ARTICULATIO TEMPOROMANDIBULARIS Temporomandibular joint Temporomandibular joint.
Synovial chondromatosis of the temporomandibular joint · Invited Review Paper TMJ Disorders...
Transcript of Synovial chondromatosis of the temporomandibular joint · Invited Review Paper TMJ Disorders...

Invited Review Paper
TMJ Disorders
Int. J. Oral Maxillofac. Surg. 2010; 39: 745–755doi:10.1016/j.ijom.2010.03.028, available online at http://www.sciencedirect.com
Synovial chondromatosis of thetemporomandibular joint:a case description withsystematic literature review
L. Guarda-Nardini, F. Piccotti, G. Ferronato, D. Manfredini: Synovialchondromatosis of the temporomandibular joint: a case description with systematicliterature review. Int. J. Oral Maxillofac. Surg. 2010; 39: 745–755. # 2010International Association of Oral and Maxillofacial Surgeons. Published by ElsevierLtd. All rights reserved.0901-5027/080745 + 011 $36.00/0 # 2010 Inte
rnational Association of Oral and Maxillofacial SurgeL. Guarda-Nardini1, F. Piccotti2,G. Ferronato3, D. Manfredini1
1TMD Clinic, University of Padova, Italy;2Marina di Carrara (MS), Italy; 3Department ofMaxillofacial Surgery, University of Padova,Italy
Abstract. Synovial chondromatosis (SC) of the temporomandibular joint (TMJ) is arare disease characterized by the presence of calcified loose bodies within the joint,and few systematically gathered data are available about its epidemiology. The aimof this paper was to describe a case of SC of the TMJ, and to carry out a systematicreview of the literature on epidemiology over the past decade. A case of a 53-year-old female with the classical triad of signs and symptoms of SC (pain, swelling,restricted mouth opening) is described. A systematic search in the National Libraryof Medicine’s PubMed Database was performed. 155 cases were described in 103publications. Most dealt with single case reports. Females are affected more thanmales with a 2.5:1 ratio and the mean age of patients was about 46 years. Latediagnosis is common and in most cases more than 2 years elapsed between symptomonset and surgical intervention. Open TMJ surgery is the treatment of choice, sinceless invasive techniques, such as arthroscopy, allowed complete removal of theloose bodies only in about half of cases. A single recurrence was described,confirming the benign nature of the disease.
Key words: temporomandibular joint; synovialchondromatosis; systematic review; TMJ sur-gery.
Accepted for publication 26 March 2010
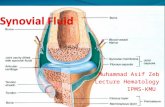
Synovial chondromatosis (SC) is a carti-laginous metaplasia of the mesenchymalremnants of the synovial tissue of thejoints. Its main characteristic is the for-mation of cartilaginous nodules that maybe pedunculated and/or detach from thesynovial membrane, becoming loosebodies within the joint space36. Theaetiology of SC is not fully understoodand cases are divided into primary SC(without identifiable aetiological factors)
and secondary SC (with a known aetiol-ogy). Secondary cases are often thoughtto be related to previous trauma, repeti-tive microtrauma or degenerative arthri-tis. Primary cases cannot be associatedwith any supposed aetiological factorsand are considered to be more aggres-sive23.
SC usually affects large synovial joints,such as the elbow and knee, and it isuncommon in the temporomandibular
joint (TMJ)30. The main clinical symp-toms are preauricular swelling, pain, lim-itation of jaw movement and crepitus jointsounds. The diagnosis is made by compu-terized tomography (CT) and magneticresonance imaging (MRI)22. Surgery isthe therapeutic choice to remove nodulesand loose bodies from the joint space.Several approaches have been described,depending on the extension of the lesionwith respect to the cranial fossa10.
ons. Published by Elsevier Ltd. All rights reserved.

746 Guarda-Nardini et al.
The first reported case of SC of the TMJwas in 1933, when Axhausen reportedmetaplastic chondrogenesis in the syno-vial membrane4. After that, reports werecharacterized by inconsistencies ofnomenclature, until the 1980s when theterm ‘SC’ was adopted32,40,54. A literaturereview of the period up to 1997 showedthat 74 cases of SC of the TMJ weredescribed, mainly as isolated casereports55. More recent studies haveattempted to summarize the literaturedata3,30,58, but none has satisfied the needfor a systematic assessment, and the find-ings are inconsistent regarding the totalnumber of SC cases.
The aim of the present paper is todescribe a case of SC of the TMJ and tocarry out a systematic review of the lit-erature over the past decade to update theepidemiological data.
