The Biology of Scar Formation
-
Upload
oscar-barrios-bravo -
Category
Documents
-
view
20 -
download
0
Transcript of The Biology of Scar Formation

The Biology of Scar Formation
Scar, our body's "glue" is formed through a highly organized sequence of physiologic events. The ability of one type of collagenous tissue to weld various tissues, adapt to their structural integrity, impart tensile strength, and permit return of function is reviewed. A knowledge of wound healing enables the clinician to design and implement treatment strategies based on scar biology. The purposes of this overview are 1) to address the three phases of repair (inflammatory, fibroplastic, and remodeling), 2)to discuss the cellular processes occurring in each phase, 3)to review appropriate intervention methods based on research findings, and 4) to describe complications that interfere with normal healing. [Hardy MA: The biology of scar formation. Phys Ther 69:1014-1024, 1989]
Key Words: Cicatrix; Collagen; Hand injuries; Inflammation; Upper extremity, hand and wrist; Wound healing.
Maureen A Hardy
How We Heal
A wound, in its most basic definition, is a disruption of unity. Primitive animals respond to this threat by mitosis of their cells; that is, they are capable of regenerating exact duplicates of the missing parts. Select organs in our body still retain this biological gift of regeneration. Scratches and mild burns of the skin are healed by epidermal regeneration. Hepatocytes in the liver are capable of regrowth following mild toxic conditions. Peripheral nerves heal by axoplasm regeneration distally to restore nerve tracts. The ability of these tissue examples to regenerate or "reduplicate" their original condition is limited to minor injuries and healing under optimal conditions. Certainly, more devastating insults such as full-thickness burns, cirrhosis, and large nerve gaps overwhelm their limited regeneration potential.
Nature has provided us with another means of survival. It is an inferior method compared with regeneration, but it is the primary means of repair for all vertebrates. Special cells in our body respond to injury by forming a collagenous "glue." This body glue is called granulation scar tissue Maintenance of our well-being depends on our body's ability to sense a disruption of unity, signal the appropriate cells, and carry through the sequence of repair without complications. This review of scar biology presents an overview of how healing occurs. Certainly, each component of the repair process is an area of intense research efforts, both in the clinic and in the laboratory. Although a comprehensive treatise on each section is beyond the scope of this manuscript, the reference list will enable interested readers to pursue further information.
Scar Characteristics
How is it possible for the body's repair system to duplicate the original form and function of the injured tissue with only one type of glue? Our body structures can be divided into at least 14 different types of collagen. Mature scar is formed from type-I collagen; yet it is the greatest chameleon in its ability to imitate the structure of other collagen types. Somehow, the scar formed in dense tissue "senses" the need for strength and attempts to mimic the surrounding tissue in structure. Likewise, scar, filling a defect in loose, flexible tissue, will change in its last phase of healing to reproduce, as much as possible, these physical characteristics. Thus, in response to certain internal and external influences, scar does differentiate to become quasi-tissue-specific. Experience tells us that often this attempt by scar to blend in cosmetically and functionally is not successful. Enhancing the potential of scar to duplicate the desired outcome is the basis for surgical, pharmacological, and therapeutic management protocols.
M Hardy, MS, PT, is Director, Hand Management Center, St Dominic Hospital, 969 Lakeland Dr, Jackson, MS 39216-4699 (USA), and Instructor, School of Health Related Professions, University of Mississippi Medical Center, 2500 N State St, Jackson, MS 39216.
22/1014 Physical Therapy/Volume 69, Number 12/December 1989

The patient's wound-healing status is certainly an integral part of each initial evaluation in acute care. However, a descriptive history of how the repair progressed in a patient with well-healed scar will alert the clinician to certain potential problems. Reports of prolonged swelling, excessive skin sloughing, dramatic color or temperature changes, progressive pain, and paresthesias alert us to the presence of associated complications. The extent of wound infection or dehiscence may predict the amount of scar formed in the tissue. The duration and type of immobilization affects the mobility and stability of the scar. Underlying disease processes and pre-injury medications can influence the timing of repair.
Normal Wound-Healing Phases
All forms of trauma, to any tissue, anywhere in the body, signal the reparative sequence to begin. The sequence of events is highly organized and predictable. One process is stimulated to begin, and its completion in turn signals another cellular response until the wound is bridged by scar. The ultimate goal in collagen research may be the discovery of healing without scar formation. Until then, to prevent scar formation is to prevent healing.
The response to injury, either surgically or traumatically induced, is immediate. The wound then passes through three phases toward final repair: 1) the inflammatory phase, 2) the fibroplastic phase, and 3) the remodeling phase. The inflammatory phase prepares the area for healing, the fibroplastic phase rebuilds the structure, and the remodeling phase provides the final form.
Timetables for the beginning and end of each phase must be understood as general guides. Different tissues heal at different rates, and even one wound can show various areas healing rapidly or slowly.
At what point is healing complete? This question is important in determining return to work, the timing of
further surgical intervention, and permanent impairment ratings. Knowledge regarding injury time frames combined with objective appraisal of the scar give us our best basis on which to make these decisions.
Inflammatory Phase
Inflammation is a normal and necessary prerequisite to healing. Changes in vascular flow are responsible for the clinical symptoms we use to detect an inflammatory response. The majority of the specialized cells involved in this phase of the wound-healing process come from our blood. Obviously, any blood vessels that traversed the wound were cut at the time of injury. These cut vessels poured whole blood into the wound, which then coagulated, sealing off the injured vessels and lymphatic channels, thus temporarily closing the wound.
In addition to this direct blood vessel injury, noninjured vessels dilate in response to chemicals released from injured tissues. Most cells in injured tissue release histamine. Histamine causes brief vasodilation in neighboring noninjured vessels. This combination of whole blood exudate and serous transudate creates a reddened, hot, swollen, painful environment.
