The efficacy of the VACO®Diaped+ diabetic foot system in ... internationali con Vacodiaped.pdf ·...
Transcript of The efficacy of the VACO®Diaped+ diabetic foot system in ... internationali con Vacodiaped.pdf ·...

The efficacy of the VACO®Diaped+ diabetic foot system in reducing plantar forefoot pressures in diabetic neuropathic patients
Summary
S.A. Bus1,2, R. Waaijman1, M. Arts1, H. Manning2
1Department of Rehabilitation, Academic Medical Center Amsterdam, 2Diabetic Foot Unit, Twenteborg Ziekenhuis Almelo
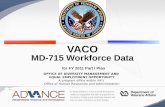
Plantar foot ulcers are a significant burden in patients with diabetes mellitus which may lead to infection and eventually amputation if not adequately treated. The VACO®Diaped+ system is specifically designed as treatment option for offloading plantar diabetic foot ulcers. The system comprises a vacuum cushion, which can be remodeled instantly to accommodate for structural deformity of the patients’ foot, a dampening insole and a roller bottom outsole configuration with the goal to reduce plantar forefoot pressures. However, little is known about the biomechanical efficacy of this device. The purpose of this study was therefore to determine the pressure-relieving effect of the VACO®Diaped+ system in the plantar forefoot of diabetic neuropathic patients in comparison with a forefoot offloading shoe and a control shoe condition. Fifteen diabetic neuropathic subjects (14 male, 1 female) at high risk for plantar ulceration (neuropathy and foot deformity) were included and underwent in-shoe dynamic plantar pressure assessment in five different footwear conditions: VACO®Diaped+ system with custom molded vacuum insole and a roller outsole (RollMold), VACO®Diaped+ system with custom molded vacuum insole and a flat outsole (FlatMold), VACO®Diaped+ system with flat vacuum insole and a roller outsole (RollFlat), Forefoot Offloading Shoe (FOS, Rattenhuber Talus), and Pulman control shoe (Control). The RollMold condition was the standard VACO®Diaped+ condition. The other two were tested to assess the specific effects of (1) outsole configuration (RollMold vs. FlatMold) and (2) custom molding of the vacuum insole (RollMold vs. RollFlat). After initial assessment of comfortable walking speed in the RollMold condition, walking speed was standardized between footwear conditions. All test shoes were worn on the right foot, and the patients’ own shoe on the left foot. Peak pressures, pressure-time integrals (PTI), and force-time integrals (FTI) were calculated from the pressure readings for 6 different foot regions: heel, midfoot, first metatarsal head, 2nd-5th metatarsal heads, hallux and lateral toes. Additionally, perceived comfort of walking was compared between footwear conditions using a 0 to 10 point VAS score. Forefoot peak pressures and PTIs were significantly lower in all four footwear intervention conditions when compared with the control shoe (see Figure, P<0.05)). The FOS condition
©2007 All rights reserved. No part of this document may be reproduced in any form or by any means without permission in writing from the first author mentioned.

showed the lowest 2nd to 5th metatarsal head peak pressures, with significant differences compared with the VACO®Diaped+ conditions. No significant differences between the FOS and the VACO®Diaped+ conditions were found at the first metatarsal head, hallux and toes. PTIs and FTIs were not significantly different between FOS and VACO®Diaped+ conditions in any of the six foot regions. Pressure results between each of the three VACO®Diaped+ conditions were very similar with no significant differences found. Perceived comfort of walking was lowest in the FOS (score 3.4) and highest in the FlatMold condition (7.4). The molded VACO®Diaped+ conditions (RollMold and FlatMold) scored significantly higher for perceived comfort than the FOS. The data showed that the VACO®Diaped+ system offloads the forefoot of at-risk patients better than a control shoe and is comparable to the FOS at the medial forefoot and toe regions. Characteristic features of the VACO®Diaped+, such as the instant vacuum cushion and roller outsole did not prove beneficial in pressure reduction. Patients perceive the VACO®Diaped+ as more comfortable to walk in compared with the FOS. In conclusion, the pressure results in combination with the findings on perceived comfort of walking makes the VACO®Diaped+ system a useful alternative option for the FOS for offloading the plantar forefoot in diabetic patients. Clinical studies will have to prove if the VACO®Diaped+ system is effective in healing plantar diabetic forefoot ulcers.
216 23
0
230
221
322
138
143 15
0
123
107
183 19
9
171
145
330
190 20
7
191
140
344
133
126 14
9
176
235
163 17
2
165
161
274
0
50
100
150
200
250
300
350
400
450
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Rol
lMol
d
Flat
Mol
d
Rol
lFla
t
FOS
Con
trol
Heel Midfoot MTH1 MTH2-5 Hallux Toes2-5
Peak
pre
ssur
e (k
Pa)
$
$
$$
#
Figure. Peak pressures shown per region and per condition for the right foot (study foot). Data areshown as mean values in kPa with 1 standard deviation error bars. Brackets denote significant differences (P<0.05), $: significantly different compared to all other conditions, #: significantlydifferent compared to all VACO®Diaped+ conditions. ©2007 All rights reserved. No part of this document may be reproduced in any form or by any means without permission in writing from the first author mentioned.

Clinical Biomechanics xxx (2009) xxx–xxx
ARTICLE IN PRESS
Contents lists available at ScienceDirect
Clinical Biomechanics
journal homepage: www.elsevier .com/locate /c l inbiomech
The efficacy of a removable vacuum-cushioned cast replacement systemin reducing plantar forefoot pressures in diabetic patients
S.A. Bus a,b,*, R. Waaijman a, M. Arts a, H. Manning b
a Department of Rehabilitation, Academic Medical Center, University of Amsterdam, P.O. Box 22700, Room A01-419, 1100 DE Amsterdam, The Netherlandsb Diabetic Foot Unit, Department of Surgery, Twenteborg Ziekenhuis, Almelo, The Netherlands
a r t i c l e i n f o
Article history:Received 9 July 2008Accepted 13 February 2009Available online xxxx
Keywords:Diabetic footOffloadingPlantar pressureFootwearVacuum device
0268-0033/$ - see front matter � 2009 Elsevier Ltd. Adoi:10.1016/j.clinbiomech.2009.02.004
* Corresponding author. Address: Department of Reical Center, University of Amsterdam, P.O. Box 2270Amsterdam, The Netherlands.
E-mail address: [email protected] (S.A. Bus).
Please cite this article in press as: Bus, S.A., etpressures in diabetic patients. J. Clin. Biomech.
a b s t r a c t
Background: The purpose of this study was to determine the plantar forefoot offloading efficacy of a newprefabricated vacuum-cushioned cast replacement system designed for foot ulcer treatment in neuro-pathic diabetic patients.Methods: Fifteen diabetic subjects with peripheral neuropathy underwent in-shoe plantar pressureassessment while walking in five different footwear types: a standard vacuum-cushioned system withinstantly moldable vacuum cushion and roller outsole, two modified vacuum-cushioned systems, onewith flat surface vacuum cushion and one with flat outsole, a forefoot offloading shoe, and a control shoe.Regional peak pressures, pressure–time integrals, and inter-regional load transfers were calculated todetermine the mechanical action of the footwear. Perceived walking comfort was tested using a 10-pointvisual analogue scale.Findings: Forefoot peak pressures and pressure–time integrals were significantly lower (by 41–56%) inthe vacuum-cushioned system compared to control. Compared to the forefoot offloading shoe, the vac-uum-cushioned system showed significantly higher metatarsal head peak pressures, similar metatarsalhead pressure–time integrals, and significantly lower hallux peak pressures and pressure–time integrals.A major transfer of forefoot load to the midfoot explained the offloading efficacy of the vacuum-cush-ioned system. Few significant differences were present between the modified and standard vacuum-cushioned systems. Perceived walking comfort was significantly higher in the vacuum-cushioned system(score 6.6) than in the forefoot offloading shoe (score 3.4).Interpretation: The results showed that the vacuum-cushioned cast replacement system was effective inoffloading the plantar forefoot of diabetic patients at risk for ulceration, although the contribution of theinstantly moldable vacuum cushion and roller outsole were relatively small. The combined peak pressure,pressure–time integral and walking comfort results indicate that the vacuum-cushioned system may be auseful alternative for the forefoot offloading shoe in offloading the plantar diabetic forefoot.
� 2009 Elsevier Ltd. All rights reserved.
1. Introduction
Foot ulcers are a significant burden in patients with diabetesmellitus. These ulcers may lead to infection and eventually ampu-tation if not adequately treated (Boulton et al., 2004). Excessivemechanical pressure on the foot causing trauma which is not rec-ognized by the patient due to loss of protective sensation is a majorrisk factor for the development of foot ulcers, in particular on theplantar surface (Veves et al., 1992). Reducing these excessive pres-sures (named ‘offloading’) is the most important component oftreatment of these neuropathic plantar foot ulcers. Different de-vices are used for this purpose in clinical practice. The total contact
ll rights reserved.
habilitation, Academic Med-0, Room A01-419, 1100 DE
al. The efficacy of a removable(2009), doi:10.1016/j.clinbiome
cast (TCC) is the best described offloading modality and has provento be highly effective in reducing plantar foot pressures (Baumhau-er et al., 1997; Beuker et al., 2005; Lavery et al., 1996) and in heal-ing neuropathic plantar foot ulcers (Armstrong et al., 2001).However, the use of the TCC requires trained casting personneland sufficient time for application and re-application of the cast.Furthermore, complications may occur with the use of the TCCand patient acceptance is not always high. For these reasons, theuse of the TCC for ulcer treatment is limited in many centers asdata from a recent US survey shows (Wu et al., 2008).
As alternatives for casting, prefabricated devices are commonlyused in clinical practice. These devices include below-the-kneesystems such as removable walking braces and ankle-high devicessuch as half shoes and forefoot offloading shoes. All these deviceshave been shown to be effective in reducing plantar foot pressures(Beuker et al., 2005; Bus et al., 2009; Fleischli et al., 1997; Laveryet al., 1996), and many have also been shown to be effective in
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

