The Impact of Health Insurance and Other Social Benefits ... · and private health insurance...
Transcript of The Impact of Health Insurance and Other Social Benefits ... · and private health insurance...

1
The Impact of Health Insurance and Other Social Benefits on Poverty in New York State
Sanders Korenman, Dahlia K. Remler and Rosemary T. Hyson Marxe School of Public and International Affairs
Baruch College, CUNY and CUNY Institute for Demographic Research
Final Report to the Howard J. Samuels State and City Policy Center
July 18, 2018

2
Contents
I. Executive Summary
II. Why New York State Needs a Poverty Measure that Accounts for Health Insurance
III. Measures
A. Poverty measures
1. OPM, SPM, HIPM
2. NYC housing costs, advantages and the NYCgov poverty measure
B. Integrating free care into poverty measurement
IV. Data
V. Methods
A. Impact of current policy on poverty rates using baseline HIPM
B. Impacts of current policy on poverty gaps using baseline HIPM
C. Impacts of current policy on HIPM poverty rates and gaps that incorporate free care
D. Impacts of expanded insurance on HIPM poverty rates and gaps
E. Impacts of Rollbacks of Medicaid Expansion on HIPM poverty rates and gaps
VI. Results: Baseline and Free Care
A. Poverty rates and gaps, not incorporating free care to the uninsured
B. Poverty rates including free care to the uninsured
C. Poverty gaps including free care to the uninsured
VII. Results: Policies to Expand and Contract Health Insurance Benefits
A. Impact of expanded health insurance policies on HIPM poverty rates and gaps
B. Impact of Rollbacks of Medicaid Expansion on HIPM Poverty rates
VIII. Discussion
A. Limitations
B. Implications for Policy in New York State
IX. Appendixes
Appendix 1: Additional figures and tables
Appendix 2: Poverty Measure Concepts Table: Official, Supplemental and Health Inclusive
Appendix 3: Methods for Implicit Insurance Value of Free Care

3
Acknowledgements
We thank the Samuels Center for supporting this research. We thank Patrick Orecki of the Citizens Budget Commission for guidance on budgetary information on uncompensated and indigent care in New York, Deborah D’Orazi for research assistance on indigent care in New York State, and the CUNY Institute for Demographic Research for administrative and technical support. We thank Victoria Grimshaw and Mark Levitan for their comments on a draft version of this report. We are responsible for all errors and interpretations.

4
I. Executive Summary
This report presents analyses of the impact of public and private health insurance benefits and many social policies on poverty in New York State. It uses a recently developed health-inclusive poverty measure that incorporates a need for health insurance and a value of health insurance benefits, including Medicaid. It also accounts for the substantial free care provided to the uninsured in New York. The study also estimates the impacts on poverty of proposed expansions and contractions of health insurance benefits, including the New York Health Act and Medicaid Expansion Rollbacks.
These are the first analyses to show the impacts of health insurance benefits on poverty in New York State. Such estimates have not been available previously because poverty measures from the US Census Bureau and the New York City Mayor’s Office for Economic Opportunity do not incorporate a need for health insurance in the poverty threshold and do not count health benefits as resources that help the poor to meet basic needs. In articles in the Journal of Health Economics and Health Affairs, we developed a poverty measure that includes health needs and benefits, the Health Inclusive Poverty Measure or “HIPM”, and provided estimates for the United States.1
This report explains the need for a HIPM in New York State. It describes the HIPM and special considerations for New York State such as high housing costs in New York City and free care for the uninsured throughout the state. It describes methods for estimating the impacts on poverty of current social and health benefits: public and private health insurance, subsidies for insurance premiums under the Affordable Care Act, major social insurance programs such as Social Security and Unemployment Insurance, means-tested benefits such as food and housing assistance programs, and tax credits such as the federal Earned Income Tax Credit. Incorporating the impact of free care on poverty is new and involves several approximations. We therefore present estimates of the impact of social and health benefits both with and without incorporating free care.
Because our focus is the impact of health insurance policy changes, our analysis sample excludes households with disability benefit recipients and households composed entirely of persons over age 65.
Those populations are not the subject of proposed policy changes analyzed in this report. Note that for all our analyses, we use the same sample definitions and exclusions in order to compare different poverty measures or to compare poverty across geographic areas (e.g., NY State vs USA).
The report describes methods for simulating the impact on health-inclusive poverty of the following expansions and contractions of public health insurance benefits:
• “ACA+”: Expanding Medicaid to provide universal health insurance with no out-of-pocket expenses, for everyone < 133% of the federal poverty line. And expanding Affordable Care Act means-tested subsidies to cover all lower and middle-income uninsured persons (between 100% and 400% of the federal poverty level, or up to $100,000 for a family of four).
• “NYHA”: Adopting the New York Health Act (NYHA) that would provide universal insurance to all with no out-of-pocket expenses.
• “Rollback”: Rolling back Medicaid Expansion so as to cover only families with incomes below the Federal Poverty Level. In this analysis, we consider two scenarios regarding the free care available to those who lose Medicaid benefits and other uninsured persons. “Rollback1” maintains at current levels the per capita spending on free care for the uninsured, despite a large increase in their number. This scenario would require increased total funding for such care. “Rollback2” maintains total spending on the uninsured, thereby reducing per capita spending on care for the uninsured and increasing HIPM poverty further.
Major Findings 1. In 2015, the HIPM poverty rate for NY State stood at 18.5%, nearly two percentage points higher than the Census Bureau’s Supplementary Poverty Measure (SPM). The HIPM and SPM are directly comparable since essentially they differ only because the HIPM includes health insurance needs and benefits. The HIPM rate should generally exceed the SPM rate because the HIPM’s health insurance need is only partly met by existing health insurance benefits. The HIPM poverty rate is high relative to the SPM rate for groups lacking

5
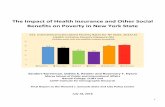
health insurance benefits. For the uninsured persons, the NY State HIPM poverty rate exceeded the SPM rate by more than 15% points. 2. The HIPM poverty rate for NY State is 2.5% points above the national average. This difference reflects the high HIPM rate in the New York City Metro area, which is more than 4% points above the national average. 3. Demographic differences in HIPM poverty are similar to demographic differences in other poverty rates such as the SPM. Rates are high for single-parent families, one-adult household, Hispanics, non-Hispanic Blacks, and immigrants, especially non-citizens. 4. Health insurance benefits have major impacts on poverty. Medicaid (including CHIP) reduced the HIPM poverty rate in NY State by 6% points, and in the NYC Metro area, by 9% points. Employer-sponsored insurance is also important, reducing poverty in NY State by over 4% points. The impacts on poverty of all social insurance programs combined, all means-tested benefits combined and tax credits were 4, 5 and 2.7% points, respectively. For children, Medicaid reduced poverty by 7.5% points. While households with children benefit greatly from social programs, single adults with no children present get little poverty reduction from social or health benefits. Figure ES1 summarizes the key finding from our policy estimates and policy simulations. The figure shows HIPM poverty rates for New York State where data for 2014 and 2015 have been combined.
5. We estimate that assigning an insurance value to the Free Care provided to the uninsured in NY State reduces the overall poverty rate for the state from 18.8% to
18.0%. The effect is modest because only about 8.6% of the population is uninsured. However, Free Care reduces the poverty of the uninsured by nearly 6% points. 6. Under the “ACA+” simulation, when ACA coverage and benefits are expanded, the HIPM poverty rate falls to 14.7%. With the NYHA (universal coverage with no out-of-pocket costs), the HIPM poverty rate falls to 13.7%, or by about one quarter compared to the status quo HIPM rate with Free Care. 7. In the Medicaid Rollback scenarios, the uninsured population of New York State would more than double and the number of uninsured children would nearly quadruple. As a result, poverty would increase by two to three percentage points, to 21 percent (Rollback1). That scenario assumes that the care available through free care would be maintained, requiring that funding be doubled. If no additional funds for free care became available, the number of poor persons in New York State would rise by about 600,000, including an additional 200,000 poor children (Rollback2).
Figures ES2 and ES3 summarize the estimated and simulated impacts for NYC Metro area within NY State, and the area of the state outside the NYC Metro.

6
8. The impact of expansions of health insurance benefits would be felt across the state. The absolute size of the decline in the poverty rate under benefit expansions would be greater in the NYC Metro area than outside, but the proportionate decline would be larger outside the Metro area. The NYHA would reduce the HIPM rate 4.4% points relative to the baseline with Free Care in the NYC Metro area and 4.0% points outside. As a proportion of the baseline rate with Free Care, those changes amount to a 22.3% reduction in poverty in the NYC Metro area, but a 29.2% decline outside.
9. Medicaid Rollbacks would have much larger impacts in the NYC Metro area than outside. For example, Rollback2 would increase poverty by 4.0% points in the NYC Metro area, or by 20%. In NY State outside the Metro area, the increase would be 1.4% points, or roughly 10%.
10. Poverty changes would be greatest among those most directly affected by the policy changes. Among those initially covered by Medicaid, poverty would increase by between 5 and 13% points under the Rollback scenarios. The poverty rate of the uninsured would also increase as many have family members who would lose Medicaid benefits. In the Rollback2 scenario, poverty of the uninsured rises further because as the number of uninsured persons increases, per capita spending on Free Care for the uninsured falls, lowering the “insurance value” of Free Care.

7
II. Why New York Needs a Poverty Measure that Accounts for Health Insurance
Between 2013 and 2016, the percentage of New York State residents without health insurance was cut nearly in half, from 10.7% to 6.1%.2 The gain in health insurance coverage was twice as large in absolute terms among low-income adults (aged 19 to 64): their uninsurance rate fell from 26 to 15 percent.3 Did poverty decline in New York as a result? Would it decline further with universal health insurance? Would poverty increase if the Affordable Care Act (ACA) were repealed or its Medicaid expansions reversed?
The answer depends on what we mean by poverty—how it’s conceptualized—and how it’s measured. Poverty is defined as a household not having the resources to meet a standard of basic need. Is health care a basic need? Is health insurance?
The United Nations’ Universal Declaration of Human Rights listed medical care among the basic human rights.4 Similarly, Article XVII (Social Welfare) of the NY Constitution requires the State provide both “aid, care and support of the needy” (sec. 1) and “protection and promotion of the health of the inhabitants of the state” (sec. 3). Both international and New York State documents suggest that NY State considers health care a basic need and that those without the resources to meet that need are poor.
Yet, if neither health care nor health insurance is treated as a basic need and if health insurance is not counted as a resource, as in the case of the official US Census poverty measure, then health insurance benefits cannot reduce poverty by meeting a basic need. To address this measurement problem, in a series of papers we developed a health-inclusive poverty measure, meaning that health insurance is explicitly treated as a basic need and health insurance benefits are counted as resources to meet that need.5
New York State has a tradition of generous health programs and relatively strict insurance regulation.6 In 2000, New York State effectively expanded Medicaid through its Family Plus Program, which covered childless adults up to 100% of the Federal Poverty Level (FPL, which is similar to the Official Poverty Measure poverty line)7 and families with children up to 150% of FPL.8 Finally, New York has a widespread system of
clinics that provide free care to the uninsured.9 Failing to incorporate health insurance needs and resources misses important impacts of NY State health insurance policy and regulations on poverty.
This report presents estimates of the impact of public and private health insurance benefits (and other social benefits) on health-inclusive poverty in New York State. Some estimates incorporate an implicit insurance value of free care provided to the uninsured. The report also considers the likely impact on poverty of policies that make insurance universally available and affordable, and those that reduce health insurance benefits, such as efforts to roll-back ACA Medicaid expansions.
III. Measures
A. Poverty measures
Historically, US poverty measures could not be used to estimate the impact of health insurance on poverty. As a 1995 report of the National Academy of Sciences explained, since standard poverty measures do not include a need for health care or health insurance in the basic need standard or “poverty threshold”, it is inconsistent to count health insurance benefits as resources available to meet basic needs.10 At the time, they could find no valid and practical way to include either health care or health insurance in the needs threshold.11
Two health insurance regulations make it possible to include health insurance in the poverty threshold.12 Guaranteed issue, meaning insurers cannot refuse to sell anyone insurance, and community rating, meaning that insurance premiums cannot depend on health status, make it possible to determine a dollar value for health insurance in the poverty threshold. Both regulations came to New York State in 199313, and to the US as a whole in 2014 as a result of the Patient Protection and Affordable Care Act (ACA).
Once the poverty threshold includes a need for health insurance, it is possible to consistently count health insurance benefits in resources. We developed and applied this approach in our health inclusive poverty measure (HIPM).14 The HIPM’s validity rests on the premise that health insurance is considered a basic need. The US experience with the Affordable Care Act

8
suggests that agreement with that premise, while widespread, is not universal. That said, if health insurance is considered a basic need, then, demonstrably, health insurance matters a great deal for poverty. For example, for the United States overall, in 2014 Medicaid reduced child poverty more than all other means-tested benefits combined.15
1. OPM, SPM, HIPM
In addition to the Health Inclusive Poverty Measure, we use two other measures published annually by the US Census Bureau in cooperation with the Bureau of Labor Statistics: the Official Poverty Measure (OPM) and the Supplemental Poverty Measure (SPM).16 The Health Inclusive Poverty Measure17 is a modification of the SPM. Table 1 summarizes the main differences among the three measures, with key differences between the HIPM and the SPM shown in bold.
OPM. The US Census Bureau has published the poverty rate for the United States annually since mid-1960s. Its measure of resources is a family’s cash income before taxes. Its needs threshold, commonly called the “poverty line,” is three times the cost of an emergency food budget for the family, which differs according to family size and age-composition. These thresholds have been updated annually for overall price inflation using the Consumer Price Index. A family is deemed poor according to the OPM if its resources are less than needs.
The OPM is thought to be obsolete for a variety of reasons. Most importantly for our purposes, it does not count as resources the non-cash benefits many low-income families receive such as food assistance (SNAP, WIC), housing assistance (public housing, “section 8” housing choice vouchers) or public or private health insurance benefits (Medicaid, Medicare, etc.).
Furthermore, the OPM thresholds are not adjusted for the substantial regional differences in housing costs; they are the same throughout the nation. Finally, the family unit used for the OPM are people living together who are related by blood, marriage or adoption. Unmarried cohabiters are treated as separate families, for example. Concerns about the ability of the OPM to identify the poor and assess the impact of social policies on poverty have grown as the size of non-cash transfers
have grown and as living arrangements and family structures have become more complex.
SPM. The Supplemental Poverty Measure (SPM) was designed to address the shortcomings of the OPM. It is based on the recommendations of a 1995 report of the National Academy of Sciences,18 and an Inter-Agency Working Group.19 The Census Bureau began publishing SPM poverty estimates in 2011.20
The principle differences between the OPM and SPM are shown in columns 1 and 2 of Table 1. The SPM uses a broader definition of family than the OPM. The definition of basic needs, or the SPM threshold, is based on expenditures on four necessities: food, clothing, shelter and utilities, plus “a bit” for other needs. It adjusts the shelter portion of the threshold for regional differences in housing costs. Given the high cost of housing, the housing adjustment results in a noticeably higher poverty rate in the New York City metropolitan area. As for resources, unlike the OPM, the SPM counts non-cash benefits such as food and housing assistance as resources available to help families meet their basic needs. However, the SPM, like the OPM, does not count health insurance benefits as resources. The SPM adjusts resources to remove (subtract) expenses in three categories: taxes, necessary work and child care expenses and all medical out-of-pocket spending (MOOP) on health insurance premiums, health care and over-the-counter drugs. The logic of this deduction is that these expenses reduce the income available for spending on the basic needs of food, clothing, shelter and utilities, and are non-discretionary. However, if discretion is involved or such expenditures are responsive to resources (such as wealth or savings), then the SPM will make those with somewhat higher resources who choose to spend more on health insurance “look poorer.”