Bradykinins, derived from plasma in the area of the injury, contribute to more prolonged vascular permeability. Prostaglandins, produced by all cells in the body, are released with any breach of cell membrane integrity. Certain prostaglandins further contribute to long-term vascular vasodilation. The fibrin plugs that clotted in the wound also form in the lymphatic vessels. Lymphatic flow is blocked to seal off the wound and prevent the spread of infection. These channels do not reopen until later in the healing process.1
The mast cells also release hyaluronic acid and other proteoglycans into the wound milieu, which bind with the watery wound fluid to create a gel.2
This gel then does not flow. The inflammatory edema fills all spaces in
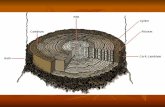
the wound and surrounds all damaged or repaired structures, binding them all together as one unit, or one wound (Figure 1A). This type of edema causes loss of dermal fat, thus thinning normal skin in the area.3
This thinning of normal skin is hypothesized to be the cause of the clinical condition of fingertip "pencil pointing" that occurs following chronic edema conditions.
That some swelling in a wound is inevitable and needed is a fact. Yet a balance is needed. If there is no inflammation, healing does not begin. If too little inflammation occurs, healing is slow. If too much inflammation occurs, excessive scar is produced.
This inflammatory fluid, derived from the blood, is high in fibrinogen.4
Fibrinogen coagulates in the wound and in the surrounding tissues that are now fluid filled. The coagulated gel will later mature into a dense, binding scar (Fig. 1B). Excessive swelling, therefore, must not be permitted. Primary wound care ensures that all blood vessels have been repaired, cauterized, or clotted. Hematomas, the result of ongoing bleeding in the wound, create extra exudate, a powerful stimulus to scar formation.5 Secondary wound care addresses the contribution made by induced vasodilation, which continues in relation to the severity of the wound. This serous transudate can be diminished by the classic "RICE" regimen of rest, ice, compression, and elevation. Pharmacological use of steroids and aspirin affects the transuda-tive edema.6 Their action aids in inhibiting prostaglandin release. All wounds, and even controlled surgical procedures, require edema care. Ward showed that the use of a tourniquet in hand surgery significantly increased hand edema, as compared with controls, as long as one month postoperatively.7
Excessive inflammatory fluid also affects joint positioning. Eyring and Murray performed joint distention studies by infusing saline in normal hands.8 They found that each joint responds to swelling by assuming a
Physical Therapy/Volume 69, Number 12/December 1989 1015/23

Fig. 1. Resolution of repair: (A) Shaded area represents fluid edema bathing all injured tissues; (B) the wound fluid has coalesced into one scar binding all tissues; (C) scar absorption and reorganization has occurred through successful remodeling.
predictable position to lessen tension on joint receptors. The patient with a swollen hand characterized by a "dropped" wrist, extended metacarpophalangeal (MP) joints, flexed inter-phalangeal (IP) joints, and adducted thumb posture confirms their findings. Young et al9 and deAndrade et al10 demonstrated further that swelling in a joint causes joint receptors to fire in a biased manner. They facilitate muscle action that draws the joint into the "comfortable" position and neuro-logically inhibit antagonistic muscles. These findings imply that hands in this phase need to be supported and positioned correctly through the use of external dressings and splints. Active exercise may be disadvantageous during this phase unless the edema is first reduced, thus removing the inhibitory effect of distended joint receptors.
For healing to commence, two prerequisite events must occur: l)The wound must be decontaminated
(phagocytosis), and 2) a new blood supply (neovascularization) must then be available. Each of these processes will be described.
Phagocytosis. Within blood vessels adjacent to the wound, white blood cells begin to stick to the dilated endothelial walls.11 Chemical changes in the wound induce and attract these cells to slip through the enlarged capillary pores and migrate to the site of injury. Anti-inflammatory steroids also act at this point by inhibiting the amount and mobility of white blood cells.
The main purpose of this portion of the phase is to prevent or rid the wound of infection. All wounds, even under meticulous sterile conditions, are contaminated. Fortunately, our system of defense is adequate to prevent minor contamination from developing into a major infection. Certain conditions can tip the scale in favor of infection developing: the type of bac
teria present, presence of foreign objects, necrotic tissue, poor oxygen supply, malnutrition, certain vitamin deficiencies, radiated tissues, and immunosuppression.
The first white blood cells to reach the wound are polymorphonuclear leukocytes. These short-lived cells begin the process of phagocytosis by fixing to bacteria, extending their membrane around them, then enzy-matically dissolving and digesting the invaders. In a few days, another type of phagocyte will predominate and remain in the wound until all signs of inflammation cease. This cell, the macrophage, has two important roles in the process of repair.12 First, it continues the important job of phagocytosis. Second, the macrophage has been termed the "director cell" of repair because of its influence on scar production. As a scavenger cell, the macrophage not only attacks and engulfs bacteria but also disposes of necrotic tissue in the wound. It is capable of phagocytosing in poorly nourished tissues with low oxygen levels or can consume oxygen at over 20% of the basal rate for enhanced phagocytosis. Because ischemic tissues are more prone to infection than normal tissues, the oxygen tension of the wound is a critical factor. Maintenance of an adequate arterial oxygen supply for optimum phagocytosis is dependent on sufficient blood volume and percentage of atmospheric oxygen breathed, as opposed to local, topically applied oxygen.13
As macrophages ingest microorganisms, they also excrete products of digestion. Ascorbic acid, hydrogen peroxide, and lactic acid are byproducts of phagocytosis. Hydrogen peroxide aids in controlling anaerobic microbial growth. Ascorbic acid and lactic acid are believed to be the substances that signal the extent of damage.14 Build-up of these acids is interpreted as a need for assistance from more macrophages. More macrophages produce more by-products. The net result of an increased macrophage population is a more intense and prolonged inflammatory response.
