Testing Options For Adrenal Cortisol and DHEA...
Transcript of Testing Options For Adrenal Cortisol and DHEA...
YOUR LOGO
Testing Options For Adrenal Cortisol and DHEA Assessment
Copyright© 2016, Kurt N. Woeller, D.O., Tracy Tranchitella, N.D. and Educational Resource Association. This material may not be
reprinted, distributed or used without permission. 1
YOUR LOGO
Lecture Overview
• What are the best tests for adrenal cortisol and DHEA assessment?
• How to interpret a salivary adrenal hormone profile – the basics
• Adrenal markers – reading between the lines for a deeper assessment of an individuals adrenal problem.
• Factors that negatively affect cortisol and DHEA
• Clinical pearls for initial and re-testing accuracy
2
YOUR LOGO
Support Documents For Module #2
• Interpreting A Salivary Adrenal Hormone Profile – The Basics (pdf).
• Things To Do To Increase Accuracy Of Your Adrenal Test - handout
• Medications That Can Alter Cortisol and DHEA Levels (pdf)
• Lecture slides (pdf)
• Lecture slides - note taking (pdf)
3
YOUR LOGO
Comparing Blood, Saliva and Urine Cortisol
• Serum cortisol – measures both ‘free’ (biologically active) and protein bound (cortisol binding globulin (CBG)) cortisol.
• Urine and saliva – both measure ‘free’ cortisol only. However, these values should correlate closely with serum free cortisol levels.
• Obtaining diurnal variation of cortisol, multiple samples need to be collected throughout the day, i.e., 8 am and 4 pm.
5
YOUR LOGO
Serum Cortisol
• Done as a screening assessment of abnormal output of cortisol (high or low) for Addison’s disease or Cushing’s syndrome:• Cushing’s - when pituitary makes too much ACTH because of
excessive growth or tumor.
• Serum cortisol (8 am sample): 6 to 23 mcg/dl (reference ranges may vary slightly from lab to lab).
• Serum cortisol – most is bound to a carrier protein (CBG = Cortisol Binding Globulin) with just a small amount being the ‘free’ fraction.
7
YOUR LOGO
Serum Cortisol
• To obtain diurnal variation compared to saliva or urine, testing multiple samples would be required throughout the day, i.e. morning, noon, afternoon and evening. • Not practical for most people.
• Could do an average cortisol output with just an 8 am collection and 4 pm collection.
• Blood tests would need to be the ‘free’ fraction
9
Serum Cortisol - Pros & Cons
• Main measurement used to assess cortisol output for Addison’s disease and Cushing’s syndrome .
• Established reference ranges for serious adrenal and pituitary diseases.
• Serum test evaluates for ‘free’ fraction and protein-bound cortisol.
• Need to make sure to order ‘free’ fraction.
• Requires multiple blood draws throughout the day to correlate functionally with saliva and urine cortisol assessment.
10
Pro Con
YOUR LOGO
K. Sayyed, et. al. Measurements of serum DHEA and DHEA sulphate levels improve the accuracy of the low-dose cosyntropin (LDC) test in the
diagnosis of central adrenal insufficiency. J Clin Endocrinol Metab. 2012 Oct.
Abstract
• The diagnosis of central adrenal insufficiency (AI) continues to be challenging, especially when it is partial. We have recently demonstrated the value of measuring serum dehydroepiandrosterone sulfate (DHEA-S) in establishing the diagnosis of central AI. The current investigation examined the added value of measuring serum dehydroepiandrosterone (DHEA) levels during low-dose (1 μg) cosyntropin (LDC) stimulation in patients suspected to have central AI.
• Baseline and LDC-stimulated cortisol, DHEA, and DHEA-S were measured preoperatively in 155 consecutive patients with pituitary masses and 63 healthy subjects. Hypothalamic-pituitary adrenal (HPA) function was normal (NL-HPA) in 97 of the patients and was impaired (impaired HPA) in 58 patients. Patients with NL-HPA underwent surgical removal of the sellar masses and received no glucocorticoids before, during, or after surgery.