Case report
A 53-year-old woman was referredbecause of severely restricted mouth open-ing and pain in the TMJ area. She pre-sented a slight swelling in the rightpreauricular area, she was unable to openher mouth more than 20 mm and the mid-line of the mandible was deflected slightlyto the right side (Fig. 1). Symptoms hadbeen present for about 1 year before theappointment and the restriction of mouthopening had worsened progressively. Forabout 6 months, the patient had worn anoral appliance prescribed by a generaldental practitioner on the basis of an
Fig. 1. Preoperative mouth opening withdeflection on the affected side and slight pre-auricular swelling.
unspecified diagnosis of ‘craniomandibu-lar dysfunction’ without experiencing anyimprovement. After that, the family phy-sician had treated her with anti-inflamma-tory drugs (ketoprofene 80 mg, twice aday for 7 days) but her symptoms hadremain unchanged and she was thenreferred to the authors’ tertiary centre.During history taking, she denied any pasttrauma or diagnosis of any rheumatologi-cal conditions. Physical examinationrevealed that, despite the preauricularswelling, neither dysfunction of the facialnerve nor hearing disturbances were pre-sent. Joint sounds on the right side wereabsent and the contralateral joint wasnegative on palpation. An orthopantomo-gram seemed to reveal one small calcifi-cation around the condyle, so furtherstudies using imaging techniques wererequested.
MRI showed an hypoechoic arealocated anteriorly to the condyle in theclosed mouth position and located poster-iorly to the condyle in the open mouthposition (Fig. 2). CT confirmed the pre-sence of at least two loose bodies withinthe right TMJ and the diagnostic hypoth-esis of SC was made. The patient wasscheduled for surgery.
A classical surgical approach to theTMJ was chosen owing to the impossi-bility of removing wide loose bodies bymeans of arthroscopy alone. Under gen-eral anaesthesia, the right TMJ wasexposed using a preauricular incision.Immediately after opening the joint cap-sule, some transparent and viscous fluidcame out of the joint space. A large calci-fied loose body was present in the upper
Fig. 2. MRI revealing a large hypoechoic area (ment of the right TMJ. (For interpretation of thereader is referred to the web version of the artic
joint space and was removed (Fig. 3),another fibrous micronodular loose bodywas found around the condyle (Fig. 4).Two large loose bodies were detectedwithin the TMJ, in contrast to the largenumber of small bodies described in othercases (Fig. 5). Synovectomy was per-formed to allow clearage of the jointcompartment from any potential residualof metaplastic activity. Post-surgical his-tological examination revealed chondro-metaplasia of the synovial membrane andconfirmed the diagnosis of SC of the rightTMJ, classified as third stage according toMilgram’s classification (Fig. 6)36.
The postoperative course was unevent-ful and only painkillers and antibioticswere prescribed. The day after surgery,a postoperative mouth opening of 28 mmwas recorded, with no motor deficit on theright side of the face. Vigorous phy-siotherapy was started 1 week before sur-gery, and follow-up assessments werescheduled at 1 week, 1 month, 3 months,6 months and 1 year. At the 1 year appoint-ment, a maximum mouth opening of43 mm was recorded, with no signs ofrecurrence (Fig. 7).
Literature review
On 30 July 2009 a systematic search in theNational Library of Medicine’s PubMedDatabase was performed to identify allpeer-review papers in the English litera-ture dealing with cases of SC of the TMJ.The studies included for discussion in thereview were clinical studies describingsurgical interventions performed on oneor more new cases of SC of the TMJ with
yellow arrow) in the posterosuperior compart-references to color in this figure legend, the
le.)

Synovial chondromatosis of the TMJ 747
Fig. 3. Removal of a large calcified loose body from the joint space.
respect to the last comprehensive reviewcarried out by VON LINDERN et al.55.
The search strategy comprised foursteps: a search based on the Medical Sub-jects Headings (MeSH) of the PubMeddatabase; a word terms search within thePubMed database; a search withinPubMed related articles to find theselected ones; a search within the refer-ences lists of the selected articles.
The following MeSH terms were usedto identify a list of potential papers to beincluded in the review.
� T
Fi
MJ: an articulation between the con-dyle of the mandible and the articular
g. 4. Removal of a second large loose body, wh
tubercle of the temporal bone. Yearintroduced: 1997.
� S
C: rare, benign, chronic, progressivemetaplasia in which cartilage is formedin the synovial membranes of joints,tendons sheaths, or bursae. Some ofthe metaplastic foci can becomedetached producing loose bodies. Whenthe loose bodies undergo secondarycalcification, the condition is calledsynovial osteochondromatosis. Yearintroduced: 1990 (previous indexing:chondroma, 1966–1989).The search was limited to papers in theEnglish language published later than 01/
ich had a fibrous micronodular aspect.
01/1998 and the combination of the twoMeSh terms allowed the identification of23 citations, the abstracts of which wereread to select articles to be retrieved in fulltext. After abstract reading, 12 paperswere selected for inclusion in the review.
In the second step of the literaturesearch the combined word terms ‘TMJ’and ‘SC’ were used to identify otherpotential papers to be included in thereview. Limits were set as describedabove. This search strategy provided a listof 49 new citations, the abstracts of whichwere read to select articles to be retrievedin full text. After abstract reading, 30additional papers were selected for inclu-sion in the review.