24/1016 Physical Therapy/Volume 69, Number 12/December 1989

The significance of these findings is twofold. First, the fact that most wounds heal without infection is a credit to the microbicidal capacity of the potential macrophage population. Second, chronically activated macrophages create a chronically inflamed wound.15
Clinically, we can potentially mitigate this process by assisting the macrophage in its work. Studies have confirmed the use of low-dosage, pulsed ultrasound in water baths significantly decreases infection.1617 Hunt and Van Winkle point out that ultrasound agitation is capable of disintegrating macrophages.11 Their debris may then signal more phagocytic cells to the infected area. Removal of all foreign materials, debridement of necrotic tissue, evacuation of hematomas, use of antibiotics, use of wet-to-dry dressings as a form of microdebridement, and frequent whirlpool cleaning will result in a clean wound bed that is ready for healing. Once this condition exists, the inflammatory phase is over.
Another cell type (the fibroblast) will soon respond to the chemical signals issued from the macrophage. Our body must evaluate the extent of the wound in order to mobilize a sufficient number of repair cells. The macrophage thus "directs" the future course of repair by chemically influencing the number of fibroblastic repair cells activated. A local platelet-derived growth factor released from platelets during clotting and from macrophages signals fibroblasts.18
Topical administration of this growth factor is being used to enhance cellular activity in chronic, nonhealing wounds.19 Conversely, use of steroids inhibits the macrophage level, resulting in lack of wound debridement and a delay in scar production.12
The macrophage has been described as a key factor in regulating events in this inflammatory period. Its presence is vital as a phagocytic agent and appraiser of damage. Its role in recruiting fibroblasts is significantly related to the final amount of scar produced.
Neovascularization. The inflamma-tory response so far has proceeded without any new regrowth of blood vessels. Healing will not proceed unless new, functioning blood vessels are present to supply oxygen and nourishment to the injured tissue. Hunt and Van Winkle's statement that "as neovascularization goes, so goes the wound,"11(P14) emphasizes the importance of this phase. Once again, it is suspected that the macrophage may signal this vascular regeneration to begin.
Patent vessels in the wound periphery develop small buds or sprouts that grow into the wound area, probably directed by ischemia.20 These outgrowths will eventually come in contact with and join other arteriolar or venular buds to form a functioning capillary loop. These new circulatory loops fill the wound, creating a highly pink to reddish color throughout the one wound. The young wound will remain redder in contrast to the normal adjacent tissues throughout healing because of this inundation of capillary loops. Areas that remain gray in appearance or have a delayed blanch test following pressure show inadequate circulation. As the wound approaches final maturity, an unknown signal causes the majority of loops to cease functioning and retract. Thus, a fully matured scar appears whiter than adjacent tissue. The color of scar, therefore, is an excellent prognostic guide as to the potential for further changes in scar characteristics.
The capillary sprouts, when first formed, lack full thickness, which renders them delicate and easily disrupted. Immobilization is essential during this phase to permit vascular regrowth and prevent new microhem-orrhages. Lotz et al's study of the effect of early shoulder motion in the inflammatory phase following mastectomy showed increased serous collection, wound breakdown, and infection as compared with controls.21 They concluded that early motion protocols should commence at the completion of this phase. Paletta et al's work showed that heat application during
this portion of the phase will cause increased bleeding from these fragile vessels and is therefore contraindicated.22
As this phase comes to a close, fibrin-olysin from blood vessels is produced to assist in dissolving clots. The lymphatic channels open to assist in reducing the wound edema.
Reviewing the complex, interrelated dynamics that have occurred in this first phase would lead one to believe that weeks must be necessary for completion. In normal conditions, all these events happen within the first four days after injury.11 Complications, major injuries, and secondary trauma elsewhere in the body can prolong the inflammatory period. Our main directive is to minimize all factors that can prevent or prolong inflammation. Treatment is directed toward assisting the role of the macrophage through the use of antibiotics, debridement, wound cleaning, RICE regimen, and proper positioning.
Fibroplastic Phase
With the inflammatory phase completed, rebuilding can commence. This phase is named for the primary cell of scar production—the fibroblast. Although many different cells are involved in the inflammatory phase, fewer types of cells operate in the fibroplastic phase; their work will last about three weeks. The purpose of this phase is to resurface and impart strength to the wound.
Fibroblasts originate from mesenchymal cells located in loose tissue around blood vessels and fat. In response to chemotactic influence from the injury, these precursors of the fibroblast transform into cells with migratory ability. These migratory fibroblasts follow the fibrin meshwork created earlier in the wound fluid milieu. Because the wound fluid bathed all injured structures, the fibroblast has access to all depths of the wound. Once in place, the fibroblast is ready to begin its synthesis of the collagen molecule. Three processes occur
Physical Therapy/Volume 69, Number 12/December 1989 1017/25

simultaneously in this phase to achieve coalescence and closure: l)epithelialization, 2) wound contraction, and 3) collagen production.
Epithelialization. There is a priority of nature inherent in healing. Factors critical to survival such as phagocytosis, blood flow, and surface covering occur early in healing. The body "knows" invading organisms are from the outside environment. Providing even a one-cell layer of its own covering will reduce the chances for infection. A protective barrier will further aid healing by preventing loss of fluid from the wound.