9
Table 1: Overview of Poverty Measures: Official, Supplemental and Health Inclusive
Official Poverty Measure (OPM)
Supplemental Poverty Measure (SPM)
Health Inclusive Poverty Measure (HIPM)
Needs Threshold
3X Basic Food Needs in in 1960s, updated for inflation with CPI
33rd percentile of spending on Food, Shelter, Clothing, and Utilities, plus a bit
33rd percentile of spending on Food, Shelter, Clothing, and Utilities, plus a bit + cost of basic health insurance
Resources
Pre-tax cash income
After-tax cash income + tax-credits + in-kind benefits (non-health insurance)
After-tax cash income + tax-credits + in-kind benefits (non-health insurance) + health insurance benefits Subtractions from
Resources
- Work & childcare expenses - out-of-pocket expenditures on care
(non-premium MOOP) - out-of-pocket expenditures on
insurance (premium MOOP)
- Work & childcare expenses - capped out-of-pocket expenditures on
care (non-premium MOOP)
This table is based on one constructed by Dr. Sayeh Nikpay for a discussion of our paper at the 2018 ASHEcon conference; it includes information from similar tables in Korenman and Remler (2016, Table 1), and Short (2013, page 3). Appendix Table 2 provides a more detailed description of these measures.

10
Most importantly, health insurance benefits can only affect poverty, as measured by the SPM, if they affect out-of-pocket expenditures on care or insurance (MOOP). The HIPM cannot detect if people go without health insurance or needed care in order to pay for other basic needs. But if health care or insurance were explicitly included among the basic needs, along with food, clothing, shelter and utilities, then health insurance benefits would directly meet basic needs. That is, health insurance benefits would directly reduce poverty by meeting a basic need, even if they do not reduce MOOP spending. We call a poverty measure that includes an explicit health need in the poverty threshold and that counts health insurance benefits in resources a Health Inclusive Poverty Measure (HIPM).
HIPM. Our particular HIPM is a modification of the SPM. It extends the SPM by adding a “basic need” for health insurance in the SPM need threshold, in addition to the need for food, clothing, shelter and utilities. And, the HIPM resource measure includes a value for the health insurance benefits a family receives, from an employer or government (e.g., Medicaid, Medicare, ACA premium subsidies). Because the HIPM includes an explicit need for health insurance in the threshold and an explicit value for health insurance benefits in resources, it does not subtract MOOP expenditures on insurance premiums from resources.
The health insurance need for the HIPM threshold is the second cheapest “Silver” plan sold on the ACA marketplace in the area where the family resides. We selected this plan because it is the benchmark plan for ACA premium subsidies, and the ACA intended to make it affordable. ACA guaranteed issue regulations mean that any citizen or legal resident must be able to purchase that plan. Further, the plan price must not vary according to health status (community rating means insurance companies cannot charge higher premiums for those with pre-existing conditions). With these regulations, a basic insurance need for insurance can be determined for each family from information on the family’s residential location (ACA rating area) and the ages of family members.
New York uses a family tier system, so that premiums are based only on the number of adults and children in the household.21
While health care needs are primarily met through health insurance, fully meeting health care needs also requires paying out-of-pocket for cost-sharing, such as deductibles and co-payments. Therefore, we follow the SPM by deducting the portion of MOOP expenditures that is for care only. We also limit the deduction to the cap on such payments available based on the person’s insurance status.22
2. NYC housing costs, advantages and the NYCgov poverty measure
Housing costs are higher in the New York City metro area compared to the national and state average. The SPM thresholds are adjusted to reflect these higher costs. However, the SPM housing adjustment for NYC may be insufficient to reflect the high market-rate rentals in NYC.23 At the same time, the SPM also does not adjust for some of the rental “advantages” prevalent in NYC such as rent controlled and rent regulated apartments.
Since 2008, the NYC Mayor’s Office of Economic Opportunity has produced a poverty measure for New York City, now called the New York City Government Poverty Measure (NYCgov).24 Like the SPM, the NYCgov measure is based on the recommendations of the 1995 NAS Report, and in fact the NYCgov preceded the SPM.
The housing cost adjustment used for the NYCgov is greater than the SPM adjustment, so the NYCgov thresholds are commensurately higher, by approximately 6.5 percent.25 Alone, the higher thresholds increase the NYCgov poverty rate relative to the SPM rate for NYC. However, the NYCgov includes housing benefits or “advantages” the SPM does not. While both measures include public housing and housing vouchers, the NYCgov measure also includes imputed values for advantages such as rent-controlled and rent-regulated units.26 Alone, counting additional housing resources lowers the NYCgov poverty rate relative to the SPM rate.
Below, we present rates for the entire NYC Metro area within New York State.27 We estimate that our SPM and HIPM poverty rates for the NYC metro area are overstated by about two percentage points by not counting all NYC housing “advantages” imputed for the NYCgov measure. For the same reason, since the NYC metro population is roughly half the state population,

11
we overstate poverty in NY State by about one percentage point.28
Finally, if we assume the NYCgov thresholds are correct for NYC, then our thresholds for HIPM and SPM poverty in NYC are about 6.5% too low. This lowers our HIPM and SPM estimates for NYC. Thus, in all, our HIPM and SPM poverty rates for the NYC metro area and NY State still likely overstate poverty, but by slightly less than 2 and 1 percentage points, respectively.
Data limitations prevent us from implementing the NYCgov measure as a HIPM for estimates for NYC. 29
B. Integrating Free Care into Poverty Measurement
The HIPM is premised on the notion that people need basic health insurance to meet their basic health care needs. Certainly, people, especially low-income people, could not possibly afford to pay out-of-pocket for any serious medical condition, given the high level and, at times, ruinous medical care costs.30 31 However, uninsured people who cannot afford to pay for health care out of pocket receive substantial amounts of health care. In New York, such care is funded and provided through a wide variety of mechanisms.32
Consider first hospitals and the acute care they provide. Hospitals cannot turn away unstable patients, irrespective of ability to pay. For those who arrive uninsured, hospitals first determine if the patients are eligible for Medicaid, then if eligible for other NY State programs, then if their income qualifies them for free care, and finally, if eligible for discounted care.33 The free and discounted care is funded by the Disproportionate Share Hospital (DSH) Program, as well as other programs that also provide funds to financially distressed hospitals for care to the insured as well as the uninsured.34 Patients may also be billed, with unpaid portions eventually becoming bad debt that providers write off, in full or in substantial part.35
Hospitals, especially “safety net” hospitals also provide non-acute specialist care, outpatient, as well as inpatient, often through a system of clinics. Much free primary and specialist care for chronic conditions is provided at Federally Qualified Health Centers (FQHCs). FQHCs also care for people covered by Medicaid, Medicare, employer-provided insurance or individually purchased insurance. Overall, in New York State FQHCs,
16% of FQHC patients are uninsured, 59% have Medicaid or CHIP, 6% Medicare and 19% have some kind of private insurance (employer or individual).36
Free care available to the uninsured provides partial implicit insurance, inferior to formal insurance. Free care provides part of the three essential protections of health insurance: access to care, financial protection and risk reduction 37 In order to estimate how much free care policies reduce health-inclusive poverty we would like to estimate the implicit insurance value of this free care. Conceptually, we define the implicit insurance value of free care as the actuarial value of the care provided to the uninsured population (e.g., of NY State), plus standard administrative costs. There are no readily available estimates of this value. We therefore use two different estimation approaches.
One approach to estimating the implicit insurance value of free care measures all inflows of funds for free care to the uninsured and assumes it is spread evenly across all uninsured individuals. A problem with this approach is that, in reality, such funds may also pay for care to insured individuals who can’t or don’t pay their out-of-pocket costs for care (cost-sharing), or have insurance that pays an amount considered insufficient. For example, the federal Disproportionate Share Hospital (DSH) program is explicitly intended to pay not only for uncompensated care of the uninsured, but also for the portion of the cost of care to Medicaid patients that Medicaid payments do not cover, because prices paid by Medicaid are lower than those paid by other insurers. A second problem with using this in-flow approach for poverty measurement is that it does not capture care for the uninsured that is cross-subsidized by payments for insured individuals.
Another approach to estimating an implicit insurance value of fee care to the uninsured is to measure care that is received but not paid for, often termed uncompensated care.38 For example, Bovbjerg et al. (2006) estimated the amount of such care in New York State prior to the passage of the ACA.39
Whatever approach is taken, it is unclear how one should attach costs to particular treatments and therefore to particular patients. Health care costs are largely fixed —meaning that they must be paid however much or little care is provided—such as the costs

12
associated with the purchase and maintenance of hospital buildings. Health care costs are also often “joint costs” — meaning that they are simultaneously incurred by multiple patients and cannot be clearly allocated to any one patient or treatment. For example, the cost of purchasing and maintaining a CT scan machine is large: how should those costs be allocated to different patients and conditions? These features make the allocation of costs to specific patients fairly arbitrary.
We use the funding inflow approach for our main estimates of the insurance value of free care. This approach allows us to directly link outlays for free care to implicit insurance values and to link those values to poverty. Thus, it allows us to simulate the impacts on poverty that would result from increases in the uninsured population if Medicaid Expansion were to be rolled-back. However, we recognize that the funds inflow approach is an under-estimate of the implicit insurance value of free care since it does not count cross-subsidies. Therefore, as a sensitivity analysis, we also use an uncompensated care approach based on evidence from the Oregon Health Insurance Experiment.
IV. Data
The primary data source for this analysis is the Current Population Survey Annual Social and Economic Supplement file, the same data the Census Bureau uses for construction of official and supplemental poverty measures. We included undocumented immigrants in our samples by imputing undocumented status using a method developed by George Borjas.40
We used health insurance premium and cost-sharing information from three sources: data on ACA marketplace plans from The Robert Wood Johnson Foundation41; data on Medicare Advantage Prescription Drug Plans (basic plan for Medicare recipients) from the Center for Medicare and Medicaid Services downloaded from the NBER website42; and information on Medicaid and CHIP program rules primarily from Kaiser Family Foundation reports.43 44 45 46 47 48
V. Methods
A. Impact of current policy on poverty rates using the baseline HIPM measure
We use a standard poverty budget accounting approach to estimate the impact of a benefit (or benefit group) on HIPM poverty rates. These estimates are sometimes called “marginal impacts.” They estimate how much the HIPM poverty rate would change if one benefit or group of benefits were eliminated. To estimate such impacts, we set to zero the value of that benefit in family resources and recalculate the HIPM poverty rate. The difference between the recalculated rate (without the benefit) and the actual HIPM poverty rate is the impact of that benefit.
These impacts should be interpreted as the change in poverty that would result from the elimination of a benefit, all else the same. They are not causal estimates of the effect of elimination of a benefit because they do not account for behavioral or health responses to program elimination. For example, people might work longer hours or retire later if a benefit were eliminated.49
B. Impacts of current policy on poverty gaps using the baseline HIPM measure
The poverty gap is a measure of the depth of poverty. It measures how far the resources of the poor fall short of the poverty threshold. Analyses of program impacts on poverty gaps are an important complement to analyses of their impacts on poverty rates since many social programs raise the incomes of the poor but do not remove them from poverty. Thus, poverty gaps can show how government transfers assist poor families even when they remain poor.
For our analyses of the HIPM poverty gap, we begin with families whose market incomes after taxes and work and child expenses fall below the HIPM poverty threshold.50 First, we calculate how far the market income (after-taxes and work expenses) of these families falls below the poverty line, on average. For example, if market income alone meets 60% of the basic needs of these families, the pre-transfer HIPM poverty gap is 40%. Next, we sequentially add employer-provided health insurance benefits and the different public benefits that families receive to their resources, recalculating the poverty gap after each addition. This exercise shows how much each benefit