2 S.A. Bus et al. / Clinical Biomechanics xxx (2009) xxx–xxx
ARTICLE IN PRESS
healing plantar diabetic foot ulcers (Armstrong et al., 2005;Chantelau et al., 1993; Katz et al., 2005). The data from these stud-ies also show that ankle-high devices do not reduce pressure to thesame level as below-the-knee devices but have the advantage thatthey are lighter in weight and do not immobilize the ankle joint,which facilitates walking, prevents muscle atrophy with long termuse, and improves patient acceptance.
A new prefabricated ankle-high vacuum-cushioned castreplacement system (VCRS) has been designed for treatment ofplantar forefoot ulcers in diabetic patients. This system comprisesa vacuum cushion (bean bag) in conjunction with a roller walkingsole. The vacuum cushion can be remodeled instantly to accommo-date for structural abnormalities or changes in the shape of the pa-tients’ foot. Furthermore, the system features a lightweight stablelattice frame structure in which the foot and lower leg are placedto provide stability. The VCRS is a removable device which canbe reapplied instantly for wound control purposes and it requiresonly limited instruction to apply. Currently, no scientific evidenceexists for the efficacy of the VCRS in reducing pressures under-neath the forefoot in diabetic patients. Therefore, the purpose ofthis study was to assess the plantar forefoot offloading efficacy ofthe VCRS in neuropathic diabetic patients at risk for plantar ulcer-ation and compare this with a forefoot offloading shoe (FOS) and acontrol shoe condition. Furthermore, we aimed to assess the spe-cific contribution of the instantly moldable vacuum cushion andthe roller outsole of the VCRS in offloading the forefoot as well asperceived walking comfort using this system. We hypothesizedthat the VCRS would be more effective than the control shoe andsimilarly effective as the FOS in reducing plantar forefoot pressuresin diabetic patients. Furthermore, we anticipated a significant con-tribution of the custom molded vacuum cushion and roller outsolein the forefoot offloading effect of the VCRS together with a higherwalking comfort in the VCRS than in the FOS.
2. Methods
2.1. Study design
This study was conducted using a repeated measures study de-sign in which five different footwear conditions were tested in eachpatient during one single test session.
Fig. 1. (A) The components of the VCRS, including a vacuum cushion filled with small pldual density cushioning insole, a detachable roller walking sole, and a small vacuum pmolded vacuum cushion (RollMold), (C) VCRS with flat outsole and custom molded vacuu(RollFlat), (E) Pulman control shoe and (F) Rattenhuber Talus forefoot offloading shoe.
Please cite this article in press as: Bus, S.A., et al. The efficacy of a removablepressures in diabetic patients. J. Clin. Biomech. (2009), doi:10.1016/j.clinbiome
2.2. Subjects
Fifteen diabetic patients at high risk for developing plantar footulcers were recruited from our outpatient diabetic foot clinic andparticipated in this study. All patients had loss of protective sensa-tion due to peripheral neuropathy as confirmed by the inability tosense a 10 g monofilament on the plantar hallux, first metatarsalhead, or fifth metatarsal head (Apelqvist et al., 2008) or a vibrationperception threshold above 25 V measured at the dorsal halluxusing a Bio-thesiometer (Bio-Medical Instrument Company, New-bury, OH, USA) (Pham et al., 2000). All patients had one or morefoot deformities, including claw/hammer toe deformity, hallux val-gus, hallux rigidus, prominent metatarsal heads, pes cavus, or pesplanus. Patients with a current foot ulcer, midfoot Charcot neuro-osteoarthopathy, equines deformity, lower extremity amputationsor the inability to walk unaided were excluded from the study. Allpatients gave their written informed consent prior to the study,which was approved by the medical ethics committee of the Uni-versity of Amsterdam Medical Center.
2.3. Footwear
Five different footwear conditions were tested in this study,including three VCRS conditions (VACO�Diaped Plus, OPED, Valley,Germany, www.oped.de), a forefoot offloading shoe (FOS) and acontrol shoe (Fig. 1). Besides the standard VCRS condition, twomodified VCRS conditions were tested to assess the biomechanicalefficacy of the roller walking sole and to test the efficacy of the in-stant custom molding of the vacuum cushion. In the standard VCRScondition, the vacuum cushion was custom molded and a rolleroutsole was attached to the system (RollMold). In the first modifiedVCRS condition, the vacuum cushion was custom molded and a flatoutsole was attached to the system (FlatMold). In the second mod-ified VCRS condition, a flat surface vacuum cushion was createdand a roller outsole was attached to the system (RollFlat).
Custom molding of the vacuum cushion in the RollMold andFlatMold conditions was achieved by manually shaping the airfilled bean bag into a flat cushion, then inserting the cushion intothe system, subsequently having the patient walk a few stepswhile wearing the system, and finally drawing the air out of thecushion with a vacuum pump to fixate the instantly customized
astic balls which is inserted into a soft cover, a lightweight lattice frame structure, aump to extract the air from the cushion, (B) VCRS with roller outsole and customm cushion (FlatMold), (D) VCRS with roller outsole and flat surface vacuum cushion
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

S.A. Bus et al. / Clinical Biomechanics xxx (2009) xxx–xxx 3
ARTICLE IN PRESS
cushion. For the RollFlat condition, the air was drawn from thecushion directly after manually shaping the cushion into a flat sur-face providing a rigid non-customized vacuum device. For each pa-tient a new VCRS was used. The VCRS was available in two sizes:standard and small. All but one subject used the standard sizedevice.
A FOS was used as comparison condition because the FOS is alsoan ankle-high device, which is frequently used in clinical practiceas treatment modality for plantar diabetic foot ulcers. Further-more, the FOS shows good efficacy in relieving forefoot pressuresin the diabetic foot (Bus et al., 2009; Fleischli et al., 1997). TheFOS (Rattenhuber Talus II, www.rattenhuber.de) consisted of arocker-bottom negative heel outsole configuration. A 13-mm dualdensity flat inlay was placed inside the FOS. The control shoe was aPulman shoe (www.fld.fr) with flexible outsole and flat insole.
Each test shoe was worn on the right foot without socks, whilethe patients’ own footwear was worn on the left foot in each of thefive footwear conditions. This footwear consisted mostly of cus-tom-made orthopedic footwear.
2.4. Procedures
At the start of the test session, data on health history, neuro-pathic status, and foot deformities were recorded. Table 1 providesa summary of baseline patient characteristics. After this baselineassessment, each of the five different footwear conditions wastested in a random order with the patient repeatedly walking alonga 12 m walkway in the gait laboratory. Walking speed was mea-sured using photocells positioned at a 6 m distance from eachother halfway along the walkway (Tag-Heuer, Switzerland). Eachpatient was tested at a self-chosen walking speed which was deter-mined prior to each measurement session in the RollMold VCRScondition by averaging the speed from three walking trials. Walk-ing speed was then standardized between walking trials withineach footwear condition (maximum variation 10%) and betweenfootwear conditions (maximum mean difference 5%). Before theactual pressure measurements in each device took place, patientswalked several times across the laboratory to become accustomedto wearing the device.
In-shoe dynamic plantar foot pressures were recorded using thePedar-X system (Novel, Munich, Germany). The Pedar system com-prises a matrix of 99 sensors in 2-mm thick capacitance based flex-ible insoles which were placed between the foot and the insoles ofthe shoe and sampled at 50 Hz. The Pedar insoles were available in
Table 1Baseline patient characteristics. Data are expressed as mean (SD) or as number (N).Data for vibration perception threshold and foot deformity are shown for the rightfoot (=study foot).
Variable Mean (SD) or N Range
Number of subjects 15Age (yrs) 58.9 (7.9) 39–74Height (cm) 178.4 (7.5) 169–199Body mass (kg) 100.8 (25.4) 62–155Body mass index (kg/m2) 31.4 (6.4) 20.7–39.5Male/Female 14/1Diabetes duration (yrs) 21.0 (14.3) 6.5–41.0DM type 1/2 6/9Vibration perception threshold (V) 39.1 (12.1) 10–50 (=max.)
Foot deformity:Claw/hammer toes 5Hallux valgus 2Halllux rigidus 3Prominent metatarsal heads 6Pes cavus 5Pes planus 4
Shoe size (European) 42.9 (2.0) 39–47
Please cite this article in press as: Bus, S.A., et al. The efficacy of a removablepressures in diabetic patients. J. Clin. Biomech. (2009), doi:10.1016/j.clinbiome
five different sizes to accommodate different foot sizes of thetested patients. A minimum of 20 midgait steps per foot were col-lected in four walking trials. Directly after testing each footwearcondition patients scored their perceived walking comfort bydrawing a vertical line on a 10 cm visual analogue scale (VAS),where the far left of the scale denoted ‘lowest possible comfort’and the far right ‘highest possible comfort’.
2.5. Data analysis
In-shoe pressure data was analyzed with Novel software. Peakpressure pictures of both feet were divided by an automated mask-ing procedure into six anatomical regions: heel, midfoot, firstmetatarsal head, second-to-fifth metatarsal heads, hallux and les-ser toes. For each region, the peak pressure, pressure–time integral,force–time integral (synonymous for force impulse or load), con-tact time, and average peak pressure were calculated. The lasttwo parameters were only calculated to explain potential differ-ences between peak pressure and pressure–time integral resultsat specific regions. The force–time integral data was used to defineload transfer diagrams with which the mechanisms of action of theintervention footwear with respect to the control shoe could bedetermined. These load transfer diagrams were slightly adaptedfrom previously reported diagrams (Bus et al., 2004). For this pur-pose, the regional force impulses in the VCRS and FOS conditionswere normalized to the total force impulse in the control shoe con-dition. Based on the regional load differences between the offload-ing and control footwear, load transfer was then calculated fromregions where load was reduced to regions where load was in-creased by means of the offloading footwear. Load transfer calcula-tion started with the toe regions and ended with the heel region.The VAS score for perceived walking comfort was determined bymeasuring the distance from the far left of the scale to the verticalline drawn by the patient using a ruler.
All pressure, walking speed, and comfort data were statisticallyanalyzed using repeated measures analysis of variance (ANOVA).Bonferroni post-hoc analysis, including Bonferroni corrected confi-dence intervals, was used for multiple pairwise comparisons be-tween the different footwear conditions. Separate analyses wereconducted for comparing the standard VCRS with the FOS and con-trol shoe (primary comparison) and for comparing the two modi-fied VCRS conditions (FlatMold and RollFlat) with the standardVCRS condition (RollMold) (secondary comparison). This separa-tion was done to increase focus and to avoid comparisons betweenconditions that we did not consider relevant and would only in-crease the number of pairwise comparisons and the risk for a type1 error. For both analyses, three footwear conditions were chosenfor the within-subject variable factor. A P < 0.05 was consideredstatistically significant in all analyses. For all statistical analysesSPSS version 14.0 (SPSS Inc., Illinois, Chicago, USA) was used.
3. Results
Walking speed varied marginally between footwear conditionsand no significant differences were present. The results for walkingspeed, peak pressure, pressure–time integral, and perceived walk-ing comfort are summarized in Table 2.
Peak pressures were significantly lower in both VCRS and FOSconditions when compared with the control shoe in each of thesix foot regions, except the midfoot, with the largest pressurereductions found at the metatarsal heads: 45–59%. At the midfoot,peak pressure was lowest in the control shoe, which was signifi-cantly different compared to the VCRS. At the metatarsal heads,peak pressures were significantly lower in the FOS condition thanin the VCRS with a 21% difference measured at the first metatarsal
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