A search within the PubMed relatedarticles for each of the included papersand a hand-made search within the refer-ences lists of the included papers wereperformed, but no additional relevantpapers were identified.
A total of 42 papers were selected forinclusion and discussion in this review onthe basis of abstract reading. Retrieval offull texts was possible for 38 papers, whilein four cases the full text of the paper wasnot retrieved because the authors wereunavailable because of address changesor did not respond to the authors’ request.
For each of the included studies, thefollowing data were recorded for discus-sion: sample size; age of the patient at thetime of surgical intervention; male-to-female ratio; right-to-left joint ratio; clin-ical signs and symptoms; duration of symp-toms before intervention; diagnosticimaging technique; type of surgical tech-nique; number of loose bodies extractedfrom the joint space; follow-up period atthe time of last observation after interven-tion; presence/absence of recurrence(Table 1). Papers available only in abstractform were included in the table to provideas much comprehensive data as possible onthe prevalence and demographic features ofthe disease; most of them provided suffi-cient information but little information onthe other features of the cases was avail-able, and is thus missing from the table.
Results
Number of cases and demographic
features
The selected studies accounted for 80 newcases of SC of the TMJ. Only 8 studiesdescribed more than one case, and 2 of themdescribed only two cases of SC. The age ofthe patients ranged between 12 and 81 yearsin the 38 studies for which age data wereavailable (77 cases from 38 full texts and

748 Guarda-Nardini et al.
Fig. 5. This case of SC was characterized by the presence of only two large loose bodies.
Fig. 7. Mouth opening at the 1 year follow up.
one abstract), with an approximate meanage of 46.3 years. Only one case of a patientunder 18 years affected by SC wasdescribed. Females are affected almostthree times more than males, with a ratioof 56:20 (76 cases from 38 full text papers).The right and left TMJs seem to be affectedequally; 40 cases to the right and 37 to theleft joint (76 cases from 38 full text papers).Only a single new case of bilateral involve-ment was reported, even if surgical data areavailable only for one joint.
Signs and symptoms
The three cardinal signs and symptoms ofSC of the TMJ were confirmed to be pain
Fig. 6. Histopathological findings showing cho
in the preauricular area (69 out of 76 casesfor which data are available), swelling,facial asymmetry or joint deformity (62/76 cases) and impairment in jaw function(49/76). Other less frequent symptomswere, in order of prevalence: occlusalchanges, joint sounds, trismus, headache,sensory disturbances, facial nerve palsy.
The duration of symptoms before inter-vention ranged from 1 month to 15 years;the time span between symptom onset andsurgery was reported in only 64 cases (26studies). 20 of the 26 studies that providedsuch data described cases with symptomslasting from 2 years or more before correctdiagnosis was made and surgery was per-formed.
ndrometaplasia of the synovial membrane.
Diagnostic imaging techniques
The type of imaging techniques used fordiagnosis and surgical planning was speci-fied for 74 cases. CT and MRI were themost common techniques, being used in 56and 54 cases, respectively. Orthopantomo-graphy was used additionally in 31 cases.Other less frequently used techniques werearthrography (4 cases), cone-beam CT (3cases) and sagittal tomography (2 cases).
Surgical techniques
Most studies described open surgery inter-ventions, which were performed in 63/76cases. Five of those cases were descrip-tions of computer-assisted surgery. Syno-vectomy was the most frequent procedureassociated with loose body removal fromthe joint space, often accompanied bydiskectomy and, less frequently, by con-dylectomy. Precise data on the frequencywith which these procedures were per-formed could not be gathered due to thepaucity of studies that provided descrip-tions of the surgical technique. In a fewcases (4/76) an intracranial extension wasdescribed and repair of the cranial fossawas needed. Arthroscopy was used in 11/76 cases, followed by open surgery in 4cases to allow removal of all loose bodiesand declared by the authors to be onlypartially successful at removing loosebodies in one case, thus accounting for a6/11 (55%) success rate for arthroscopywhen used alone. Arthrocentesis was usedin one case, while in one case the type ofsurgical intervention was not specified.

Syn
ovia
lch
on
dro
ma
tosis
of
the
TM
J749
Table 1. Summary of data from the studies included in the review. Legends: F = female; M = male; R = right; L = left; MIO = mouth interincisal opening; MR = magnetic resonance;CT = computerized tomography; AR = arthrography; OPT = orthopantomography; CBCT = cone-beam computerized tomography; ST = sagittal tomography; N.S.: = not specified.
Study’s firstauthor andyear
Samplesize Age
F/Mratio
R/Ljoint Clinical signs and symptoms
Duration ofsigns andsymptoms
Diagnosticimaging
technique Surgical techniqueNr. of
loose bodies
Follow-upspan
(months) Recurrence
CAI, 20098 1 21 1 F 1 L Pain, reduced MIO, click, concurrentpigmented villonodular sinovitis
N.S. MR Arthroscopy Multiple(unspecified)
13 No
PENG, 200942 1 58 1 F 1 R + L Slight diffuse swelling, reduced MIO,preauricular tenderness
N.S. OPT, CT Open surgery withdiskectomy
Multiple(unspecified)
N.S. N.S.
