The conducting system of the heart 1. The nodal system: Which consists of two nodes in the right...
-
date post
21-Dec-2015 -
Category
Documents
-
view
234 -
download
0
Transcript of The conducting system of the heart 1. The nodal system: Which consists of two nodes in the right...
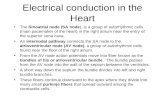
11 . .The nodal system: Which consists of two nodes in the right The nodal system: Which consists of two nodes in the right atriumatrium::
The sinoatrial node (also called the S-A node or the sinus The sinoatrial node (also called the S-A node or the sinus node)node) . .
The atrioventricular node (also called the A-V node)The atrioventricular node (also called the A-V node)..
22 . .The internodal pathwayThe internodal pathway::
33 . .The purkinje system (also called the His-Purkinje system)The purkinje system (also called the His-Purkinje system):: The atrioventricular bundle (also called the A-V bundle or The atrioventricular bundle (also called the A-V bundle or
the bundle of His)the bundle of His).. The right and left bundle branchesThe right and left bundle branches . .
The Purkinje fibersThe Purkinje fibers..
The conducting system of the heartThe conducting system of the heart
Functional histologyFunctional histology
11 . .The contractile muscle fibersThe contractile muscle fibers::
Differences between the contractile cardiac Differences between the contractile cardiac muscle fibers and skeletal muscle fibersmuscle fibers and skeletal muscle fibers..
22 . .Nodal fibers of the S-A and A-V nodesNodal fibers of the S-A and A-V nodes::
33..The Purkinje fibers of the Purkinje systemThe Purkinje fibers of the Purkinje system::
STRUCTURE OF A MYOCARDIAL CELLSTRUCTURE OF A MYOCARDIAL CELL
Mitochondria Sarcolemma
T-tubuleSR
Fibrils
Functions of the atriaFunctions of the atria
11 . .The main function of the atria is to The main function of the atria is to accommodate blood returning to the heart during accommodate blood returning to the heart during ventricular systole until it is passed on to the ventricular systole until it is passed on to the ventricles during ventricular diastoleventricles during ventricular diastole..
22 . .The pumping action of the atria increases the The pumping action of the atria increases the ventricular filling. This increases the pumping ventricular filling. This increases the pumping capacity of the ventricles by 15-20%capacity of the ventricles by 15-20%..
Function of the ventriclesFunction of the ventricles
The ventricles are the central pumps of the The ventricles are the central pumps of the circulatory system. They pump the venous return circulatory system. They pump the venous return which they received by the atria. The right ventricle which they received by the atria. The right ventricle pumps the systemic venous return into the pumps the systemic venous return into the pulmonary circulation and the left ventricle pumps pulmonary circulation and the left ventricle pumps the pulmonary venous return back into the systemic the pulmonary venous return back into the systemic circulationcirculation..
Ventricular volumesVentricular volumesEnd-diastolic volume (EDV): is the volume of blood in the ventricle at End-diastolic volume (EDV): is the volume of blood in the ventricle at the end of diastole. It is about 130 mlthe end of diastole. It is about 130 ml..
End-systolic volume (ESV): is the volume of blood in the ventricle End-systolic volume (ESV): is the volume of blood in the ventricle at the end of systole. It is about 55 mlat the end of systole. It is about 55 ml..
Stroke volume (SV): is the volume of blood that is pumped by the Stroke volume (SV): is the volume of blood that is pumped by the ventricle per beat. It is equal to the difference between the EDV and ventricle per beat. It is equal to the difference between the EDV and ESV. Its is about 75 mlESV. Its is about 75 ml..
Diastolic filling volume (DFV): is the volume of blood which flows Diastolic filling volume (DFV): is the volume of blood which flows from the atrium into a ventricle during diastole. It is equal to the from the atrium into a ventricle during diastole. It is equal to the difference between the EDV and the ESV. It is about 75 mldifference between the EDV and the ESV. It is about 75 ml..
