The Journal of Diabetic Foot Complications Open access ...The Journal of Diabetic Foot...
Transcript of The Journal of Diabetic Foot Complications Open access ...The Journal of Diabetic Foot...

Open access publishing The Journal of Diabetic Foot Complications
8
Non-surgical treatment for foot deformities and lesions in patients with diabetes mellitusAuthors: Dong Yu*, Xing Si-yuan2, Wang Ying3, Wang Fu-sheng1, Wang Yu1, Xu Xu-ying1, Wang Guang-yu1, You Wei1
The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14 © All rights reserved.
Key words: Diabetic Foot, Foot Deformities, Foot Lesions, Foot Orthoses
Corresponding author* Dong Yu
Surgeon Ulcerous Vascular Surgical Department Beijing Hospital of Traditional Chinese Medicine affiliated to Capital Medical University Beijing 100010, China Email: [email protected]
Affiliations1 Wang Fu-sheng, Wang Yu, Xu Xu-ying, Wang Guang-yu, You Wei
Beijing Hospital of Traditional Chinese Medicine affiliated to Capital Medical University, Beijing 100010, China
2 Xing Si-yuanChina Quality Certification Center, Beijing 100070, China
2 Wang YingBeijing Haidian section of Peking University Third Hospital, Beijing 100080, China
Abstract:Patients with diabetes mellitus (DM) are likely to also have a variety of deformities and lesions in the feet such as ingrown toenails, hallux valgus, hammertoes, flat feet, and cracked feet. Left untreated these mild deformities and lesions frequently and gradually increase in severity, causing paronychia, callus, and corns. These often lead to pressure ulcer and foot infections. This acquired condition of poor blood glucose control frequently predisposes these patients to a high risk of post-operative infection and delayed wound healing; therefore, these patients are regarded as poor surgical candidates. In this study we review the option of non-surgical management for these patients with the goal of alleviating foot deformities and heel fissures, and reducing the incidence of foot ulcer and infection.
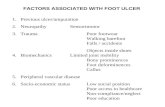
Diabetic foot ulcer (DFU) is a serious complication of diabetes that is usually marked with a long healing period, high disability rate, and great medical expense.1 Due to peripheral neuropathy and angiopathy patients with DM are prone to present with a variety of deformities and lesions in their feet. These include hammertoes, Charcot foot, cracked/fissuring skin, etc.2,3 Previous studies indicated that toe and foot deformities are the major causes of abnormally increased plantar pressure, which is the early predictor for foot ulcer.4,5 In addition, untreated ingrown toenails and cracked feet (fissures) also lead to foot ulcer and infection.6,7
Surgical management has been shown to be effective for correcting foot deformities and treatment of these lesions. However, most of these surgical procedures are operated on
soft tissues, joints, and bones.8,9,10 With poor blood glucose control or insufficient perfusion in the lower limb, a surgical option is often deferred by the attending physician, or patients themselves, after consideration of post-operative complications such as infection or delayed wound healing.11 Even with mild lesions, if left untreated, the gradual deterioration of a foot deformity will subsequently decrease the foot weight-bearing area, thus abnormally increasing plantar pressure. This then causes callus, corn, paronychia, and foot ulcer development.12 Foot orthoses can treat foot deformities and lesions with the goal of reducing the incidence of foot ulcer.13,14,15,16 In this study we review the common foot deformities and lesions, as well as conservative management options.
INTRODUCTION

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
9
Common Foot Deformities and Lesions in Patients with Diabetes Mellitus1. Skin Lesions
Diabetic peripheral neuropathy (DPN) is usually associated with a skin nutrition disorder, subsequently resulting in lowering of skin temperature, skin paleness, sweating deficiency, and dry skin. Left untreated, dry and cracked feet will occur, with eventual development of foot ulcer (Figure 1).
2. Nail and Toe DeformitiesDPN is usually accompanied by sensory
disturbance and movement disorder in feet. Due to decreased pain sensation, patients may not realize that unfitted shoes can lead to the toenails, hallux, and lesser toes being constantly under significant pressure. This causes the sides or corners of the toenail to be forced into the skin at the end or side of the toe, leading to ingrown nail and paronychia (Figure 2). Furthermore, the
hallux is bent outward and the first metatarsal head is bent inward, and the lesser toe is bent inward and the fifth metatarsal head is bent outward toward the midline of the body leading to hallux valgus (Figure 3) and little toe varus (Tailor's Bunion) (Figure 4), respectively. Due to uncoordinated movement of joints and muscle tendons, the joints of toes may be dislocated, and hammertoe, mallet toe, or claw toe may occur.
Figure 1. Heel fissure.
Figure 2. Ingrown nail.
Figure 3. Hallux valgus.
Figure 4. Little toe varus (Tailor's Bunion).