Patients with impaired HPA function have a more severe loss in DHEA secretion than that of glucocorticoids. Measurements of serum DHEA levels during LDC simulation provide additional valuable information that improves the diagnostic accuracy of LDC in patients suspected to
have central AI. We recommend the inclusion of DHEA and DHEA-S measurements in the laboratory assessment of HPA function.
11
YOUR LOGO
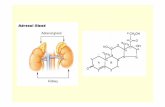
Cortisol
Pregnenolone
Pregnenolone Steal =
B5 Acetyl CoA
Cholesterol
17- Hydropregnenolone
Dehydro -
epiandrosterone
Androstenedione
19 - Hydroxy -
androstenedione
Estrone
Estradiol - 17β
Cholesteryl Sulfate
Dehydro -
epiandrosterone
Sulfate
16α - Hydroxydehydro -
epiandrosterone
16α- Hydroxy -
androstenedione
16α 19 - Dihydroxy -
androstenedione
Estriol
17α - Hydroxylation
Testosterone
5α - Dihydro -
testosterone
19 - Hydroxy -
testosterone
Estradiol - 17α
Progesterone
17 - Hydroxyprogesterone
21 - Hydroxylation
11 - Deoxycortisol
11β - Hydroxylation
11 - Deoxy -
corticosterone
Corticosterone
Aldosterone Cortisone16α - Hydroxyestrone
Circulating LDLs
Steroidal Hormone Principle Pathways
(Illustrating the chronic stress response/pregnenolone steal)
Androstenediol
12
DHEA versus DHEA-S
DHEA DHEA-S
• Made in the adrenals, ovaries and testis.
• DHEA is changed into DHEA-S in the adrenal glands and liver.
• In both men and women estrogen and testosterone depend on DHEA.
• DHEA also involved in insulin growth factor 1 production (IGF-1).
• Form of DHEA produced by adrenal glands.
• Serum test commonly performed in women with excessive hair growth or male characteristics.
• Children who are developing too fast.
• Preferred test for adrenal assessment over DHEA.
13
YOUR LOGO
High DHEA Levels In Women
Signs and Symptoms:
• Acne
• Baldness (female pattern)
• Deeping voice
• Hirsutism (excessive hair growth on the face and body).
• Increased muscle mass and definition
• Abnormal menses, or sterility
14
Other Concerns For High DHEA Levels
• High levels can lead to early puberty in boys.
• High levels in girls can lead to early menses or abnormal periods.
• High levels may indicate adrenal cancer, tumors, or excess growth of hormone-producing tissue (hyperplasia).
15
YOUR LOGO
Other Tests To Consider With High DHEA-S
• Serum ACTH
• Serum Androstenedione – made from DHEA before being converted into testosterone or estradiol.
• Estrogens
• Testosterone
16
YOUR LOGO
Low Levels Of DHEA-S
Main Problems:
• Aging (does occur naturally)
• Chronic adrenal stress
• Dementia
• Erectile dysfunction
• Diabetes or metabolic syndrome
• Osteoporosis
• Vaginal atrophy or inflammation/irritation – happens because of thinning and shrinking of the vaginal tissues and decreased vaginal lubrication.
21
YOUR LOGO
Standard Urine Analysis
• Just like saliva, measures ‘free’ fraction cortisol
• 24-hour urinalysis required
• Does not show diurnal variation
• Measures only the amount of total unbound cortisol produced in a 24-hour period of time.
• Urine testing can be useful for assessing increased cortisol production over a 24-hour period as reflected by abnormal ACTH stimulation.
23
Standard Urine Cortisol - Pros & Cons
24
• Measures ‘free’ fraction of cortisol, instead of protein bound.
• Convenient at home collection.
• Can provide important information about total cortisol production when correlated clinically with patient or client.
Pro
• Doesn’t provide diurnal variation.
• Cannot determine at what time of day levels are high, low or normal.
• Some inconvenience with regards to collection.
Can
YOUR LOGO
Dutch Urine Test
• Dried urine test
• Can test urine cortisol output at same time as saliva would be tested (morning, noon, afternoon and nighttime).
