the horizontal Sutter Puller (P-87; Sutter Instruments, San Rafael, CA), and were processed further on a De Fonbrune-type microforge (MF-1; Technical Products International, Inc., St, Louis, MO) and a Narishige microgrinder (EG-4; Narishige, Tokyo, Japan). The microinjection pipette had an internal diameter of 5 to 6 pm, an external diameter of 7 to 9 pm, and a bevel angle of 40”, with a sharp spike on the tip. The holding pipettes had an exter- nal diameter of 80 pm and an internal diameter of 40 pm.
Metaphase II oocytes were held under negative pressure by the holding pipette with the polar body at the 6- or 1Zo’clock position. The microinjection pipette, which had aspirated a single sperm tail first, was pushed through the ZP and into the cytoplasm of the oocyte at the 3-o’clock position. After punctur- ing and breaking the oolemma by sucking in a mi- nute amount of cytoplasm, a single spermatozoon was injected into the ooplasm with a minimal vol- ume of sperm-PVP medium. The injection pipette was removed slowly and the oocyte was released from the holding pipette.
Evaluation of the Oocytes
Eighteen to 20 hours after injection, the oocytes were checked for formation of 2 pronuclei and were fixed in 1% glutaraldehyde, stained with aceto- orcein, and examined for sperm head decondensa- tion and male pronuclear formation under x100 magnification. The state of the sperm nucleus within the cytoplasm of the oocyte was classified as one of five stages, as shown in Figure 1: stage a was an intact sperm nucleus; stage b was a decondensing sperm nucleus; stage c was a completely decon- densed sperm nucleus; stage d was a round sperm nucleus enclosed within a nuclear membrane; and stage e was an enlarged nucleus with nucleoli. Ab indicated abnormal decondensation.
Vol. 68, No. 2, August 1997 Ahmadi and Ng SSC test for selection of viable sperm 347

Figure 1 Development of human sperm heads to male pronuclei within hamster oocyte: stage a, intact sperm head (X 1,000); stage b, decondensing sperm head (X 1,000); stage c, completely decon- densed sperm head (~1,100); stage d, the sperm nucleus is round and the nuclear membrane has formed (~1,100); stage e, the nu- cleus has enlarged and nucleoli have appeared (X 1,000); Ab, ab- normal decondensation has occurred (X 1,000).
Statistical Analysis
Frequencies of sperm head decondensation and male pronuclear formation in the treatment and con- trol groups were compared using a Student’s t-test, and a P value of 0.05 was considered statistically significant. The calculations were made using the SPSS software package (SPSS, Inc., Chicago, IL) on a personal computer.
RESULTS
Our preliminary observations showed that expo- sure of viable single sperm to SSC medium with an osmolarity of 100 mOsm&g resulted in curling of the tail. We believed this technique could be useful in the selection of viable sperm in very severe cases of low sperm count, as well as in testicular and epididy- ma1 samples. We studied its effect on fertilization before clinical application. Table 1 summarizes the results of our experiment in which the sperm were exposed to SSC medium followed by either washing (ICSI-SSC washed group) or no further washing
(ICSI-SSC unwashed group) before ICSI. Sperm head decondensation and male pronuclear formation were evaluated within the hamster oocyte. In the experimental groups, 133 and 119 oo- cytes underwent ICSI, resulting in 6% and 11% degeneration rates in the ICSI-SSC washed and ICSI-SSC unwashed groups, respectively. Decon- densation of the sperm head and male pronuclear formation were seen in 88 (70%) and 61 (48.8%), respectively, of the ICSI-SSC washed group, com- pared with 63 (59.4%) and 45 (42.4%), respectively, of the ICSI-SSC unwashed group (Table 2). There was a significant difference in sperm head deconden- sation between these two groups (P < 0.01). How- ever, there was no difference in male pronuclear for- mation (P > 0.01). In the control group, of 114 oocytes injected with sperm, 8 (7%) were damaged during the procedure. Of the rest, 68.8% and 46.2% had sperm head decondensation and male pronu- clear formation, respectively. There were no signifi- cant differences in sperm head decondensation (P > 0.01) and male pronuclear formation (P > 0.01) between the experimentals and control groups. Sham injection resulted in 23.5% parthenogenic acti- vation of oocytes after the injection of SSC medium only (no sperm).