ZHA, 200959 1 44 1 M 1 L Crepitation, deflection, hard 3.5 cmmass in the preauricular area
3 years CT, MR Open surgery withno diskectomy orcondylectomy
Multiple(90–95)
60 No
ADACHI, 20082 1 25 1 F 1 L Trismus, TMJ pain exacerbated withfunction
9 months N.S. Arthrocentesis Multiple(unspecified)
N.S. N.S.
FERNANDEZ-
SANROMAN, 200813
5 34–56 3 F, 2 M 3 R, 2 L Pain (5/5 cases), occlusal changes(4/5), swelling (3/5), dysfunction (3/5)
34–48months
OPT,MR, CT
Arthroscopy (3)or open surgery (2)
Multiple(unspecified)
16–108 No
HOHLWEG-
MAJERT, 200822
5 12–66 4 F, 1 M 1 R, 4 L Preauricular swelling and pain in 4/5cases, only pain in 1 case
1–36months
OPT (1)MR (4)CT (3)CBCT (2)
Computer-assisted surgery
Multiple(unspecified)
0–132 No
HONDA, 200824 1 35 1 F 1 R TMJ pain and reduced MIO 10 years MR, AR,CBCT
Arthroscopy (onlywith partial removalof loose bodies)
Multiple (15) 12 No
KADEMANI, 200827 1 55 1 F 1 R Preauricular swelling, open bite on theaffected side, headache
N.S. OPT, CT Open surgerywith condyloplastye glenoid fossa repair
Multiple(unspecified)
N.S. N.S.
SEMBRONIO, 200849 1 28 1 F 1 R Pain and swelling N.S. MR Arthroscopy plusopen surgery toallow removal ofall loose bodies
Multiple(unspecified)
N.S. N.S.
YOKOTA, 200858 1 52 1 M 1 R Pain, swelling, difficulties to open themouth
N.S CT, MR Combinedtranszygomatictemporal skull baseand perauricularapproach(condylectomy andcranial fossa repair)
Multiple(unspecified)
N.S. No
ACAR, 2007*,1 1 72 – – – – – – – – –
BALLIU, 20076 1 31 1 M 1 R Painful swelling N.S. CT, MR Open surgery Single mass(cartilagineousnodulessurroundedby synovia)
0 No

750
Gu
ard
a-N
ard
ini
eta
l.Table 1 (Continued )
Study’s firstauthor andyear
Samplesize Age
F/Mratio
R/Ljoint Clinical signs and symptoms
Duration ofsigns andsymptoms
Diagnosticimaging
technique Surgical techniqueNr. of
loose bodies
Follow-upspan
(months) Recurrence
D’SOUZA, 200711 1 63 1 F 1 L Pain, swelling, crepitus, history of pastunresolutive interventions
10 years CT 2 Open surgeries,the second withsynovectomy,diskectomy andinterposition ofdermis-fat graft(programmed for acondylar resection)
Multiple(unspecified)
�72 Yes
LIEGER, 200730 1 42 1 F 1 R Pain on function, slight deflection onmouth opening
5 years OPT, MR,CT
Open surgerywith synovectomy
Multiple(unspecified)
9 No
MANDRIOLI, 2007*,33 1 – – – – – – – – – –
REYES MACIAS,200745
1 54 1 F 1 R Pain on jaw movement, deformity ofthe TMJ
5 years N.S. Open surgery Multiple(unspecified)
8 No (infiltrationwith steroids tocontrol painafter 1 month)
XU, 200756 1 49 1 F 1 L Pain, headache, swelling 7 years MR, CT Open surgery Multiple(unspecified)
24 No
HAMMODEH, 2006*,20 1 – – – – – – – – – –
HUH, 200625 1 74 1 M 1 L Swelling with intermittent pain 2 years OPT,CT, MR
Open surgery withhigh condylectomy
Multiple(unspecified)
N.S. N.S.
ARDEKIAN, 20053 11 19–72 8 F,3 M
6 R, 5 L TMJ pain (10/11 cases), swelling (8/11), reduced MIO (3/11)
1–180months
OPT,CT, MR
Open surgerywith synovectomy(11/11) anddiskectomy (7/11)with temporalisflap (6/11)
Multiple in7/11 cases,no in 4/11(diagnosisconfirmed byhistologicexamination)
12–120 No (onecase of orthosurgery neededto correctocclusionafter SC)
HAMILTON, 200519 1 66 1 F 1 L Asymptomatic preauricular mass 2 years CT, MR Unsuccessfulaspirationfollowed by opensurgery
Multiple(unspecified)
N.S. N.S.