Properties of the cardiac muscleProperties of the cardiac muscle
The heart has four basic properties which are The heart has four basic properties which are essential for its functioning as the central essential for its functioning as the central pump of the CVS. These arepump of the CVS. These are::
11 . .AutorhythmicityAutorhythmicity
22 . .ConductivityConductivity
33 . .ExcitabilityExcitability
44 . .ContractilityContractility
AutorhythmicityAutorhythmicity
AutomaticityAutomaticity
RhythmicityRhythmicity
AutorhythmicityAutorhythmicity
Autorhythmicity is a myogenic innate Autorhythmicity is a myogenic innate property of the heart independent of its property of the heart independent of its
nerve supplynerve supply..
AutorhythmicityAutorhythmicity The conducting system of the heart is responsible for The conducting system of the heart is responsible for generating rhythmic, electrical impulses which drive generating rhythmic, electrical impulses which drive the heart to beat in a rhythmic waythe heart to beat in a rhythmic way..
The focus which generates the highest frequency of The focus which generates the highest frequency of impulses is he one that drives the whole heart and is impulses is he one that drives the whole heart and is called the pacemaker of the heartcalled the pacemaker of the heart..
The normal pacemaker of the human heart is the S-A The normal pacemaker of the human heart is the S-A nodenode..
AutorhythmicityAutorhythmicity There are several possible sites in the conducting system that There are several possible sites in the conducting system that can act as possible pacemakerscan act as possible pacemakers::
Sino-atrial (SA) nodeSino-atrial (SA) nodeAtrio-ventricular (AV) nodeAtrio-ventricular (AV) nodePurkinje systemPurkinje system If the primary pacemaker is damaged or blocked, the If the primary pacemaker is damaged or blocked, the secondary pacemaker takes over. If the flow of impulses secondary pacemaker takes over. If the flow of impulses from the atria to the ventricles stops completely, the tertiary from the atria to the ventricles stops completely, the tertiary pacemaker takes over and the ventricles continue to beat at pacemaker takes over and the ventricles continue to beat at the idioventricular rhythmthe idioventricular rhythm..
THE RESTING MEMBRANE THE RESTING MEMBRANE POTENTIAL OF THE CARDIAC CELLPOTENTIAL OF THE CARDIAC CELL
K+
145mEq
K+
5mEq
IN OUT
Em= -60LogKi/Ko-90mv
Na+Na+
145mEq
10mEq
The pacemaker potentialThe pacemaker potential
The pacemaker cells are The pacemaker cells are characterized by having an unstable characterized by having an unstable
membrane potentialmembrane potential . .
This is the basis for automaticityThis is the basis for automaticity
The pacemaker cells are characterized by having an unstable The pacemaker cells are characterized by having an unstable membrane potential. After firing an action potential, the membrane potential. After firing an action potential, the membrane potential decreases i.e. the membrane membrane potential decreases i.e. the membrane depolarizes gradually from a basal value of ~ -60mV to a depolarizes gradually from a basal value of ~ -60mV to a critical firing level of –45 mV. At this level, an action critical firing level of –45 mV. At this level, an action
potential is fired and the cycle is repeatedpotential is fired and the cycle is repeated . .
The gradual depolarization of the S-A nodal cells is called the The gradual depolarization of the S-A nodal cells is called the pacemaker potential or the prepotential. The early part of pacemaker potential or the prepotential. The early part of the pacemaker potential is caused by a decrease in the the pacemaker potential is caused by a decrease in the permeability of the membrane to Kpermeability of the membrane to K++. The late part is caused . The late part is caused by Caby Ca++++ influx through the transient (T-type) Ca influx through the transient (T-type) Ca++++-channels-channels..
The pacemaker potentialThe pacemaker potential
The pacemaker action potentialThe pacemaker action potential
When the pacemaker potential reaches the When the pacemaker potential reaches the critical level (~ -45 mV), an action potential critical level (~ -45 mV), an action potential
is produced in the pacemaker cellsis produced in the pacemaker cells..
This action potential propagates to the This action potential propagates to the surrounding myocardial cellssurrounding myocardial cells..
