The Implication of Teamwork and Communication on ICU Patient ...
-
Upload
changezkn -
Category
Health & Medicine
-
view
2.196 -
download
1
description
Transcript of The Implication of Teamwork and Communication on ICU Patient ...

The Implication of Teamwork and Communication on ICU Patient Discharge
Process
Frances Lin (PhD Candidate)Professor Wendy ChaboyerProfessor Marianne Wallis
School of Nursing & Midwifery Research Centre for Clinical and Community Practice Innovation
Griffith University, Gold Coast, Australia

Better teamwork was found to be associated with less mistakes, decreased LOS, reduced cost, and increased patient safety (Jain et al., 2006; Nemeth, et al., 2006; Pronovost et al., 2003;Salas & Cannon-Bowers, 2000; Sims, Salas & Burke, 2004).
Sub-optimal communication among team members was found to be associated with increased adverse events (Pronovost et al., 2002).
Poor communication between doctors and nurses was associated with preventable adverse events (Donchin et al., 1995).
Poor clinical handover was associated with increased mistakes (Jagsi et al, 2005), preventable adverse events (Petersen, 1994) and critical incidents (Sabir et al., 2006).
The Impact of Teamwork and Communication on Patient Safety

A literature review of organisational, individual and teamwork factors contributing to THE ICU discharge process (Lin, Chaboyer, & Wallis, 2009)
Organisational Factors
Guidelines, policiesResource availability Flow and performance
Teamwork FactorsCommunicationCoordination
StructureLeadership
ICUDischarge
Patient FactorsClinical conditionsCommunication
Personality and social factors
IndividualeFactors Knowledge/experience,
Decision making Skill mix
Use/not use protocols

Aim of The Study To describe ICU patient discharge process in an Australian
metropolitan hospital in order to make recommendations for clinical practice improvement.
This research was the first phase of a larger action research project - Enhancing Intensive Care Unit discharges through multidisciplinary approaches. Phase 2 and 3 of the larger study focused on implementing and evaluating an improved ICU patient discharge process.

Research Questions
1. What is the ICU patient discharge process?
2. What are the factors contributing to the ICU patient discharge process?
3. How are discharge decisions made in the ICU patient discharge process and who are the main decision-makers?
4. What roles, responsibilities does each member play in the discharge process and how do the team members interact?
5. What are the vulnerabilities in this process that may present risks to patient safety?

Methodology Qualitative research. Theoretical underpinnings: Distributed Cognition (Hutchins, 1999) and
Activity Theory (Engestrom, 1987).
Methods: Cognitive ethnography: using ethnographic data collection
techniques (Williams, 2006).
Setting: A large Australian metropolitan tertiary public teaching hospital with a level 3 ICU was selected.
Participant recruitment: ICU and ward. Ethics approval was obtained and all participants gave written
consent.

Activity Theory
Rules Division of LabourCommunity
Tools
Subject Objective Outcome
(Engestrom, 1987)

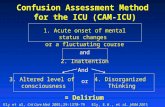
Distributed Cognition
The ICU discharge process is a cognitive process which involves multidisciplinary teams.
The elements of Distributed Cognition: Cognitive process is distributed among members of the group. Team members interact with each other in a meaningful context. Team members interact with artefacts (tools, discharge decision-
making principles). (Hutchins, 1999)

Data Collection
Field work: Participants recruitment. Observations. One on one semi-structured interviews. Contact summaries. Field notes.
Examining/collecting existing documents. Demographic data sheet. Hospital database.

Data Analysis
Preliminary data analysis during data collection: Managing data. Contact summaries and case summaries.
Transcribing data: checking transcripts against audio tape files. Coding, recoding, and recoding. Synthesising codes. Looking for patterns and themes. Data triangulation.