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
10
Hammertoe is defined as downward bending of the proximal interphalangeal joints of a toe (Figure 5), and mallet toe is defined as downward bending of the distal interphalangeal joints of a toe (Figure 6). Claw toe is defined as downward bending of both the proximal and distal interphalangeal joints (Figure 7).
3. Foot Arch DeformitiesIf left untreated, joint and muscle tendon
deformities and lesions often lead to the development of flat feet. Flat feet is defined as flattening of the arch on the inside of the feet, allowing entire soles of the feet to have contact with the floor when in a standing posture. 4. Foot and Ankle Deformities
Neuropathic arthropathy, usually known as Charcot foot, refers to progressive degeneration of the weight bearing joints, a process marked by bone destruction, bone resorption, and eventual deformity (Figure 8). If the pathological process is left unnoticed and untreated, it can develop into joint deformities, ulcers, infection, loss of function, and in the worst-case scenario, amputation or even death.
Figure 5. Hammertoe.
Figure 8. Charcot foot.
Figure 6. Mallet toe.
Figure 7. Claw toe.

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
11
Foot Orthoses1. Silicone Gel Heel Protector
This soft medical silicone gel product helps to protect the skin against peeling and cracking (Figure 9).
2. Ingrown Toenail BracingThe toenail strip is comprised of a thin and
flexible material with good elasticity. It is bonded across the surface of the ingrown toenail to apply a gentle and persistent force that straightens the curve of the toenail. The toenail strip gradually lifts each side of the nail reducing its pressure against the skin. When pressure from each side of the toenail is reduced, the ingrown toenail is corrected (Figure 10).
3. Hallux Valgus CorrectorThe hallux valgus corrector applies a 3-point
pressure system. Adjustable toe strap and hinge realign the big toe and stabilize the foot arch,
helping to reduce the hallux valgus angle for gradually relieving the hallux valgus deformity (Figure 11).
4. Lesser Toe SeparatorThis soft medical silicone gel product helps
to protect the lesser toe and the fifth metatarsal from knocking and bumping to restore the normal alignment of toe shape (Figure 12).
Figure 11. Hallux valgus corrector.
Figure 10. Ingrown toenail bracing.
Figure 9. Silicone gel heel protector.
Figure 12. Lesser toe separator.

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
12
5. Toe StraighterThis is designed for the correction of
hammertoe, mallet toe, claw toe, and overlapping toes. The adjustable, cotton-covered elastic sleeve holds the toe in the proper position as the attached pad cushion separates adjacent toes and protects the ball of foot (Figure 13).
6. Orthotic Arch Support Insole and Diabetic Shoes
These are designed to provide stable support for hindfoot, midfoot, and forefoot to evenly distribute body weight across the foot. Doing this avoids persistent painful pressure points, and finally minimizes the risk of skin ulcers for diabetics (Figure 14 and 15).
7. Diabetic Walking BootCharcot foot is usually accompanied by
severe deformities of the foot and ankle, including collapse of the midfoot arch and/or instability of the ankle and hindfoot. Early correction is recommended to limit morbidity. The diabetic walking boot is designed to support, or stabilize, the foot to minimize weight-bearing and deformity on the affected foot/ankle (Figure 16).
Figure 15. Diabetic shoes.
Figure 16. Diabetic walking boot.
Figure 13.Triple toe straighter.
Figure 14. Orthotic arch support insole.