• Measures ‘free’ cortisol + cortisol metabolites: • Deeper assessment of cortisol production
• Saliva only evaluates for ‘free’
• Example – Obesity:• ‘Free’ cortisol tends to be low
• Cortisol metabolites tend to be high
25
YOUR LOGO
Saliva Analysis
• Measures specifically the ‘free’ fraction of cortisol
• Measures ‘free’ fraction of DHEA-S
• Can obtain multiple samples throughout the day for more optimal diurnal rhythm assessment.
• Lab test provides individual reference ranges for morning, noon, afternoon and nighttime values, along with average of two DHEA-S measurements.
• Lab profiles provide graphic representation of cortisol output.
• Total Cortisol + Cortisol/DHEA ratio provided.
27
Saliva Testing - Pros & Cons
Con
• Not always recognized by conventional physicians, i.e. endocrinologists.
• Lack of insurance coverage• Can be easily manipulated by
sublingual tablets or liquids, i.e. DHEA, hydrocortisone.
• No metabolite assessment
30
Pro
• Measures ‘free’ fraction• Easy to obtain multiple
samples throughout the day.• Highly effective at correlating
information about clinical picture of patient/client.
• Provides dynamic information about output of cortisol throughout the day.
YOUR LOGO
Interpreting a Salivary Adrenal Hormone Profile –
The BasicsThe BioHealth Laboratory #201 Profile
31
YOUR LOGO
1. ALWAYS correlate the test data to the clinical history of the patient.
2. Scan each individual cortisol value (ideally want to see the values in the upper 1/3 of normal range). Total cortisol should be upper 1/3 of normal too.
3. Scan total representation of all 4 cortisol’s (look at the total picture – highs and lows)• Example: Rollercoaster pattern
4. DHEA – low, normal, high• Ideal ratio is 5-6:1 (Total Cortisol:DHEA)
Steps To Take When Evaluating Salivary Adrenal Test
YOUR LOGO
Cortisol
Pregnenolone
Pregnenolone Steal =
B5 Acetyl CoA
Cholesterol
17- Hydropregnenolone
Dehydro -
epiandrosterone
Androstenedione
19 - Hydroxy -
androstenedione
Estrone
Estradiol - 17β
Cholesteryl Sulfate
Dehydro -
epiandrosterone
Sulfate
16α - Hydroxydehydro -
epiandrosterone
16α- Hydroxy -
androstenedione
16α 19 - Dihydroxy -
androstenedione
Estriol
17α - Hydroxylation
Testosterone
5α - Dihydro -
testosterone
19 - Hydroxy -
testosterone
Estradiol - 17α
Progesterone
17 - Hydroxyprogesterone
21 - Hydroxylation
11 - Deoxycortisol
11β - Hydroxylation
11 - Deoxy -
corticosterone
Corticosterone
Aldosterone Cortisone16α - Hydroxyestrone
Circulating LDLs
Steroidal Hormone Principle Pathways
(Illustrating the chronic stress response/pregnenolone steal)
Androstenediol
33
YOUR LOGO
Pregnenolone Steal
• Preferential pathway under stress
• Body prioritizing to maintain cortisol to maintain cellular and organ system function.
• Long-standing problems often show:• low normal or low cortisol(s)
• low normal or low DHEA-S
34
YOUR LOGO
• Each individual cortisol value is reflected by what was going on prior to its production:• Morning cortisol – middle of the night/early morning:
• Erratic sleep or blood sugar imbalance• Chronic infections
• Noon cortisol – earlier in the morning:• Breakfast or lack of food• Stimulants• Morning stress
• Afternoon cortisol – lunch time/early afternoon:• Lunch, lack of lunch• Afternoon slump
• Nighttime cortisol – early evening:• Stress from days events• Workout• Afternoon stimulants • High energy at nigh
What Do The Individual Cortisol Values Relate To?
YOUR LOGO
• Morning Routine:• What time do they get up?
• Do they feel rested upon awakening?
• How long before eat breakfast? What do they eat?