Figure - Activity Theory in ICU patient discharge process adopted from Engestrom (1987)
Rules
Subject
Tools
Objective
Community
Division of Labour
Discharge summariesComputer programs for bed management
Conflicting objectives across departments
RoutinesGuidelines and policiesCapacity alert
Bed cleanersDischarge script
Outcome
Distrusting relationships, teamwork, communication
ICU and ward doctors, nurses, ward clerks, etc
Findings – Description of The ICU Discharge Process

Themes & Subthemes (on teamwork and communication)
Communicating ineffectively among teams and departments Barriers of ICU to ward nursing handover. Communicating ineffectively between departments. Communicating insufficiently between medical and nursing teams
within departments. Working collaboratively to optimise the discharge process
Working beyond team and departmental boundaries for optimised discharge.
Pushing the discharge process forward. Nurses safe-guarding the discharge process to improve
communication among teams. Supporting inexperienced team members.

DiscussionSub-optimal communication may contribute to adverse events, and
discharge delays ICU to ward nursing handovers – followed a strong routine but need
standardised protocol and structure as suggested by the Australian Commission on Safety and Quality in Health Care (2010) and Australian Resource Centre for Healthcare Innovations (2009).
Tools’ design and use issues - such as computer programs were not used effectively to communicate vital information timely. The use of some tools was found to optimise coordinated patient care (Maloney, Wolfe, Gesteland, Hales, & Nkoy, 2007; Nicholls & Young, 2007).
The poor communication may have contributed to discharge delays .
The lack of interdisciplinary communication between doctors and nurses in ICU and on the wards may have patient safety implications (Alvarez & Coiera, 2006; Donchin et al. 1995; Nadzam, 2009; The Joint Commission, 2007).

Discussion
Collaborative teamwork optimised the discharge process Collaborative teamwork shortened ICU discharge delays, which
improved the efficient use of hospital resources and may optimise patient outcome (Valentin et al., 2006).
Supporting other team members (ICU nurses supporting junior doctors, ICU liaison nurse supporting ward nurses) are essential for better teamwork (Flin et al., 2008), which may contribute to better patient outcomes (Ball, Kirkby, & Williams, 2003; Chaboyer et al., 2005; Priestley et al., 2004).

Research limitations
Single setting. Researcher as instrument. Participants change of behaviour due to the observer’s presence.

Conclusion and Recommendations
Improve clinical communication Standardise clinical handover structure and protocol. Leadership involvement in improving interdisciplinary communication. Reinforce tools’ use in clinical communication using organisational
change principles. Redesign tools related to handover.
Encourage collaborative teamwork Adopt collaborative teamwork initiatives across the hospital.

Contributions of The Research Findings Interventions informed by the research findings were
implemented. Examples of the interventions: ICU to ward nursing handover process was redesigned, emphasis
was given to the face to face handover. Tools modified and implemented to facilitate communications. ICU provide predicted discharge date to the wards in order to help
the wards to plan patient care.
Outcome: shortened discharge delays (4.6 hours prior, and 1.0 post intervention), but no change to mortality.
(Chaboyer, et al., 2010, Submitted for publication)

Acknowledgement
The participants The hospital Queensland Health Clinical Practice Improvement Centre (CPIC)
funding The research group for the larger project Supervisors

References Australian Commission on Safety and Quality in Health Care. (2010). The OSSIE guide to
clinical handover improvement. Sydney: ACSQHC. Australian Resource Centre for Healthcare Innovations (ARCHI). (2009). Standard key
principles for clinical handover. Retrieved from http://www.archi.net.au/e-library/safety/clinical/nsw-handover/2
Alvarez, G., & Coiera, E. (2006). Interdisciplinary communication: an uncharted source of medical error? Journal of Critical Care, 21, 236-242.
Ball, C., Kirkby, M., & Williams, S. (2003). Effect of the critical care outreach team on patient survival to discharge from hospital and readmission to critical care: non-randomised population based study. British Medical Journal, 327, 1014-1017.
Chaboyer, W., Gillespie, B., Foster, M., & Kendall, M. (2005). The impact of an ICU liaison nurse: a case study of ward nurses’ perceptions. Journal of Clinical Nursing 14, 766-775.
Donchin, Y., Gopher, D., Olin, M., Badihi, Y., Biesky, M., Sprung, C., et al. (1995). A look into the nature and causes of human errors in the intensive care unit. Critical Care Medicine, 23(2), 294-300.
Engestrom, Y. (1987). Learning by expanding: An activity-theoretical approach to developmental research. Helsinki: Orienta-Konsultit.
Flin, R., O'Connor, P., & Crichton, M. (2008). Safety at the sharpe end: a guide to non-technical skills. Burlington, USA: Ashgate Publishing Company.