13
reduces the poverty gap, thereby reducing the depth of poverty. The poverty gap that remains after all resources have been added is the HIPM poverty gap or the post-transfer HIPM poverty gap.
C. Impacts of current policy on HIPM poverty rates and gaps that incorporate free care
Methods for free care.
Our main estimate of the implicit insurance value of free care is based on inflows of funds to providers to care for the uninsured. We first compiled information on funds to hospitals and FQHCs intended for “indigent care” and assumed that they were spent on the uninsured. Our total flows estimate is the sum of: Disproportionate Share Hospital program allocated to care for the uninsured; Federally Qualified Health Centers (FQHCs) Federal funding from Health Resources and Services Administration (HRSA); and Philanthropic funding for FQHCs. We explain our logic and methods further below.
We assume that the revenues provided by insurers, on average, cover the cost of care for insured patients, and no more. Consequently, we assume that all direct government funding (HRSA Federal funding) and all charitable care funds care for the uninsured.
We obtained Federal HRSA funding for NY State HRSAs from the Health Resources Service Administration web site.51 We lacked 2014 and 2015 information on charitable contributions. Therefore, we estimated charitable care contributions for 2014 and 2015 using current (2017) information on the ratio of revenue from philanthropic sources to revenue from Federal HRSA funding and 2014-2015 information on Federal HRSA funding.52
Financial responsibility for Disproportionate Share Hospitals (DSH) is split evenly between Federal and New York State governments.53 We obtained Federal DSH contributions for 2014 and 2015 from the Kaiser Family Foundation.54 However, DSH funds do not just pay for the uninsured but also for the uncompensated part of Medicaid. Retrospective audits ensure that Federal payments to hospitals, typically through the states, to cover uncompensated care, are ultimately based on the care provided and its estimated cost. Specifically, those costs are for uncompensated care for the uninsured and
for “under-payment” by Medicaid.55 We can use those audited results to estimate the share of DSH funds going to the uninsured, relative to Medicaid.
However, the audits and funding adjustments take many years. In effect, total inflows for the uninsured in a particular year often cover care provided in earlier years. Therefore, As of June 2018, the last finalized DSH audits available from Medicaid.gov were completed only up to 2013.56
In 2013, the ratio of uncompensated uninsured costs to total DSH spending was 67%.
We simulate poverty rates for 2014 and 2015 (pooled). Therefore, we estimate an implicit insurance value of the total in-flows of funds to providers to care for the uninsured for 2014 and 2015. To do so, we divide the sum of the 2014 and 2014 in-flows by the number of people uninsured in 2014 plus the number uninsured in 2015 (according to the American Community Survey). We adjust the dollar flows to the uninsured to account for the age distribution of the uninsured population. We estimate an implicit insurance value per uninsured person in New York State of $1,807. Further details of our calculation of the insurance value of free care are provided in Appendix 2.
However, we do not assume a uniform implicit insurance value of free care for New York State. Rather, we assumed that free care provides an equal replacement share of the silver plan available for purchase on the ACA marketplace, the premium of which varies across the state. Specifically, since $1,807 represents 41% of the average adult second low-cost sliver basic plan premium state-wide, we assumed that the implicit insurance value of free care is 41% of the value of such a silver plan in the area of residence.
We also estimated an implicit insurance value of free care based on uncompensated care delivered to the uninsured from the Oregon Medicaid Expansion Experiment.57 A study of that experiment revealed that poor adults who applied for Medicaid and would have been eligible but remained uninsured as a result of the experiment (i.e., because randomly assigned to the control group) received 60% of the care of those who in fact were insured by Medicaid as a result of the experiment.58

14
Generalizing from Oregon in 2008 among poor adults potentially eligible for Medicaid to all uninsured in NY State in 2014-15 presents several problems. First, 2008 is prior to the ACA, though Oregon had partly expanded Medicaid at that time. Second, we estimate that 20% of the uninsured in NY state in our 2014-15 sample are undocumented (compared to 16.8% nationally). Both their health conditions and the amount of care they receive conditional on health status could differ from citizens and documented immigrants in the Oregon study. Finally, New York State has a particularly well-developed system of indigent care.
Thus, for our main estimates of the impact of free care on the poverty of the uninsured, we used the 41% estimate based on dollar inflows for free care in NY State in 2014 and 2015. We also used the 60% estimate from the Oregon health insurance experiment as a sensitivity analysis. Specifically, free care has an implicit insurance benefit that partially meets the basic health insurance need: namely, a resource value equal to between 41% and 60% of the health insurance need.
We then used the methods described in the previous section to estimate the contribution of free care to reduction in HIPM poverty rates and gaps, treating free care as another health insurance benefit available to the uninsured. We show how the HIPM poverty rate or gap changes when the value of free care is added to family resources.
D. Impacts of expanded insurance on HIPM poverty rates and gaps
Proposals such as the New York Health Act59 would replace all health insurance in New York State, public and private, with a single-payer system where the insured have no out-of-pocket payments for insurance premiums or cost-sharing.60 Such a system would entail substantial new funding and have major implications for employers, insurance markets, health care providers and taxpayers. The challenges of simulating such far-reaching changes and tracing through their effects on poverty are a major undertaking beyond the scope of this report.61 However, we estimate the direct effects on HIPM poverty of providing universal insurance to everyone with no premiums and no cost-sharing—no out-of-pocket expenses whatsoever. We refer to this policy scenario as NYHA.
We also estimate the impact on poverty of a more incremental change, expanding eligibility for affordable health insurance to all New York State residents, irrespective of immigration status. Broadly speaking, all lower income families (below 133% of the Federal Poverty Level, FPL, which is similar to 133% of the Official Poverty Measure poverty threshold) would receive health insurance with no out-of-pocket premiums or cost-sharing of any kind. Those with higher incomes would be eligible for the ACA subsidies including those who currently face non-income restrictions based on immigration status, having access to employer-insurance and the “family glitch.”62
Thus, in describing this policy simulation, we consider two distinct populations: 1. those with family incomes below 133% of the FPL, who are not currently eligible for ACA premium subsidies in Medicaid non-expansion states, including New York, and 2. those with family incomes above 133% FPL.
< 133% FPL
Those under 133% of FPL would be eligible for insurance that covers all care deemed essential under current law, and pay no out-of-pocket premiums and no cost-sharing. In terms of the HIPM, their health insurance needs and care needs would be fully met. So, irrespective of their current health insurance status, their HIPM resources would be credited with health insurance resources equal to their health insurance need—the unsubsidized premium of the basic health insurance plan (either the 2nd low-cost Silver plan or, for Medicare recipients, the cheapest MA-PD plan). To simulate the impact of the elimination of cost sharing (deductibles and co-pays), we set their non-premium MOOP to zero. Since we do not change tax payments, we assume that any new resources required to fund this expansion of health insurance benefits would be financed by taxes on families with incomes far above the HIPM poverty threshold.
We also assume that the universal insurance program provides free secondary insurance for current Medicare beneficiaries (primarily persons aged 65 and older who reside with those under age 65 since senior-only households are excluded from the sample), so they have no premium payments or cost-sharing expenses.
> 133% FPL

15
Premium subsidies. The uninsured who were formerly categorically ineligible for ACA premium subsidies due to immigration status or family insurance status would become eligible, and credited with means-tested premium subsidies. Thus, we assume that the plan would remove all barriers to ACA eligibility for premium and cost-sharing subsidies and all newly eligible persons would take-up the benefit.
Regarding the uninsured who were formerly categorically eligible for premium subsidies but chose not to purchase insurance, we envision an additional policy change that induces them to take-up benefits, such as enforcing a health insurance mandate with penalties much higher than those included in the ACA. We therefore credit their HIPM resources with the premium subsidies for which they are eligible.
Cost sharing subsidies. All persons (regardless of insurance type or immigration status) are made eligible for means-tested cost-sharing reduction subsidies currently available to those who purchase Silver plans on the ACA marketplaces. Namely, for those with incomes between 100% and 250% of FPL, cost-sharing is reduced based on a sliding scale, so that the actuarial value is increased, a flexible way to lower cost-sharing expenditures.63
Out-of-pocket maxima for current Medicaid/CHIP and Medicare beneficiaries do not change. Those covered by an insurance policy of someone who does not reside in their household continue to have out-of-pocket limits without no subsidies, the income of the non-resident policyholder is not reported in the CPS.
E. Impacts of Rollbacks of Medicaid Expansion on HIPM poverty rates and gaps
We focus on the impacts of rolling-back Medicaid eligibility, although some proposals to replace the Affordable Care Act would also eliminate subsidies for individual insurance purchased on the ACA marketplaces. However, the overall impact of premiums subsidies on poverty is small, although non-negligible for some populations (see Results).
On the other hand, the impact of Medicaid cut-backs on poverty could be large given their size, the targeting of the low-income population for eligibility, and their
currently large impact on poverty (see Results). Proposals have been forwarded to eliminate the ACA funding for Medicaid expansions, and change program funding overall from a matching entitlement to a block-grant, for example, fixing per capita expenditures at their 2016 levels.64 Analysts anticipate that block-granting Medicaid would erode the funding available to serve the currently-eligible population.65 Although some proposals would also undermine funding for elderly and disabled Medicaid beneficiaries, we assume their eligibility and benefits would not be affected.
The impact of changes such as these on poverty in New York depends in part on how the state reacts. We assume that the state would preserve Medicaid eligibility for those served by traditional Medicaid, especially the lowest-income families. Specifically, we assume that, in the long run, children and parents up to 100% of FPL would remain eligible for Medicaid. Adults with no-children present would lose eligibility as would parents and children with incomes above 100% FPL. Covering parents to 100% of FPL is similar to pre-expansion Medicaid in NY State. As such, our assumption might be considered too generous. On the other hand, not covering children above the poverty line is harsher than pre-expansion Medicaid and in fact more restrictive than eligibility criterion in current non-expansion states who generally cover children up to 200% FPL with Medicaid/CHIP.66
Finally, we assume that those who lose eligibility for Medicaid become uninsured but have access to the “free care” as described above. The critical question is how much free care can be provided for the substantially larger population that will be uninsured under this simulation scenario?
Once again, we make two assumptions. First, we assume that per capita spending on care for the uninsured remains unchanged at 41%, despite a large increase in the number of uninsured. For the second scenario, we assume that total spending on all the uninsured remains the same, so that the per capita insurance value of free care declines as the uninsured population expands.
As a result of the Medicaid Rollback the uninsured population of New York State would more-than double and the number of uninsured children would nearly

16
triple. As a result, in the second Rollback scenario the implicit insurance value of free care falls to 20%.
Although neither scenario is particularly realistic, they provide reasonable upper- and lower-bounds for expenditures on free care and the implicit insurance value of free care to the uninsured.
Even with full maintenance of free care, people who lose Medicaid benefits would likely pay more out-of-pocket for care.67 Modeling how out-of-pocket expenditures on care change when people lose Medicaid benefits is beyond the scope of this work. Therefore, to ensure our estimates focus only on the direct effect of losing insurance, we maintain the baseline deduction from resources of expenditures on care (capped non-premium MOOP).
VI. Results: Baseline and Free Care
A. not incorporating free care to the uninsured
i. Poverty rates
We begin with estimates of poverty rates that, like estimates produced by the Census Bureau, do not take into account the impact of “free” medical care provided to the uninsured. We refer to these as our baseline estimates.
Figure 1 shows estimates of poverty rates in 2015 according to the Official Poverty Measure (OPM), Supplemental Poverty Measure (SPM) and Health-Inclusive Poverty Measure (HIPM) for the US and New York State. The sample for Figure 1 includes all households other than those composed entirely of persons aged 65 and over.
Official poverty is slightly higher in NY State than the nation as whole. However, the SPM and HIPM rates are over two percentage points higher in NY State. The difference between the SPM and OPM rates mainly reflects the impacts of two SPM adjustments. First, the SPM threshold is raised relative to the OPM threshold in areas such as NYC with high housing costs. The SPM also adds a value for non-health in-kind benefits to resources. The first of these adjustments raises SPM poverty relative to OPM poverty while the second adjustment lowers it.
Figure 1 shows that, for the nation as a whole, these two adjustments essentially offset: the US OPM and SPM poverty rates are 14.4% and 14.6%, respectively. In NY State, however, the increase in SPM poverty from high housing costs exceeds the decrease from counting additional benefits. As a result, SPM poverty in NY State is 16.8% and the OPM rate is 15.0%.
The HIPM adjusts the SPM poverty measure to incorporate both a health insurance need in the threshold and, for families with health insurance benefits, a value of those benefits in resources. To the extent that health insurance needs are not completely met, the HIPM poverty rate will exceed the SPM rate68 Figure 1 shows the impact is similar in the US and NY State: the HIPM poverty rates is 1.5% points higher than the SPM in the US as a whole, and 1.7% points higher in NY State.
Figure 2 shows similar figures for a subsample of persons in households with no disability recipients. For the rest of this report, we exclude households with disability program recipients because disability recipients have not been the focus on health insurance reform, and because their inclusion in the sample distorts the poverty impact analysis for other low-income populations.
Since disability recipients have very high rates of poverty, removing them from the sample lowers all poverty rates somewhat (compare Figures 1 and 2). The difference between the HIPM and SPM poverty rates is somewhat greater (a difference of 2.0% points in NY State and 1.7% points nationally). This reflects the meeting of the basic insurance needs of disability recipients under Medicare and Medicaid.