MARTIN-GRANIZO,200534
1 49 1 F 1 L Pain, swelling, joint sounds 6 months CT, MR Open surgeryafter unsuccessfularthroscopy
Multiple(over 200)
12 No
MUPPARAPU, 200539 1 65 1 F 1 R Premature dental contact in the left andopen bite in the right side
18months
CT, MR Open surgerywith steel plateto repair cranialperforation
Multiple(unspecified)
3 No
SARLANI, 200447 1 35 1 F 1 L Limited MIO, asymmetry of the TMJ 7 years MR Open surgerywith partialparotidectomy
Multiple (109) 6 No
HOLMLUND, 200323 9 24–81 7 F,2 M
6 R, 3 L TMJ pain and impaired mandibularfunction
8–72months
OPT(9/9 cases),MR (4/9),CT (3/9),AR (1/9)
Open surgery Multiple (3–80) 12–194 No

Syn
ovia
lch
on
dro
ma
tosis
of
the
TM
J751
ISHII, 200326 1 38 1 F 1 L Pain, swelling, reduced MIO 3 years CT Open surgery,calcification of thelateral pterygoidmuscle left in placeto avoid excessivebleeding
Multiple(unspecified)
120 No
ROOTKIN-GRAY,200346
1 56 1 M 1 R Pain, swelling, trismus N.S. ST Open surgery Multiple(110)
18 No
SHIBUYA, 200350 1 51 1 F 1 R Pain, reduced MIO N.S. ST Open surgerywith diskectomy
Multiple(unspecified)
24 No
AYDIN, 20025 1 39 1 M 1 L Intermittent pain, mass over thezygomatic arch
3 years CT, MR Open surgerywith diskrepositioning
Multiple(unspecified)
24 No
SHIBUYA, 200252 1 57 1 F 1 R Pain, reduced MIO, mandibulardeflection to the affected side duringmovement
2 years MR, AR Arthroscopy Multiple(unspecified)
10 No
VON LINDERN, 200255 8 26–71 5 F, 3 M 4 R, 4 L Typical symptoms not present in allcases
N.S. CT, MR Open surgery withsynovectomy anddiskectomy
Multiple(unspecified)
N.S. N.S.
GAY-ESCODA, 200114 1 42 1 M 1 L Pain that increate with movements 3 years CT Open surgery withpartial synovectomyand remodelingcondylectomy
Multiple (4) 60 No
KOYAMA, 200129 2 47 2 F 2 L Pain, mandibular deviation toward theother side at rest
N.S. CT Open surgerywith diskectomy
Multiple(up to 95)
N.S. N.S.
YILDIZ, 200157 1 39 1 M 1 L Facial asymmetry, mobile perauricularmass
4 years MR, CT Open surgery Multiple(unspecified)
N.S. N.S.
MIYAMOTO, 200037 2 21–37 2 F 2 R Pain, reduced MIO, deflection on theaffected side during mouth opening
15–120months
MR (1 case),CT (1 case)
Arthroscopy(1 case) oropen surgery(1 case)
Multiple(2–20)
10–15 No
PETITO, 200043 4 31–63 4 F 3 R 1 L Pain, limited MIO, swelling 1–24months
CT(2/4 cases),MR (1/4),AR (1/4)
Open surgery Multiple(unspecified)
0–36 No
REDDY, 200044 1 64 1 M 1 L Infratemporal swelling N.S. CT, MR Open surgerywith cranialfossa repair
Multiple(unspecified)
N.S. No
SHIBUYA, 2000*,51 1 – – – – – – – – – –
ERCOLI, 199812 1 54 1 F 1 R Pain, swelling, occlusal changes, jointsounds
N.S. OPT, CT,MR
N.S. Multiple(unspecified)
3 No
GIL-SALU, 199815 1 65 1 F 1 L Sensory disturbances, pain, peripheralfacial nerve palsy
8 years CT, MR Open surgerywith skullbase repair
Singlegiant mass
15 No
KARLIS, 199828 1 45 1 F 1 R Pain, swelling, history of multipletrauma
N.S. CT Open surgery Multiple(unspecified)
N.S. N.S.
LOUIS, 199831 1 32 1 F 1 R ‘Fullness’ in the preauricular area 6 months CT, MR Unsuccessfularthroscopyfollowed byopen surgery
Multiple(15–20)
24 No
* Indicates the studies for which full text could not be achieved.

752 Guarda-Nardini et al.
A large variability in the number ofloose bodies removed from the joint spacewas described, ranging from two largebodies to over 200 small nodules. In mostcases, the exact number of loose bodieswas not provided, and only some genericdescriptions about their composition (cal-cified nodules) and location (mainly in theupper joint compartment) were given. Intwo cases, a single giant mass wasdescribed.
