The Diabetic Foot: What You Need to Know
-
Upload
omar-haqqani -
Category
Health & Medicine
-
view
170 -
download
2
Transcript of The Diabetic Foot: What You Need to Know

THE DIABETIC FOOT: WHAT YOU NEED TO KNOW
Dr. Jeffrey Stone, DPMDiplomate, American Board of Foot and Ankle SurgeryFellow, American College of Foot and Ankle surgeons

DISCLOSURE
Author does not have any disclosures

DIABETES: THE STATISTICS
• In the past 30 years the incidence of diabetes among the worlds adult population has nearly quadrupled, rising to over 422 million individuals worldwide, a number that is expected to increase to 642 million by 2040.1

DIABETES: THE STATISTICS
• It is estimated that in the U.S., 29.1 million people (9.3% of the population) have diabetes, with 21 million being diagnosed and 8.1 million being undiagnosed.2,3,4
• The U.S. government estimates that approximately 2 out of every 5 Americans will develop type 2 diabetes at some point during their adult lives.5

DIABETES: THE STATISTICS
• People affected by diabetes have a 25 percent lifetime risk of developing a diabetic foot ulceration (DFU).
• Annually, approximately $ 480 billion dollars worldwide goes toward the treatment of DFU’S.6,7,8

DFU: DIABETIC FOOT ULCERS
• There are approximately 6 million people in the U.S. with chronic, non-healing pedal ulcers, costing the health care system more than 3 billion per year.9,10
• The most common chronic wounds are found on the lower extremities.

DFU: DIABETIC FOOT ULCERS
• 98% of these chronic ulcers are either vascular or diabetic in etiology, and 85% affect patients whom are 65 years or older.11,12
• Ulcers are considered chronic if they have not gone through and orderly and timely healing process, producing anatomic and functional integrity over 3 months, or have not shown a 15% reduction weekly or approximately a 50% surface area reduction over a 1 month period.13,14

DFU: DIABETIC FOOT ULCERS
• Diabetic foot infections (DFI) are often a serious consequence of DFU’S. Consequently, DFI’S are the most common cause of non-traumatic foot amputations in the U.S.15,16
• Fifteen percent of DFU’S result in a
more proximal amputation leading to high rates of mortality, within 5 years.

DFU: DIABETIC FOOT ULCERS
• Driver and colleagues in 2008 reported that uncomplicated DFU’S cost upwards of $8,000—Infected foot ulcers up to $17,000. If amputation is required the costs exceed $45,000 per person.17
• Peripheral vascular disease (PVD) inflates the cost of treating a purely neuropathic wound (DFU) by four times.18

DFU: DIABETIC FOOT ULCERS
• DFU recurrence rates are reported as high as 34% at 1 year, 61% at 3 yrs, 70% at 5 yrs.19
• Existing prevention methods have the potential to decrease the risk of amputation in diabetics with a L.E. ulcer history by 50%.20
• As quality health care providers, we are striving to perfect the REMISSION of the diabetic foot.

VASCULAR DISEASE AND DIABETES
• 83% of vascular-related L.E. amputations in the U.S. are associated with DM, however P.A.D. with or without diabetes is another leading cause of L.E. amputations.21
• PAD is a progressive disease that can lead to critical limb ischemia (CLI), in the most advanced form.
• 3-10% of the global population has PAD, with an increase to 15-30% in pts. > 70 years old, and with D.M.
• Patients with CLI require revascularization and even with surgery amputation rates can reach 25%.22

PAD WORKUP
• The initial PAD workup is prompted by the clinical exam: pedal pulses, digital c.f.t., shiny hairless digits, pallor on elevation and rubor with dependency (loss of vasomotor control), intermittent claudication or rest pain.
• RISK FACTORS INCLUDE: smoking, dm, genetics, hyperlipidemia, lower extremity ulcerations.22

PAD WORKUP
• Non-invasive vascular studies, ankle Brachial index (ABI), pulse volume recordings (PVR’S), MAY OR MAY NOT SHOW AN OCCLUSIVE LESION. If suspected, next we perform an angiogram (CTA, MRA, OR DIAGNOSTIC).