• Coffee (other caffeine) consumption. How much?
• Activity level – exercise?
• Work – stay at home, commute
Questions To Ask ALL Patients/Clients With Regards To
Their Test Results
YOUR LOGO
• Before Noon:• What is their energy like during the morning?
• What time do they eat lunch?
• What do they usually consume?
• Caffeine use
• Exercise
• Work related activities
Questions To Ask ALL Patients/Client With Regards To
Their Test Results
YOUR LOGO
• Afternoon:• What is their energy like?
• Are they hungry in the afternoon?
• More caffeine use?
• Work related activities
Questions To Ask ALL Patients/Client With Regards To
Their Test Results
YOUR LOGO
• Nighttime:• What is their energy like?
• What time do they eat dinner?
• Any caffeine use at night?
• Exercise at night?
• Do they get a “second wind” at night?
Questions To Ask ALL Patients/Client With Regards To
Their Test Results
YOUR LOGO
• Sleep:• What time to bed?
• How long to fall asleep?
• How long stay asleep?
• Nighttime routine/sleep hygiene (bath, temperature of bedroom, computer, etc.).
• Evening meal, alcohol use at night?
Questions To Ask ALL Patients/Client With Regards To
Their Test Results
YOUR LOGO
Jane Doe
• 59 year old female
• CC: “tired all the time.” difficult time with managing daily stress, along with poor memory. Little to no sex drive.
• Social history: • Works as a receptionist for a busy dental office.
• No smoking, but does consume wine about 4 times weekly.
• Exercise: does treadmill at community center gym 3 times weekly for about 20 minutes; periodic aerobics class.
43
YOUR LOGO
Jane Doe
• Medical history: • Fibromyalgia and chronic fatigue for about 6 years
• Menopause for 7 years
• Medications: • Sertraline (Zoloft) – for depression and anxiety
• Tylenol – uses for periodic headaches
• Supplements: • Centrum multivitamin
• Fish oil
44
YOUR LOGO
Lab Test Observations
• All cortisol values low, except nighttime which is normal.• Question – anything to consider with regards to low
daily cortisol values, but then a normal nighttime levels?
• Total cortisol low at 21.6
• DHEA low at 1.93• Question - how might this relate to some of her
complaints?
• Cortisol/DHEA-S ratio – high at 11.2
YOUR LOGO
Lifestyle Changes:
• Improve bedtime/sleep routine
• Healthy snack before bed
• More consistent exercise, but outdoors. Reduce cardio and more resistance training.
• Improve quality of diet, i.e. more healthy fats, consistent meals, fruits and vegetables, less carbs.
• Patient/client to read through ‘Adrenal Health Restoration Handout’ and incorporate 3 to 4 things from each category.
Adrenal Health Restoration Program (example)
YOUR LOGO
BioMatrix One Products (www.BioMatrixOne.com):
• Support Adrenals – 2 capsules w/breakfast and 2 capsules w/lunch.
• Support Minerals – 3 tablets in the evening• Support Glucose – 1 capsule with each meal• Pregnenolone (liquid) – 10 drops three times daily (best
between 6 to 7 am, 11 am to noon and 2 to 3 pm). Licorice Root (liquid) – 3 drops three times daily at same time as Pregnenolone.
• DHEA (liquid) – 1 drop three times daily at same time as pregnenolone and licorice root.
NOTE: Avoid taking pregnenolone, licorice root and DHEA after 6 pm at night.
Adrenal Supplement Program
YOUR LOGO
Additional Supplements
• Magnesium glycinate – 400mg before bed
• GABA – 1000mg one hour before bed
• L-Theanine – 200mg one hour before bed
51
YOUR LOGO
Additional Testing Considerations
• Blood chemistry profile:• Blood sugar, electrolytes
• fasting insulin, hemoglobin A1c
• TSH, free T4, free T3 or Total T3 (module #5)
• Lipid panel
• Organic Acids Test (to be discussed as Bonus Lecture)
• Food sensitivity (module #6)
• Gastrointestinal pathogen test (module #6)
52
YOUR LOGO
Medications That Can Alter Cortisol and DHEA Levels
58
For a more detailed description see handout in Module #2 titled“Medications That Can Alter Cortisol and DHEA Levels”
YOUR LOGO
Medications That Can Raise Cortisol
• Progesterone – progesterone is a precursor to cortisol.