Fig. 2. Load transfer diagrams showing the mean regional differences and inter-regional load transfer in normalized FTI values between (A) the VCRS (RollMold)and the control shoe and (B) between the FOS and the control shoe. The breadth ofeach arrow is proportional to the absolute amount of load transfer MTH: metatarsalhead.
Table 2Results for walking speed, peak pressure, pressure–time integral, and perceived walking comfort. Pressure results are shown for the right foot (=study foot).
Variable Footwear condition
Control shoe FOS VCRS (RollMold) VCRS (FlatMold) VCRS (RollFlat)
Mean (SD) Mean (SD) %e Mean (SD) %e Mean (SD) Mean (SD)
Walking speed (m/s) 1.18 (0.17) 1.16 (0.17) 1.18 (0.18) 1.19 (0.18) 1.17 (0.19)
Peak pressure (kPa)Heel 322 (107)b,c 221 (46)a �31 216 (40)a �33 233 (45) 230 (35)Midfoot 107 (41)c 123 (24) +15 138 (36)a +29 141 (39) 150 (41)Metatarsal head 1 330 (71)b,c 145 (23)a,c �56 183 (39)a,b,d �45 200 (43)c 171 (42)Metatarsal head 2–5 344 (75)b,c 140 (19)a,c �59 190 (35)a,b,d �45 210 (40)c 191 (45)Hallux 235 (107)b,c 176 (72)a,c �25 133 (59)a,b �43 125 (61) 149 (66)Lesser toes 274 (82)b,c 161 (45)a �41 163 (54)a �41 174 (55) 165 (48)
Pressure–time integral (kPa s)Heel 86.6 (22.8)c 72.0 (19.1) �17 69.8 (11.5)a �19 70.2 (17.9) 84.3 (41.8)Midfoot 42.5 (23.5) 60.5 (17.8) +42 68.1 (27.7) +60 67.8 (25.4) 75.3 (30.5)Metatarsal head 1 110.3 (38.1)b,c 60.8 (14.0)a �45 56.0 (16.7)a �49 59.2 (15.2) 54.0 (14.8)Metatarsal head 2–5 119.9 (35.8)b,c 62.2 (12.0)a,c �48 62.7 (14.6)a,b,d �48 67.5 (15.4)c 67.6 (17.8)Hallux 51.3 (25.7)b,c 32.4 (16.6)a �37 22.5 (13.2)a �56 21.9 (12.3) 24.2 (13.5)Lesser toes 84.5 (26.3)b,c 47.7 (9.7)a �44 38.2 (15.5)a �55 42.8 (15.4) 38.5 (14.6)
Perceived walking comfort (VAS) 5.5 (2.0)b 3.4 (2.5)a,c 6.6 (1.6)b 7.4 (1.7) 5.2 (2.2)
a Significantly different to control shoe at P < 0.05.b Significantly different to FOS P < 0.05.c Significantly different to VCRS (RollMold) at P < 0.05.d Significantly different to VCRS (FlatMold) at P < 0.05.e Percentage difference compared with control shoe condition.
4 S.A. Bus et al. / Clinical Biomechanics xxx (2009) xxx–xxx
ARTICLE IN PRESS
head and a 26% difference at the second-to-fifth metatarsal heads.In contrast, hallux peak pressure was significantly lower by 24% inthe VCRS than in the FOS. No significant differences in peak pres-sure were found between the VCRS and FOS in the other foot re-gions. When comparing peak pressures between the standardand the modified VCRS conditions, relatively small differenceswere found overall. In the standard VCRS condition (RollMold),peak pressure was significantly lower by 9% at the first metatarsalhead and by 10% at metatarsal head 2–5 when compared with theVCRS condition with flat outsole (FlatMold). No other significantdifferences were found.
In all forefoot regions (including toes) pressure–time integralswere significantly lower in the VCRS and FOS conditions whencompared with control shoe. Percentage differences were between45% and 49% for the metatarsal head regions and between 37% and56% for the toe regions. Midfoot pressure–time integral was signif-icantly higher in the VCRS and FOS when compared with the con-trol shoe. In the heel, pressure–time integral was significantlylower in the VCRS than in control. None of the foot regions showedsignificant differences in pressure–time integrals between theVCRS and FOS, except for the hallux in which pressure–time inte-gral was significantly lower in the VCRS by 31%. When comparingthe pressure–time integrals between the standard VCRS and themodified VCRS conditions, the only significant difference foundwas at the metatarsal head 2–5 region with significantly lowerpressure–time integral in the RollMold than in the FlatMold VCRScondition.
Contact time at the first metatarsal head was on average 657 msin the FOS compared with 598 ms in the VCRS. At the second-to-fifth metatarsal heads, contact times were 684 ms and 677 ms inthe FOS and VCRS, respectively. Average peak pressure at the firstmetatarsal head was on average 92.5 kPa in the FOS and 92.8 kPain the VCRS. At metatarsal head 2–5 average peak pressures were90.6 kPa and 92.4 kPa in the FOS and VCRS, respectively.
Inter-regional transfer of load through the action of the offload-ing footwear, calculated using the load transfer diagrams, is shownin Fig. 2 for the standard VCRS and FOS conditions. The largest loadtransfers were present between the metatarsal heads and midfoot.The portion of force impulse present in the forefoot (includingtoes) which was transferred proximally was 53% for the VCRS
Please cite this article in press as: Bus, S.A., et al. The efficacy of a removablepressures in diabetic patients. J. Clin. Biomech. (2009), doi:10.1016/j.clinbiome
(RollMold) and 36% in the FOS. The diagrams also showed a trans-fer of load of �20 N s from the heel to the midfoot.
For the left foot, which was fitted with the patients’ own shoe ineach of the five test conditions, pressure results were comparablebetween VCRS, FOS and control shoe. The only significant differ-
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