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
13
SUMMARYDiabetic patients with lower limb peripheral
neuropathy are prone to developing foot deformities and lesions. For patients who cannot tolerate, or refuse to accept surgical corrections, foot orthoses should be considered. A comprehensive assessment of the foot function is required, including the range of joint motion, strength of the muscles, position of the bones when standing, and gait. Nocturnal application of a silicone gel heel protector, hallux valgus corrector, lesser toe separator, and toe straighter are optimal for patient convenience. Orthotic arch support insole and diabetic shoes are fundamental treatments that should be applied on a daily basis. Patients need to regularly clean the orthoses with mild soap and rinse thoroughly with water. They should be dried before use. Foot
orthoses are usually prescribed with rehabilitative training, such as a program with stretching and strengthening exercises to improve the posture and alignment. Finally, foot deformities and lesion correction are long-term problems; patients should be advised to visit an orthopedic surgeon or podiatrist regularly until foot orthoses are fitted for proper functioning. In some cases, small adjustments are needed.
Conflict of Interests: The authors declare there is no conflict of interests regarding the publication of this article.
Acknowledgments: The authors thank Wuyang Yang for his English editing and Yinuo Li for drawing pictures of this manuscript.
References
1. Brem H, Sheehan P, Rosenberg HJ, Schneider JS, et al. Evidence-based protocol for diabetic foot ulcers. Plast Reconstr Surg. 2006 Jun;117(7 Suppl):193S-209S; discussion 210S-211S.
2. Rogers LC, Frykberg RG, Armstrong DG, Boulton AJ, et al. The Charcot foot in diabetes. J Am Podiatr Med Assoc. 2011 Sep-Oct;101(5):437-446.
3. Tang UH, Zügner R, Lisovskaja V, Karlsson J, et al. Foot deformities, function in the lower extremities, and plantar pressure in patients with diabetes at high risk to develop foot ulcers. Diabet Foot Ankle. 2015 Jun 17;6:27593.
4. Bus SA, Maas M, de Lange A, Michels RP, Levi M. Elevated plantar pressures in neuropathic diabetic patients with claw/hammer toe deformity. J Biomech. 2005 Sep;38(9):1918-1925.
5. Ledoux WR, Shofer JB, Cowley MS, Ahroni JH, et al. Diabetic foot ulcer incidence in relation to plantar pressure magnitude and measurement location. J Diabetes Complications. 2013 Nov-Dec;27(6):621-626.
6. Yu X, Yu GR, Chen YX, Liu XC. The characteristics and clinical significance of plantar pressure distribution in patients with diabetic toe deformity: a dynamic plantar pressure analysis. J Int Med Res. 2011;39(6):2352-2359.
7. Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015 May 6;10(5):e0124446.
8. Harmonson JK, Harkless LB. Operative procedures for the correction of hammertoe, claw toe, and mallet toe: a literature review. Clin Podiatr Med Surg. 1996 Apr;13(2):211-220.
9. Karaca N, Dereli T. Treatment of ingrown toenail with proximolateral matrix partial excision and matrix phenolization. Ann Fam Med. 2012 Nov-Dec;10(6):556-559.
10. Cassinelli SJ, Herman R, Harris TG. Distal Metatarsal Osteotomy for moderate to severe Hallux Valgus. Foot Ankle Int. 2016 Oct;37(10):1137-1145.
11. Parisi MC, Moura Neto A, Menezes FH, Gomes MB, et al. Baseline characteristics and risk factors for ulcer, amputation and severe neuropathy in diabetic foot at risk: the BRAZUPA study. Diabetol Metab Syndr. 2016 Mar 17;8:25.

Open access publishing The Journal of Diabetic Foot Complications, 2017; Volume 9, Issue 1, No. 2, Pages 8 - 14
14
12. Fernando ME, Crowther RG, Pappas E, Lazzarini PA, et al. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: a meta-analysis of observational studies. PLoS One. 2014 Jun 10;9(6):e99050.
13. Boulton AJ. Pressure and the diabetic foot: clinical science and offloading techniques. Am J Surg. 2004 May;187(5A):17S-24S.
14. Actis RL, Ventura LB, Lott DJ, Smith KE, et al. Multi-plug insole design to reduce peak plantar pressure on the diabetic foot during walking. Med Biol Eng Comput. 2008 Apr;46(4):363-371.
15. Bus SA, Van Deursen RW, Kanade RV, Wissink M, et al. Plantar pressure relief in the diabetic foot using forefoot offloading shoes. Gait Posture. 2009 Jun;29(4):618-622.
16. Bowling FL, Reeves ND, Boulton AJ. Gait-related strategies for the prevention of plantar ulcer development in the high risk foot. Curr Diabetes Rev. 2011 May;7(3):159-163.
References (continued)