Follow up and recurrence rate
Follow-up data were provided only for 58cases, ranging from 1 month to 18 years.The recurrence rate was low, with onlyone case described in the literature. In twocases, corrective surgery was needed someweeks after the intervention. In one ofthose cases, injection of steroids wasneeded to achieve good pain relief, andin the other case, orthognathic surgery wasperformed to correct dental occlusion. Thepostoperative course was uneventful andeasily controlled with common pain killersand antibiotics and symptom improve-ment was achieved in most cases (54/58).
Discussion
A systematic assessment of the literatureon SC of the TMJ over the past decadeallowed the identification of 80 new casessince the last comprehensive review byVON LINDERN et al.55. 154 cases have beendescribed in 102 publications (Table 2).Most studies dealt with single case reports,and multiple case series describing from 2to 11 patients were seldom reported (15/102 publications). Females are affectedalmost three times more than males, andno changes in this trend could be identifiedby a comparison of the most recent andpast studies.
Both reviews described only studies inwhich surgery was performed as well as apost-surgical histopathological confirma-tion of diagnosis. This type of inclusioncriterion might have led to the exclusion of
Table 2. Summary of data from the present systVON LINDERN et al. (2002)55.
Thisreview
Nr. of studies reviewed 42Single case reports 34Total cases 80Male:female ratio 20:56**
Left:right joint ratio 37:40***
* = data were recounted on the basis of Tabl** = data are available only on 76 cases.*** = 1 bilateral case.**** = data were available on 68 cases.
some other potential cases of SC and bethe reason for some of the discrepancies inthe reviews of prevalence of SC of theTMJ27,30,47. The summary of data from thepresent review, which systematicallyassessed all available publications from1998 to the present, and that by VON LIN-
DERN et al.55, which covered most paperspublished before 1998, represent the bestavailable evidence for describing the epi-demiological features of the disease.
SC usually occurs in large joints, suchas the knee or shoulder. Its prevalence isvery low, with less than 300 cases beingreported in the literature41. It is a benign,chronic, and progressive condition thatdoes not seem to undergo spontaneousresolution, since the presence of multipleloose bodies with the joint space interfereswith function and requires surgicalremoval. In the case of larger joints, theclassical triad of signs and symptoms isrepresented by restricted joint range ofmotion (65%), pain (57%), swelling(46.5%), which are also the main signsand symptoms identified in cases of SC ofthe TMJ3. Pain and swelling were presentin most cases selected for this review, witha prevalence of up to about 90 and 80%,respectively, while limited range ofmotion was described in about 65% ofpatients.
Symptoms are often unspecific andhard to relate to SC, so late diagnosis iscommon10. Data on the duration of symp-toms before diagnosis and interventionwere not always reported, but the percen-tage of cases with long-lasting symptomsseems to be very high, since about 80% ofthe studies providing such data describedcases with symptoms lasting for morethan 2 years. Advanced imaging techni-ques, such as MRI and CT, may be helpfulfor depicting joint changes and the pre-sence of loose bodies, suggesting thediagnosis of SC21. MRI may be usefulfor depicting the nodules in the earlystages of formation, before ossification4,and for planning surgery in the earlystages.
ematic review of the literature and the one by
Review by VonLindern et al., 200210 Total
60 10253* 8774 15423:51* 43:107 (1:2.5)31:37**** 68:77 (1:1.1)
e 1 of the original report.
Surgery has always been recommendedas the therapy of choice10,35, but someauthors advocate less invasive techniques,such as arthroscopy and two-needlearthrocentesis, to remove the loose bodiesfrom the joint space9. Data from the pre-sent systematic review did not support thehypothesis that minor surgery may beenough to treat SC. The reported successrate for arthroscopy was no better than55%, since in almost half the cases com-plete removal of loose bodies from thejoint cavity was not achieved by arthro-scopy and needle aspiration alone, andopen surgery was needed to clear thesynovia thoroughly. Such observationsare in line with current suggestions thatTMJ arthroscopy has little place in themodern era of TMJ surgery, because ithas no advantage over arthrocentesis interms of efficacy and none over opensurgery in terms of post-surgicalcourse16,17.
In many cases, additional procedures,such as total synovectomy, diskectomyand condylectomy were performed forloose body removal alone; the choicehas to be based on the stage of the dis-ease10. From a histopathological view-point, the disease has been described interms of three distinct and progressivestages based on the phases of the meta-plastic process7,36. During the first stage ofthe disease there is active synovial meta-plastic activity without loose bodies; thesecond stage is characterized by the pre-sence of metaplastic nodules plus loosebodies; in the third stage there are multipleloose bodies but no signs of active syno-vial disease36. In cases characterized by anadvanced stage of the disease, in whichdegeneration and calcification of the loosebodies has taken place and there is aninactive synovial membrane, aggressivesurgery with synovectomy might not benecessary due to the non-proliferative nat-ure of the disease at this stage. Althoughcalcifications and ossifications of thenodules might have affected the diskand/or reached extra-articular structures,requiring extensive joint clearage as well.The literature data did not provide usefulinformation on the correlation between thestage of the disease and the type of surgi-cal intervention. It seems that the sur-geon’s experience is the maindeterminant of the additional proceduresto be performed as well as loose bodyremoval.