S.A. Bus et al. / Clinical Biomechanics xxx (2009) xxx–xxx 5
ARTICLE IN PRESS
ences found were lower peak pressures and pressure–time inte-grals at metatarsal heads 2–5 in the FOS and VCRS when comparedwith the control shoe.
For perceived walking comfort, large variations between thetested footwear conditions were found (Table 2). Both the standardVCRS (VAS score 6.6) and control shoe (VAS score 5.5) scored sig-nificantly higher than the FOS (VAS score 3.4). Between the stan-dard VCRS condition and both modified VCRS conditions, nosignificant differences in VAS scores were found.
4. Discussion
The results of the study show that the VCRS was effective inrelieving forefoot pressures in the neuropathic diabetic patientstested. Between 41% and 56% relief in peak pressure and pres-sure–time integral were found when compared with the controlshoe condition. The VCRS was less effective than the FOS in reduc-ing peak pressure at the metatarsal heads, but more effective inrelieving the hallux region. Furthermore, the results showed thatthe offloading contribution of the instant custom molding was neg-ligible and the contribution of the roller outsole configuration wassmall (maximum 10% difference found between the modified andstandard VCRS conditions). For the left foot, which was fitted withthe patients’ own shoes, no relevant differences were found be-tween the conditions. This shows that pressure transfer effects tothe contralateral foot were not present.
When compared with reported results on other commonly usedoffloading devices, the VCRS was less effective than a TCC (�80%forefoot pressure relief) or removable waking brace (�70% forefootpressure relief) but more effective than a healing sandal or post-operative shoe (�20% pressure relief) (Fleischli et al., 1997). Thedifferences with the TCC and walking braces may be explainedby the fact that in these below-the-knee devices significantamounts of load are carried by the lower leg providing extra pres-sure relief at the foot compared with ankle-high devices such asthe VCRS. The offloading efficacy measured in the VCRS was com-parable to that found in a cast shoe (Beuker et al., 2005), a devicewhich has been reported to be efficacious in healing plantar neuro-pathic forefoot ulcers (Hissink et al., 2000). Whether the pressurereductions found in the VCRS are sufficient to promote healing ofplantar forefoot ulcers in diabetic patients remains to be investi-gated in future clinical studies.
The more effective relief of metatarsal head peak pressure in theFOS compared with the VCRS may be explained by the contributionof the negative heel rocker-bottom outsole configuration of theFOS which shifts weight-bearing proximally during stance and lim-its active dorsiflexion of the toes; the VCRS does not incorporatethese design features. However, when considering the integral ofpeak pressure at the metatarsal heads, the beneficial effect of theFOS in relation to the VCRS was lost. This result is difficult to ex-plain. In general, contact time and average peak pressure are thetwo factors that define the pressure–time integral. The resultsshowed that contact time at the first metatarsal head was 10%longer in the FOS than in the VCRS and that average peak pressurewas not different between conditions. The difference in contacttime may be responsible for leveling the values on pressure–timeintegral between these conditions, despite differences in peakpressure. The longer contact times measured in the FOS may bean effect of the differences in roll-over mechanisms between thesetwo devices. However, at metatarsal head 2–5, a difference be-tween footwear conditions was not present for contact time norfor average peak pressure so that it remains to be identified whatcaused the contrasting results in peak pressure and pressure–timeintegral at this region. The more effective offloading of the hallux inthe VCRS compared with the FOS may be associated with the
Please cite this article in press as: Bus, S.A., et al. The efficacy of a removablepressures in diabetic patients. J. Clin. Biomech. (2009), doi:10.1016/j.clinbiome
observation that several patients walking in the FOS tip the shoeagainst the ground in terminal stance which may have createdsome localized pressure at this region.
The mechanisms of action of the VCRS and the FOS were definedby assessing inter-regional load redistribution in comparison withthe control shoe condition using adapted versions of previously de-fined load transfer diagrams (Bus et al., 2004). These diagramsshowed a substantial transfer of load from the forefoot to the mid-foot, both in the VCRS (53% of total forefoot load) and in the FOS(36%). They also showed a transfer of load from the heel to themidfoot. These results clearly demonstrate that the midfoot isthe primary target location for load redistribution in these offload-ing devices. But despite these high concentrations of load at themidfoot, a concomitantly large increase in peak pressure was notfound, probably because pressures were well distributed over alarge midfoot contact area. These results suggest that pressurescan be safely redistributed to this region of the foot without neces-sarily increasing the risk for ulceration. This principle of action maybe given more consideration in the future designs of offloadingfootwear for the diabetic foot which is not complicated with mid-foot deformity.
Two modified VCRS conditions were tested in order to specifi-cally assess the offloading efficacy of the instant custom moldinginterface and the detachable roller outsole. As the results showed,the instant custom molding of the vacuum cushion did not seem tocontribute to the offloading efficacy of the VCRS, with only smalldifferences in peak pressure and pressure–time integral found be-tween the molded (RollMold) and flat surface (RollFlat) vacuumcushion conditions of the VCRS. This may be related to the fact thatthe instant molding process merely accommodates the foot surface(through total contact) but does not correct it, something that isnormally achieved using a metatarsal pad or bar, or a medial archsupport, which have been shown to be effective pressure-reducingmodalities for the diabetic foot (Bus et al., 2004; Guldemond et al.,2007). The VCRS with roller outsole (RollMold) offloaded the meta-tarsal heads significantly better than the VCRS with flat outsole(FlatMold). Although the differences found were relatively small,this provides support for the use of a roller outsole configurationwhich reduces active dorsiflexion of the toes and, therefore, fore-foot contribution in foot propulsion. However, forefoot offloadingusing the roller outsole may still have been sub-optimal, consider-ing the fact that all participating subjects with European shoe size39–47 (14 out of 15) wore the same size VCRS. This clearly in-creases the variability of the roller pivot point location relative tothe metatarsal heads, which has an optimum location directlyproximal to the heads (van Schie et al., 2000). These results suggestthat improvements in this design of the VCRS are indicated.
Perceived comfort of walking was scored significantly better inthe VCRS (VAS score 6.6) than in the FOS (VAS score 3.4), and alsobetter, although not significantly, in the VCRS than in control shoe(VAS 5.5). The difference found in VAS scores between the VCRSand the FOS are suggested to be due to the fact that the VCRS, un-like the FOS, does not incorporate a negative heel rocker-bottomoutsole configuration, a construction feature patients normallydo not have in their shoes and, hence, may be felt as uneasy to walkin. The low VAS score in the FOS confirms earlier findings on walk-ing comfort in different FOS models (Bus et al., 2009). We wouldsuggest that perceived walking comfort may affect adherence totreatment, which by itself is important for promoting ulcer healingwith removable devices. Therefore, the results suggest that thismay be less of a factor in the VCRS than in the FOS.
In the chosen experimental setup of this study, each subject wasgiven only a brief period (i.e. several walking trials) to becomeaccustomed to wearing each offloading device. This brief habitua-tion period may have prevented the assessment of robust walkingcomfort ratings in the tested footwear. Furthermore, in this study
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

6 S.A. Bus et al. / Clinical Biomechanics xxx (2009) xxx–xxx
ARTICLE IN PRESS
only normal pressures were measured. We acknowledge the po-tential contribution of shear pressures in causing plantar foot ul-cers, and we therefore suggest that such measures should beincorporated in future studies as soon as equipment is capable ofmeasuring these shear pressure components.
5. Conclusions
This study was performed to assess the offloading efficacy,mechanisms of offloading and the perceived walking comfort of anew prefabricated vacuum-cushioned cast replacement system indiabetic patients at risk for plantar foot ulceration. The use of theVCRS resulted in a substantial pressure relief in the forefoot whencompared to a control shoe condition. In comparison with a FOS,the VCRS was less effective in relieving peak pressures at the meta-tarsal heads, similarly effective in reducing pressure–time integralsat these regions, and more effective in relieving peak pressures andpressure–time integrals at the hallux. The mechanism of offloadingwith the VCRS seems the transfer of substantial amounts of loadfrom the forefoot to the midfoot. The exact design features respon-sible for forefoot offloading in the VCRS are difficult to determinebased on the data obtained since the instant custom molding ofthe vacuum cushion did not seem to contribute significantly toforefoot pressure relief. Perceived walking comfort was scored sig-nificantly higher in the VCRS than the FOS, and this result may im-prove adherence to treatment. Based on the combined pressureand comfort results, the VCRS may be a useful alternative for theFOS in offloading the plantar forefoot in diabetic patients. How-ever, whether the VCRS is effective in healing diabetic plantar fore-foot ulcers remains to be investigated in a prospective clinical trial.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the help of Tessa Busch,physiatrist, in recruiting patients for this study. The study wassponsored by OPED GmbH (Valley, Germany) who provided anunrestricted research grant to conduct the study. The sponsor didnot have any involvement in the setup, data collection, analysisor interpretation of the study, the writing of the manuscript, orthe decision to submit the manuscript for publication.
Please cite this article in press as: Bus, S.A., et al. The efficacy of a removablepressures in diabetic patients. J. Clin. Biomech. (2009), doi:10.1016/j.clinbiome
References
Apelqvist, J., Bakker, K., van Houtum, W.H., Schaper, N.C., 2008. Practical guidelineson the management and prevention of the diabetic foot: based upon theInternational Consensus on the Diabetic Foot (2007) prepared by theinternational working group on the Diabetic Foot. Diabetes Metab. Res. Rev.24 (Suppl. 1), S181–S187.
Armstrong, D.G., Lavery, L.A., Wu, S., Boulton, A.J.M., 2005. Evaluation of removableand irremovable cast walkers in the healing of diabetic foot wounds: arandomized controlled trial. Diabetes Care 28, 551–554.
Armstrong, D.G., Nguyen, H.C., Lavery, L.A., Van Schie, C.H.M., Boulton, A.J.M.,Harkless, L.B., 2001. Off-loading the diabetic foot wound: a randomized clinicaltrial. Diabetes Care 24, 1019–1022.
Baumhauer, J.F., Wervey, R., McWilliams, J., Harris, G.F., Shereff, M.J., 1997. Acomparison study of plantar foot pressure in a standardized shoe, total contactcast, and prefabricated pneumatic walking brace. Foot Ankle Int. 18, 26–33.
Beuker, B.J., van Deursen, R.W., Price, P., Manning, E.A., van Baal, J.G., Harding, K.G.,2005. Plantar pressure in off-loading devices used in diabetic ulcer treatment.Wound Repair Regen. 13, 537–542.
Boulton, A.J., Kirsner, R.S., Vileikyte, L., 2004. Clinical practice. Neuropathic diabeticfoot ulcers. New. Engl. J. Med. 351, 48–55.
Bus, S.A., Ulbrecht, J.S., Cavanagh, P.R., 2004. Pressure relief and load redistributionby custom-made insoles in diabetic patients with neuropathy and footdeformity. Clin. Biomech. 19, 629–638.
Bus, S.A., van Deursen, R.W.M., Kanade, R.V., Wissink, M., Manning, E.A., van Baal,J.G., Harding, K.G., 2009. Plantar pressure relief in the diabetic foot usingforefoot offloading shoes. Gait Posture. doi:10.1016/j.gaitpost.2009.01.003.
Chantelau, E., Breuer, U., Leisch, A.C., et al., 1993. Outpatient treatment of unilateraldiabetic foot ulcers with ‘half shoes’. Diabetic Med. 10, 267–270.
Fleischli, J.G., Lavery, L.A., Vela, S.A., Ashry, H., Lavery, D.C., 1997. Comparison ofstrategies for reducing pressure at the site of neuropathic ulcers. J. Am. Podiatr.Med. Assoc. 87, 466–472.
Guldemond, N.A., Leffers, P., Schaper, N.C., Sanders, A.P., Nieman, F., Willems, P.,Walenkamp, G.H., 2007. The effects of insole configurations on forefoot plantarpressure and walking convenience in diabetic patients with neuropathic feet.Clin. Biomech. 22, 81–87.
Hissink, R.J., Manning, H.A., van Baal, J.G., 2000. The MABAL shoe, an alternativemethod in contact casting for the treatment of neuropathic diabetic foot ulcers.Foot Ankle Int. 21, 320–323.
Katz, I.A., Harlan, A., Miranda-Palma, B., Prieto-Sanchez, L., Armstrong, D.G., Bowker,J.H., Mizel, M.S., Boulton, A.J., 2005. A randomized trial of two irremovable off-loading devices in the management of plantar neuropathic diabetic foot ulcers.Diabetes Care 28, 555–559.
Lavery, L.A., Vela, S.A., Lavery, D.C., Quebedeaux, T.L., 1996. Reducing dynamic footpressures in high-risk diabetic subjects with foot ulcerations. A comparison oftreatments. Diabetes Care 19, 818–821.
Pham, H., Armstrong, D.G., Harvey, C., Harkless, L.B., Giurini, J.M., Veves, A., 2000.Screening techniques to identify people at high risk for diabetic foot ulceration:a prospective multicenter trial. Diabetes Care 23, 606–611.
van Schie, C., Ulbrecht, J.S., Becker, M.B., Cavanagh, P.R., 2000. Design criteria forrigid rocker shoes. Foot Ankle Int. 21, 833–844.
Veves, A., Murray, H.J., Young, M.J., Boulton, A.J., 1992. The risk of foot ulceration indiabetic patients with high foot pressure: a prospective study. Diabetologia 35,660–663.
Wu, S.C., Jensen, J.L., Weber, A.K., Robinson, D.E., Armstrong, D.G., 2008. Use ofpressure offloading devices in diabetic foot ulcers: do we practice what wepreach? Diabetes Care 31, 2118–2119.
vacuum-cushioned cast replacement system in reducing plantar forefootch.2009.02.004