Hutchins, E. (1999). Cognition in the wild. Cambridge: MIT Press. Jagsi, R., Kitch, B. T., Weinstein, D. F., Campbell, E. G., Hutter, M., & Weissman, J. S.
(2005). Residents report on adverse events and their causes. Archives of Internal Medicine, 165(22), 2607-2613.
Jain, M., Miller, L., Belt, D., King, D., & Berwick, D. M. (2006). Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Quality & Safety Health Care, 15, 235-239.
Lin, F., Chaboyer, W., & Wallis, M. (2009). A Literature Review of organisational, individual and teamwork factors contributing to the ICU discharge process. Australian Critical Care, 22, 29-43.
Maloney, C. G., Wolfe, D., Gesteland, P. H., Hales, J. W., & Nkoy, F. L. (2007). A tool for improving patient discharge process and hospital communicatio practices: the aatient tracker Paper presented at the AMIA 2007 Symposium Prodeedings, Chicago.
Nadzam, D. M. (2009). Nurses’ role in communication and patient safety. Journal of Nursing Care Quality, 24 (3), 184-188.
Nemeth, C. P., O’Connor, M., Klock, P. A., & Cook, R. I. (2006). Discovering healthcare cognition: The use of cognitive artifacts to reveal cognitive work. Organization Studie, 27, 1011-1035.

Nicholls, A. G., & Young, F. R. (2007). Innovative hospital bed management using spatial technology. Spatial Science Queensland, 2, 26-30.
Priestley, G., Watson, W., Rashidian, A., Mozley, C., Russell, D., Wilson, J., et al. (2004). Introducing Critical Care Outreach: a ward-randomised trial of phased introduction in a general hospital. Intensive Care Medicine, 30, 1398-1404.
Peterson, G. L. (1994). Communicating in organizations: a casebook. Scottsdale, Arizona: Gorsuch Scarisbrick Publishers.
Pronovost, P., Wu, A. W., Dorman, T., & Morlock, L. (2002). Building safety into ICU care. Journal of Critical Care, 17(2), 78-85.
Pronovost, P., Berenholtz, S. M., Ngo, K., McDowell, M., Holzmueller, C., Haraden, C., et al. (2003). Developing and pilot testing quality indicators in the intensive care unit. Journal of Critical Care, 18(3), 145-155.
Sabir, N., Yentis, S. M., & Holdcroft, A. (2006). A national survey of obstetric anaesthetic handovers. Anaesthesia, 61(4), 376-380.
Salas, E., & Cannon-Bowers, J. A. (2000). The science of training: a decade of progress. Annual Review of Psychology, 52, 471-499.
Sims, D. E., Salas, E., & Burke, S. C. (2004). Is there a "big five" in teamwork? Paper presented at the 19th annual meeting of the Society for Industrial and Organisational Psychology, Chicago.

The Joint Commission. ( 2007). Improving handoff communication. Joint Commission Resources,
Williams, R. F. (2006). Using cognitive ethnography to study instruction. Paper presented at the 7th international conference on Learning Sciences, Bloomington, Indiana.
Valentin, A., Capuzzo, M., Guidet, B., Moreno, R. P., Dolanski, L., Bauer, P., et al. (2006). Patient safety in intensive care: results from the multinational Sentinel Events Evaluation (SEE) study. Intensive Care Medicine, 32, 1591-1598.