Within hours after injury, undamaged epithelial cells at the wound margin begin to reproduce. It is hypothesized that the stimulus for this epithelial mitosis is a loss of restraint that cells in contact exhibit over each other.23
This accelerated reproduction causes a ridge to form around the periphery. The new cells are true epithelial cells; therefore, this is a regeneration process.24 Surviving epidermal structures such as hair shafts and sweat glands also give rise to epithelial mitosis. If the wound bed is viable and good blood supply available, then migration of these new cells begins, with those from the periphery moving in and those from appendages moving out. These migratory cells remain attached to their parent cells; therefore, their movement causes a "pull" on the normal skin around the wound edge. The advancing edge of the epithelium seeks out moist, oxygen-rich tissue. Dressings, kept moist and not permitted to dry out, will facilitate this migration. If allowed to dry, the dressings will adhere to this thin skin, and removal will result in microdebridement of this healing tissue.2
Should the epithelial edge meet eschar, foreign material, sutures, or blood clots, it will dive downward to maintain contact with the vascular-loop network in the wound. The epithelial margin must release lytic enzymes, which act to cleave the attachments of nonviable tissue from the viable wound bed. As it gradually
undermines, the eschar loosens and detaches from the wound. A red, highly vascular wound with a thin, almost transparent covering is now visible. It is believed that the scab forms a temporary barrier for the wound and should not be disturbed until epithelialization is complete. If the necrotic tissue or the wound is too extensive or oxygen availability is poor, epithelial migration cannot proceed. Some investigators claim beneficial effects of local application of oxygen in accelerating the migration process,11 but further research is needed to validate this claim. If sufficient capillary circulation is not available to maintain epithelial integrity, wound dehiscence can occur.25
When epithelial cells from one direction meet similar migratory cells, contact inhibition causes cessation of movement. Although clean, approximated wounds are clinically resurfaced within 48 hours, larger, open wounds require a longer period. Several weeks are required for this thin covering to become multilayered and to differentiate into the various strata of normal epidermis. The thickening process of skin healing is called intus-susceptive growth. Skin healed in this manner, however, never truly develops a full basal layer of cells and will always be thinner in appearance.26
Epithelialization can be facilitated by maintaining moist dressings, protecting the wound from minor repetitive trauma, avoidance of chemical irritants or infection, debridement, and possibly topical oxygen therapy.27
Wound contraction. There is another force at work aimed at closing the wound. Unlike epithelialization, which closes the wound surface, contraction is a process that actually pulls the entire wound together, in effect shrinking the defect. Successful contraction results in a smaller wound to be repaired by scar formation. Minimizing the area to be healed is truly beneficial in certain tissues with fixed, deep structures covered by mobile, loose skin, such as on the abdomen or gluteal area. Wound contraction, however, may be harmful in the hand. The close interplay of multi
ple joints, muscles, tendons, and sheaths all joined by fascial connections requires every millimeter of skin and tissue length. Permitting an open wound on the hand to heal by uncontrolled contraction is inviting trouble. If contraction occurs, the centripetal force will pull all structures toward the wound. Joint contractures, as sometimes seen in full-thickness hand burns, are often the result of uncontrolled wound contraction.
Wound contraction begins about four days postinjury. If the wound is not closed by 14 to 21 days postinjury, contraction stops because of the restraint of the surrounding stretched tissue. This phenomenon is an active event dependent on an active cell. This specialized cell was identified in 1971 by Gabbiani et al28 and named a myofibroblast. The myofibroblast is derived from the same blood vessel adventitia and fat cells as are fibroblasts. The difference is that these cells contain the contractile properties of smooth muscle cells. The myofibroblasts attach to the skin margins and pull the entire epidermal layer inward. These unusual cells have been identified in other conditions associated with a contraction process, such as Dupuytren's contracture, tenosynovitis, and hypertrophic scars, and in fibrous capsules formed around implants.29
The "picture-frame theory" identifies the wound margin beneath the skin as the location of myofibroblast action.30 A ring of these contractile fibroblasts convene near the wound perimeter, forming a "picture frame" that will move inward, decreasing the size of the wound. Although contractile forces start out equal in all wounds,31 the shape of the picture frame predicts the resultant speed of contraction: Linear wounds contract rapidly, square or rectangular wounds contract at a moderate pace, and circular wounds contract slowly.32
Because contraction in the hand results in deformities, the goal should be inhibition of wound contraction. Approximated and sutured wounds minimize the need for contraction
26/1018 Physical Therapy/Volume 69, Number 12/December 1989

forces, but not all wounds can be closed primarily. Studies have shown that contraction is diminished through the use of skin grafts.33,34 The thickness of the graft correlates with the degree to which contraction is suppressed. Split-thickness grafts diminish contraction of the wound bed by 31%; full-thickness grafts diminish contraction by 55%. The early combined use of full-thickness grafts with splinting inhibits contraction by 77%. Rudolph points out that grafts must be applied early, in the inflammatory phase before contraction is initiated.35
If the myofibroblasts are already mobilized and functioning, then excision of the wound margins prior to graft application is necessary to prevent contraction from occurring beneath the graft.
Collagen production. The climax of wound healing occurs with collagen production. If this event does not occur, the wound will not heal. Migratory fibroblasts are now present throughout the wound. The wound environment is responsible for stimulating the fibroblasts to synthesize and secrete collagen. As described earlier, the build-up of lactic acid will influence the amount of collagen produced. Adequate supplies of oxygen, ascorbic acid, and other cofactors such as zinc, iron, and copper are needed to create the proper background for fibroplasia. Having its metabolic needs met for nutrients, the fibroblast synthesizes three polypeptide chains. These chains coil to form a right-handed helix. These spiraled chains, now called procollagen, are then extruded from the fibroblast out into the extracellular space. Once exocytosed, the triple-helical molecule undergoes cleavage at specific terminal sites. The helix is now called a tropocollagen molecule. Tropocolla-gens spontaneously associate in an overlapping array. The amassing continues as tropocollagen convolves with other tropocollagen molecules to form a collagen fibril (Fig. 2).