THE CHALLENGING D.F.U.
• Diabetic foot ulcers may result from a combination of neuropathy, vasculopathy, pressure/shear, and or infection.
Pathophysiology• Diabetic hyperglycemic states in
individuals leads to the development of glycoproteins, basement membrane thickening, endothelial proliferation, decreased vessel permeability and altered cell migration.23

THE CHALLENGING D.F.U.
• Extracellular matrix degradation and faulty cellular regulation induce high concentrations of inflammatory cytokines within the wound environment.
• Cellular senescence (fibroblasts), and increased protease enzymes develop, these cascades degrade growth factors, receptors, and wound matrix and support structures. Angiogenesis decreases and an environment with an imbalance of matrix metalloproteinases (MMP’S) and tissue inhibitor metalloproteinases (TIMP) develops.24

THE CHALLENGING D.F.U.
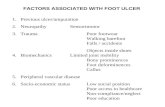
FACTORS THAT PREVENT CHRONIC WOUNDS FROM HEALING
• Poor vascular supply• Elevated mechanical pressures, either from fat pad
atrophy, biomechanical abnormalities, or foot deformity
• Poor glycemic control• Decreased albumin levels (3.5)• Infections, including the presence of biofilms• Neuropathy (sensory, motor, autonomic).• Unrecognized foot trauma and the presence of foreign
bodies • Diminished growth factors, collagen, and or hyaluronic
acid• Elevated matrix metalloprotease (mmp’s) levels25

THE CHALLENGING D.F.U.
Source: podiatrym.com

D.F.U. TREATMENT OPTIONS
• Tissue debridement: sharp, ultrasonic• Inflammation and infection control • Revascularization • Local wound care • Offloading: contact cast techniques, DH pressure
relief cam boot, instant contact cast• Larval therapy • HBO, • Negative pressure wound therapy (VAC) • Advanced skin substitutes and grafts: Theraskin
(human cryopreserved allograft), EPIFIX (dhacm)• Collagen: triple stranded helical structure and major
protein comprising the wound extracellular matrix.

D.F.U. TREATMENT OPTIONS
COLLAGEN IN WOUND HEALING Healing Phase COLLAGEN INFLAMMATORY PHASEHEMOSTASIS ASSISTS WITH HEMOSTASISVASODILATION ATTRACT MACROPHAGESNEUTROPHILS-ATTRACT MACROPHAGES ENHANCES INFLAMMATORYMACROPHAGES ATTRACT FIBROBLASTS INFILTRATION TO IMPROVEINDUCE COLLAGEN SYNTHESIS WOUND CLEANSING PROLIFERATIVE PHASEFibroblasts initiate collagen synthesis Scaffold for fibroblast attachmentGranulation tissue forms Attracts additional fibroblasts to siteAngiogenesis Becomes a template for new growth Presents attachment site for
fibroblasts MATURATION PHASEConnective tissue matrix reorganizes Aid in deposits of oriented collagen fibersCollagen fibrils consolidate into thicker fibers Improves strength, replacing and Reinforcing scar tissueCells gain more tensile strength

D.F.U. TREATMENT OPTIONS
THE DIABETIC FOOTWOUND MANAGEMENT
• The American Diabetes Association recommends that all patients with diabetes see a lower extremity specialist for foot screenings at routine intervals depending on need
• At least every six months for a basic evaluation
• At least 2 months for those at greater risk for DFU’S.25

D.F.U. TREATMENT OPTIONS
DAILY DIABETIC FOOT CARE• Foot inspections at home with a mirror if
needed, diabetic seamless socks reduce frictions, foot exercising to promote circulation, and topical antifungal or hydrating lotions.
• Inform at risk pts. To avoid self-damaging behavior, like barefooted walking, using ill-fitting foot wear, poor glycemic control, or delaying medical professional foot inspection and nail care.

DIABETIC NEUROPATHY
• Nerve damage caused by high blood sugar levels.
• Affects 30% of the Diabetic population and nearly 70% of patients with diabetes greater than 10 years.
• High blood sugar levels cause chemical changes within the nerve cells that lessen the supply of blood that goes to the nerves
• Autonomic, Sensory, Motor

DIABETIC NEUROPATHY
• These changes damage the nerves ability to transmit signals.
• Symptoms: numbness, pain, burning, tingling. Usually in the hands, feet or legs.
• Can affect internal organs leading to indigestion, diarrhea, rapid heart rate, abnormal sweating, genital / urinary problems.

DIABETIC NEUROPATHY
Decreased sensory perception of:• Vibration• Temperature• Touch• Pain

DIABETIC NEUROPATHY
• Autonomic Neuropathy causes decreased sweating in the extremities resulting in dry, scaly, cracked skin. This can also lead to infections.

DIABETIC NEUROPATHY
NEUROPATHY OFFICE EXAMS

DIABETIC NEUROPATHY
MOTOR NEUROPATHY• Small intrinsic muscles of the foot
atrophy• A muscle imbalance of the flexors
and extensors develops• Hammer and claw toes• MPJ become unstable with prominent
metatarsal heads (ball of the foot)

DIABETIC NEUROPATHY
MOTOR NEUROPATHY• Soft tissue covering the ball of the
foot is exposed to abnormal pressures with walking and standing; callus formation develops. This can lead to pressure ulceration.