DISCUSSION
On exposure of the cell plasma membrane to a hypo-osmotic solution, water enters the membrane until an iso-osmotic pressure is attained. Because of the influx of fluid, the volume of the cell increases and the cell membrane expands, causing bulging of the plasma membrane. In the case of sperm, the plasma membrane surrounding the tail fibers ap- pears to be more loosely attached than the mem- brane surrounding the principal portion, so that the tail region shows the swelling most clearly. When the plasma membrane swells (balloons) under hypo- osmotic conditions, curling and bending of the tail fibers occurs within the plasma membrane. Curling is due to ballooning of the plasma membrane; there- fore, a sperm that shows a curled tail is swollen. A
Table 1 Results of the Single Sperm Curling Test on Sperm Head Decondensation After Injection Into the Hamster Oocytes
Group Injected
No. of eggs Sperm head decondensation stage
Cultured Activated* e d C b a Abnormal
ICSI-SSC washed 133 125 5 61 4 10 13 35 2 ICSI-SSC unwashed 119 106 4 45 5 6 7 40 3 ICSI-control 114 106 3 49 3 9 12 31 2 Sham injection? 86 85 20
* Oocytes with one pronucleus seen at 18 to 20 hours after ICSI.
348 Ahmadi and Ng SSC test for selection of viable sperm
t Injected with SSC medium only (without sperm).
Fertility and Sterility@

Table 2 Sperm Head Decondensation and Male Pronucleus Formation After Treatment of Sperm With Single Sperm Curling Medium Before Microinjection Into Hamster Oocytes
Group
No. of oocytes No. of oocytes with decondensed with male
sperm heads*? pronuc1ei.t
ICSI-SSC washed4 88/125 (70.0) 61/125 (48.8) ICSI-SSC unwasheds 63/106 (59.4) 45006 (42.4) ICSI-controlg 73/106 (68.8) 49/106 (46.2)
* Significant difference in sperm head decondensation between groups 1 and 2 (P < 0.01).
t No significant difference in sperm head decondensation be- tween groups 1 and 3 (P > 0.01).
$ No significant difference in male pronucleus formation be- tween groups 1,2, and 3 (P > 0.01).
9 Values in parentheses are percentages.
sperm with a chemically and physically intact mem- brane shows tail curling under hypo-osmotic condi- tions, whereas a sperm with a damaged membrane does not.
Supravital staining techniques are based on the principle that dead cells with damaged membrane take up stain (dye exclusion). This sperm viability staining technique results in the death of the sperm, making this test unsuitable for the selection of live sperm for ICSI. It should be noted that viability staining is used as an indicator of the physical integ- rity of the sperm membrane, whereas the HOS test indicates both the physical and the biochemical in- tegrity of the sperm plasma membrane (6). Although a physically disrupted membrane will not swell, an undisrupted membrane may not be biochemically in- tact. This property makes the HOS test more inclu- sive in the selection of live sperm for ICSI.
Short-term exposure of sperm to HOS solution, which is not strong enough to cause rupture of the membrane and despiralization, apparently is not too injurious to the motility mechanism. Drevius and Eriksson (7) observed that sperm greatly swollen as a result of exposure to HOS medium retained their motility. Further, they revealed by electron micro- scopic investigation that this structure is able to ex- hibit contractile activity in spite of its abnormal form. They concluded that this movement could oc- cur because all portions of the convolutions of the coil are not in close contact with the cell membrane. Their investigation also showed that the absence of movement in some swollen sperm is not due to cell death, because these sperm uncoil and recommence flagellation after exposure to isotonic medium. How- ever, Chang and Thorsteinsson (8) found that insem- ination of HOS-treated rabbit spermatozoa reduced the fertilization rate by only 15% when compared with control spermatozoa.
Casper et al. (2) used the standard HOS test for
the selection of viable sperm for ICSI in cases of sperm with 0% motility. They incubated approxi- mately 200,000 sperm in HOS solution (75 mM of fructose and 25 mM of sodium citrate) at 37°C for 1 hour. The curled sperm then were aspirated and rinsed several times in culture medium and PVP before ICSI. This resulted in significantly improved fertilization and cleavage rates of 43% and 39%, re- spectively, when compared with a randomly selected group (26% and 23%, respectively). In another study, the HOS test was used for immobilization of sperm before ICSI (3).
Apart from motility, the major problem in testicu- lar and epididymal samples is low sperm harvest. Further, tissue usually contains red blood cells and other blood components. Exposure to HOS solution may result in the lysis of cells, causing them to re- lease their contents into the suspension medium. The lysed cells and their released components could be picked up during sperm selection and injected into the ooplasm. This may affect the outcome, in- cluding fertilization and development before and after implantation. This might be a reason that preg- nancy rates after ICSI with testicular and epididy- ma1 sperm are low.