These filaments lay disorganized in the wound, still in a gelatinous state. The amount of collagen filaments formed does not build strength..
Fig. 2. Collagen aggregation from one helical filament amassing with others to form fibrils and collagen fibers.
Wound durability, or tensile strength, is dependent on the microscopic welding that must occur within each filament and from one filament to another. These sites of bonding are called cross-links.
Initially, weak electrostatic forces aid in attracting and holding the three chains together at the procollagen stage. These ionic charges together with early hydrogen bonds keep the molecule weakly stable. Salt water application, vibration, heat, and enzymes can easily denature and separate the chains. With further maturation into tropocollagen, the chains change at specific sites to permit stronger cross-links to form. Covalent bonds are now in place, which enhance stability but remain soluble.36
These cross-links are called intramolecular cross-links because they occur within a single tropocollagen molecule (Fig. 3A).
Intermolecular bonds form from one tropocollagen molecule to another (Fig. 3B). They are the major force holding tropocollagen filaments together, thus imparting tensile strength to the wound. The number of intermolecular bonds formed will enhance the strength of the filament. Bone tissue has the highest ratio of intermolecular bonds, and this dense connective tissue can be considered highly cross-linked. Figure 4 depicts a clear solution of collagen in a beaker. The rigid, opaque gel on the plate is also collagen. The only difference
Physical Therapy/Volume 69, Number 12/December 1989 1019/27

Fig. 3 . Collagen bonding increases tensile strength: (A) Weak intramolecular crosslinks form between amino acid chains within one collagen filament; (B) stronger inter-molecular cross-links form from one collagen filament to another.
between the two is in their degree of cross-linkage.37
The fibroblast also synthesizes gly-cosaminoglycans (GAG), which fill in the space between and around collagen fibers.38 This GAG ground substance, combined with water, provides lubrication and acts as a spacer between moving collagen fibers. Ake-son et al have shown that immobilization causes a loss of ground substance.39 When this important buffer interface is diminished, new cross-links are formed, rendering mobile tissue immobile. It is believed that the composition of this nonfi-brous substance is also related to the amount and location of cross-links formed. Thus, a relationship between GAG ground substance and collagen dictates scar architecture.
The wound at the end of this three-week time frame has the greatest mass of collagen assembled, but the
tensile strength is roughly only 15% of normal.40,41 A bulky, rough, tender, red scar is visible and palpable. The formation of cross-links in this phase allows the wound to tolerate early, controlled motion without fear of disruption. Wounds are bidirectional at this time; under optimal healing circumstances, they proceed to the next phase, but complications can cause a recurrence of inflammation. Edema, infection, and rough handling can cause the wound to become rein-flamed. Mobilization aimed at breaking scar will create a new wound, ultimately with further scar formation.42 A secondarily inflamed wound results in collagen deposition in addition to that already present.
The quantity of scar produced at this time is an indication of final outcome. Brand summarizes this point as follows: "The amount of scar to be remodeled is inversely related to the return of function."43
Remodeling Phase
Successful wound healing requires more than closing the wound with sufficient tensile strength. The ultimate goal is the return of function. Remodeling requires the scar to change to fit the tissue. Repaired ligaments must have firm, intransigent scar formed with a parallel weave in order to resist deforming joint forces during stretching activities, yet the scar fibers must pleat with relaxation when tension is removed. Just millimeters away, however, the scar formed between ligaments and bone or moving parts must have a random orientation of scar fibers, with thin and lengthy adhesions to permit motion between parts. Wound repair is optimal when this remodeling of scar tissue occurs and less than optimal when it does not occur. The process of scar remodeling, which is not fully understood, is responsible for the final aggregation, orientation, and arrangement of collagen fibers.
Several factors assist in the maturation and final physical characteristics of the scar. The influence of synthesis-lysis balance and fiber orientation will be described as they relate to the remodeling scheme.
Synthesis-lysis balance. Despite the fact that collagen synthesis continues at a high rate, no further increase in scar mass occurs. In adults, the tissues are in a steady state; that is, they make new collagen and break down old collagen in a balanced fashion.
Inflammation from injury causes hormonal stimulation for increased collagen destruction by the enzyme colla-genase. Collagenase is derived from polymorphonuclear leukocytes, the migrating epithelium, and the wound granulation bed.44 It is a pervasive enzyme found also in rheumatoid synovial cells, bone, and postpartum uterine tissues. Collagenase is capable of cleaving the strong cross-links in the tropocollagen molecule. Breaking the bonds causes the molecule to become soluble and excreted from the body as waste by-products.45 Col-
28/1020 Physical Therapy/Volume 69, Number 12/December 1989

Fig. 4- Beaker of clear collagen solution and rigid collagen gel produced as result of collagen bonding. (Reprinted with permission from Peacock EE. Production and polymerization of collagen in healing wounds of rats: Some rate-regulating factors. Ann Surg 155251-257, 1962.)
lagenase action is highest at the site of injury.
Studies on fascial wounds have revealed that not only does the area of injury experience this accelerated synthesis-lysis process, but neighboring, noninjured tissues are also affected, although to a lesser degree.46
This finding explains why an injured hand, held immobile throughout all three phases, can have multiple contractures in injured and noninjured structures alike. Merritt's statement that "the hand is an organ; if one part is injured, the entire organ suffers"47
reminds us that a fundamental principle of hand management is to keep all noninjured structures normal throughout the repair process.
Synthesis is oxygen dependent, whereas lysis is not.11 This fact becomes important when the balance between the two processes is abnormal. Hypertrophic scar and keloids are examples of normal synthesis following wounding combined with a genetic inhibition of lysis. We can restore the balance in hypertrophic
scarring by the application of pressure to the scar. Prolonged pressure renders an ischemic condition. With lowered oxygen tension, synthesis is depressed, whereas lysis continues.48
Eventually, balance is achieved when scar bulk is flattened to approximate normal tissue. This pressure treatment must be continued until remodeling is complete and all collagen turnover returns to a normal level.