• Hydrocortisone – generally used with very low total cortisol on an adrenal test and correlating clinical picture. Used in divided dosages throughout the day starting with a higher dosage in the morning followed by lower dosages for the rest of the day. Used for a short period of time and gradually weaned off.
• Cortef - a pharmaceutical brand of hydrocortisone; has glucocorticoid activity.
59
YOUR LOGO
Higher Potency Steroids
• Chronic Use of Steroid Medication:• Prednisone, Medrol Dose Pak, Dexamethasone,
Triamcinolone, Fluocinalone.
• Florinef - used specifically for Addison’s disease.
• Initial rise of cortisol on test samples with any kind of steroid medication.
• Long term use is suppressive to normal cortisol production.
60
YOUR LOGO
Medications That Can Raise Cortisol
• Allergy and Asthma medication, decongestants –any medication classified as sympathomimetic (stimulates the sympathetic nervous system) has the potential to raise cortisol levels.
• Stimulants used in the treatment of ADD such as Dexedrine, Adderall, Ritalin – stimulate the central nervous system. Studies have shown a rise in cortisol in children on these medications.
• Caffeine – central nervous system stimulant.
61
YOUR LOGO
Higher Potency Steroids
• Chronic Use of Steroid Medication:• Prednisone, Medrol Dose Pak, Dexamethasone,
Triamcinolone, Fluocinalone.
• Initial rise of cortisol on test samples with any kind of steroid medication.
• Long term use is suppressive to normal cortisol production.
63
YOUR LOGO
Steroidogenesis Inhibitors
• Ketoconazole (Nizoral) – inhibits cortisol production in adrenal cortex.• Nizoral not used much anymore as an antifungal for
common/routine fungal infections.
• Generally reserved for serious fungal infections.
• Mitotane (Lysodren) – used to treat Cushing’s syndrome. • Inhibits production of cortisol by reducing the activity of
the cells of the adrenal cortex.
64
YOUR LOGO
Steroidogenesis Inhibitors
• Cytadren (aminoglutethimide) – inhibits enzymatic conversion of cholesterol to pregnenolone resulting in a decrease in the production of adrenal glucocorticoids, mineralocorticoids, estrogen and androgens. • Also, inhibits synthesis of thyroxine resulting in elevated
TSH. Does not have an effect on prolactin.
• Used in the treatment of Cushing’s syndrome.
65
YOUR LOGO
Neuromodulatory Agents
• Octreotide (Sandostatin) – somatostatin analogue which inhibits the release of peptide hormones in various tissues; suppresses pathological release of ACTH and cortisol in Cushing’s disease. • Primarily used in the treatment of Cushing’s syndrome.
• Bromocriptine (Parlodel, Cycloset) – inhibits the release of CRH from the hypothalamus; is a dopamine receptor agonist (promoter) and is used to treat Parkinson’s Disease. • Also, used to treat infertility and amenorrhea in relation to
elevated prolactin levels. Treatment for pituitary prolactinomas and overproduction of GH resulting in acromegaly. Can also be used in the treatment of Type II Diabetes.
66
YOUR LOGO
Neuromodulatory Agents
• Cyproheptadine (Periactin, Peritol) – antihistamine, serotonin antagonist, anticholinergic; affects cortisol output by modulating output of ACTH.
• Pharmacology mechanism indicates that serotonin has an influence over adrenal function.• This medication is commonly used to improve appetite
stimulation.
67
The link to Adrenal Function, ACTH and Serotonin will be discussed in more detailIn Module #8 of Adrenal Mastery Course.
YOUR LOGO
Cortisol Receptor Antagonists
• Mifepristine (Korlym) – competitively binds to glucocorticoid receptors inhibiting the effects of cortisol.
• Does not affect production of other hormones.