Once the loose bodies have beenremoved, the recurrence rate of SCappears to be very low. Only one caseof recurrence has been documented in theliterature11. This may suggest that sponta-

Synovial chondromatosis of the TMJ 753
neous inactivation of the metaplastic pro-cess occurs in most cases and that surgerymay be considered a radical and definitivetreatment for most SC patients, sincerecurrence was not reported even in caseswith incomplete removal of calcifica-tions26. A differential diagnosis of chon-drosarcoma should be considered becauseof the life-threatening features of chon-drosarcoma, which is a rare primarymalignancy of the TMJ, described in lessthan 20 cases48. Owing to the aggressivenature of SC cases for which a knownaetiology cannot be identified, it was sug-gested that primary cases may be neoplas-tic in origin and secondary casesmetaplastic in origin, thus representingmild and benign tumoral variants53.Malignant transformation of SC is veryrare, and only two cases have beenreported in other joints18,38, but somehistopathological signs of SC, such ascellular atypia, may easily be misinter-preted as signs of malignancy53.
The case report described in the presentpaper shares several aspects with most ofthe literature cases. Late diagnosis was afeature, in line with literature suggestions,and imaging techniques provided an accu-rate depiction of the joint and helped toplan surgery. Open surgery was selected asthe most suitable procedure to remove thelarge loose bodies identified with CT, andthe uneventful postoperative course sup-ports the benign prognosis and successfultherapeutic outcome described for allcases of SC of the TMJ.
Epidemiological data gathered by thissystematic review may help researchersidentify some shortcomings to beaddressed in future studies. Knowledgeon SC of the TMJ will be augmented byan improvement in the quality of the lit-erature on this disease. Information on thestages of the disease was lacking in manyof the reported cases included in thisreview as well as a detailed descriptionof the surgical technique used. Staging thedisease using the three-stage classificationis information that is easy to collect and itshould help to link the histopathologicalfindings with the extension of the diseaseand the type of surgical procedure. Betterinformation about the patient’s history, interms of anamnesis and symptom dura-tion, should be provided in future studies,to identify the potential risk factors for theonset and progression of the disease. Thecase report described here shows howdifficult it is to identify risk factors. Nostudy has conducted a detailed investiga-tion of risk factors.
In conclusion, SC is a rare and benigndisease that rarely affects the TMJ. The
case of a patient presenting with the clas-sical signs and symptoms of SC has beendescribed and a systematic literaturereview over the past decade has beenpresented. 155 cases of SC of the TMJwere described, with a 2.5:1 female:maleratio and a mean age of about 46 years. Asingle case of bilateral localization as wellas a single case of disease in a patientunder 18 years were reported. A few casesof aggressive behaviour of the disease,with invasion of extra-articular structureswere described, but information is lackingon the relation of this extra-articularextension with time. Owing to the non-specific symptoms, late diagnosis is com-mon and in general over 2 years occurredbetween the symptom onset and surgicalintervention. Surgery is the treatment ofchoice. Additional procedures of syno-vectomy, diskectomy and condylectomyhave been used in some cases with noevidence-based relation with the aetiologyor the stage of the disease. Minor surgerytechniques, such as arthroscopy, have alow success rate owing to the difficulty ofremoving all the loose bodies using needleaspiration and should not be recom-mended as a treatment tool on the basisof the systematic assessment of the litera-ture. The recurrence rate is very low, withonly one case reported in the literature. Allthe information gathered through this sys-tematic assessment of the literature shouldbe used to relate the potential risk andprognostic factors to the least aggressivesurgical intervention.
Funding
None.
Competing interests
None declared.
Ethical approval
Not required.
References
1. Acar GO, Cansiz H, Guvenc MG,Mercan H, Dervisoglu S. Synovialchondromatosis of the temporomandibu-lar joint with skull base extension. J Cra-niofac Surg 2007: 18: 241–243.
2. Adachi PL, Kaba SP, Martins MT,Hueb CH, Shinohara EH. Arthrocent-esis in the treatment of loose bodies of thetemporomandibular joint associated withsynovial chondromatosis. Br J Oral Max-illofac Surg 2008: 46: 320–321.
3. Ardekian L, Faquin W, Troulis MJ,Kaban LB, August M. Synovial chon-
dromatosis of the temporomandibularjoint: report and analysis of eleven cases.J Oral Maxillofac Surg 2005: 63: 941–947.
4. Axhausen G. Pathologie und therapiedes kieferegelenks. Fortschr Zahnheilk1933: 9: 171–186.
5. Aydin MA, Kurtay A, Celebioglu S.A case of synovial chondromatosis of theTMJ: treatment based on stage of thedisease. J Craniofac Surg 2002: 13:670–675.