Collagen synthesis and lysis are in balance with each other in a normal wound, even though both rates are higher than preinjury rates. Collagen turnover is accelerated as old fibrous tissue is removed and new fibrous tissue is formed. This process continues until the remodeling phase ends at six months to a year postinjury, depending on the extent of the injury. The high rate of collagen turnover in this phase can be either beneficial or detrimental. As long as the scar exhibits a rosier appearance than normal, remodeling is underway. If joints and tissues can lose mobility quickly, they can also regain it quickly with proper management.
Collagen fiber orientation. During remodeling, collagen turnover allows the randomly deposited scar tissue to be rearranged, in both linear and lateral orientation. The "one-wound concept" of similar scar found throughout the wound is resolved (Fig. 1C). Two important questions must be addressed: 1) How does a change in scar orientation change tissue function? and 2) What forces direct the alignment of the collagen fibers?
The first question can be answered with a common household example. Scar is nonelastic.49 A Slinky* toy is made from nonelastic metal. Its spiral shape allows it to expand and contract with play. Scar that forms with redundant folds will permit mobility of the structures to which it is affixed. Seyfer and Bolger used a scanning electron microscope to visualize the form of adhesions that affect tendon gliding.50 They found that gliding tendons had lengthy, elongated adhesions, like a Slinky, whereas restricted tendons had short, dense adhesions. The physical weave of the collagen fibers is largely responsible for the final functional behavior of the wound.
What forces are at play to direct this collagen realignment? Two theories are given regarding these forces: 1) the induction theory and 2) the tension theory. The induction theory hypothesizes that scar attempts to mimic the characteristics of the tissue it is healing. The tissue structure induces the collagen weave.51 Thus, dense tissues induce dense, highly cross-linked scar; pliable tissues induce a loose, coiled, less cross-linked scar. Scar can adapt through the remodeling forces of synthesis and lysis. Dense tissues seem to have preference or greater influence when multiple tissue types are found in close proximity. Using principles inherent in the induction theory, the surgeon attempts to design the repair field by separating dense and soft tissues.43 Tendon repairs left immobile over bone fractures will ultimately resolve into bony adhesions encasing the nongliding tendon. *James Industries, Inc, PO Box 230, Hollidaysburg, PA 16648.
Physical Therapy/Volume 69, Number 12/December 1989 1021/29

When repair sites cannot be separated by hand positioning, sequencing of repair, or interposition of fat and areolar tissues, then early controlled-movement protocols are beneficial.43
The tension theory refers to internal and external stresses that affect the wound area during the remodeling phase. Muscle tension, joint movement, passive gliding of fascial planes, soft tissue loading and unloading, splinting, temperature changes, and mobilization are all examples of forces acting on the collagen array. The tension theory was given validity by the work of Arem and Madden.52
The results of their study confirmed that a physical change of scar length could be achieved through the application of stress during the appropriate healing phase (Fig. 5). They found that two variables were most responsible for successful remodeling: the phase of the repair process when forces are introduced and low-load-long-duration application of stress.
The clinical implication is that stretching scar achieves only a temporary lengthening. Permanent elongation of scar requires long-duration application of stress for scar tissues to remodel to the new position.53
Dynamic splints, serial casting, positional heat and stretching techniques, functional electrical stimulation, and selective hand activities are examples of methods used to achieve the low-load-long-duration stress necessary to change scar configuration.
Other studies have demonstrated that the application of tension causes an increase in tensile strength during healing.54-62 Fascia,55 skin,56 tendon,57
ligament,58 cartilage,59 capsule,60 and bone61 have all been shown to lose tensile strength and normal collagen array with immobilization and stress deprivation. The recovery curves for tissue experimentally immobilized for two to four weeks reveals that reversibility requires months to complete and often is never fully successful.62
Fig. 5. Appearance of three-week-old scar following four weeks of tension. Upper sponge pair from unstressed control side; lower sponge pair from stressed side. (Repri ed with permission from Arem and Madden.52)
Remodeling factors. Pharmacologi-cal manipulation of scar seeks to alter metabolism at specific sites. Changing the wound chemistry, selectively inhibiting or enhancing synthesis-lysis, and controlling cross-linking are areas of intense research.63,64 These advances remain limited in clinical application because of their generalized effect on normal and healing tissues.
Controlling the amount and location of scar can be addressed, to a limited degree, by gentle inspection of the wound, planned surgical procedures, and rational postoperative care. The current clinical advances in tissue remodeling are taking place in controlled-motion protocols. Each type of tissue depends on some type of stress for its functional integrity. The goal during the remodeling phase is to reintroduce a controlled stress as the scar matures, in an attempt to influence scar formation.
Tendon and ligament repairs are held immobile for two to three days during the inflammatory phase, and controlled motion is then initiated.57,58
Controlled, or protective, restrictive
motion is used so as not to disrupt the repair or incite inflammation, yet permit forces through the tissue and wound bed. In both types of tissue, a dense, parallel union of scar to tissue is the desirable outcome.
Silastic† rods used in two-stage tendon reconstruction depend upon the induction theory of remodeling to form a smooth-surfaced scar around the entire length of the rod.65 When the rod is removed, the hand has a new scar tunnel ready to accept a tendon graft.
Joint implants in the hand enable us to remodel the new scar formed around the implant as close to normal capsule architecture as possible.66
Through splinting forces, positioning, and selective exercises, tension is exerted on the dorsal and volar sides of the capsule, which requires redundancy for movement into flexion and extension. The lateral sides of the new scar capsule are permitted to form denser scar to resist deviation deformities.