• Used to treat ectopic ACTH-producing tumors.
68
YOUR LOGO
Antidepressants and Anxiolytics
• Tricyclics – Amitriptyline (can be used for sleep problems).
• Serotonin Reuptake Inhibitors (SSRI) – Prozac, Lexapro, Zoloft…
• Benzodiazepines – Ativan, Xanax…
Effect of all of these seems to be primarily on hypothalamic release of CRF.
69
DHEA
Raise Lower
• Xanax (Alprazolam) – anxiety
• Norvasc (Amlodipine) - antihypertensive
• Arimidex (Anastrozole) – lowers estrogen in postmenopausal women; breast cancer.
• Procardia (Nifedipine) – angina
• Danazol (Danocrine) – suppresses gonadotropins.
• Cardizem (Diltiazem) – antihypertensive
• Ritalin (Methyphenidate) – ADHD
• Thorazine (chlorpromazine),Seroquel (quetiapine) and other antipsychotic medications.
• Pulmicort (Budesonide)• Estrogens• Oral contraceptives • Dexamethasone (Decadron),
and other corticosteroids.• Metformin (Glucophage)
70
YOUR LOGO
Clinical Pearls For Adrenal Testing
Factors That Can Affect Initial and Retesting of Salivary Adrenal
Hormones of Cortisol and DHEA
71
YOUR LOGO
Steps Your Patients/Clients Need To Do For Accurate Adrenal Testing
• Test should be done on a typical day:• Regular work day or week
• Not while on vacation
• If any significant event that is unusual occurs, they should empty vials and start again in a few days:• Traffic accident
• Significant injury
• Family crisis
• Major personal mental/emotional event
72
YOUR LOGO
Steps Your Patients/Clients Need To Do For Accurate Adrenal Testing
• Avoid ALL caffeine products on day of testing
• Avoid excessive stressful exercise that is beyond what is typical.
• If patient/client didn’t sleep well the night before test collection then do collection on another day. This is particularly important if the lack of sleep was significant and out of the ordinary.
73
YOUR LOGO
Things You Need To Do Before Salivary Adrenal Testing
• Discontinue cortisol and/or DHEA promoting supplements:• Pregnenolone, DHEA and Licorice Root
• Alcohol version (liquid) – 48 to 72 hours or longer
• Sublingual Tablets – 7 to 10 days
• Oral capsules or tablets – 3 to 5 days
• Transdermal Creams – 30 to 60 days
• Transdermal gels – 10 to 14 days
74
YOUR LOGO
Things You Need To Do Before Salivary Adrenal Testing
• Steroids (i.e. prednisone, hydrocortisone) – 3 to 5days after medical taper.
• Support Adrenals (BioMatrix) – avoid taking for 5 days prior to collection.
• AdaptAlign (BioMatrix) – okay to test while taking
• Adrenal glandular/cortex – avoid taking for 5 days.
• Other: adaptogenic adrenal products should be okay to continue with while testing.
75
YOUR LOGO
Gain access to comprehensive testing including Organic Acids, Comprehensive Digestive Stool Analysis, Adrenal Hormone, Hair,
Amino Acids, etc.
• All tests kits sent to your home or office• No doctor visit needed for ordering• Each lab reviewed personally by integrative medicine doctor• Written lab review provided with recommended action steps based on lab test markers• Access to professional line supplements • Great Plains Laboratory, BioHealth Laboratory, Doctors Data, ZRT, etc.
www.labtestsplus.com for a
complete list of lab tests available . 76
YOUR LOGO
Topic
• The Stages of Adrenal Dysfunction:• Understanding what stage of adrenal dysfunction your
patient/client is currently in.
• Improving clinical outcomes with regards to adrenal remedy intervention.
• What order to introduce adrenal supplements for improved clinical outcome and to avoid problems.
• Creating a program for your patient/client
• Why you need to retest patients adrenal profiles
• What to do with supplement or medication sensitive individuals.
Module #3
77
YOUR LOGO
Thank YouKurt N. Woeller, D.O.
www.AdrenalMasteryCourse.com
78