Gait & Posture xxx (2009) xxx–xxx
G Model
GAIPOS-2741; No of Pages 5
Vacuum cushioned removable cast walkers reduce foot loading in patientswith diabetes mellitus
Arne Nagel a,b, Dieter Rosenbaum a,*a Movement Analysis Lab, Orthopaedic Department, University Hospital Munster, Germanyb Motion Analysis Lab Walstedde – Centre for Motion Analysis and Therapy, Drensteinfurt-Walstedde, Germany
A R T I C L E I N F O
Article history:
Received 12 June 2008
Received in revised form 7 February 2009
Accepted 15 February 2009
Keywords:
Diabetes mellitus
Vacuum orthoses
Foot loading
Plantar pressure
Biomechanics
A B S T R A C T
Background: Diabetes mellitus is one of the most common diseases worldwide and the number of
patients is expected to increase dramatically in future. Plantar ulceration is partly caused by high plantar
pressures and a major complication in diabetic patients.
Purpose: The aim of this study was to investigate the pressure-relieving effects of two vacuum orthoses
in patients with diabetes mellitus.
Methods: Twenty patients with diabetes mellitus were included. They presented with plantar callosities
but no ulceration. Exclusion criteria included the use of walking aids and other systemic diseases. Plantar
pressure distribution was measured with sensor insoles (Pedar-X, Novel GmbH) during walking in two
vacuum orthoses, a post-operative shoe and an off-the-shelf shoe as reference condition. Statistical
analysis was conducted using Friedman and Wilcoxon signed-rank tests.
Results: Significant differences in plantar pressure distribution were found between the four walking
conditions. The contact area increased in the midfoot with the vacuum orthoses. Maximum force and
peak pressures showed a significant decrease under the rearfoot and forefoot and increased in the
midfoot area during walking with both vacuum orthoses. The high-cut vacuum orthosis revealed equal
pressure relief under the forefoot and significantly lower rearfoot pressures compared to the post-
operative shoe.
Conclusions: The vacuum orthoses demonstrated a comparable pressure-relieving efficacy under the
forefoot to post-operative shoes. Using vacuum orthosis significantly benefited re-distribution of plantar
pressure and the roll-over process. Clinical significance of the pressure-relieving efficacy could not be
confirmed in this investigation and has to be addressed in further studies.
� 2009 Elsevier B.V. All rights reserved.
Contents lists available at ScienceDirect
Gait & Posture
journa l homepage: www.e lsev ier .com/ locate /ga i tpost
1. Introduction
Diabetes mellitus is one of the most frequent diseases world-wide. More than 180 million patients suffer from diabetesaccording to data from the World Health Organization (WHO;http://www.who.int/mediacentre/factsheets). Furthermore, theWHO anticipates that the number of diabetic patients will morethan double by 2030. Diabetic neuropathy damages the nerves ofalmost 50% of diabetic patients and is a major cause for the diabeticfoot syndrome that leads to high morbidity, reduced quality of lifeand high health-care costs [1,2]. Foot ulceration is a majorcomplication in patients with diabetes mellitus [3] and 15–25% ofdiabetic patients develop foot ulcers during their lifetime [4–6].
* Corresponding author at: Movement Analysis Lab, Orthopaedic Department,
University Hospital Munster, Domagkstr. 3, D-48151 Munster, Germany.
Tel.: +49 251 835 2970; fax: +49 251 835 2993.
E-mail address: [email protected] (D. Rosenbaum).
Please cite this article in press as: Nagel A, Rosenbaum D. Vacuum cwith diabetes mellitus. Gait Posture (2009), doi:10.1016/j.gaitpost.2
0966-6362/$ – see front matter � 2009 Elsevier B.V. All rights reserved.
doi:10.1016/j.gaitpost.2009.02.007
High plantar pressures during the roll-over process combined withperipheral neuropathy are believed to increase the risk for plantarulceration [7]. An association between neuropathy and highplantar pressures has been reported [8,9]. Therefore, reducingpressure from the region of diabetic foot ulcers is a major part ofthe ulcer prevention management [5].
In diabetic patients, a redistribution of plantar pressure, whichprevents high local pressures has been achieved with custom-madeorthotic insoles [10–12]. A load transfer from the highly loadedforefoot to the midfoot region was demonstrated [13]. The risk offoot ulcers and re-ulceration is suggested to be minimized bywearing appropriate off-the-shelf or custom-made footwear [4]. Incases of acute foot ulcers, total contact casts are suggested as thegold standard to relieve plantar pressure from the ulcers [14].Furthermore, post-operative shoes are widely used to reduceplantar pressure in the forefoot region in case of acute ulcers.Originally designed to offload the toes and forefoot after surgery,post-operative shoes came into use as a simple and cost-effectivedevice in diabetic patients with foot ulceration. Another alternative
ushioned removable cast walkers reduce foot loading in patients009.02.007