ELECTROPHYSIOLOGY OF THE ELECTROPHYSIOLOGY OF THE CONTRACTILE FIBERCONTRACTILE FIBER
mv
t (msec)
-90
0
+20
0 300
0
12
3
4
Cardiac Cell
AMP
To oscilloscope
ME
MB
RA
NE
PO
TE
NT
IAL
(m
V)
-90
0
0
12
3
4
TIME
PHASE0 = Rapid Depolarization0 = Rapid Depolarization (inward Na(inward Na++ current) current) 1 2 = Plateau (inward Ca++ current)
3 = Repolarization (outward K+ current)4 = Resting Potential
ACTION POTENTIALS FROM ACTION POTENTIALS FROM DIFFERENT AREAS OF THE HEARTDIFFERENT AREAS OF THE HEART
mv
0
-90mv
mv
0
-90mv
mv
0
-60mv
ATRIUM VENTRICLE
SA NODE
time
ME
MB
RA
NE
PO
TE
NT
IAL
(m
V)
0 0
-50 -50
-100 -100
SANVENTRICULULARCELL
ACTION POTENTIALS
0
12
3
4
4
0 3
The pacemaker action potential differs from the The pacemaker action potential differs from the action potential of the contractile myocardial action potential of the contractile myocardial cells in the followingcells in the following::
Depolarization phase is mainly due to CaDepolarization phase is mainly due to Ca2+2+ influx influx through long-lasting (L-type) Cathrough long-lasting (L-type) Ca2+2+-channels-channels..
Depolarization phase is relatively slow to developDepolarization phase is relatively slow to develop..
There is no plateau phase. Repolarization There is no plateau phase. Repolarization immediately follows depolarizationimmediately follows depolarization..
Ectopic fociEctopic foci An ectopic focus is an area in the contractile An ectopic focus is an area in the contractile myocardium, which discharges electrical myocardium, which discharges electrical impulsesimpulses..
Normally, the contractile myocardium has a stable Normally, the contractile myocardium has a stable resting membrane potential and is incapable of resting membrane potential and is incapable of discharging impulsesdischarging impulses..
Under some non-physiological conditions, some Under some non-physiological conditions, some myocardial cells acquire rhythmic electrical myocardial cells acquire rhythmic electrical activity and act as foci that send un-timed activity and act as foci that send un-timed electrical impulses or might even take over the electrical impulses or might even take over the heart and act as the pacemakerheart and act as the pacemaker..
ChronotropismChronotropism
Chronotropism means an influence on the Chronotropism means an influence on the heart rateheart rate..
A +ve chronotropic factor (or effect) is one A +ve chronotropic factor (or effect) is one that increases the heart ratethat increases the heart rate..
A –ve chronotropic factor (or effect) is one A –ve chronotropic factor (or effect) is one that decreases the heart ratethat decreases the heart rate..
Factors that influence cardiac Factors that influence cardiac autorhythmicityautorhythmicity
Several factors influence autorhythmicity Several factors influence autorhythmicity by influencing the rate of discharge from by influencing the rate of discharge from the heart pacemaker. These factors could the heart pacemaker. These factors could
be classified intobe classified into::
Nervous factorsNervous factors
Chemical factorsChemical factors
Physical factorsPhysical factors
Mechanical factorsMechanical factors
Nervous factorsNervous factors
The most important factor in the The most important factor in the regulation of the heart rate is the activity regulation of the heart rate is the activity
of the cardiovascular centers in the of the cardiovascular centers in the medulla oblongatamedulla oblongata . .
This activity is transmitted to the heart via This activity is transmitted to the heart via its sympathetic and parasympathetic its sympathetic and parasympathetic
nerve supplynerve supply..
Sympathetic nerve supplySympathetic nerve supply There is a resting sympathetic tone that tends to increase the There is a resting sympathetic tone that tends to increase the heart rate up to 120 beats/minheart rate up to 120 beats/min . .
This tone is weak and is masked by the strong inhibitory vagal This tone is weak and is masked by the strong inhibitory vagal tone that decreases the heart rate down to 75 beats/min during tone that decreases the heart rate down to 75 beats/min during restrest . .
However, stimulation of the sympathetic cardiac nerves has a +ve However, stimulation of the sympathetic cardiac nerves has a +ve chronotropic effect. The heart rate may g up to 200 beats/minchronotropic effect. The heart rate may g up to 200 beats/min . .