17
Changes 2014-15. Between 2014 and 2015, OPM poverty worsened slightly, by 0.7% points, but both SPM and HIPM poverty declined substantially (Figure 3). What explains the decrease in SPM and HIPM poverty? Changes in the income distribution is the likely explanation (i.e., income increased near the SPM threshold but not below the OPM threshold). Other possibilities such as increases in the generosity or receipt of in-kind benefits seem less likely.
Increased employment and earnings, combined with work-oriented refundable tax credits (EITC & CTC) likely reduced the SPM and HIPM rates. Improved health insurance coverage is another possibility. However, since the decrease in the HIPM poverty rate was only 0.1 percentage points larger than the decrease in the
SPM rate, improved coverage is at most a partial explanation.
Differences within New York State. Figure 4 shows SPM and HIPM rates for the NYC metro area within NY State, for NY State outside the NYC metro, for NY State as a whole and for the US. In order to increase precision of estimates for various subsamples, we have pooled data for 2014 and 2105.
Our focus here is on differences between SPM and HIPM rates within each area rather than differences in poverty between areas. As we noted in Methods, lack of data on rent-regulated housing units in the NYC metro area may lead the SPM and HIPM rates to overstate poverty in the metro area.
The difference between the HIPM and SPM rates is somewhat smaller outside the NYC metro area than within (1.6% points outside versus 2.1% points within the metro area). This difference is driven partly by the higher proportion uninsured in the NYC metro area. Poverty rates in NY State outside the NYC metro area are somewhat lower than rates for the country as a whole. The high rates in the metro area raise the rates for NY State above those of the nation.

18
Poverty rates by demographic group. Nationally, children, single parent families, racial/ethnic minorities and immigrants are among the groups at higher risk of poverty. That is also true in New York State. In addition, some groups have better access to health insurance resources than others. Thus, we examine poverty according to both the SPM and HIPM. Rates of poverty among children are slightly higher than the rates among all persons, according to both the SPM and HIPM, while poverty rates of adults aged 55-65 are below the population average (Figure 5).
SPM poverty rates among adults living alone and persons in one-parent families are very high (25.9% and 32.3%, respectively). HIPM rates are even higher (27.9% and 37.3%).
Hispanics, non-Hispanic Asians and non-Hispanic Blacks have poverty rates far higher than non-Hispanic Whites. The difference between the HIPM and SPM rate is also larger for the three minority groups than for Whites, the impact of greater receipt of private and/or public insurance benefits for Whites.
Poverty differences by immigration/citizenship status are larger. Non-citizens (including noncitizens that we impute to be undocumented) have SPM poverty rates in excess of 30% and HIPM rates in excess of 35%. The gap between the HIPM and SPM rate (8% points) is
particularly large among those we impute to be undocumented, presumably due to their ineligibility for Medicaid (other than “Emergency Medicaid”).69
Compared to differences between citizens and non-citizens, difference in poverty between naturalized citizens and citizens by birth are modest.
We saw earlier that poverty rates are slightly higher in NY State than in the nation as a whole. The higher rate in NY State could be due either to a different demographic composition of NY State (i.e., a greater representation in the population of groups at high risk of poverty) or because group-specific poverty rates are higher in NY State. Figure 6 compares rates of HIPM poverty between the US and NY State, within demographic groups.
For the most part, the overall NY State – US difference is also found within most demographic groups. Exceptions are persons aged 55-64 and non-Hispanic Blacks, for whom rates are slightly lower in NY State than for the entire US. HIPM rates are particularly high in NY State for Hispanics, Non-Hispanic Asians, person imputed to be undocumented and persons in lone-parent families. We also calculated SPM and HIPM poverty rates for the US and NY State separately by health insurance type and status (Figure 7). Not surprisingly, those covered by Employer-Sponsored Insurance (ESI) or other group

19
insurance have very low poverty rates, both in NY State and nationally. The low SPM rate results from the higher income of families of persons that work for an employer who provides health insurance as a benefit. The HIPM poverty rate for this group falls slightly below the SPM rate; this is possible in well-insured populations because their health insurance meets their health insurance needs and, as explained in Methods, the HIPM caps out-of-pocket expenditures on care at
the limit available to the family, based on their insurance types.
In NY State, rates of SPM poverty among those covered by Medicaid and those who buy individual insurance are 35% and 30%, respectively (Figure 7). While high poverty rates among Medicaid recipients (which, in our analyses, always includes the CHIP program)70 and the uninsured population are roughly similar to those for

20
the US as a whole, the high rate among the individually insured in NY State is distinct. Why? This results from the higher housing costs and higher thresholds that result in NYC, relatively high basic plan premium in New York compared to the rest of the US, and premium subsidies based on the Federal Poverty Level that does not adjust for high housing costs.
Differences between HIPM and SPM poverty rates are due primarily to unmet health insurance needs among lower-income families. Thus, it is not surprising to find large (13 to 15 percentage point) gaps between HIPM and SPM poverty rates among the uninsured, both in NY State and the nation as a whole. Over 45% of the uninsured in NY State live in poverty, according to the HIPM.
The high rate of SPM and HIPM poverty among Medicaid recipients is also not surprising given that eligibility for the program for adults in New York State ends at 133% of FPL. (Pregnant women and infants under 1-year of age are eligible up to 233% of FPL.)
We also estimated HIPM poverty rates by health insurance type and status for the NYC metro area and NY State outside the NYC metro area (Figure 8). For comparison, we include aggregate figures for NY State.
For the individually insured, the HIPM rate for NY State outside the metro area is somewhat higher than the national rate for the individually insured (27% in Fig 8 vs. 24% in Fig 7), but the corresponding rate for the NYC Metro area is far higher (40%, Fig 8). This finding supports the idea that the high HIPM poverty rates among the individually insured in NY State are driven by the high housing costs in the NYC metro area, and the fact that the ACA premium subsidy is not adjust for housing costs.
HIPM poverty rates for the uninsured approach 50% in the NYC metro area and 38% outside the NYC, close to national average for the uninsured, 40%.
ii. Impact of health and social policies on HIPM poverty rates and poverty gaps
We begin with by examining the impact of individual health and social benefit programs on HIPM poverty rates in the US and in New York State. Non-health insurance transfers include Social Insurance (Social Security, worker’s compensation, unemployment insurance, some Veterans payments), Means-Tested Transfers (MTTs) (TANF, SNAP, WIC, school nutrition programs, SSI, housing benefits, energy subsidies), and federal refundable Tax Credits (Earned Income Tax Credit, Child Tax Credit). Figure 9 shows program impacts as the difference in poverty rates that result from the program, and does not show the baseline level of poverty.
The most striking feature of this figure (and all the analyses of this section) is the dominant role of health insurance benefits in poverty reduction. This result shows the value of the HIPM as a poverty measure since neither the SPM nor OPM can capture the direct effects of health insurance benefits on poverty: meeting the basic need for health insurance or care.
Medicaid alone removes nearly six percent of the New York State population from health-inclusive poverty, compared to just over three percent nationally. The impacts of (non-health) means-tested transfers and social insurance are greater in NY than the nation as a whole. The poverty-reducing impact of Medicare and Social Insurance would be far greater if households composed of entirely of elderly persons entirely were included in the sample.

21
Employer insurance benefits are also important, reducing poverty by over 4% points in NY State and nearly 4% points nationally. Federal refundable tax credits have a slightly large impact nationally than in NY State (3.2% versus 2.7%).
How do these benefit impacts differ between the NYC metro area and the remainder of the state? Generally, a higher percent of the NYC metro population is removed from HIPM poverty by health and social benefits (Figure 10). That should not be surprising since the rate of poverty is also much higher in Metro NYC.
Health insurance benefits, especially employer-sponsored insurance and Medicaid, have a greater impact in Metro NYC than outside. Means-tested benefits (MTTs) are also more important in NYC. On the other hand, the impact of social insurance programs and tax credits on poverty are somewhat larger outside the metro area.
Program impacts by demographic group. Many programs are intended to reduce poverty among children or families with children. As a result, health and social programs remove a high percentage of children from poverty.
Figure 11 shows impacts on child poverty and on adults aged 55-64. Families with children are more likely to be eligible for assistance for two reasons: they tend to have lower incomes, qualifying them for means-tested benefits, and some programs are either available only to families with children present or provide more generous benefits to those families (e.g., the EITC). Means-tested benefits have a greater impact on the poverty of children (over 6% points) than 55-64 year- olds (less than 1.5% points) The impact of tax credits exceeds 5% for children versus less than 1% for 55-64 year-olds.
Conversely, the impact of social insurance programs is greater for those aged 55 to 64. Older adults and those they live with are more likely to receive Social Security benefits. Eligibility for retirement benefits through Social Security begins at age 62, albeit at a reduced level. Our analysis sample includes persons aged 65 and over, nearly all of whom receive Social Security, if they co-reside with someone under age 65.
Health insurance benefits reduce poverty markedly for all ethnic/racial groups (Figure 12). For Hispanics, Medicaid is the single most effective anti-poverty program, reducing their HIPM poverty rate by 9.5 percentage points. Also effective at reducing poverty among Hispanics are employer-sponsored insurance, means-tested transfers and tax credits.
For Non-Hispanic Asians, employer-sponsored insurance and Medicaid have the largest impacts (reducing poverty by 6.0 and 5.3 percentage points, respectively), though tax credits are also important (2.5% points).
Employer insurance, Medicaid and means-tested transfers remove roughly equally proportions of Non-

22
Hispanics Blacks from poverty (7.8% points each), followed by tax credits (nearly 5.8% points).
And, although Non-Hispanic Whites have lower poverty rates overall, employer insurance and Medicaid each reduce poverty by about 2.5% points.
We earlier noted the extraordinarily high poverty rates of lone-parent and lone-adult households in NY State (over 25% each). Without these redistributional programs, poverty rates, especially for single-parent families, would be far higher (Figure 13).
Means-tested transfers remove 18% of persons in lone-parent households from poverty, Medicaid 12%, tax credits 11%, and employer-sponsored insurance 7%.
Two-parent (with children present) families also benefit substantially from all these programs (Employer-Sponsored Insurance, Medicaid, tax credits, and means-tested transfers) though less than single parents, commensurate with their generally higher market incomes. Medicaid is the most important program for poverty reduction among two-parent families in New York State (reducing their poverty by 6% points).
Medicaid reduces poverty among persons in two-adult (no children present) families by close to two percentage points.
On the other hand, although they are nearly as poor as lone-parent families, lone-adult households get very little poverty relief from social transfers (Figure 13).
Impacts on HIPM poverty gaps. The poverty gap is a measure of the depth of poverty (see Methods). It is the amount by which the resources of the average poor family fall short of the HIPM poverty line. Analyses of impacts of social and health benefits on poverty gaps provide an important complement to analyses of impacts on poverty rates since some social programs increase the resources of poor families importantly yet fail to remove them from poverty.
Poverty gap analyses are conducted for New York State households with market incomes (after taxes and some work and child care expenses) less than the HIPM poverty line. The health and social benefits they receive are then added to this market income, sequentially, to show how much such benefits reduce the depth of poverty.
For all persons, the poverty gap based on market income alone is about 47 percent, meaning private income alone meets just over half their basic needs (Figure 14).
Health insurance benefits (employer insurance, Medicare, Medicaid and ACA premium subsidies) meet about 17% of needs. Put differently, these health insurance benefits close 36% of their pre-transfer poverty gap (that is, 17/47 = 0.36).

23
Social insurance, means-tested transfers and tax credits together meet another 13% of needs, resulting in a poverty gap after all benefits of 16.9%. Thus, among those with market incomes below the HIPM poverty line, average resources after all benefits amount to 83% of basic needs: market income fills 53% of basic needs of poor families, all benefits together fill another 30%; so over half of the poverty reduction from benefits is attributable to health insurance.
Among households with low market incomes, the impact of health insurance benefits does not differ greatly across racial/ethnic groups in NY State. All racial/ethnic groups see very substantial poverty gap reductions from employer insurance and Medicaid (Figure 14).
Means-tested transfers have especially large impacts on poverty gaps for Hispanics and non-Hispanic blacks, although non-Hispanic whites and Asians benefit as well. Mainly as a result of the difference in the impact of means-tested benefits, the post-transfer poverty gap is somewhat higher among poor whites and Asians (18.5% and 22.0%, respectively) than among poor Hispanics and blacks (15.7% and 13.0%).
The impact of health and social benefits on poverty gaps varies by family structure. These benefits greatly reduce the depth of poverty among poor one- and two-parent families; respectively, their poverty gaps are 60% and 44% before counting health and social benefits, but 14% and 13% after. For single-parents, health insurance benefits (mostly Medicaid) account for 19 of the 46-percentage-point-impact from all benefits; means-tested benefits contribute another 20 points. For poor two-parent families, health insurance benefits account for over half the reduction in the depth of poverty.
Lone adults’ pre-transfer poverty gaps exceed 60%. Yet they get little poverty relief from health and social benefits. Employer insurance and Medicaid together fill about 10% of their needs and all other social benefits another 8%. The post-transfer poverty gap for poor lone adults is 42%, meaning that, on average, all their resources combined cover just over half (58%) of their basic needs.
Two-adult families without children present are also left with a large poverty gap (27%, on average) after all benefits. These families benefit more than lone adults

24
from health insurance (especially Medicaid) and means-tested benefits.
Finally, health insurance benefits have large impacts on the poverty gaps of program recipients and their families (Figure 14). Medicaid alone meets 20% of the basic needs of poor Medicaid recipients. Employer insurance meets over 10% of the needs of poor persons with employer insurance coverage. Post-transfer poverty gaps of those covered by employer insurance or Medicaid are 11.2% and 12.5% respectively, meaning that their resources meet nearly 90% of their basic needs.
The story is quite different for the low-income individually insured or uninsured persons. For the individually insured, premium subsidies meet 3.5% of their basic needs. All benefits combined reduce the poverty gap of the individually insured from 52% to 30% so that, after all transfers, their resources amount to only 70% of their basic needs, on average.
The situation is similar for poor uninsured persons. Their poverty gap after all transfers stands at 31%. (However, the poverty gap of the uninsured is reduced by the health insurance benefits of other family members since poverty is determined for entire family units.) These estimates for the uninsured do not account for any of the free care that the uninsured receive.
B. Poverty rates including free care to the uninsured
We next turn HIPM poverty rates that incorporate two different insurance values for estimated “free care” provided to the uninsured: “HIPM Free Care” and “HIPM Free Care – Alt.”
“HIPM Free Care” is based on our estimates of budgetary expenditures per uninsured person from DSH and both direct Federal funding and charitable funding for FQHCs (see Methods). The Free Care implicit insurance benefit represents a substantial increase of resources for the uninsured and their families compared to the HIPM, where the uninsured are assumed to have no health benefits. On average, we estimate expenditures on the uninsured amount to 41% of the basic plan cost (i.e. 41% of the basic insurance need, see Methods). Thus, for estimates reported in this section, we have added to the resources of the
uninsured a health insurance benefit equal to 41% of the health insurance need.
“HIPM Free Care-Alt” is similar to “HIPM Free Care,” but based on the results of the Oregon Medicaid experiment. For HIPM Free Care–Alt estimates, we add to the resources of the uninsured a health insurance benefit equal to 60% of the health insurance need (see Methods).
Figures 15 shows these results for the NYC Metro Area within NY State, for NY State outside Metro NYC, and for NY State as a whole. For reference, these figures also include the SPM rate and the HIPM rate without free care (“HIPM”).
Adding an insurance value for free care reduces the HIPM poverty rate by 0.9 to 1.5 percentage points in Metro NYC, 0.6 to 0.7 percentage points in NY State outside Metro NYC, and by about 0.8 to 1.3 points for the NY State as a whole.
This 0.8 to 1.3 percentage point poverty impact of free care on HIPM poverty rates in NY State is far smaller than the impact of employer insurance, Medicare or Medicaid, but larger than the impact of ACA premium subsidies (e.g., see premium subsidy impact in Fig. 9).
The reduction in these poverty rates from free care necessarily reflects the impact of free care on the poverty of the uninsured and their families. The larger impact of free care in Metro NYC than outside reflects the higher uninsurance rate in the Metro area (9.0% vs. 7.7%, Appendix Table A1), since the impact of free care on the poverty of the uninsured is similar in the two areas (Figure 16). Specifically, among the uninsured, “Free Care” lowers the poverty 5.6 percentage points in Metro NYC and 6.5 percentage points outside.