A. Nagel, D. Rosenbaum / Gait & Posture xxx (2009) xxx–xxx2
G Model
GAIPOS-2741; No of Pages 5
to reduce high local pressures is the removable cast walker. Thisdevice is claimed to provide similar pressure relief to total contactcasts. Removable cast walkers can be removed and reapplieddirectly and therefore allow wound control, adaptation to foot/wound status and improved hygiene of the patient. In some studiestotal contact casting demonstrated shorter healing times for footulcers in comparison to removable cast walkers and therapeuticfootwear [15,16]. However, reviews of studies concerning woundhealing in diabetes patients provided little evidence for greaterefficacy of total contact casts in wound healing in comparison toother offloading techniques [14,17].
The aim of this study was to investigate the effects of com-mercially available cast walkers with vacuum cushioning todecrease plantar foot loading in patients with diabetes. Wemeasured plantar pressure distribution during walking in a standardshoe, a post-operative shoe and in two designs of vacuum orthoses todetect changes in foot loading. The vacuum orthoses provideindividual support by adapting the insole to the foot shape based ona vacuum cushion in combination with a dampening insole.
2. Methods
2.1. Subjects
The study included 20 patients (13 females, 7 males) with diabetes mellitus type
I (4) or II (16). The mean age was 56.4 � 15.7 years with a range from 18 to 74 years.
The body mass index varied between 19 and 41 kg/m2 with a mean value of
29 � 6.8 kg/m2. The disease duration was 12.8 � 12.1 years (range: 2–58 years). The
patients’ feet had plantar callosities but no ulcerations. Exclusion criteria were the use
of walking aids and other systemic diseases, such as rheumatoid arthritis or
Parkinson’s disease. All patients gave informed consent to participate in the study.
2.2. Shoes and vacuum orthoses
The vacuum orthoses (Oped GmbH, Valley, Germany) are removable cast walkers
using vacuum pads in conjunction with a cushioning dual-density insole and a
rocker bottom sole (Fig. 1c and d). The vacuum pads were similar in both orthoses
and consisted of a bag filled with Styrofoam ‘beans’ of about 1 mm of diameter.
These pads conform to the individual shape of the plantar surface after walking a
few steps with the orthoses. The individual shape of the bean bag was conserved by
removing the air between the beans thus creating a vacuum. This is meant to
maximize contact area of the foot and reduce high local pressures. The
VACOdiaped1 is a device with a knee-high shaft and includes a rigid frame that
provides strict movement restriction to the ankle joint. The orthosis can be fixed on
the patients’ shank and foot with an additional strap to improve the wearing
compliance. Removal of the strap by the patient can be easily monitored as it would
be observed that the seal is broken at the next clinical examination. The
VACOdiaped-Plus1 contains a short shaft (low-cut design) without a rigid frame.
The DARCO1 Light was the third orthosis used in this study (Fig. 1b). This post-
operative shoe was constructed to unload the whole forefoot region and to allow
load transfer only in the midfoot and rearfoot regions. The subjects wore each
orthosis on the right foot. On the left foot they wore an off-the-shelf shoe to
replicate the usual application situation and ensure comparable conditions for all
subjects. Reference measurements were conducted while wearing a pair of these
off-the-shelf shoes. They were wide in shape and are usually recommended for
people with foot problems (Fig. 1a).
2.3. Pedobarography
The pedobarography measurements were performed in a 25-m corridor. Plantar
pressure distribution was measured with capacitive sensor insoles with 99 sensors
(Pedar-X, sampling rate 50 Hz, Novel GmbH, Munich, Germany). Good reliability
has been previously demonstrated with this method [18,19]. The patients
Fig. 1. Three walking conditions were tested: (a) standard shoe, (b) post-opera
Please cite this article in press as: Nagel A, Rosenbaum D. Vacuum cwith diabetes mellitus. Gait Posture (2009), doi:10.1016/j.gaitpost.2
performed two trials of walking in each condition in a randomized testing order.
They were asked to walk at a comfortable speed. At least 15 steps of each walking
condition were selected for further data analysis. After determining the mean
values of the 15 steps the foot was subdivided with standard software (Database
Pro-M, Novel GmbH, Munich, Germany) in three areas of interest: rearfoot, midfoot
and forefoot. The following parameters were determined: contact area (CA), contact
time (CT), maximum force (MF), force–time integral (FTI), i.e. the product of the
amplitude and duration of force application as the overall effect loading effect in a
region and peak pressure (PP) as the highest local load within the region.
Furthermore, the gait line as an indicator for the roll-over process was analyzed. The
gait line consists of the center of pressure of every recorded frame and is suggested
to reveal information about gait velocity and locomotor capability [20,21].
Gait velocity was controlled with light gates (DLS-LA Timing System, AF Sport,
Wesel, Germany). Velocity was allowed to be different between subjects but had to
stay constant between shoe conditions for each individual.
2.4. Statistical analysis
Statistical analysis was undertaken using SPSS for Windows 13.0 (SPSS Inc.,
Chicago, IL, USA). Non-parametric tests were used after testing for normal
distribution with the Kolmogorow–Smirnov-test. Friedman tests were used to
investigate general differences between walking with orthoses and standard shoes
(p < 0.05). The paired Wilcoxon signed-rank test was then conducted (p < 0.0083
after Bonferroni correction).
3. Results
The results revealed significant differences in the plantarpressure patterns between the four walking conditions (Table 1).No significant differences were found in contact times. Thisconfirmed comparable gait dynamics without significant differ-ences in walking velocity between the four walking conditions.
3.1. Contact area
The contact area of the foot during the roll-over process differedbetween the off-the-shelf shoe and the three orthoses (Fig. 2).Thus, an increase of contact area up to 45.1% (p < 0.006) could beseen in the midfoot in both vacuum orthoses and also for the wholefoot compared to the control condition. The post-operative shoerevealed an increase of 29.1% (p < 0.000) in the midfoot region.Comparing orthoses revealed higher contact areas in the midfootfor the VACOdiaped-Plus1.
3.2. Maximum force and force–time integral
Maximum force and force–time integral revealed significantdifferences in foot loading for the off-the-shelf shoe with respect tothe three orthoses in every foot region. Maximum force wassignificantly reduced in the forefoot during walking with bothvacuum orthoses by 36.8% and 38%, respectively (p < 0.001). Thepost-operative shoe showed a reduction of 44.8% (p < 0.001) in theforefoot region. The orthoses significantly increased the maximumforce in the midfoot region. The VACOdiaped-Plus1 provided themost pronounced effect (+47.6%, p < 0.001). The force–timeintegrals showed a similar effect as the maximum force in thesefoot regions. Under the rearfoot the post-operative shoe revealed adecreased maximum force but an increased force–time integral.The vacuum orthoses showed a decrease of maximum force and
tive shoe, (c) high-cut vacuum-orthosis and (d) low-cut vacuum-orthosis.
ushioned removable cast walkers reduce foot loading in patients009.02.007

Table 1Results of plantar pressure measurements (MW � S.D.) for all subjects (n = 20) and conditions.
Off-the-shelf footwear (OSF) Post-operative shoe (POS) VACOdiaped (high-cut) VACOdiaped-Plus (low-cut)
Contact area [cm2]
Rearfoot(6) 28.4 � 4.5 28.8 � 3.9 27.3 � 5.4 28.3 � 4.9
Midfoot(1,2,3,5) 36.6 � 8.6 47.3 � 9.4 50.6 � 9.1 53.1 � 8.1
Forefoot(5) 68.6 � 9.0 63.4 � 8.6 63.3 � 12.3 66.0 � 13.2
Contact time [ms]
Rearfoot 714.2 � 210.0 724.0 � 118.9 753.5 � 158.6 677.2 � 130.5
Midfoot 731.6 � 192.7 721.5 � 120.1 761.9 � 132.3 723.4 � 122.4
Forefoot 757.9 � 190.2 725.8 � 116.0 755.0 � 118.0 725.2 � 114.3
Force–time integral [N s]
Rearfoot(1,4,5) 142.8 � 38.4 180.4 � 54.4 141.3 � 54.5 131.8 � 42.7
Midfoot(1,2,3,4,5) 101.7 � 65.9 148.7 � 83.3 176.7 � 75.9 195.2 � 83.7
Forefoot(1,2,3) 321.9 � 107.4 198.4 � 66.6 199.5 � 86.6 203.4 � 75.9
Maximum force [N]
Rearfoot(1,2,3,4,5,6) 528.2 � 123.1 458.8 � 126.8 320.9 � 92.9 385.2 � 98.9
Midfoot(1,2,3,5,6) 272.5 � 140.0 314.3 � 140.4 340.3 � 130.3 402.3 � 148.4
Forefoot(1,2,3,5,6) 890.3 � 191.5 491.0 � 117.8 516.8 � 189.0 615.8 � 205.1
Peak pressure [kPa]
Rearfoot(1,2,3,4,5) 306.7 � 67.4 224.4 � 57.1 176.2 � 34.1 194.4 � 38.3
Midfoot(1,2,4,6) 154.0 � 58.8 117.4 � 33.4 121.3 � 28.8 146.8 � 38.5
Forefoot(1,2,3,4,6) 420.5 � 99.3 153.4 � 39.9 160.9 � 50.2 191.8 � 54.2
1Significant difference between the OSF and the POS (p < 0.0083); 2Significant difference between the OSF and the high-cut vacuum orthosis (p < 0.0083); 3Significant
difference between the OSF and the low-cut vacuum orthosis (p < 0.0083); 4Significant difference between the POS and the high-cut vacuum orthosis (p < 0.0083);5Significant difference between the POS and the low-cut vacuum orthosis (p < 0.0083); 6Significant difference between the two vacuum orthosis (p < 0.0083).
A. Nagel, D. Rosenbaum / Gait & Posture xxx (2009) xxx–xxx 3
G Model
GAIPOS-2741; No of Pages 5
minimum change in the force–time integrals in the rearfoot. TheVACOdiaped revealed significantly lower maximum forces in theall foot regions than the VACOdiaped-Plus1.
3.3. Peak pressure
Plantar peak pressures were significantly altered duringwalking with the three orthoses (Figs. 2 and 3). Peak pressureswere elevated under the midfoot whereas a significant decreaseof plantar pressures could be seen under the rearfoot and
Fig. 2. Plantar pressure distribution of a 24-year-old female
Please cite this article in press as: Nagel A, Rosenbaum D. Vacuum cwith diabetes mellitus. Gait Posture (2009), doi:10.1016/j.gaitpost.2
forefoot, i.e. the sites where ulcers predominantly occur. TheVACOdiaped1 and the post-operative shoe revealed similarpressure reduction in the forefoot whereas the rearfoot pressureswere significantly higher while walking in the post-operativeshoe compared to the two vacuum orthoses. The VACOdiaped-Plus1 showed significantly higher peak pressures under theforefoot as compared to the VACOdiaped1 and the post-operative shoe (Figs. 2 and 3). Furthermore, the VACOdiapedrevealed significantly lower peak pressures in the rearfoot regionthan the VACOdiaped-Plus1.
patient during walking with the four-shoe conditions.
ushioned removable cast walkers reduce foot loading in patients009.02.007

Fig. 3. Significant differences in peak pressure between the four walking conditions
(mean + S.D., $ = p < 0.0083).
A. Nagel, D. Rosenbaum / Gait & Posture xxx (2009) xxx–xxx4
G Model
GAIPOS-2741; No of Pages 5
3.4. Gait line
The gait line showed remarkable differences between the fourwalking conditions. The gait line of the off-the-shelf shoe started inthe center of the rearfoot and ended in the distal part of the forefoot(Fig. 4). The vacuum orthoses showed a gait line from the distalpart of the rearfoot to the center of the forefoot. The gait line whilewalking in the post-operative shoe showed a similar starting pointas the off-the-shelf shoe but ended before reaching the center ofthe forefoot.
4. Discussion
The aim of this study was to investigate pressure-relievingeffects of vacuum orthoses in patients with diabetes mellitus. Thevacuum orthoses proved to be as effective in redistributing plantarpressures as cushioning orthotic insoles [10,11]. The same re-distribution pattern could be seen with an increased midfootloading and a pressure relief in the rearfoot and forefoot regions[13].
This more evenly distributed plantar pressure pattern is anadvantage in comparison to the post-operative shoe that showedsignificantly higher peak pressures under the rearfoot whilerevealing the same pressure relief under the forefoot as the high-cut vacuum orthosis. The combination of moulding the plantarsurface and using a rocker bottom sole in the vacuum orthosestherefore lead to a highly efficient pressure relief under the whole
Fig. 4. Gait line of a 24-year-old female patient during the walking conditions: (a) stan
vacuum orthosis.
Please cite this article in press as: Nagel A, Rosenbaum D. Vacuum cwith diabetes mellitus. Gait Posture (2009), doi:10.1016/j.gaitpost.2
foot. The efficacy of midfoot rockers for pressure relief in diabeticpatients has been demonstrated by Drerup et al. [13]. Furthermore,the rigid frame structure of the high-cut vacuum orthosisimmobilized the upper ankle joint. This seemed to provideadditional pressure relief in comparison to the low-cut vacuumorthosis as shown in significantly lower peak pressures andmaximum forces under the forefoot region. In that case the loadmay have partly been carried by the rigid frame structure of thehigh-cut vacuum orthosis. Another explanation could be apronounced load transfer in the midfoot region due to restrictedpush-off efficacy under the forefoot.
The assessment of the roll-over process of the foot using the gaitline revealed remarkable differences between the three orthosis.The two vacuum orthoses indicated a more physiological patternin the push-off phase in comparison to the post-operative shoe.The shortened gait line of the post-operative shoe suggested anearly termination of the roll-over process of the foot whereas thesubjects executed an almost complete roll-over process whilewearing the vacuum orthoses. This could lead to a morecomfortable gait and a better compliance.
The comparison to total contact casts is difficult due to only fewstudies measuring the pressure re-distribution capacity of totalcontact casts. Studies investigating the efficacy of total contactcasts mainly described the healing rate or healing time of footulcers [14,15,22]. However, Armstrong and Stacpoole-Sheareported a significantly better relief of plantar pressure underthe heel in total contact casts compared to removable cast walkers[23]. The efficacy of removable cast walkers in healing rate andhealing time of foot ulceration was improved by fixing them on thepatients’ foot and shank not allowing self-removal of the castwalker [24]. The high-cut vacuum orthosis includes the option tobe used as a non-removable cast walker. Therefore, this orthosismight be equally as effective in wound treatment as total contactcasts.
4.1. Limitations of the study
There was no total contact cast included in this study, althoughit is the gold standard in the treatment of plantar ulcers in diabeticpatients. The aim of this study was to evaluate the pressure-relieving efficacy of the two vacuum orthoses in diabetic patientswithout acute ulcers and therefore it was not possible to apply atotal contact cast to the subjects for a pressure measurement inthis study. Furthermore, the literature review showed that theefficacy of total contact casts is mainly evaluated in clinical studies
dard shoe, (b) post-operative shoe, (c) high-cut vacuum-orthosis and (d) low-cut
ushioned removable cast walkers reduce foot loading in patients009.02.007