The sympathetic chemical transmitter noradrenaline decreases The sympathetic chemical transmitter noradrenaline decreases the permeability of the pacemaker membrane to Kthe permeability of the pacemaker membrane to K++. This . This accelerates the depolarization of the membrane → shortens the accelerates the depolarization of the membrane → shortens the duration of the pacemaker potential → increases the frequency duration of the pacemaker potential → increases the frequency of discharge of impulses from the S-A node → increases the of discharge of impulses from the S-A node → increases the heart rateheart rate..
Parasympathetic nerve supplyParasympathetic nerve supply
There is a resting inhibitory vagal tone that keeps the There is a resting inhibitory vagal tone that keeps the heart rate at its resting level of ~ 75 beats/minheart rate at its resting level of ~ 75 beats/min . .
During deep quite sleep, the vagal tone increase and the During deep quite sleep, the vagal tone increase and the heart rate decreases down to 60 beats/minheart rate decreases down to 60 beats/min . .Vagal stimulation has a –ve chronotropic effectVagal stimulation has a –ve chronotropic effect . .
The parasympathetic chemical transmitter acetyl choline The parasympathetic chemical transmitter acetyl choline increases the permeability of the pacemaker increases the permeability of the pacemaker membrane to Kmembrane to K++. This slows down the depolarization . This slows down the depolarization of the membrane → prolongss the duration of the of the membrane → prolongss the duration of the pacemaker potential → deccreases the frequency of pacemaker potential → deccreases the frequency of discharge of impulses from the S-A node → decreases discharge of impulses from the S-A node → decreases the heart ratethe heart rate . .
Cutting or blocking the vagal nerve supply to the heart Cutting or blocking the vagal nerve supply to the heart (e.g., by atropine) leads to an increase in the heart rate (e.g., by atropine) leads to an increase in the heart rate
up to ~ 120 beats/minute. This is the sinus rhythm up to ~ 120 beats/minute. This is the sinus rhythm boosted by the resting sympathetic toneboosted by the resting sympathetic tone..
If this is followed by cutting or blocking the sympathetic If this is followed by cutting or blocking the sympathetic nerve supply to the heart (e.g., by atenolol), the heart nerve supply to the heart (e.g., by atenolol), the heart rate decreases down to 105 beats/minute; the natural rate decreases down to 105 beats/minute; the natural
inherent sinus rhythminherent sinus rhythm . .
Cutting or blocking the sympathetic nerve supply to the Cutting or blocking the sympathetic nerve supply to the heart with an intact vagal parasympathetic supply heart with an intact vagal parasympathetic supply produces no significant change in heart rate, i.e. it produces no significant change in heart rate, i.e. it
remains at its resting level of ~ 75 beats/minuteremains at its resting level of ~ 75 beats/minute..
Chemical factorsChemical factors
Adrenaline and noradrenaline are released Adrenaline and noradrenaline are released into the blood under conditions of stressinto the blood under conditions of stress . .
Both substances have a +ve chronotropic Both substances have a +ve chronotropic effecteffect..
Physical factorsPhysical factors
Arise in body temperature by 1 Arise in body temperature by 1 °°C increases the heat C increases the heat rate by 20 beats/minuterate by 20 beats/minute . .
The rise in body temperature increase the heart rate The rise in body temperature increase the heart rate by increasing the permeability of he membrane to by increasing the permeability of he membrane to
CaCa++++ during the pacemaker potential and during the pacemaker potential and increasing the speed of ionic fluxes across the increasing the speed of ionic fluxes across the
membrane during the action potentialmembrane during the action potential . .
The only physiological condition that rises body The only physiological condition that rises body temperature above the normal resting range is temperature above the normal resting range is
muscular exercisemuscular exercise . .
The sick sinus syndromeThe sick sinus syndrome
This is a pathological condition where there This is a pathological condition where there is bradycardia accompanied by frequent is bradycardia accompanied by frequent
attacks of dizziness and syncopeattacks of dizziness and syncope . .
It is caused by a disease of the S-A node It is caused by a disease of the S-A node depressing its activity and decreasing the depressing its activity and decreasing the
rate of impulse generationrate of impulse generation . .