25
However, “Free Care-Alt” lowers HIPM poverty by ten percentage points in Metro NYC, seven percentage points in NY State outside Metro NYC, and nine
percentage points in NY State overall.71 Recognizing the insurance value of free care to the uninsured, however,
does not change the fact that the uninsured are very poor, with HIPM poverty rates exceeding 36% in the state after including an insurance value of free care.
C. HIPM poverty gaps including Free Care to the Uninsured
In New York State, free care reduces the poverty gap overall by a modest amount, but substantially for some groups, particularly the uninsured (Figure 17). For all persons, Free Care meets 1.5% of basic needs. The impact of free care on the poverty gap is far smaller than that of Medicaid or employer health insurance, though larger than the impact of ACA premium subsidies.
The larger impact of free care compared to ACA premium subsides reflects the greater number of uninsured than individually insured among the pre-transfer poor. Free care alone meets 7.7% of the basic needs of the uninsured. As a result, the post-transfer poverty gap among poor uninsured persons falls from 31.1% when free care is ignored (Figure 14) to 24.4% when an insurance value of free care is included in
resources (Figure 17). Thus, free care reduces the post-transfer poverty gap by over a fifth. The remaining post-transfer gap among the poor uninsured is less than the post-transfer gap of poor individually-insured persons (about 30%). Free care appears to close more of the poverty gap of the uninsured than premium subsidies close of the individually insured.

26
Table 2: Summary of Policy Scenarios
Policy Simulation Scenario
Income Below 100% or 133% FPL
Income Above 100% or 133% FPL
ACA+
Income < 133% FPL: All have a basic plan with no premiums and no cost-sharing required.
Income >133% FPL: 1. uninsured undocumented persons and family members of those with affordable ESI (“family glitch”) become eligible for and receive ACA premium subsidies and cost-sharing-reduction subsidies, based on income. a 2. individually insured: full take-up of ACA premium and cost-sharing reduction subsidies, based solely on income with no other restrictions. a 3. ESI: made eligible for ACA premium and cost-sharing-reduction subsidies, based on income.a (Reduces deductions from resources for premiums and cost-sharing.)
NYHA
Income < 133% FPL: All have a basic plan with no premiums and no cost-sharing required.
Income >133% FPL: All have a basic plan with no premiums and no cost-sharing required
Rollback1 b
Income < 100% FPL: All non-elderly, non-disabled adult Medicaid recipients with no children present lose Medicaid; it is replaced with “Free Care” with an implicit insurance value of 41% of the Basic Plan.
Income > 100% FPL: All non-elderly, non-disabled Medicaid/CHIP recipients lose Medicaid/CHIP; it is replaced with Free Care with an implicit insurance value of 41% of the Basic Plan.
Rollback2 b
Income < 100% FPL: non-disabled, non-elderly adult Medicaid recipients with no children present lose Medicaid; replaced with “Free Care – Alt” with an implicit insurance value of 20% of Basic Plan.
Income > 100% FPL: All non-elderly, non-disabled Medicaid/CHIP recipients lose Medicaid/CHIP; it is replaced with Free Care – Alt with an implicit insurance value of 20% of the Basic Plan.
Notes: FPL: Federal Poverty Level; ESI: Employer Sponsored Insurance a. Income-based eligibility: up to 400% FPL for premium subsidies; up to 250% FPL for cost-sharing-reduction subsidies. b. We do not estimate counterfactual out-of-pocket spending for Medicaid Rollback scenarios. This leads us to under-estimate the increase in poverty under this scenario. However, we also do not allow Medicaid losers to access ACA premium subsidies or gain employer insurance. This (likely) leads us to over-statement poverty under this scenario.

27
VII. Results: Policies to Expand and Contract Health Insurance benefits Table 2 summarizes the different policy simulation scenarios. For additional details, see Methods. Recall that these impacts are not causal estimates, because they do not account for behavioral or health responses to program changes.
A. Impact of expanded insurance on HIPM poverty rates and gaps
Figures 18 through 21 show poverty rates and program impacts under two insurance scenarios: the more incremental ACA+ and the universal NYHA.
We compare estimated rates under the expansion scenarios to the HIPM Free Care rate to show the additional poverty reduction from expansions of insurance, above and beyond that provided by free care. We also compare rates under the expansion scenarios to the baseline HIPM rate.
The HIPM poverty rate in NY State would be far lower than the baseline (status quo) rate under either expansion policy: 18.8% baseline vs. 14.7% under ACA+ or 13.7% under NYHA (Figure 18). The more incremental ACA+ achieves about 4/5 of the poverty reduction that the NYHA would achieve for NY State.
Compared to the poverty rate that incorporates an insurance value of Free Care for the uninsured, HIPM Free Care, the reduction in the HIPM poverty rate is still substantial: 3.3 percentage points under ACA+ or 4.3 percentage points under NYHA.
This 4.3 percentage point reduction in poverty from enacting the NYHA exceeds the current impact shown in Figure 9 for all non-health social insurance program combined, all refundable tax credits (3.2% points) and is
nearly as larger as the combined impact of all non-health means-tested benefits (5.1% points).
Overall, the impact of universal insurance is fairly similar in the NYC metro area and outside: compared to the baseline HIPM, the ACA+ would reduce poverty by 4.1% points in the NYC metro area and by 4.2% points outside. However, relative to the ACA+, NYHA would reduce poverty by an additional 1.2% point in the NYC Metro area but by only an additional 0.4% points outside.
We would expect the primary beneficiaries of universal insurance to be currently uninsured persons and those with individual or employer insurance who have large out-of-pocket payments. Figure 19 shows the impact of universal insurance according to baseline insurance status.
As expected, expanding insurance would greatly reduce the poverty of the uninsured. The HIPM rate would fall from a baseline of 45.5% to 30.4% under ACA+ and to 28.1% under the NYHA, a 17.4% point reduction. (The reduction is 11.6% points compared to HIPM Free Care.) Put differently, over half (54.5%) the uninsured are “not poor” and so could not be removed from poverty by NYHA. But the NYHA would lift 38% of the uninsured poor from poverty.
Expanded insurance would also provide major benefits to the individually insured, reducing their poverty rate from 37.3% to 25.9% under ACA+ and to 22.2% under the NYHA. And, although those with employer insurance (ESI) have very low poverty rates, they would nonetheless benefit from ACA+ and NYHA. The NYHA would cut their poverty by over two percentage points.
Since coverage and benefits for current Medicaid recipients would be similar to the ACA+ and NYHA

28
policies, we did not expect their poverty rates to be much affected by expanded insurance. That expectation was only partly fulfilled. Poverty rates of Medicaid recipients would fall by 4% points under the ACA+ and by 5% points under NYHA (Figure 19). Medicaid recipients benefit from gains in insurance coverage by family members who were uninsured or insured but
made substantial out-of-pocket payments for premiums or care.
All demographic groups benefit from expanded insurance (Figure 20). For many groups, the ACA+ would reduce poverty by about five percentage points and the NYHA would reduce poverty by an additional 1 to 2% points.
Noncitizens would experience the greatest (absolute) poverty reductions from expanded insurance. For all noncitizens, the ACA+ would reduce poverty by over seven percentage points and the NYHA by 9 percentage points. Among those we impute to be undocumented, the ACA+ would reduce poverty by 10 percentage points and the NYHA would reduce it by 11.3 percentage points. Thus, the ACA+ would achieve 2/3 or more of the poverty reduction of the NYHA.
As we have seen, universal insurance would raise a substantial fraction of the poor out of poverty. But it would also reduce poverty gaps: the depth of poverty among those who are poor based on their private income alone. Figure 21 shows the HIPM poverty gaps (how much the income of the poor falls below the HIPM
poverty threshold) under the baseline, free care, ACA+ and NYHA.
For NY State, private cash income of the poor (after taxes and necessary work expenses) meets just over half of basic needs, leaving a poverty gap of 47.8% of the needs threshold (see Figure 14). All cash and in-kind benefits meet about 30% of the basic needs of the pre-transfer poor, leaving a “baseline” poverty gap of 16.9% (shown in Figure 21). Simulations indicate that universal insurance would reduce the poverty gap further, to 11.1% (ACA+) or 10.8%, (NYHA). Thus, the NYHA would cut the poverty gap by more than one third.

29
The impact of expanded insurance differs across current health insurance types. The uninsured get comparatively little relief from current transfer programs: thus, their baseline post-transfer poverty gap is 31.1%. But universal insurance would cut the baseline poverty gap of the uninsured by more than half: the ACA+ by 15.8% points and the NYHA by 16.4% points.
The poor individually-insured would also experience great reductions in poverty gaps (14-15% points) from expanded insurance. Poor Medicaid beneficiaries would get little additional poverty gap reduction from either expanded insurance policy, since they have similar coverage currently. The ACA+ and the NYHA reduce the poverty gap of low income persons covered by employer sponsored insurance only modestly, from 11% to 8%.
B. Impacts of Medicaid Expansion Rollbacks on HIPM Poverty Rates.
Figures 22 through 25 show poverty rates and program impacts under two scenarios rolling back the Medicaid and CHIP programs (“Rollback1” and “Rollback2”). The same Medicaid recipients are projected to lose benefits in the two scenarios: everyone in households with incomes above 100% of FPL and all non-elderly, non-disabled adults without children with incomes below 100% FPL. Table 2 summarizes the scenarios. For additional details, see Methods.
The two scenarios differ only in assumptions about the free care available to Medicaid losers (and to all uninsured persons). Under Rollback1, spending on Free Care for the uninsured per uninsured person remains constant, so the implicit value of free care remains at 41% of a basic insurance plan. Under Rollback2, the
budget for financing Free Care remains constant despite growth of the uninsured population, so the implicit insurance value of Free Care falls to 20% of the basic plan value.
Since, like other uninsured persons, those who lose Medicaid are assumed to get some Free Care, we compare the simulated Medicaid Rollback poverty rates to current HIPM Free Care rates. Poverty rates would rise sharply under either Rollback scenario (Figure 22). In NY State, the HIPM rate would rise 2 to 3% points, from 18.0% to 19.9% (Rollback1) or 21.0% (Rollback2). The increases in poverty are sharper in the NYC Metro: 2.4 to 4.0 percentage points. Outside the NYC Metro area, HIPM poverty would increase 0.7 to 1.4 percentage points.
Medicaid rollbacks hit Medicaid enrollees particularly hard (Figure 23): their HIPM poverty rates rise five to thirteen percentage points under the Rollback1 and Rollback2 scenarios, respectively. Poverty of the uninsured also rises under Rollback1 (1 to 4 percentage points) as persons with whom they live lose Medicaid benefits. Poverty of the uninsured rises further under Rollback2 as the growing number of uninsured reduces per capita expenditures on care of the uninsured, thus eroding the implicit insurance value of free care for the uninsured.
The poverty rates of people with Individual or Employer-Sponsored Insurance are mostly unaffected by Medicaid Rollbacks (Figure 23).

30
Poverty among lone-parent families, Hispanics and Non-Hispanic Blacks in NY State would increase 4 to 6 percentage points under Medicaid Rollbacks (Figure 24).
The increase in child poverty (2-4% points) is moderated by our assumption that the poorest families with children (<100% FPL) remain eligible for Medicaid.