A. Nagel, D. Rosenbaum / Gait & Posture xxx (2009) xxx–xxx 5
G Model
GAIPOS-2741; No of Pages 5
concerning healing rates of acute ulcers. The clinical efficacy of thevacuum orthoses has to be proven in clinical trials with the totalcontact cast as competitor.
The study population demonstrated a wide distribution of ageand body weight and this may have influenced their gait. Thestatistical analysis with Wilcoxon signed-rank tests includescomparison of the four conditions within the same person. Thisseems to be the appropriate way to obtain valid results in such aheterogeneous group.
5. Conclusion
In summary, the vacuum orthoses proved to be goodalternatives to typically used post-operative shoes in diabeticpatients. They revealed the same pressure relief in the forefootregion but demonstrated advantages in the re-distribution ofplantar pressure and the roll-over process. Clinical trials includinghealing rates of acute ulcers would have to demonstrate theclinical efficacy of the vacuum orthosis. In these studies the totalcontact cast, which is the gold standard in the treatment of plantarfoot ulcers, would have to be used as the criterion for comparison.
Conflict of interest
The authors state that there is no financial or other conflict ofinterest.
Acknowledgement
The company OPED GmbH (Valley, Germany) provided financialsupport like research funding and representation allowance forthe patients.
References
[1] Goodridge D, Trepman E, Sloan J, Guse L, Strain LA, McIntyre J, et al. Quality oflife of adults with unhealed and healed diabetic foot ulcers. Foot Ankle Int2006;27(4):274–80.
[2] Nabuurs-Franssen MH, Huijberts MS, Nieuwenhuijzen Kruseman AC, WillemsJ, Schaper NC. Health-related quality of life of diabetic foot ulcer patients andtheir caregivers. Diabetologia 2005;48(9):1906–10.
[3] Ribu L, Hanestad BR, Moum T, Birkeland K, Rustoen T. A comparison of thehealth-related quality of life in patients with diabetic foot ulcers, with adiabetes group and a nondiabetes group from the general population. QualLife Res 2006.
Please cite this article in press as: Nagel A, Rosenbaum D. Vacuum cwith diabetes mellitus. Gait Posture (2009), doi:10.1016/j.gaitpost.2
[4] Fard AS, Esmaelzadeh M, Larijani B. Assessment and treatment of diabetic footulcer. Int J Clin Pract 2007;61(11):1931–8.
[5] Rathur HM, Boulton AJ. The neuropathic diabetic foot. Nat Clin Pract Endo-crinol Metab 2007;3(1):14–25.
[6] Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients withdiabetes. JAMA 2005;293(2):217–28.
[7] Veves A, Murray HJ, Young MJ, Boulton AJ. The risk of foot ulceration in diabeticpatients with high foot pressure: a prospective study. Diabetologia1992;35(7):660–3.
[8] Stess RM, Jensen SR, Mirmiran R. The role of dynamic plantar pressures indiabetic foot ulcers. Diabetes Care 1997;20(5):855–8.
[9] Frykberg RG, Lavery LA, Pham H, Harvey C, Harkless L, Veves A. Role ofneuropathy and high foot pressures in diabetic foot ulceration. Diabetes Care1998;21:1714–9.
[10] Albert S, Rinoie C. Effect of custom orthotics on plantar pressure distribution inthe pronated diabetic foot. J Foot Ankle Surg 1994;33(6):598–604.
[11] Bus SA, Ulbrecht JS, Cavanagh PR. Pressure relief and load redistribution bycustom-made insoles in diabetic patients with neuropathy and foot deformity.Clin Biomech (Bristol Avon) 2004;19(6):629–38.
[12] Owings TM, Woerner JL, Frampton JD, Cavanagh PR, Botek G. Custom ther-apeutic insoles based on both foot shape and plantar pressure measurementprovide enhanced pressure relief. Diabetes Care 2008.
[13] Drerup B, Hafkemeyer U, Moller M, Wetz HH. Effect of walking speed on pressuredistribution of orthopedic shoe technology. Orthopade 2001;30(3):169–75.
[14] Gray M. Is total contact casting effective for treating diabetic foot ulcers? JWound Ostomy Continence Nurs 2006;33(4):359–62.
[15] Caravaggi C, Faglia E, De Giglio R, Mantero M, Quarantiello A, Sommariva E,et al. Effectiveness and safety of a nonremovable fiberglass off-bearing castversus a therapeutic shoe in the treatment of neuropathic foot ulcers: arandomized study. Diabetes Care 2000;23(12):1746–51.
[16] Caravaggi C, Sganzaroli A, Fabbi M, Cavaiani P, Pogliaghi I, Ferraresi R, et al.Nonwindowed nonremovable fiberglass off-loading cast versus removablepneumatic cast (AircastXP Diabetic Walker) in the treatment of neuropathicnoninfected plantar ulcers: a randomized prospective trial. Diabetes Care2007;30(10):2577–8.
[17] Spencer S. Pressure relieving interventions for preventing and treating dia-betic foot ulcers. Cochrane Database Syst Rev )2000;(3). CD002302.
[18] Putti AB, Arnold GP, Cochrane L, Abboud RJ. The Pedar in-shoe system:repeatability and normal pressure values. Gait Posture 2007;25(3):401–5.
[19] Barnett S, Cunningham JL, West S. A comparison of vertical force and temporalparameters produced by an in-shoe pressure measuring system and a forceplatform.. Clin Biomech (Bristol Avon) 2001;16(4):353–7.
[20] Nigg B, Hintzen S, Ferber R. Effect of an unstable shoe construction on lowerextremity gait characteristics. Clin Biomech (Bristol Avon) 2006;21(1):82–8.
[21] Mizelle C, Rodgers M, Forrester L. Bilateral foot center of pressure measurespredict hemiparetic gait velocity. Gait Posture 2006;24(3):356–63.
[22] Mueller MJ, Diamond JE, Sinacore DR, Delitto A, Blair 3rd VP, Drury DA, et al.Total contact casting in treatment of diabetic plantar ulcers: controlled clinicaltrial. Diabetes Care 1989;12(6):384–8.
[23] Armstrong DG, Stacpoole-Shea S. Total contact casts and removable castwalkers: mitigation of plantar heel pressure. J Am Podiatr Med Assoc1999;89(1):50–3.
[24] Armstrong DG, Lavery LA, Wu S, Boulton AJ. Evaluation of removable andirremovable cast walkers in the healing of diabetic foot wounds: a randomizedcontrolled trial. Diabetes Care 2005;28(3):551–4.
ushioned removable cast walkers reduce foot loading in patients009.02.007

Plantar ulcerations are a frequent complication for patients with diabetes mellitus [1] and restrict the quality of life forthe patients involved [2]. In particular, high plantar pressure loads as a component of the diabetic foot syndrome aredescribed as a cause of this symptom [3]. A successful treatment of plantar ulcerations should aim at effectivelyrelieving pressure on the area involved [3]. The objective of this investigation was to examine the possible reliefmechanisms of various therapeutic shoe models. Two models of a vacuum orthosis, designed to relieve plantarpressure for diabetics with plantar ulcerations, were examined in comparison with a forefoot-relief/wedge shoe and a“health shoe”.
INTRODUCTION
For 20 patients with diabetes mellitus (56.4±15.7 years) a plantar pressure distribution measurement was performedusing capacitive measuring soles (Pedar-X, Novel GmbH, Munich) (Fig. 2a), as they each walked a length of 20meters wearing a “health shoe”, a wedge shoe and two vacuum orthoses. The vacuum orthoses (VACOdiaped andVACOdiaped Plus, OPED GmbH, Valley) consisted of an orthosis shell, the inner shoe with vacuum cushions and arocker bottom sole. The VACOdiaped stood out here through a high and stable shaft (Fig. 1). The load was determinedin three areas of the foot, the forefoot, midfoot and hindfoot (Fig. 2b), using established parameters of pressuredistribution measurement (maximum force, pulse, peak pressure) and then compared for the different products.
METHODS
OBJECTIVE OF STUDYInvestigation of the pressure relief mechanisms of the VACOdiaped vacuumorthoses in comparison with a wedge shoe and a “health shoe” for patients
with diabetes mellitus
A comparative investigation of plantar pressure relief throughVACOdiaped vacuum orthoses from OPED®
* * *Measurements of plantar pressure distribution for patients with diabetes mellitus
Arne Nagel, Dieter RosenbaumDepartment of Motion Analysis, Clinic and Polyclinic for General Orthopedics, University Hospital of Muenster
Fig. 1: orthoses and shoe models (from left): “health shoe”, wedge shoe, VACOdiaped, VACOdiaped Plus.
Fig. 2:
a) Inserting the sensor soles to measure the pressuredistribution, here with theexample of the VACOdiaped
b) Areas of the foot for detai-led evaluation of loading (hind-foot, midfoot and forefoot)