Another problem with testicular and epididymal sperm is their high rate of abnormal morphology. Further, exposure to HOS medium changes the mor- phology of sperm. Therefore, it could be difficult to select morphologically normal sperm after exposure to HOS medium. To overcome these problems, we have developed the SSC test for the selection of via- ble sperm for ICSI. In this technique, individual morphologically normal sperm are aspirated by mi- croinjection pipette and exposed to SSC solution for a brief period, so sperm membrane damage is minimal and the chance of selecting morphologically normal sperm is greater because individual sperm are se- lected before exposure.
To prepare SSC medium, HEPES-buffered EBSS is diluted with mil1i-Q water. Culture medium is used to prepare SSC medium, to avoid exposure to addi- tional factors present in conventional HOS medium that may be harmful to the sperm, which will be de- posited into the ooplasm. In this study, sperm head decondensation and male pronuclear formation were monitored after the injection of human sperm exposed to modified HOS medium into the hamster oocyte. Our results show that applying this technique does not affect sperm head decondensation and male pro- nuclear formation. Of interest is the injection of SSC medium into the ooplasm (sham injection; Table 1) revealed that this medium does not have any adverse effect on the development of the hamster oocyte; more than 20% of the injected oocytes underwent the acti- vation process and developed female pronuclei, and
Vol. 68, No. 2, August 1997 Ahmadi and Ng SSC test for selection of viable sperm 349

the degeneration rate was approximately 1%. Fur- ther, the injection of unwashed sperm exposed to SSC medium did not influence male pronuclear formation, although sperm head decondensation was lower. In contrast, the degeneration rate in the ICSI-SSC un- washed group was higher. This could be due to either the elimination of PVP, which somehow affected smooth control of sperm during injection, or curling, which resulted in difficulty of movement inside the microinjection needle.
In conclusion, the SSC test is useful for the selec- tion of vital sperm for ICSI. It also allows the behav- ioral study of single sperm in hypo-osmotic condi- tions. This procedure would be of special benefit in testicular biopsies or very severe cases of low sperm count in which only a few sperm are found among many other cells and artifact. This test is very easy to perform. It has no influence on oocyte develop- ment and supports sperm head decondensation and male pronuclear formation. The curls of the sperm with intact membranes are easy to identify. We are currently using this technique successfully in our clinical cases.
Acknowledgments. We thank Ariff Bongso, DSc., of the Depart- ment of Obstetrics and Gynaecology, National University of Sin-
gapore, for his support. We also thank the staff of the micromanip- ulation, IVF, and andrology laboratories for their help.
1.
2.
3.
4.
5.
6.
7.
8.
REFERENCES
Jeyendran RS, Van der Ven HH, Perez-Pelaez M, Crabo G, Zaneveld LID. Development of an assay to assess the func- tional integrity of the human sperm membrane and its rela- tionship to other semen characteristics. J Reprod Fertil 1984;70:219-28. Casper RF, Meriano JS, Jarvi KA, Cowan L, Lucato ML. The hypo-osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete as- thenozoospermia. Fertil Steril 1996;65:972-6. Chida S. Immobilized and hypo-osmotic swollen spermatozoa on intracytoplasmic sperm injection. J Assist Reprod Genet 1995; 12:453-5. Ahmadi A, Bongso A, Ng SC. Intracytoplasmic injection of human sperm into the hamster oocyte (hamster-ICSI assay) as a test for fertilizing capacity of the severe male factor sperm. J Assist Reprod Genet 1996; 13:647-51. Ahmadi A, Bongso A, Ng SC. Induction of acrosome reaction in human sperm by exposure to an electrical field. Arch An- drol 1997;38:57-65. Schrader SM, Platek SF, Zaneveld LJD, Perez-Pelaez M, Jey- endran RS. Sperm viability: a comparison of analytical meth- ods. Andrologia 1986; 18:530-B. Drevius LO, Eriksson H. Osmotic swelling of mammalian spermatozoa. Exp Cell Res 1965;42:136-56. Chang MC, Thorsteinsson T. Effects of osmotic pressure and hydrogen-ion concentration on the motility and fertilizing ca- pacity of rabbit spermatozoa. Fertil Steril 1958;9:510-20.
360 Ahmadi and Ng SSC test for selection of viable sperm Fertility and Sterility@