This condition is treated by implantation of This condition is treated by implantation of an artificial pacemakeran artificial pacemaker..
ConductivityConductivity
Impulses can spread easily between cardiac Impulses can spread easily between cardiac muscle fibersmuscle fibers..
Yet, conduction in the heart is normally Yet, conduction in the heart is normally carried out by the specialized conducting carried out by the specialized conducting
system to ensure the spread of the system to ensure the spread of the excitation wave from the S-A node to all excitation wave from the S-A node to all
over the heart in certain patternover the heart in certain pattern..
The origin and pathway of the The origin and pathway of the cardiac impulsecardiac impulse
The normal cardiac impulse originates inside the S-A The normal cardiac impulse originates inside the S-A node, the normal pacemaker of the heart. The node, the normal pacemaker of the heart. The impulse is then conducted to the surrounding atrial impulse is then conducted to the surrounding atrial wall through the peripheral S-A nodal tissue. Then wall through the peripheral S-A nodal tissue. Then it propagates in three pathwaysit propagates in three pathways::
To the right atrium through the atrial muscle fibersTo the right atrium through the atrial muscle fibersTo the left atrium through the interatrial To the left atrium through the interatrial ‘Bachmann’s bundle‘Bachmann’s bundle’’
To the A-V node through the internodal bundlesTo the A-V node through the internodal bundles
The impulse picked up by the A-V node is The impulse picked up by the A-V node is delayed for 0.1 – 0.15 second, then passed delayed for 0.1 – 0.15 second, then passed
on to the A-V bundleon to the A-V bundle . .
The A-V bundle conducts the impulses to The A-V bundle conducts the impulses to the buddle branchesthe buddle branches . .
Then from the bundle branches to the Then from the bundle branches to the Purkinje fibers on to the ventricular Purkinje fibers on to the ventricular
muscle fibersmuscle fibers..
Important functional Important functional characteristics of the A-V nodecharacteristics of the A-V node
The A-V node is characterized byThe A-V node is characterized by::Very slow conductivity:Very slow conductivity: This delays the transmission of This delays the transmission of impulses to the ventricles (A-V nodal delay). This delay impulses to the ventricles (A-V nodal delay). This delay allows the atria to finish with their systole before passing allows the atria to finish with their systole before passing the impulse to the ventricles to start ventricular systolethe impulse to the ventricles to start ventricular systole..
Long absolute refractory period after conducting an Long absolute refractory period after conducting an impulse:impulse: This limits the number of impulses that can be This limits the number of impulses that can be transmitted from the atria to the ventricles to 230 transmitted from the atria to the ventricles to 230 impulse/min. This protects the ventricles from receiving impulse/min. This protects the ventricles from receiving
high frequency of impulses from the atriahigh frequency of impulses from the atria..
Factors that influence Factors that influence conductivityconductivity
Sympathetic stimulation accelerates Sympathetic stimulation accelerates conduction and decreases the A-V nodal conduction and decreases the A-V nodal delaydelay..
Parasympathetic stimulation slows Parasympathetic stimulation slows conduction and may produce various conduction and may produce various
degrees of heart blockdegrees of heart block..
The one-way conduction in the A-The one-way conduction in the A-V bundleV bundle
The A-V bundle conducts impulses only in The A-V bundle conducts impulses only in one direction, i.e. from the A-V node to one direction, i.e. from the A-V node to
the bundle branchesthe bundle branches . .
This prevents the reentry of impulses from This prevents the reentry of impulses from the ventricles into the atriathe ventricles into the atria..
ExcitabilityExcitability
Excitability is the ability to respond to stimuliExcitability is the ability to respond to stimuli..
The resting membrane potential of the The resting membrane potential of the contractile fibers is stable at about – 90 mV. contractile fibers is stable at about – 90 mV.
When an effective stimulus is applied, a When an effective stimulus is applied, a propagated action potential is produced in propagated action potential is produced in
the cell membranethe cell membrane..