31
Although undocumented persons are generally not eligible for Medicaid (and none of those we impute to be undocumented get Medicaid), nonetheless, poverty of imputed undocumented persons is projected to rise roughly 5 to 7% points under Medicaid Rollbacks. This rise has two sources. First, losses of Medicaid to co-resident family members makes the entire family poorer. Second, since many undocumented persons are uninsured, in the Rollback2 scenario, poverty among undocumented persons rises further as free care spending per uninsured person falls and, consequently, reduces the implicit insurance value of free care to uninsured undocumented persons.
Rolling-back Medicaid expansion would also increase the poverty gap in New York State (Figure 25).
The largest impacts are felt by Medicaid recipients: an increase in the gap of 4 to 6 percent, or roughly one third to one half. However, the uninsured also experience large increases in poverty gaps, especially from Rollback2 (which increase their poverty gap by nearly 5 percentage points, or by one fifth). Poverty gaps of those with Individual or Employer Insurance change little.
VIII. Discussion
A. Limitations
Our policy simulations show the direct effects of adding or removing health insurance benefits from family resources, but not the effects of changes in behavior that occur as a result, such as changes in labor supply or income. Most importantly, with the exception of the New York Health Act and ACA+ policies, we do not attempt to model the effects of policy changes on out-of-pocket spending for health care.
For the NYHA, which eliminates cost-sharing, it is straightforward to incorporate its effect on out-of-pocket spending by no longer deducting out-of-pocket expenses from resources. Modeling how out-of-pocket expenses change when people lose Medicaid benefits is, however, beyond the scope of this work and the most significant limitation. Future research should implement the HIPM using counterfactual estimates of out-of-pocket spending under Medicaid Rollbacks.72
On the other hand, we assume that all Medicaid losers become uninsured and resort to Free Care, though some would likely obtain individual insurance (and ACA subsidies) or Employer-Sponsored Insurance. For those reasons, we would modestly overstate the increase in HIPM poverty from Rollbacks. On balance, we likely underestimate the increase in poverty from rollbacks of Medicaid Expansion, yet nonetheless estimate large increases in health-inclusive poverty.
Our estimate of the implicit insurance values of free care are approximate, as explained in Methods. Our preferred estimate, 41% of the cost of a basic plan, is based on documented in-flows of funds meant for free care for the uninsured, but is likely an underestimate. First, it neglects care funded by cross-subsidies from insured patients. Second, it does not include funds for NY State hospitals in financial distress that are not specifically targeted for the uninsured. Finally, it misses philanthropic funding of health care for the uninsured, other than that going to Federally Qualified Health Centers. On the other hand, our alternative free care estimates of 60% of the basic plan are based on care received, albeit in a different state. The overall poverty rate estimates are not very sensitive to this choice, although the poverty rates for some groups, such as the uninsured, are affected.
Our Medicaid Rollback scenarios, unlike some ACA replacement proposals73, remove Medicaid and CHIP from all children above 100% FPL, but preserve Medicaid eligibility for all parents below 100% FPL. If NY State or the Federal government were to provide more generous eligibility for children in Rollbacks, then our simulations would over-estimate the impact on child poverty.
Our estimates of the effects of expansionary policies, ACA+ and the New York Health Act, consider only their

32
direct impacts on health inclusive poverty. We do not model how the financing of these programs would affect tax burdens, or the other resulting changes in employment, health insurance markets and so on. Especially for a large and complex reform like the NYHA, some of these indirect effects could be substantial. Advocates also suggest that that health care costs, and thus the premium of the Basic Plan, would fall, an indirect effect that could lower poverty further.74
We used the Current Population Survey for our estimates and simulations, the same dataset the US Census Bureau uses for its poverty measures. While the CPS provides representative estimates for states, its estimates may not be representative for smaller geographic units. Consequently, our separate estimates for NYC Metro and the remainder of the state may suffer from lack of representativeness. We also do not have direct survey information on undocumented status and so imputed it using the method of Borjas.75 Inaccuracy of our imputation method and under-representation or selective participation of undocumented persons in the survey would both affect the accuracy of results.
Finally, the SPM has a number of limitations,76 and because the HIPM is a modification of the SPM, it shares those limitations.77 Despite these limitations, some policy implications seem clear.
B. Implications for policy in New York State
Health care and insurance are expensive for individuals, employers and government. Many proposals, such as the recent Health Care Choices Proposal,78 would cut or erode health insurance benefits to lower-income households, through Medicaid rollbacks, and requirements for work and out-of-pocket spending. Other plans would expand and enhance health insurance benefits for households with low and moderate incomes. Expansion plans include the New York Health Act we examined, a variety of “Medicare for all” proposals, and more incremental proposals, such as the ACA+ policy we examined.
How would such policies to contract or expand health insurance affect inequality, or at least the ability of people to meet their most basic needs? Traditional
poverty measures cannot tell us. As Gary Burtless said to New York Times columnist Eduardo Porter in 2012, “Our entire system of redistribution is tilted in the favor of giving the poor medical care, but we’re not going to count that? […] That’s ridiculous!”79
The health inclusive poverty measure we used in this report does count the health insurance benefits to the poor. It defines a family as poor if it lacks the resources to pay for health insurance and out-of-pocket payments for care, as well as basic food, shelter, clothing, utilities and other needs. This approach raises the poverty threshold (poverty line), about 45% above80 the Census Bureau’s Supplemental Poverty Measure threshold. For those who consider health insurance a basic need, it’s the right way to measure poverty. Further, the HIPM allows analysts to study the direct impact on poverty of policies that would expand or contract health insurance.
These estimates also represent the first attempt to incorporate the value of free care for the uninsured into health inclusive poverty. Incorporating free care is especially important for understanding the impacts of policies that are designed to replace, wholly or in part, free care. Neglecting free care over-estimates the impact of expansionary policies. Neglecting free care also under-estimates the poverty-increasing effects of contractionary policies, such as Medicaid rollback. However, free care provision is not necessarily static; it depends on funding.
To make good decisions about health policies, New Yorkers need to know how many more—or fewer—New Yorkers will be poor under those policies. That requires a poverty measure that incorporates health insurance needs and benefits.
Our results show that policies to expand health insurance benefits would reduce the poverty rate substantially in New York State, by about one quarter. The incremental policy (ACA+) reduces poverty overall nearly as much as the more universal, NYHA.
Proponents may prefer NYHA for many reasons, including providing the same benefits to all. Alternatively, others could prefer the incremental approach because it is less disruptive to existing systems of health insurance, health care, taxes, and the overall economy. While we analyze only one aspect of

33
these policies, their similar effects on health inclusive poverty are noteworthy.
Our results show the large increases in poverty of rolling back Medicaid expansion, even without incorporating the higher out-of-pocket spending that would likely follow. These large poverty impacts should not be surprising, given how much of US social spending takes the form of health insurance. Still, we show clearly that, if we believe health insurance is a basic need, then Medicaid Expansion Rollbacks will throw nearly 400,000 additional New Yorkers into poverty. And those results assume a doubling of expenditures on free care for the uninsured. If total spending remains flat, then the number impoverished by Medicaid Rollbacks in New York State would instead rise by nearly 600,000, including nearly 200,000 children.

30
IX. Appendix 1: Additional Tables and Figures
Table A1: Sample Means and Proportions, 2014/2015 Source: Current Population Survey Annual Social and Economic Supplement, authors tabulations
Characteristics
NYC Metro in NY State
Balance of NY State
New York State USA
Health Insurance Status and Type (%) Medicaid 19.5 15.4 18.3 15.3 Individual 9.7 7.0 8.9 8.4 Uninsured 9.0 7.7 8.6 11.7 Employer, Medicare, and other 61.8 69.9 64.2 64.6 Race/Ethnicity (%) Hispanic 24.5 19.6 18.8 19.8 Non-Hispanic Whites 44.9 59.8 55.4 59.1 Non-Hispanic Blacks 16.2 11.8 13.6 12.0 Non-Hispanic Asians and others 14.4 8.9 12.2 9.1 Age (%) 0 to 5 8.4 9.4 8.7 9.2 6 to 17 17.8 17.5 17.7 18.9 18 to 25 13.9 12.7 13.5 13.0 26 to 34 16.0 16.1 16.0 14.7 35 to 49 22.9 20.9 22.4 22.7 50 to 54 8.2 7.2 7.9 7.8 55 to 59 6.9 8.0 7.2 7.3 60 to 64 6.0 8.3 6.6 6.3 Family structure (%) Single male 6.6 6.6 6.6 6.2 Single female 5.3 5.4 5.3 4.8 Adult couple 16.3 19.7 17.3 18.6 3+ Adults, no kids 16.3 10.5 14.6 11.4 Single male with kids 0.4 0.6 0.5 0.9 Single female with kids 6.0 6.5 6.2 5.8 Two parents with kids 31.3 37.5 33.1 37.1 3+ Adults with kids 17.7 13.3 16.4 15.1 Education of head (%) Less than HS 11.5 10.8 10.3 10.8 HS grad 23.4 25.3 24.0 25.2 Some college 21.0 29.0 23.6 28.7 College grad 44.2 34.9 42.0 35.3 Citizenship (%) Citizen by birth 71.2 86.5 77.9 85.8 Naturalized citizen 14.9 5.5 11.1 5.9 Non-citizen 13.9 8.0 11.0 8.3 Non-citizen, imputed undocumented 7.5 5.1 6.0 5.2
(continues)

31
Table A1 (continued) NYC
Metro Balance of NY State
New York State USA
Non-health insurance resources relative to needs (%) < 50% of SPM threshold 4.7 3.2 4.2 4.1 50% SPM threshold to SPM threshold 10.6 6.5 9.4 7.4 SPM threshold to midpoint SPM-HIPM threshold 7.8 5.0 7.0 5.4 Midpoint SPM-HIPM to HIPM threshold 9.1 5.9 8.2 6.6 HIPM threshold to 150% HIPM threshold 22.1 19.3 21.3 21.8 Above 150% HIPM threshold 45.8 60.1 49.9 54.8 Premiums and Needs ($) Silver Plan Premium for 27 year-old (2nd cheapest) 4,402 2,790 4,210 2,861 SPM threshold 28,858 23,768 26,750 23,990 HIPM threshold 42,303 34,785 39,375 35,113 Health Insurance Need 13,445 11,017 12,625 11,123 Non-health insurance resources 78,753 69,317 75,686 69,728 Benefit receipt (%) TANF or welfare 0.7 0.5 0.7 0.5 SNAP 11.8 11.8 11.6 11.8 Unemployment compensation 1.2 1.6 1.5 1.6 EITC or Child Tax Credit 26.5 23.8 25.7 27.7 Social Security 1.1 1.5 1.5 1.5 Housing assistance 6.3 3.7 5.5 2.6 Medical Out-of-Pocket Expenditures: MOOP ($) Total SPM Unit MOOP 4,359 4,959 4,406 4,933 Total Health Insurance Unit MOOP 2,770 3,303 2,825 3,280 Premium MOOP, HIU 1,726 1,887 1,728 1,880 Capped Premium MOOP, HIU 1,478 1,704 1,500 1,694 Non-Premium MOOP, HIU 782 1,174 849 1,157 Capped Non-Premium MOOP, HIU 660 1,042 735 1,025 Capped Non-Premium MOOP, SPMU 1,012 1,519 1,126 1,497 Housing tenure (%, except where indicated) Owns home outright 16.1 18.7 17.4 18.6 Owns with mortgage 33.2 46.2 38.0 45.6 Renter 50.7 35.1 44.6 35.8 Housing subsidy amount (SPMU, capped) ($) 593 179 490 197 Employment status, ages 18+ (%) Works FT 58.8 58.5 58.0 58.5 Works PT 9.7 13.2 11.3 13.1 Unemployed 3.8 4.0 3.7 4.0 Out of labor force 27.6 24.3 26.9 24.5 Health Insurance Subsidy, if individually insured Subsidy amount, if individually insured ($) 1,308 1,630 1,191 1,614 Received subsidy if individually insured (%), imputed 30.0 33.9 29.3 33.7 Unweighted Sample Count 8,538 3,330 11,868 300,587

32
IX. Appendix 2: Poverty Measure Concepts Table: Official, Supplemental and Health Inclusive
Official Poverty Measure (OPM)
Supplemental Poverty Measure (SPM)
Health Inclusive Poverty Measure (HIPM)
Measurement Units
Families or unrelated individuals
Families, including any co-resident unrelated children who are cared for by the family and any cohabiters and their relatives, or unrelated, non-cohabiting individuals
Same as SPMi
Non-Health Needs
Three times cost of minimum food diet in 1963ii
The mean of expenditures on food, clothing, shelter, and utilities (FCSU) over all two-child consumer units in the 30th to 36th percentile expenditure range, multiplied by 1.2
Same as SPM measure of non-health needs
Adjustments to Non-health Needs
Vary by family size, composition, and age of householder
Geographic adjustments for differences in housing costs by owner/renter status and a three-parameter equivalence scale for family size and composition
Same as SPM
Updating Non-health Needs
Consumer Price Index: all items
5-year moving average of expenditures on FCSU Same as SPM
Health Insurance Needs
Small amount implicit in the 3X multiplier
Explicitly: None. However, implicitly, all out-of-pocket expenditures on insurance premiums (premium MOOP), because they are deducted from resources as “nondiscretionary” expenses.
Unsubsidized Premium of Basic Health Insurance Plan
Cost-sharing and Uncovered Health Care Needs
Small amount implicit in the 3X multiplier
Explicitly: None. However, implicitly all out-of-pocket expenditures on care and/or cost-sharing (non-premium MOOP), because they are deducted from resources as “nondiscretionary” expenses.
Explicitly: None. However, implicitly, capped out-of-pocket expenditures on care (non-premium MOOP, up to the available cap depending on health insurance type) because they are deducted from resources as “non-discretionary” expenses.
Resources: Non-Health
Gross before-tax cash income
Sum of cash income, plus noncash benefits that families can use to meet their FCSU needs, minus taxes (or plus tax credits), minus work expenses and child support paid to another household minus out-of-pocket medical care and insurance and over-the-counter expenses (MOOP)
SPM Resource Measure but without the MOOP subtraction
Resources: Health Insurance
None
None
For those who get private or public health insurance benefits: Unsubsidized premium of Basic Plan minus actual premium MOOP (limited to premium MOOP necessary to obtain Basic Plan). For those eligible for premium subsidies: subsidy value.
Source: Korenman and Remler (2016, Table 1). The OPM and SPM descriptions are partly based on Short (2013, page 3). i However, health insurance needs & resources are determined for Health Insurance Units, subunits of the SPM unit, then aggregated to SPM unit ii A small amount of out of pocket expenditures for health insurance and care is captured by the OPM needs threshold.