Compared with the “health shoe”, the two vacuum orthosesand the wedge shoe significantly reduced the plantar pressureloads in the hindfoot and forefoot. At the same time an in-crease in the foot load in the midfoot area was demonstrated,which was associated with an increase in the contact area inthis region. Compared with the wedge shoe (Fig. 3 a+b), bothvacuum orthoses achieved a larger contact area and higherloading in the midfoot, as well as a significantly lower pressureload in the hindfoot. Regarding comfort, the VACOdiaped Plusattained similarly high ratings as the “health shoe” that hadachieved the highest rating. The VACOdiaped (high rise boot)and the wedge shoe were rated significantly lower in regardto comfort.
RESULTS
The vacuum othoses, utilizing vacuum cushions, produce an even pressure distribution under the entire foot, avoidingpressure peaks. The VACOdiaped achieved a relief of the forefoot comparable to the wedge shoe. Pressure loads inthe wedge shoe shifted to the hindfoot, which can be dangerous for patients with diabetes who are prone to ulcera-tions. The VACOdiaped Plus, with its shorter shaft, does not achieve the same forefoot relief as the VACOdiaped andthe wedge shoe; however, patients felt it to be considerably more comfortable. To summarize, it can be stated thatthe two vacuum orthoses can achieve a more even pressure distribution, as well as an effective pressure relief, andare thus suited to avoid pressure peaks.
DISCUSSION
[1] Hader et al., Diabetes und Stoffwechsel 2004 (13).[2] Nabuurs-Franssen et al., Diabetologia, 2005 48(9).[3] Rathur and Boulton, Nat. Clin. Pract. Endocrinol Metab, 2007 3(1).
LITERATURE
CONTACT
CONCLUSIONS
➥ The vacuum orthoses achieve an effective relief, in accordance with their objectives
➥ In contrast to the wedge shoe, no significant increase in load in other foot areas were seen with the orthoses; an even pressure distribution under the entire foot is attained
➥ The vacuum orthoses allow for a staged treatment:• VACOdiaped Plus: for prevention and for less severe cases• VACOdiaped: for more severe cases
Fig. 3:
a) An example of a pressure distribution for a single test person
b) Significant differences in the maximum pressure values in the foot areas for the4 orthoses and shoe conditions (= p < 0.0125)
Prof. Dr. Dieter RosenbaumDepartment of Motion Analysis, Clinic and Polyclinic for General Orthopedics, University Hospital of MuensterDomagkstr. 3, 48149 Mü[email protected]
WM
-ST
DA
-02-
EN
a)
b)
health shoe wedge shoe VACOdiaped VACOdiaped-Plus
*

KLINIKUM
Klinikum Dortmund gGmbH, 44123 Dortmund Medizinische Klinik Nord Diabetes center Senior physician Dr. Marcus Altmeier lnternist/Gastroenterologist/Diabetologist
Address: Münsterstr. 240, 44145 Dortmund (Germany) Please contact: Dr. M. Altmeier Telephone: +49 02311953-18250 Fax: +49 0231/953- E-mail: [email protected] Your reference: My reference: altmeiermlkä Date: August 19th, 2009
Statement on the use of the VACOdiaped to relieve pressure in diabetic foot syndrome
1. Definition of diabetic foot syndrome: In diabetes patients, every lesion in the foot and distal lower leg area is categorized as diabetic foot syndrome (DFS). In the majority of cases, the origin of the lesion is a neuropathy, possibly in combination with, and rarely caused solely by, an arterial occlusive disease. In a broader sense, Charcot foot can also be classified under diabetic foot syndrome. If not properly treated, there is a risk of serious follow-up illness, down to sepsis and / or loss of limb. Pressure-relieving measures are a fundamental basis of therapy, along with optimizing the metabolism and a structured wound-dressing, as well as ensuring sufficient blood circulation.
2. Pressure-relief systems:
There is a variety of different pressure relief systems on the market. So-called forefoot and heel relief shoes should not be used if there is concurrent neuropathy and loss of sensitivity, since stress is generally put on the wound during the walking process. In classic bandage shoes, there is no significant relief of pressure - pressure can only be avoided with shoes that are not too narrow. An individually produced total contact cast (TTC, with and without padding) and if necessary, individually produced one- or two-cast orthoses (e.g. molded resin orthosis according to a construction method of the company Zieger) are still considered to be the gold standard of pressure relief. These systems demonstrate a high potential for pressure relief, but are expensive to produce and are not available at all times and at every location. The use of a VACOdiaped pressure relief system has proven itself as an alternative in clinical care. In our own pressure measurements, a considerably better pressure relief was demonstrated, especially in the area of the toes and forefoot, in comparison to the brace shoe, and an equally effective pressure relief in comparison to the TCC. The application is simple and safe, and can generally be handled easily by nursing staff or by the patient. As in all pressure relief systems, if neuropathy and / or peripheral arterial occlusive disease are diagnosed, you must be very careful of any lesions and pressure marks. There are currently not enough studies on the decision of the need for anticoagulation in joint-stiffening pressure relief systems to be able to make decisions on their necessity, and to be the subject of discussion.
Klinikum Dortmund gGmbH Akademisches Lehrkrankenhaus der Universität Münster Chairman: Dr. Gerhard Langemeyer Management: Mechthild Greive (CEO), Manfred Fiedler (CHRO) Dortmund District Court HRB 15156 Sparkasse Dortmund (BLZ 440 50199) A/c No. 001049 550 www klinikumdo.de

3. Possible indications for the use of a VACOdiaped:
From clinical experience and from the result of comparative pressure measurements between a brace shoe, a total contact cast and the VACOdiaped, the following possible indications for a VACOdiaped were revealed:
1.) Plantar forefoot lesions, especially in the area of the metatarsal bone, for pressure
relief with and without signs of infection. 2.) Condition after amputation in the region of the toes and forefoot up to the Chopart
line, for pressure relief in the scar region and the prevention of shearing forces. 3.) With sufficient clinical experience and selected patients, a therapy for acute Charcot
foot can also be undertaken in the VACOdiaped, there are currently insufficient data concerning this. In the period from 6/08 - 6/09, some 40 patients with a Charcot in Levin stage 1 were treated, in most cases medical provision with the VacoDiaped was considered to be sufficient until a final shoe was introduced.
4.) In particular situations, and after an individual decision of a physician, lesions of other types on the metatarsal to the heel, or in the distal lower leg area, can be treated with the VACOdiaped, especially if no suitable alternative is available. As with all pressure relief systems, however, the pressure relief in this area is less effective than in the forefoot area.
4. Contraindications: 4.1 All pressure relief systems have an increased risk for patients with an unstable gait, and in
certain cases, the benefit of a pressure relief must be weighed up against the danger of falling.
4.2 In particular with pressure relief systems that extend beyond the ankle, sufficient perfusion must be ensured. For critical ischemia, this may result in a further decline in perfusion through pressure in the lower legs area. In this case, these systems should not be used. An alternative could be the use of a VacoDiaped plus with a low shaft, although currently we do not yet have any own measured values with respect to pressure relief.
4.3 The VACOdiaped can, with limitations, be adjusted to the foot shape by distorting it using hot air. For major deformations and very large and wide foot shapes, it is possible that a VACOdiaped may not be suitable, but this must be decided on the basis of individual cases. The patient/family/nursing staff must take an active involvement to avoid the possibility of the device being wrongly fitted. If it is wrongly fitted (e.g. a missing vacuum or if the vacuum cushion has been forgotten) the risk of pressure points can be increased. The physician must also make the decision based on individual cases, in case the need arises.
5. Final comment: The current state of research into pressure relief systems is generally unsatisfactory. One of the fundamental problems in the effectiveness of all pressure relief systems appears to be acceptance by the patient. Many pressure relief systems are not worn sufficiently, so that often closed systems are recommended; the consequence of this is that inspections of the wound are inadequate, so that their use, particularly where there are infected wounds, must be assessed as being critical. From our experience, the VACOdiaped is well accepted by patients, and is correspondingly worn regularly. Controlled studies in accordance with the criteria of the EBM do not exist yet, especially no comparative studies between different pressure relief systems, so that evaluations overall are based on clinical experience. The treatment of patients with diabetic foot syndrome should be reserved for institutions that can demonstrate adequate knowledge and experience in the treatment of DFS (e.g. certification by the DDG / Fuß-AG).
BSNR: Seite 2

Examples for Treatmentwith VACO®diaped
➧
➧
After
Weeks
12
After
Weeks
12

OPED Inc. • 47 Loring Drive • Framingham, MA 01702 • USAFon +1/508/879 0762 • Fax +1/508/879 0769
[email protected] • www.opedinc.com
➧
➧
➧
➧
➧After
Weeks
9
After
Weeks
24
After
Weeks
7
After
Weeks
15
After
Weeks
5
WM
-IN
DA
-03
-1-U
S, ©
ww
w.a
rtra
ctio
n.d
e