Phases and ionic basis of the Phases and ionic basis of the myocardial action potentialmyocardial action potential
ME
MB
RA
NE
PO
TE
NT
IAL
(m
V)
-90
0
0
12
3
4
TIME
PHASE0 = Rapid Depolarization0 = Rapid Depolarization (inward Na(inward Na++ current) current) 1 2 = Plateau (inward Ca++ current)
3 = Repolarization (outward K+ current)4 = Resting Potential
Phase 0 (Rapid depolarization):Phase 0 (Rapid depolarization): It is caused by the rapid influx of It is caused by the rapid influx of NaNa+ + into the cellinto the cell..
Phase 1 (Early partial repolarization):Phase 1 (Early partial repolarization): During this phase, the During this phase, the permeability of the membrane to Napermeability of the membrane to Na+ + is rapidly reduced, but the is rapidly reduced, but the membrane permeability for both Camembrane permeability for both Ca2+2+ and K and K++ increases. The increases. The overall effect is a small change in the membrane potential toward overall effect is a small change in the membrane potential toward the resting membrane potential (repolarization)the resting membrane potential (repolarization)..
Phase 2 (Plateau of the action potential):Phase 2 (Plateau of the action potential): This coincides with an This coincides with an increased permeability for Caincreased permeability for Ca2+2+. The inward movement of Ca. The inward movement of Ca2+2+ and the decreased efflux of Kand the decreased efflux of K++ maintain the membrane potential maintain the membrane potential near zero during this phase of the action potentialnear zero during this phase of the action potential..
Phase 3 (Rapid repolarization):Phase 3 (Rapid repolarization): due to a reduction of the inward due to a reduction of the inward NaNa++ and Ca and Ca2+2+ currents and a large increase in the outward K currents and a large increase in the outward K++ currentcurrent..
Phase 4 (Complete repolarization):Phase 4 (Complete repolarization): the membrane goes back to the membrane goes back to the resting level (- 90 mV). Nathe resting level (- 90 mV). Na++-K-K++ pump works to drive the pump works to drive the
excess Naexcess Na++ out and the excess K out and the excess K++ in in..
Excitability changes following an Excitability changes following an effective stimulus to contractile effective stimulus to contractile
cardiac musclecardiac muscle
Following the application of an effective Following the application of an effective stimulus to ventricular cardiac muscle, stimulus to ventricular cardiac muscle, its excitability passes by the following its excitability passes by the following
phasesphases::
The absolute refractory periodThe absolute refractory period The absolute refractory periodThe absolute refractory period::
During During the absolute refractory period,the absolute refractory period, the excitability the excitability level is 0%level is 0% . .
No stimulus however strong can produce a propagated No stimulus however strong can produce a propagated action potential in the heartaction potential in the heart . .
This period begins with sarcolemmal depolarization till This period begins with sarcolemmal depolarization till mid-repolarization ( to a membrane potential of –40 to mid-repolarization ( to a membrane potential of –40 to –50 mV)–50 mV) . .
It lasts for the whole period of systole and the early part It lasts for the whole period of systole and the early part of diastoleof diastole..
The relative refractory periodThe relative refractory period
The relative refractory periodThe relative refractory period::
During the relative refractory period the During the relative refractory period the excitability level is more than 0 but less than excitability level is more than 0 but less than 100% of the resting basal level100% of the resting basal level . .The heart responds only to stronger stimuliThe heart responds only to stronger stimuli . .
It is a short period that begins at mid-It is a short period that begins at mid-repolarization and ends shortly before complete repolarization and ends shortly before complete repolarizationrepolarization..It lasts for a short period during diastoleIt lasts for a short period during diastole..
The significance of the long absolute The significance of the long absolute refractory period of the ventricular refractory period of the ventricular
musclemuscle
It lasts for the whole period of systole and the It lasts for the whole period of systole and the early part of diastoleearly part of diastole . .
This means that the ventricle would not This means that the ventricle would not respond to any stimulus until it finishes with respond to any stimulus until it finishes with
its systole and have some diastoleits systole and have some diastole . .
So the long absolute refractory period protects So the long absolute refractory period protects the ventricle against tetnization if it receives the ventricle against tetnization if it receives multiple successive stimulimultiple successive stimuli..
ContractilityContractility
Contractility is the ability of the muscle to convert the potential energy of food into mechanical
energy.
