TEMS – pushing the limits - Pelican Courses · TART inferior to TEMS ... Rectoscope tube 12 or...
Transcript of TEMS – pushing the limits - Pelican Courses · TART inferior to TEMS ... Rectoscope tube 12 or...
Scope of presentation
TART: Transanal excision (using retractors)
TEMS: Transanal endoscopic microsurgery
TEO: Transanal endoscopic operation
TAMIS: Transanal minimally invasive surgery
Which one to choose?
TART inferior to TEMS
TEO same principle as TEMS but not binocular vision and less stable platform
TAMIS early days, but seems to be less versatile and difficult to get stable platform
TEMS -what is it?
Endoluminal rectal surgery
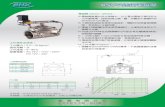
Rectoscope tube 12 or 20cm long, 40mm
Stereoscopic optics with magnification
Channels for CO2 insufflation, rectal pressure measurements, irrigation
3 ports for grasper, diathermy, suction
Specialised instrumentation
Gerhard Bueß (1948 -2010)
Developed in Cologne, West Germany 1980 – 1983
First NOTES (natural orifice transluminal endoscopic surgery), using a natural orifice to gain access to the gut i.e. rectum
Ignored outside Germany until early 1990’ies
Introduced at Good Hope Hospital by Arthur Allan in 1994
Indications and limitations
For excision of rectal tumours up to 18cm from anal verge
Allows full thickness excision and suturing
Adenoma even circumferential
Carcinoma
Carcinoid
GIST
Advantages
Excellent access and binocular view of whole rectum
Sphincters less compromised than using retractors
Constant gas insufflation stable platform
Ability to dissect and suture
TEM and rectal cancer
For cure: low risk T1 ca: G1/G2 SM1 ?SM2
For compromise: high risk T1/T2 with (chemo)radiation possibly cure
For palliation: T3 with (chemo)radiation
Unresolved:
?accurate preop staging
?when to add preop DXR/chemorad
Pathway
Referral > Assessment plus ERUS
Review of staging plus histology at MDT
If low risk / benign: TEMS
If high risk / not suitable; refer back
Review TEMS histology at MDT
If high risk, discuss standard surgery
Complications/pitfalls
Bleeding
Perforation/dehiscence
Rectal stricture
Urinary retention
Impaired continence
Recurrence
How to refer
Via network proforma MDT coordinator
E-mail / fax / phone call
Letter in the post takes a long time!
Fax: 0121 4249548 (surgical secretaries)
E-mail: [email protected]
Mobile: 07801 654781
Try to see within the week
H.M. 80y M Soiling of mesorectum (ypT1)
Wound breakdown > fistula into seminal vesicle 2 months later
Settled with defunctioning colostomy
Take care:
Start with small benign lesions
Can you close the defect if peritoneum is opened?
Can you safely perform further surgery if malignancy dictates so?
Rectal cancer treated with TEMS at GHH 1995 - 2012
154 patients (93 men):
91 without DXR
38 short course DXR
17 long course chemoradiation
8 post op DXR
No preop DXR (91)
59 pT1:
16 after prev. polyp cancer: no residual ca
33 favourable histology: no further treatment
2 local recurrences (11-51m); 1 salvage, 1 too frail
2 incompletely excised (too high): too frail for resection
8 poor prognostic features > radical resection: no recurrences, no mets
No preop DXR (91)
30 pT2:
18 radical surgery:
2 lung mets (2-18m) > 1 resected
12 too frail for radical surgery:
5 died unrelated (3-25m)
1 local recurrence (4m), 2 metastases (3-11m)> died
4 alive and well
2 pT3: radical surgery: alive and well
Preop DXR (55)
16 ypT0: complete pathological response (29%): NSR
10 ypT1: no local recurrence, 1 lung met (27m)> resected
21 ypT2:
4 local recurrence (6-27m)
3 salvage (2 further recurrence, 1 alive, 1 died)
1 stent > died from disease
3 metastatic disease (22-27m)
2 metastasectomy (1 died post op)
1 died from disease
Preop DXR (55)
8 ypT3:
2 radical surgery: one disease free, one died from metastatic disease (no LR)
1 died post op (day 11)
2 local recurrence (7-18m)> 1 salvage APR, 1 died
1 died metastatic disease (2m)
1 died unrelated (9m)