Even in the area of nerve regeneration, we are concerned with remodeling. Bora et al demonstrated that gentle tension over time results in a repair site that is stretched and taut †Dow Corning Corp, Midland, MI 48640.
30/1022 Physical Therapy/Volume 69, Number 12/December 1989

but that will respond by increasing its cross-sectional area.67 The nerve can then be stretched again and the stretched position maintained until the scar and tissues around the nerve remodel. Over six weeks of gradual repositioning, the subject in Bora et al's study was able to achieve full limb mobility without jeopardizing the repair.
Summary
These examples show that a knowledge of wound healing and repair enables the clinician to design and implement treatment regimens based on scar biology. Understanding the sequence of repair permits flexibility in management as the wound changes. Adverse reactions and complications should be recognized and addressed.
Weber and Davis have defined hand therapy based on scar biology as follows: "Hand therapy is behavioral modification of the fibroblast during the healing response. "68(P529) HOW to apply the correct stress to the correct tissue at the correct time is the "behavioral modification" of scar that we strive to achieve.
References
1 Asboe-Hansen G, Dyrbye MO, Moltke E, et al: Tissue edema: A stimulus of connective tissue regeneration. J Invest Dermatol 32:505-507, 1959 2 Cocke WM, White RR, Lynch DJ, et al: Wound Care. New York, NY, Churchill Livingstone Inc, 1986 3 Houck JC, Jacob RA: The chemistry of local dermal inflammation. J Invest Dermatol 36:451-456, 1961 4 Witte CL, Witte MH, Dumont AE: Significance of protein in edema fluid. Lymphology 4:29-31, 1971 5 Cohen IK: Complications of wound healing. In Greenfield L (ed): Complications in Surgery and Trauma. Philadelphia, PA, J B Lippincott Co, 1984, pp 3-8 6 Arvidsson RP, Eriksson E: A double-blind trial of NSAID versus placebo during rehabilitation. Orthopedics 10:1007-1013, 1987 7 Ward CM: Oedema of the hand after fasciec-tomy with or without tourniquet. Hand 8:179-185, 1976 8 Eyring EJ, Murray WR: The effect of joint position on the pressure of intra-articular effusion. J Bone Joint Surg [Am] 46:1235-1241, 1964
9 Young A, Stokes M, I l e s JF: Effects of joint pathology on muscle. Clin Orthop 219:21-27, 1987 10 deAndrade JR, Grant C, Dixon ASJ: Joint distension and reflex muscle inhibition in the knee. J Bone Joint Surg [Am] 47:313-322, 1965 11 Hunt TK, Van Winkle W: Wound Healing: Normal Repair—Fundamentals of Wound Management in Surgery. South Plainfield, NJ, Chir-urgecom, Inc, 1976 12 Leibovich SJ, Ross R: The role of the macrophage in wound repair. Am J Pathol 78:71-91, 1975 13 Mathes S: Roundtable discussion: Problem wounds. Perspectives in Plastic Surgery 2:89-120, 1988 14 Rutherford RB, Ross R: Platelet factors stimulate fibroblasts and smooth muscle cells quiescent in plasma serum to proliferate. J Cell Biol 69:196-203, 1976 15 Ryan GB, Spector WG: Macrophage turnover in inflamed connective tissue. Proc R Soc Lond [Biol] 174:269-292, 1970 16 Schoenbach S, Song I: Ultrasound debridement: A new approach in the treatment of burn wound. Plast Reconstr Surg 66:34-37, 1980 17 Nichter L, Williams J: Ultrasonic wound debridement. J Hand Surg [Am] 13:142-146, 1988 18 Pierce GF, Mustoe TA, Senia RM, et al: In vivo incisional wound healing augmented by PDGF and recombinant c-sis gene homodimeric proteins. J Exp Med 167:975-987, 1988 19 Knighton DR, Fiegel VD, Austin LL, et al: Classification and treatment of chronic nonhealing wounds: Successful treatment with autologous platelet-derived wound-healing factors. Ann Surg 204:322-330, 1986 20 Ryan G, Majno G: Inflammation. Kalamazoo, MI, Upjohn Co, 1977 21 Lotz M, Duncan M, Gerber L: Early versus delayed shoulder motion following axillary dissection. Ann Surg 193:288-295, 1981 22 Paletta FX, Shehadi SI, Mudd JG: Hypothermia and tourniquet ischemia. Plast Reconstr Surg 29:531-538, 1962 23 Carter SB: Principles of cell motility: The directional control of cell movement. Nature 208:1183-1187, 1965 24 Bryant WM: Wound healing. Ciba Found Clin 29(3):3-6, 1977 25 Carrico TJ, Mehrhof AI, Cohen IK: Biology of wound healing. Surg Clin North Am 64:721-733, 1984 26 Douglas DM, Forrester JC, Ogilvie RP: Physical characteristics of collagen in the later stages of wound healing. Br J Surg 56:219-222, 1969 27 Borges AF, Larrabee WF: Controversies in wound management. American Journal of Cosmetic Surgery 3:5-9, 1986 28 Gabbiani G, Ryan G, Majeno G: Presence of modified fibroblasts in granulation tissue and their possible role in wound contraction. Experientia 27:549-550, 1971 29 Guber S, Rudolph R: The myofibroblast. Surg Gynecol Obstet 146:641-649, 1978 30 Watts GT, Grillo HC, Gross J: Studies in wound healing: II. The role of granulation tissue in contraction. Ann Surg 148:153-160, 1958