Calcium transport across the Calcium transport across the myocardial sarcolemmamyocardial sarcolemma
There are four different ways for transport There are four different ways for transport of calcium across the myocardial of calcium across the myocardial sarcolemmasarcolemma::
Transient (T-type) calcium channelsTransient (T-type) calcium channels
Long-lasting (L-type) calcium channelsLong-lasting (L-type) calcium channels
Calcium pumpCalcium pump
NaNa++-Ca-Ca2+2+ exchanger exchanger
SARCOLEMMA
10%Mitochondria
THICKTHICKMYOFILAMENTMYOFILAMENT
THIN MYOFILAMENT
SRCa++
T-t
ub
ule
20%
80%
Excitation-contraction coupling Excitation-contraction coupling in the myocardial cellin the myocardial cell
Contraction: When the myocardial cell is excited Contraction: When the myocardial cell is excited → Na→ Na+ + influx → depolarization of the influx → depolarization of the sarcolemma → depolarization of the T-tubules sarcolemma → depolarization of the T-tubules → Ca→ Ca2+2+ influx through slow calcium channels, influx through slow calcium channels, this calcium is called depolarizing calcium → this calcium is called depolarizing calcium → release of calcium from the sarcoplasmic release of calcium from the sarcoplasmic reticulum, this calcium is called activator reticulum, this calcium is called activator calcium. → activator calcium starts contractile calcium. → activator calcium starts contractile process by binding to troponin-Cprocess by binding to troponin-C..
Excitation Contraction CouplingExcitation Contraction Coupling
Excitation contraction coupling is similar in cardiac and skeletal muscle.
Increased intracellular Ca2+ triggers contraction by binding to troponin on the thin filament.
In cardiac muscle Ca2+ comes from both the extracellular fluid and sarcoplasmic reticulum.
RelaxationRelaxation
Relaxation: Calcium is cleared from the Relaxation: Calcium is cleared from the sarcoplasm by the Nasarcoplasm by the Na++-Ca-Ca2+2+ exchanger and two exchanger and two calcium pumps, one in the sarcoplasmis calcium pumps, one in the sarcoplasmis reticulum that reuptakes calcium back into the reticulum that reuptakes calcium back into the reticulum, and another in the sarcolemma that reticulum, and another in the sarcolemma that pumps calcium out into the extracellular fluid. pumps calcium out into the extracellular fluid. The clearance of calcium from the sarcoplasm The clearance of calcium from the sarcoplasm terminates the contraction and starts the terminates the contraction and starts the relaxation processrelaxation process..
The preload and afterload of the The preload and afterload of the heartheart
During diastole, blood fills the ventricle till it reaches During diastole, blood fills the ventricle till it reaches the end-diastolic volume (EDV) before the start of the end-diastolic volume (EDV) before the start of contraction. Therefore, the EDV is called the contraction. Therefore, the EDV is called the preload of the heartpreload of the heart..
The ventricle then contracts to eject the blood against The ventricle then contracts to eject the blood against the resistance of the arterial blood pressure. the resistance of the arterial blood pressure. Therefore, the load of the arterial blood pressure is Therefore, the load of the arterial blood pressure is called the afterload of the heartcalled the afterload of the heart..
InotropismInotropism
Inotropism means an influence on Inotropism means an influence on contractilitycontractility..
A +ve inotropic factor or effect is one that A +ve inotropic factor or effect is one that increases myocardial contractilityincreases myocardial contractility..
A -ve inotropic factor or effect is one that A -ve inotropic factor or effect is one that decreases myocardial contractilitydecreases myocardial contractility..
Factors that influence Factors that influence myocardial contractilitymyocardial contractility
* *Sympathetic stimulation Sympathetic stimulation has a +ve has a +ve inotropic effectinotropic effect
* *Parasympathetic stimulation Parasympathetic stimulation has a –ve has a –ve inotropic effect on the atrial myocardium inotropic effect on the atrial myocardium only because the vagus nerves do not only because the vagus nerves do not supply the ventriclessupply the ventricles
* *The preload (EDVThe preload (EDV))::
* *Heart rateHeart rate::