33
IX. Appendix 3: Methods for Implicit Insurance Value of Free Care from Inflow of Funds and Eroded Insurance Value of Free Care Under Medicaid Rollback (“Rollback2”) This appendix provides further details of the method for calculating the implicit insurance value of free care using inflows of funds. It also provides details on the methods for calculating the reduced value under the Medicaid Expansion Rollback, where we assume maintenance of the dollar value of funds, which are spread across a larger uninsured population. Total Funds for Free Care for the Uninsured Total in-flows of money for free care for uninsured in NY State = = Federal HRSA Funding for FQHCs in NY + Charitable Funding for FQHCs in NY + DSH Funding for Hospitals in NY for the uninsured Charitable Funding for FQHCs in NY = (Estimated Federal HRSA Funding for FQHCs in NY in 2014) * (FQHC Revenue share from “Philanthropy/Other” / FQHC Revenue share from Federal HRSA) “Philanthropy/Other” refers to revenue shares as reported by the Community Health Care Center of New York State, which classify as “Other Non-Patient” revenue that is not from insurers, patients or direct government funding.81 It includes philanthropy from all sources. DSH Funding for Hospitals in NY for uninsured = DSH Funding for Hospitals in NY * (DSH estimated costs for uninsured in 2013)/(DSH total funding in 2013) Total Uninsured Population and Age Adjustment In the CPS (used for our HIPM analyses), health insurance status and type variables refer to status over the entire year. Therefore, in the CPS, the estimate of the uninsured population misses the part-year uninsured. However, the part-year uninsured make use of free care when uninsured. Therefore, we use the point-in-time estimates of the ACS to calculate the number of uninsured. Our implicit insurance value of free care is calculated as a proportion of the premium charge on the ACA marketplace the uninsured person’s place of residence (rating area). Because expenditures on care of the uninsured depend on age, we age-adjust our total spending on free care. NY State age-rates premiums for exchange plans in only three age- groups: 0-18, 19-64, 65+. Thus, let: Total population of uninsured people = U pA = Share of uninsured population in each age group = (# uninsured in group A)/U CA = Ratio of Average cost of (expenditures on) health care for age group A relative to non-elderly adults CA = 1 if Age = 19-64 = .635 if Age = 0-18 (from Federal Exchange guidelines for incremental cost of one child) = 2.991 in 2014 if Age = 65+, Full Plan Cost for MA-PD Plan/Full Plan Cost for adult 19-64

34
2.932 in 2015 So 2.962 for 2014-2015 pooled data
We use the following Identity: F = Total $ of free care on uninsured = sum over age groups of # in each group * average spending on group F = ΣA (pA * U) * (CA * E) Where E is an age adjusted per uninsured person free care expenditure. It has units of $ per uninsured person and is a constant. Rearranging, F/U = E ΣA pA * CA E = (F/U) / (ΣA pA * CA) Then each person in age group A gets CA * E in age-adjusted implicit insurance value. (Values are shown in the table below.) Dividing the total inflow of funds in 2014-15 by the sum of the estimates of the uninsured population in 2014 and in 2015 (from the ACS): Pooled: F/U = $ 5,579,417,892 / 3,077,104 = $1813 Pooled 2014-15 Uninsured population (U) & Shares of Uninsured Population by Age Group (pA)
U2014-15 (From ACS)
2014-15 pop share (pA)
CA CA * E (implicit insurance value)
<18 241,168 .08106 .635 $1,147 18-64 2,785,430 .903 1.0 $1,807 65+ 50,506 .01598 2.9615 $5,351 Total 3,077,104
F/U = E ΣA pA * CA Thus, the age-adjusted value of free care per uninsured, E = F/[U*ΣA pA * CA] = $1813/ 1.0035 = $1807 Geographic Variation Our geographic distribution adjustment gives each household (more precisely, each uninsured health insurance unit) an equal fraction of the value of the second-cheapest silver plan available in his/her ACA rating area. Specifically, this value is based on the ratio of the adult free care implicit value to the average BCP (population- weighted) for a single adult, averaged over 2014 and 2014. Benchmark Silver Plan premium adult average 2014-15 = ($4323 +$ 4481)/2 = $4402 Ratio of adult implicit free care to Benchmark Silver Plan = $1807/$4402 = 0.41 Each person, of any age, therefore, receives 41% of their Basic Plan value.

35
Implicit Insurance Value of Eroded Free Care Under Medicaid Expansion Rollback: Rollback2 Our simulations show the impact on poverty of the growth in the uninsured population that results from the Rollback of Medicaid Expansion. Our Rollback1 scenario assumes that the value of free care for the insured remains constant relative to basic insurance at 41%. That would require significant increases in funds to maintain that care. For our Rolllback2 scenario we assume that funds available for care of the uninsured remain constant and must fund care for more uninsured people. To simulate the number of newly uninsured, we estimated the proportional increase in uninsured in each of the three age from our analyses of CPS data and applied those proportions to our baseline uninsured numbers from the ACS. We then performed the same calculations as described above. Our simulations indicate that the number of uninsured would more than double. The implicit insurance value falls dramatically, as the same amount of funds are spread across the larger uninsured people. Pooled 2014-15 Uninsured population (U) & Shares of Uninsured Population by Age Group (pA)
U2014-15 (From ACS)
% growth uninsured from Rollback
Estimates Under Rollback
2014-15 pop share Under Rollback
CA CA * E (implicit insurance value)
<18 241,168 370% 1,135,185 0.158 .635 $1,147 18-64 2,785,430 98.7% 5,535,118 0.769 1.0 $1,807 65+ 50,506 0% 50,506 0.007 2.9615 $5,351 Total 3,077,104 134% 7,202,354 1.00
The above table shows the results of our simulation for the uninsured population. Since Medicaid covers many children, rolling back of Medicaid expansion results in a near-quadrupling of the uninsured child population. As a result, the overall age composition shifts toward a younger population whose care is less expensive. Consequently, the very dramatic erosion of the value of free care, as a static amount of funds are spread across far more uninsured people, is somewhat offset because so many of the newly uninsured are children, who are less expensive. Formally, the ΣA pA * CA adjustment under this scenario is 0.889 (compared to 1.0035 in Rollback1). Thus, because, on average, care is less expensive for children than adults, the age adjustment raises the implicit insurance value somewhat, although it is still much smaller than if additional funds had maintained the prior value of free care. Overall, the implicit insurance value = ($ 5,579,417,892 /7,202,354 ) / .889 = $871.03 If we assume that throughout the state, all uninsured receive free care that is an equal share of the basic plan, then that replacement rate is the ratio of this implicit insurance value to the average BCP premium = $871.03 / $4402 = .20 Thus, the increase of the uninsured population against a fixed budget for care of the uninsured lowers the implicit insurance value of free care from 41% to 20% of the value of the benchmark silver plan.

36
Notes
1 Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 2 Barnett JC and Berchick ER. 2017. Health Insurance Coverage in the United States: 2016.September 12.Report Number: P60-260, Table A-5. 3 S. L. Hayes SL, Collins SR, Radley DC and McCarthy D. 2017. What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013–2016, The Commonwealth Fund, December, Appendix Table 2, available at: http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access. 4 United Nations, 1948. The universal declaration of human rights. http://www.un.org/en/universal-declaration-human-rights/ Article 25; see also Saloner B, Daniels N. 2011. The ethics of the affordability of health insurance. J Health Politics Policy & Law 36(5):815–27. 5 Korenman SD, Remler DK. 2013. Rethinking elderly poverty: Time for a Health Inclusive Poverty Measure? NBER Working Paper No. 18900. Cambridge (MA): National Bureau of Economics Research); Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 6 http://www.statecoverage.org/files/Updated-Milliman-Report_GI_and_Comm_Rating_March_2012.pdf 7 For information on the FPL, see https://www.healthcare.gov/glossary/federal-poverty-level-fpl/ 8 Norris, L. 2017. New York and the ACA’s Medicaid Expansion. https://www.healthinsurance.org/new-york-medicaid/ . 9 Bovbjerg RR, Dorn S, Hadley J, Holahan J, Miller DM. 2006. Caring for the Uninsured in New York: What Does It Cost, Who Pays and What Would Full Coverage Add to Health Spending? Urban institute. 10 Citro CF, Michael RT, eds. 1995. Measuring Poverty: A New Approach. National Research Council of the National Academy of Sciences. Washington, DC: National Academy Press. 11 Citro CF, Michael RT, eds. 1995. Measuring Poverty: A New Approach. National Research Council of the National Academy of Sciences. Washington, DC: National Academy Press; Moon, M. 1993 Incorporating health issues in the measurement of poverty. Unpublished paper prepared for the Panel on Poverty and Family Assistance, Committee on National Statistics, National Research Council. Washington, DC: Urban Institute. 12 Korenman SD, Remler DK. 2013. Rethinking elderly poverty: Time for a Health Inclusive Poverty Measure? NBER Working Paper No. 18900. Cambridge (MA): National Bureau of Economics Research); Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 13 Hall MA. 1998. An Evaluation of New York’s Health Insurance Reform Laws. Wake Forest University School of Medicine. November, page 3. 14 Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2.

37
15 Remler, Korenman and Hyson 2017; means-tested benefits include cash assistance, and food and housing programs, but not tax credits, which were considered in a separate category. 16 Semega JL, Fontenot KR, Kollar MA. 2017. Income and Poverty in the United States: 2016. Current Population Reports P60-259. US Census Bureau. September; and Fox, L. 2017. The Supplemental Poverty Measure: 2016. Current Population Reports P60-261 (RV). US Census Bureau. September. 17 Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 18 Citro CF, Michael RT, eds. 1995. Measuring Poverty: A New Approach. National Research Council of the National Academy of Sciences. Washington, DC: National Academy Press. 19ITWG, Observations from the Interagency Technical Working Group on Developing a Supplemental Poverty Measure (Interagency), March 2010, available at www.esa.doc.gov/sites/default/files/spmtwgobservations.pdf 20 Short K. 2012. The Research Supplemental Poverty Measure: 2011. US Census Bureau Current Population Reports, P60-244. November. 21 New York State is one of two states where age rating was prohibited prior to the ACA. The Market Rules and Rate Review Final Rule (45 CFR Part 147) allowed states with community rating to opt for uniform family tiers instead of using the federally mandated age curve for premiums. In New York, this meant that there would be one rate regardless of age for individuals, and a multiplier for families with one adult plus children or two adults plus children, regardless of the number of children. See Center for Consumer Information & Insurance Oversight, Center for Medicare and Medicaid Services. State Specific Family Tier Ratios. 2013. https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/state-rating.html#family; Fontana J, Murawski T, Hilton T. 2017. Impact of Changing ACA Age Structure. Milliman Research Report. January 31, 2017, accessed June 27, 2018. http://us.milliman.com/uploadedFiles/insight/2017/MillimanACAAgeBands_0131_Final.pdf Lorenz S. 2016. Insurance Standards Bulletin Series – INFORMATION: Guidance Regarding age Curves and State Reporting. Health and Human Services Department, December 16, 2016. Accessed June 27, 2017. https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/Final-Guidance-Regarding-Age-Curves-and-State-Reporting-12-16-16.pdf 22 Further details can be found in: Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50(December): 27-35; and in the online Appendix to Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 23 Mayor’s Office of Operations, The City of New York. 2018. New York City Government Poverty Measure 2005–2016. April. http://www1.nyc.gov/site/opportunity/poverty-in-nyc/poverty-measure.page 24 Formerly called the CEO (Center for Economic Opportunity) Poverty Measure. 25 The NYCgov housing cost adjustment relative to the SPM adjustment is approximately 1.53/1.35, a 13 percent increase. Since the housing need is one-half of the full SPM threshold, the NYCgov threshold is increased by 6.5% relative to the SPM threshold. 26 For families living in rent-subsidized housing units, the adjustment equals the difference between what they would be paying for their housing if it were market rate and what they are actually paying out of pocket. The adjustment is capped so that it cannot exceed the housing portion of the NYCgov threshold. The ACS does not provide data on housing program participation. To determine which