31 Grillo HC, Watts GT, Gross J: Studies in wound healing: I. Contraction and the wound contents. Ann Surg 148:145-152, 1958 32 McGrath MH, Simon RH: Wound geometry and the kinetics of wound contraction. Plast Reconstr Surg 72:66-73, 1983 33 Sawhney CP, Monga HL: Wound contraction in rabbits and the effectiveness of skin grafts in preventing it. Br J Plast Surg 23:318-321, 1970 34 Stone PA, Madden JW: Biological factors affecting wound contraction. Surg Forum 26:547-548, 1975 35 Rudolph R: Contraction and the control of contraction. World J Surg 4:279-287, 1980 36 Peacock EE, Van Winkle W: Structure, synthesis, and interaction of fibrous protein and matrix. In Peacock EE, Van Winkle W (eds): Wound Repair. Philadelphia, PA, W B Saunders Co, 1976, pp 145-203 37 Peacock EE: Production and polymerization of collagen in healing wounds of rats: Some rate-regulating factors. Ann Surg 155:251-257, 1962 38 Dingman RO: Factors of clinical significance affecting wound healing. Laryngoscope 83:1540-1544, 1973 39 Akeson WH, Amiel D, Mechanic GL, et al: Collagen cross-linking alterations in joint contractures: Changes in the reducible cross-links in periarticular connective tissue collagen after nine weeks of immobilization. Connect Tissue Res 5:15-19, 1977 40 Howes EL, Harvey SC: Strength of healing wounds in relation to holding strength of catgut suture. N Engl J Med 200:1285-1291, 1929 41 Levenson S: Practical applications of experimental studies in the care of primary closed wounds. Am J Surg 104:273-282, 1962 42 Cummings G: Selection of Treatment of Soft Tissue Contractures. Atlanta, GA, Stokes-ville Publishing Co, 1982, vol 2 43 Brand PW: Drag. In Brand PW (ed): Clinical Mechanics of the Hand. St Louis, MO, C V Mosby Co, 1985, pp 61-87 44 Riley WB, Peacock EE: Identification, distribution and significance of a collagenolytic enzyme in human tissues. Proc Soc Exp Biol Med 124:207-210, 1967 45 Peacock EE: Collagenolysis: The other side of the equation. World J Surg 4:297-302, 1980 46 Merritt WH, Peacock EE, Chvapil M: Studies on the inductive capacity of canine fascia lata. Surg Forum 26:553-554, 1975 47 Merritt WH: Complications of hand surgery and trauma. In Greenfield L (ed): Complications in Surgery and Trauma. Philadelphia, PA, J B Lippincott Co, 1984 48 Hunt TK, Dunphy JE: Wound Healing: Disorders of Repair—Fundamentals of Wound Management in Surgery. South Plainfield, NJ, Chirurgecom, Inc, 1976 49 Peacock EE: Some biochemical and biophysical aspects of joint stiffness: Role of collagen synthesis as opposed to altered molecular bonding. Ann Surg 164:1-12, 1966 50 Seyfer AE, Bolger WE: Effects of unrestricted motion on healing: A study of posttraumatic adhesions in primate tendon. Plast Reconstr Surg 83:122-128, 1989 51 Madden JW: Wound healing: The biological basis of hand surgery. Clin Plast Surg 3:3-11, 1976
Physical Therapy/Volume 69, Number 12/December 1989 1023/31

52 Arem AJ, Madden JW: Effects of stress on healing wounds: I. Intermittent noncyclical tension. J Surg Res 20:93-102, 1976 53 Light KE, Nuzik S, Personius W, et al: Low-load prolonged stretch vs. high-load brief stretch in treating knee contractures. Phys Ther 64:330-333, 1984 54 Mason ML, Allen HS: The rate of healing of tendons: An experimental study of tensile strength. Ann Surg 113:424-456, 1941 55 Thorngate S, Ferguson DJ: Effect of tension on healing of aponeurotic wounds. Surgery 44:619-624, 1958 56 Sussman MD: Effect of increased tissue traction upon tensile strength of cutaneous incisions in rats. Proc Soc Exp Biol Med 123:38-41, 1966 57 Gelberman RH, Woo SL, Lothringer K, et al: Effects of early intermittent passive mobili
zation on healing canine flexor tendons. J Hand Surg [Am] 7:170-175, 1982 58 Noyes FR: Functional properties of knee ligaments and alterations induced by immobilization. Clin Orthop 123:210-242, 1977 59 Videman T: Connective tissue and immobilization. Clin Orthop 221:26-32, 1987 60 Akeson WH, Amiel D, Ing D, et al: Effects of immobilization on joints. Clin Orthop 219:28-37, 1986 61 Jenkin D, Cochrans T: Osteoporosis: The dramatic effect of disuse of an extremity. Clin Orthop 64:128, 1969 62 Finsterbush A, Friedman B: Reversibility of joint changes produced by immobilization in rabbits. Clin Orthop 111:290-298, 1975 63 Kulick MI, Brazlow R, Smith S, et al: Injectable ibuprofen: Preliminary evaluation of its
ability to decrease peritendinous adhesions. Ann Plast Surg 13:459-467, 1984 64 Cohen IK, McCoy B: The biology and control of surface overhealing. World J Surg 4:289-295, 1980 65 Weiner LJ, Peacock EE: Biologic principles affecting repair of flexor tendons. Adv Surg 5:145-188, 1971 66 Madden JW, DeVore G: A rational postoperative management program for metacarpophalangeal joint implant arthroplasty. J Hand Surg [Am] 2:358-366, 1977 67 Bora FW, Richardson S, Black J: The bio-mechanical response to tension in a peripheral nerve. J Hand Surg [Am] 5:21-25, 1980 68 Weber E, Davis J: Rehabilitation following hand surgery. Orthop Clin North Am 92:529-542, 1978
32/1024 Physical Therapy/Volume 69, Number 12/December 1989