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY
REDUCING PEAK PLANTAR PRESSURES• Repetitive pedal stresses in the
presence of neuropathy, bony prominences, or PVD, augments the rise of DFU’S

DIABETIC NEUROPATHY
PLANTAR PRESSURE REDISTRIBUTION• Neuropathy and decreased metabolic
response renders patients unable to organically detect repetitive stress and trauma to their plantar structures.
• pts. With DM are shown to regularly have elevated peak plantar pressures >200kPa, which is a pressure threshold shown to maintain previous ulcerated sites.26

DIABETIC NEUROPATHY
OFFLOADING DEVICES• Uccioli. et al,(Diabetes Care ), found ulcer
recurrence rates with normal footgear to be more than 200% higher than patients using diabetic certified shoes.
• It is imperative that diabetic patients with polyneuropathy or PVD convert to diabetic shoes.
• Total contact cast (tcc) usefull?-expensive, high learning curve, poor reinbursement, lengthy application, infection, additional ulcers.
• INSTANT CONTACT CAST (ICC) –short application time, less expensive, easy learning curve, less pt. apprehension.

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

DIABETIC NEUROPATHY

PEDAL ULCER TREATMENTS
• Debridement • Infection control (topical, IV or oral antibiotics)• Off loading devices• Appropriate shoes with insoles• New technology (Negative pressure (vac), HBO, Gene therapy, growth factors, biological grafts)• Dressings (gels, foams, silver, promogran, gauze)• Surgery

PEDAL ULCER TREATMENTS

PEDAL ULCER TREATMENTS
COLLAGEN POWDER

ONYCHOMYCOSIS
• Fungal infection of the nails.• Causes discoloration, and thickening
which can cause pain, infection, and ulceration.

DIABETIC NAIL INFECTIONS

THE DIABETIC FOOT
SURGICAL TREATMENTS AND METHODS OF OFFLOADING
• Forefoot deformities: hammer and claw toes, metatarsal head deformities.
• The rates of infection post digital surgeries in pts. with diabetes parallel those of pts. Without diabetes; so surgery should be considered when it is an option.

THE DIABETIC FOOT
FLEXOR TENOTOMY• Digital contracture- hammer
toe-,with a distal lesion; must be reducible and flexible

THE DIABETIC FOOT
HEALED FLEXOR TENOTOMY AT 3 WKS.

THE DIABETIC FOOT
DIABETIC FF LESIONS

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT
HALLUX ABDUCTO VALGUS BUNIONS
• Angular rotational deformity involving dislocation of the first mpj
• Symptoms: pain, prominence, swelling, redness, difficulty with fitting shoes

THE DIABETIC FOOT
HAV- BUNIONS

THE DIABETIC FOOT
TWO WEEKS POST BUNIONECTOMY AND 2ND TOE ARTHROPLASTY

THE DIABETIC FOOT
BUNIONECTOMY, HAMMER TOE , AND METATARSAL OSTEOTOMY- COMBINATION

THE DIABETIC FOOT

THE DIABETIC FOOT
EQUINUS• Definition- The inability to DF the
foot at the ankle to 90 degrees,-normal = 10 deg.
• Essentially overloads the FF increasing peak plantar pressures.
• Peak plantar pressures are reduced by up to 28% with posterior calf lengthening –(TAL, EGR)

THE DIABETIC FOOT

THE DIABETIC FOOT
Midfoot Procedures• Performed to stabilize, realign, and
allow the foot to mechanically function, reducing deformity

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT
PLATELET RICH PLASMA -PRP

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT

THE DIABETIC FOOT
SURGICAL REARFOOT OFFLOADING

THE DIABETIC FOOT

THE DIABETIC FOOT
HEEL ULCER DEBRIDEMENT WITH THERASKIN ALLOGRAFT

THE DIABETIC FOOT
MUSCULOSKELETAL DEFORMITY• Neuropathic Arthropathy (Charcot’s foot)• Characterized by chronic, progressive,
degenerative, dislocating disease of one or more bones and joints; and is identified by swelling, bleeding, increased temperature, bone changes and joint instability

THE DIABETIC FOOT
COMPARISON OF DFU RECURRENCE• 14% overall recurrence rate in re-
ulceration in patients with prior DFU who underwent prophylactic surgical offloading, versus a 42% rate of recurrence in patients whose treatments were limited to non-surgical therapies alone.29

THE DIABETIC FOOT
PLANTAR FAT PAD AUGMENTATION• Silicone- injected filler, limitations on
availability- prior adverse reactions• Autologous Fat Grafting- lipofilling
injections from abdomen—staying power?
• Graft Jacket, Dermaspan- dehydrated allogenic skin products. –good clinical outcomes.