38
households in the ACS could be participants in rental subsidy or regulation programs, we match households in the Census Bureau’s New York City Housing and Vacancy Survey (HVS) with household-level records in the ACS. See Appendix C of Mayor’s Office of Operations, The City of New York. 2018. New York City Government Poverty Measure 2005–2016. April. http://www1.nyc.gov/site/opportunity/poverty-in-nyc/poverty-measure.page 27 Specifically, we selected the portions within New York State of the Census Bureau’s “New York-Newark-Jersey City, NY-NJ-PA” Core-Based Statistical Area (CBSA). https://www.census.gov/geo/reference/gtc/gtc_cbsa.html 28 Overall, housing benefits lowered the NYCgov poverty rate nearly 6 percentage points in 2015 (NYCgov report, Table 3.6). In supplemental analyses, we estimate that all housing benefits counted in the SPM and HIPM lower the HIPM poverty rate in NYC by approximately 3 percentage point. Since the NYC population is about 2/3 of the NYC metro population (within NY State), SPM and HIPM poverty rates for the NYC metro area are overstated by 2 percentage points (2/3 times 3 = 2). Since the NYC metro population within NY State is about 57% of the State population, SPM and HIPM poverty rates for NY State are overstated by about 1 percentage point by excluding additional housing benefits in NYC counted by the NYCgov poverty measure. 29 The NYCgov poverty measure is not available for NY State as a whole, let alone the remainder of the US. Although the NYCgov measure uses the ACS, with much larger sample sizes, in theory we could use the NYCgov methods to estimate poverty for NYC residents using the CPS data that Census uses for the SPM and that we use for the HIPM. However, as a practical matter, such estimates would be quite demanding and likely unreliable. First, the CPS has limited geographic information. Second, the NYCgov uses additional data from the NYC Housing and Vacancy Survey to impute rental advantages to the ACS households. The public CPS data lack information required to impute values of rent regulation and other housing advantages for NYC. Nor could we use the ACS data because the survey lacks questions on medical out-of-pocket (MOOP) spending included in the CPS. (NYCgov imputes MOOP spending.) The ACS lacks detailed information on health insurance coverage and type. Since our focus is on the impact of health insurance policy on poverty, the superior health insurance and medical spending information in the CPS were decisive in our choice of data. Nonetheless, we would encourage the New York City Mayor’s Office for Economic Opportunity to consider creating an experimental health-inclusive version of the NYCgov poverty measure. 30 In 2015, among all ages, the 5% with the greatest expenditures had average expenditures of $50,572. https://meps.ahrq.gov/data_files/publications/st506/stat506.shtml 31 In 2014, among the those under age 65, median expenditures were $1040 and mean expenditures were $4430. https://meps.ahrq.gov/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HCFY2014&Table=HCFY2014%5FPLEXP%5F%40&VAR1=AGE&VAR2=SEX&VAR3=RACETH5C&VAR4=INSURCOV&VAR5=POVCAT14&VAR6=REGION&VAR7=HEALTH&VARO1=4+17+44+64&VARO2=1&VARO3=1&VARO4=1&VARO5=1&VARO6=1&VARO7=1&_Debug= 32 Bovbjerg RR, Dorn S, Hadley J, Holahan J, Miller DM. 2006. Caring for the Uninsured in New York: What Does It Cost, Who Pays and What Would Full Coverage Add to Health Spending? Urban institute. 33 Sachs R. 2018. “How do Hospitals Set Their Charity Care Policies? Evidence from Nonprofit Tax Returns” Presentation to the ASHEcon Meetings. 34 Orecki P. 2017. Medicaid Supplemental Payments: The Alphabet Soup of Programs Sustaining Ailing Hospitals Faces Risks and Needs Reform. https://cbcny.org/research/medicaid-supplemental-payments 35 Garthwaite C, Gross T, Notowidigdo MJ. 2018. Hospitals as Insurers of Last Resort. American Economic Journals: Applied Economics 10(1): 1-39. 36 Community Health Care Association of New York State. 2018. Federally Qualified Health Centers New York State Fact Sheet. http://www.chcanys.org/clientuploads/2018%20PDFs/Policy/Facts2018.pdf

39
37 Finkelstein, Amy, Nathaniel Hendren, and Mark Shepard. 2017. Subsidizing health insurance for low-income adults: Evidence from Massachusetts. NBER Working Paper No. 23668. August. Finkelstein, Amy, Nathaniel Hendren, and Erzo F.P. Luttmer. 2016. The Value of Medicaid: Interpreting Results from the Oregon Health Insurance Experiment. November. Revision of NBER Working 21308. 38 A disadvantage of this approach from the HIPM perspective, however, this approach involves some double counting, because such care is partly funded through cross-subsidies by insured patients (i.e., their premiums help pay for the care of the uninsured). The HIPM has already ascribed those cross-subsidies as part of the health insurance benefit of the insured, because those paying for insurance must cover them, even though they fund care for the uninsured. 39 Bovbjerg RR, Dorn S, Hadley J, Holahan J, Miller DM. 2006. Caring for the Uninsured in New York: What Does It Cost, Who Pays and What Would Full Coverage Add to Health Spending? Urban institute. 40 Borjas GJ. The labor supply of undocumented immigrants. Labour Economics. 2017; 46:1-13. 41 Robert Wood Johnson Foundation. HIX Compare 2014 [dataset] 2014 Mar. Available from: http://www.rwjf.org/en/library/research/2014/03/hix-compare-2014-dataset.html 42 National Bureau of Economic Research. CMS Landscape Files Data - Descriptions of the Drug Plans [dataset] 2016 Dec. Available from: http://www.nber.org/data/cms-landscape-files-data.html 43 Heberlein M, Brooks T, Alker J, Artiga S, Stephens J. Getting into Gear for 2014: Findings from a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP, 2012-2013. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2013 Jan. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/05/8401.pdf 44 Smith VK, Gifford K, Ellis E, Rudowitz R, Snyder L. Medicaid in a Historic Time of Transformation: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2013 and 2014. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2013 Oct. Available from: http://files.kff.org/attachment/report-medicaid-in-a-historic-time-of-transformation-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2013-and-2014 45 American Academy of Pediatrics and National Academy for State Health Policy. All 50 2014 State CHIP Fact Sheets. Washington (DC): National Academy for State Health Policy. Available from: http://nashp.org/all-50-states-and-washington-d-c-chip-fact-sheets-for-all-years/ 46 Smith VK, Gifford K, Ellis E, Rudowitz R, Snyder L. Medicaid in an Era of Health & Delivery System Reform: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2014 and 2015 [Internet]. Washington (DC): Kaiser Commission on Medicaid and the Uninsured; 2014 Oct. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2014/10/8639-medicaid-in-an-era-of-health-delivery-system-reform3.pdf 47 Brooks T, Touschner J, Artiga S, Stephens J, Gates A. Modern Era Medicaid: Findings from a 50-State Survey of Eligibility, Enrollments, Renewal, and Cost-Sharing Policies in Medicaid and CHIP as of January 2015. Washington (DC): Kaiser Commission on Medicaid and the Uninsured. 2015 Jan. Available from: http://files.kff.org/attachment/report-modern-era-medicaid-findings-from-a-50-state-survey-of-eligibility-enrollment-renewal-and-cost-sharing-policies-in-medicaid-and-chip-as-of-january-2015 48 For procedures for incorporating premium and cost-sharing information for the exchange Silver plans, Medicaid programs, and Medicare Advantage Prescription Drug plans, and merging plan information to the public-use Current Population Survey data file, see the Appendix to Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837 October 2. 49 Nonetheless, studies that incorporate behavioral responses suggest that difference between marginal impacts and causal estimates are modest for most social programs; Ben-Shalom Y, Moffitt RA, Scholz JK. 2012. An assessment of the effectiveness of antipoverty programs in the United States. In: Jefferson P, editor. The Oxford handbook of the economics of poverty. NY: Oxford University Press. p. 709–49.

40
50 The HIPM threshold used for poverty gap calculations differs from the threshold for poverty rate calculations because it is adjusted to account for needs for non-premium medical spending (i.e., cost sharing needs). For the HIPM poverty rate, we subtracted capped cost sharing expense from resources. For HIPM poverty gaps, we instead add a value for non-premium MOOP needs to the HIPM threshold. That value is capped at the out-of-pocket limit available to the family, depending on the family’s health insurance status and type. 51 https://bphc.hrsa.gov/uds/datacenter.aspx?year=2016&state=NY 52 We obtained 2014 and 2015 funding information from the Federal HRSA program center website. The Community Health Care Association website provides the revenue shares from all major sources. HRSA funding amounts to 11% of FQHC revenues in NY State and all other philanthropic and non-insurer, non-self-pay funding another 16%. Thus, we estimated charitable contributes to be 16/11 times the Federal contributions. 53 The State share is reported in a variety of places in the NY State budget, including, but not limited to the hospital indigent care fund. 54 https://www.kff.org/medicaid/state-indicator/federal-dsh-allotments/?activeTab=map¤tTimeframe=2&selectedDistributions=dsh-allotment&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D 55 Orecki, Patrick. 2017. Medicaid Supplemental Payments: The Alphabet Soup of Programs Sustaining Ailing Hospitals Faces Risks and Needs Reform. https://cbcny.org/research/medicaid-supplemental-payments 56 https://www.medicaid.gov/medicaid/finance/dsh/index.html 57 Finkelstein A, Mahoney N, Notowidigdo MJ. 2017. What Does (Formal) Health Insurance Do, and For Whom? NBER Working Paper 23718. August; Finkelstein, A, Hendren N, Luttmer E. 2016. The Value of Medicaid: Interpreting Results from the Oregon Health Insurance Experiment. November. Revision of NBER Working 21308. 58 In the Oregon Health Insurance Experiment, the uninsured (the “control compliers”) got nearly as much care as those insured by Medicaid as a result of the experiment (the “treatment compliers”), although the controls also spent more out of pocket. As a result, the implicit insurance payments to the uninsured control group were about 60% of those to the experimental Medicaid group; see Finkelstein, A, Hendren N, Luttmer E. 2016. The Value of Medicaid: Interpreting Results from the Oregon Health Insurance Experiment. November. Revision of NBER Working 21308. 59 https://www.nyhcampaign.org 60 For example, Assembly Bill A4738, 2017-2018 Legislative Session. The bill states ““It is the intent of the Legislature to create the New York Health program to provide a universal health plan for every New Yorker, funded by broad-based revenue based on ability to pay….health coverage under those [public] programs will be replaced and merged into New York Health, which will operate as a true single-payer program…no member shall be required to pay any premium, deductible, co-payment or co-insurance under the program.” See https://www.nysenate.gov/legislation/bills/2017/a4738/amendment/original. Accessed June 7, 2018. 61 See Friedman G. 2015. Economic Analysis of the New York Health Act. Report for Assemblyman Richard Gottfried. University of Massachusetts, Amherst. April. 62 Buettgens M, Dubay L, Kenney GM. 2016. Marketplace Subsidies: Changing The ‘Family Glitch’ Reduces Family Health Spending But Increases Government Costs Health Affairs 35(7):1167-75. 63 We implement the cost-sharing reduction subsidies by reducing the cap on out-of-pocket expenditures according to a sliding scale, as described in the original ACA legislation, and as used to develop the schedule of actuarial value increases for lower income households. 64 Grogan CM. 2017. How the ACA Addressed Health Equity and What Repeal Would Mean. Journal of Health Politics, Policy and Law 42(5): 985-993. (see p. 990).

41
65 Leibenluft J, Aron-Dine A, Park E. 2017. Revised Version of Cassidy-Graham Proposal Is More of the Same. Center on Budget and Policy Priorities. September 25. 66 See Kaiser Family Foundation. Medicaid/CHIP Upper Income Eligibility Limits for Children, 2000-2018 https://www.kff.org/medicaid/state-indicator/medicaidchip-upper-income-eligibility-limits-for-children, accessed June 7, 2018. 67 Sommers BD, Oellerich D. 2013. The poverty-reducing effect of Medicaid. Journal of Health Economics 32: 816-832; Blavin F, Karpman M, Kenney GM, Sommers BD. 2018. Medicaid vs. Marketplace Coverage For Near-Poor Adults: Effects On Out-Of-Pocket Spending And Coverage. Health Affairs 37(2): 299-307. 68 The HIPM also caps the deduction of medical out-of-pocket expenditures. All else the same, capping MOOP deductions reduces HIPM relative to SPM poverty. 69Office of Citywide Health Insurance Access. 2016. Medicaid for the Treatment of an Emergency Medical Condition (“Emergency Medicaid”). Fact Sheet. NYC Human Resources Administration. 70 Following the recommendations of Dr. Brett O’Hara, US Census Bureau (personal communication), we combine Medicaid and CHIP due to difficulties of distinguishing between these two programs in the CPS. 71 The poverty rate is less sensitive to the value of free care outside Metro NYC than within because the non-health resources of the uninsured below the HIPM poverty threshold are fairly close to that threshold, so even the lower value of free care is sufficient to lift many out of poverty. 72 This would use the HIPM with out-of-pocket counterfactual estimates similar to those in Sommers BD, Oellerich D. 2013. The poverty-reducing effect of Medicaid. Journal of Health Economics 32: 816-832. Zwede N, Wimer C. 2018. "Antipoverty Impact of Medicaid Growing with State Expansions and with Time." Unpublished manuscript. Columbia University School of Social Work. 73 For a discussion of multiple ACA replacement proposals, see Aron-Dine A, Broaddus M. 2018. Latest Republican ACA Repeal Plan Would Have Similar Impacts on Coverage and Health As All the Others. Center for Budget and Policy Priorities. June 20. https://www.cbpp.org/research/health/latest-republican-aca-repeal-plan-would-have-similar-harmful-impacts-on-coverage-and 74For one set of estimates, see Friedman, G. 2015. Economic Analysis of the New York Health Act. https://d3n8a8pro7vhmx.cloudfront.net/pnhpnymetro/pages/89/attachments/original/1425994768/Friedman_Fiscal_Study_New_York_Health_Act_FINAL_3-10-15_925_AM.pdf?1425994768 75 Borjas GJ. 2017. The labor supply of undocumented immigrants. Labour Economics 46:1-13. 76 Meyer BD, Sullivan JX. 2012. Identifying the Disadvantaged: Official Poverty, Consumption Poverty, and the New Supplemental Poverty Measure. Journal of Economic Perspectives 26(3): 111-36; Meyer BD, Mittag N. 2015. Using Linked Survey and Administrative Data to Better Measure income: Implications for Poverty, Program Effectiveness and Holds in the Safety Net. NBER working paper 21676. http://www.nber.org/papers/w21676 77 For further discussion of HIPM limitations, see Korenman SD, Remler DK. 2016. Including health insurance in poverty measurement: The impact of Massachusetts health reform on poverty. Journal of Health Economics 50: 27-35; Remler DK, Korenman SD, Hyson RT. 2017. Estimating the Effects of Health Insurance and Other Social Programs on Poverty Under the Affordable Care Act. Health Affairs 36(10): 1828-1837. 78 https://medium.com/@consensusgroup2018/the-health-care-choices-proposal-policy-recommendations-to-congress-a4660182d830 79 Porter, E. 2012. Health Care as Income for the Poor. New York Times. Oct. 2. https://www.nytimes.com/2012/10/03/business/debating-real-value-of-health-benefits-in-poverty-calculations.html 80 For the US, for a single parent with two children, the HIPM threshold is one third larger than the SPM threshold. For a two-parent, two-child family, the difference is 40%.

42
81 Community Health Care Association of New York State. 2018. Federally Qualified Health Centers New York State Fact Sheet. http://www.chcanys.org/clientuploads/2018%20PDFs/Policy/Facts2018.pdf