FUTURE TECHNOLOGY
• Calor, erythema, and high peak plantar pressures are some of the earliest clinical indications of inflammation that marks initiation of ulcer development.
• Integration of wearable sensors, and medical telemetry, intelligent insoles or smart socks - could potentially alert the user of warmth and pressure dangers by using real time analysis.30

MULTIDISCIPLINARY APPROACH
• Between 10%-40% of patients with diabetes also have a form of vascular disease, a comorbid factor that increases the likelihood of ulcerative recurrence by a factor of 10.
• Patients with vascular disease and peripheral neuropathy also have higher re-ulceration and amputation rates than those with neuropathy alone.31

MULTIDISCIPLINARY APPROACH
• As the predominance of neuropathic ulcers continues to shift toward the neuroischemic, the increasing adoption of the TOE and FLOW multidisciplinary model, where podiatric surgeons and vascular surgeons personify the backbone of a diabetes wound management team, will see accelerated implementation.32

MULTIDISCIPLINARY APPROACH
THE MULTIDISCIPLINARY TEAM• A coordinated professional team
approach has been shown to decrease the frequency of limb loss by as much as 70%, and perpetuate diabetic foot remissions worldwide.33

THANK YOU
THANK YOU

REFERENCES1. Gazes, et.al., assessing collagen-based modalities for diabetic foot ulcerations. Podiatry today may 2016. p51-562. Pecoraro, et. Al.. Pathways to diabetic limb amputation. Diabetes Care. 513-21. 19903. Driver,et. Al . The cost of the Diabetic foot. Diabetes Care. 17-22. 20104. Hackenthal et al ., Progress stalled in Diabetic foot ulcers. Advances in Therapy.2014:817-836.5. Center for Disease Control and Prevention. National diabetes statistics report. 20146. International Diabetes Foundation Diabetes Atlas 6th edition.7. Snyder, et,al. OSTOMY WOUND MANAGEMENT 2010,56 s1-24.8. Garwood. Et al. Bioengineered alternative tissues in diabetic wound healing. Clinics Podiat. Med. Surg., 2015 32,121-133.9. Mathieu D. Et al.,Non Healing Wounds. Handbook of Hyperbaric Medicine,2006,p401-42710. Menke NB. Et al., Impaired wound Healing. CLINICS DERMATOLOGY. 200711. Mathieu D. - 9 above. 12. Roboson MC. Guidelines of the best care of chronic wounds. WOUND REPAIR REGEN. 2006,647-710.13. Werdin F. et.al. Evidence based medicine strategies for chronic wounds. EPLASTY 2009,9-19.14. Sheehan p. Percent change in wound area of dfu……., Plastic Recon. Surg., 2006,239-44.15. Lipsky BA. ID society of America………., CLINICAL INF. DIS. 2012. 132-173.16. Lipsky BA. Diagnosis and Treatment of DfI. CLINICAL INF. DIS. 2004, 885-910.17. Driver VR. Health economic implications……….,JOURNAL OF MANAGED CARE MED. 2008,13-1918. Miller JD., wound Mgmt. PODIATRY TODAY , August 2016, p 115-21.19. Diehl K. Lower Ext. Major and Minor………………,POD. MGMT., 2105, 58-6620. Miller JD,,, 18 above21,22. Diehl K. The diabetic Foot, POD. MGMT. NOV. 2015 P 61-66.23. Driver V.,Clinical trial of Integra……,WOUND REPAIR REGEN. 2015,891-90024. Brett D. A review of collagen and collagen based wound dressings. WOUNDS 2008,20- 347-56.25. Landsman A, Wound Mgmt. PODIATRY TODAY. aug.2016, p85-89Chart 1 = wound diagram – 25Chart #2= Brenner et al. collagen treatment in the diabetic foot, POD. MGMT., NOV 2015 p111-118.26. Owings et al. Plantar Pressures in diabetic pts……..,Diabetes med. 2009, 1149-1146.27. Uccioli et al, Diabetes Care. 1995, 1376-1378.28. DC Armstrong, Lengthening of the Achilles Tendon……. J Bone Joint Surgery. 1999,535-538.29,30,31,32. JD Miller et al. The diabetic foot in remission, Podiatry Management August, 2016, pg. 115-122.