6. Balliu E, Medina V, Villanova J,Pelaez I, Puig J, trull JM, Pedraza
S. Synovial chondromatosis of the tem-poromandibular joint: CT and MRI find-ings. Dentomaxillofac Radiol 2007: 36:55–58.
7. Blankestijn J, Panders AK, Vermey
A, Scherpbier AJ. Synovial chondro-matosis of the temporomandibularjoint. Report of three cases and reviewof the literature. Cancer 1985: 55: 479–485.
8. Cai XY, Yang C, Chen MJ, Yun B.Simultaneous pigmented villonodularsynovitis and synovial chondromatosisof the temporomandibular joint: casereport. Int J Oral Maxillofac Surg 2009.10.1016/j.ijom.2009.06.014 (EPub aheadof print).
9. Carls FR, Hochstetter AV, Engelke
W, Sailer HF. Loose bodies in the tem-poromandibular joint: the advantages ofarthroscopy. J Craniomaxillofac Surg1995: 23: 215–221.
10. Clayman L. Surgical management ofbenign and malignant neoplasms. In:Laskin DM, Greene CS, Hylander
WL, eds: TMDs. An Evidence-basedApproach to Diagnosis and Treatment.Chicago, USA: Quintessence Publishing2006: 509–532.
11. D’Souza B, Dimitroulis G. A case ofrecurrence of synovial chondromatosis ofthe temporomandibular joint. Oral SurgOral Med Oral Pathol Oral Radiol Endod2007: 104: e59–e61.
12. Ercoli C, Boncan RB, Tallents RH,Macher DJ. Loose bodies of the tempor-omandibular joint: a case report. ClinOrthod Res 1998: 1: 62–67.
13. Fernandez-Sanroman J, Costas
Lopez A, Anton Badiola I, Fernan-
dez Ferro M, Lopez de Sanchez A.Indications of arthroscopy in the treat-ment of synovial chondromatosis of thetemporomandibular joint: report of 5 newcases. J Oral Maxillofac Surg 2008: 66:1694–1699.
14. Gay-Escoda C, Valmaseda-Castel-
lon E, Alaejos-Algarra C, Vaz-
quez-Rodriguez E. Condylarhyperplasia associated to synovial chon-dromatosis of the temporomandibularjoint: a case report. Cranio 2001: 19:91–95.
15. Gil-Salu JL, Lazaro R, Aldasoro J,Gonzalez-Darder JM. Giant solitarysynovial chondromatosis of the tempor-

754 Guarda-Nardini et al.
omandibular joint with intracranial exten-sion. Skull Base Surg 1998: 8: 99–104.
16. Goudot P, Jaquinet AR, Hugonnet S,Haefliger W, Richter M. Improvementof pain and function after arthroscopy andarthrocentesis of the temporomandibularjoint: a comparative study. J Craniomax-illofac Surg 2000: 28: 39–43.
17. Guarda-Nardini L, Ferronato G. TMJarthrocentesis. In: Manfredini D, ed:Current Concepts on TemporomandibularDisorders. Berlin: Quintessence Publish-ing 2010.
18. Hamilton A, Davis RI, Hayes CD,Mollam RAB. Chondrosarcoma devel-oping in synovial chondromatosis. J BoneJoint Surg Br 1987: 69: 137–140.
19. Hamilton JS, Jones-Quaidoo S,Osborne RF. Synovial chondromatosisof the temporomandibular joint space.Ear Nose Throat J 2005: 84: 342–343.
20. Hammodeh N, Nasser NA. Synovialchondromatosis of the temporomandibu-lar joint, presenting as parotid mass. JLaryngol Otol 2006: 120: e40.
21. Herzog S, Mafee M. Synovial chondro-matosis of the TMJ: MR and CT findings.Am J Neuroradiol 1990: 11: 742–745.
22. Hohlweg-Majert B, Metzger MC,Bohm J, Muecke T, Schulze D.Advanced imaging findings and compu-ter-assisted surgery of suspected synovialchondromatosis in the temporomandibu-lar joint. J Magn Reson Imaging 2008: 28:1251–1257.
23. Holmlund AB, Eriksson L, Reinholt
FP. Synovial chondromatosis of the tem-poromandibular joint: clinical, surgicaland histological aspects. Int J Oral Max-illofac Surg 2003: 32: 143–147.
24. Honda K, Yamada Y, Ejima K, Tsuki-
mura N, Kino K. Interventional radiol-ogy of synovial chondromatosis in thetemporomandibular joint using a thinarthroscope. Dentomaxillofac Radiol2008: 37: 232–235.
25. Huh JK, Park JY, Lee S, Lee SH, Choi
SW. Synovial chondromatosis of the tem-poromandibular joint with condylarextension. Oral Surg Oral Med OralPathol Oral Radiol Endod 2006: 101:e83–e88.
26. Ishii J, Kino K, Kobayashi J, Amagasa
T. Synovial chondromatosis of the tem-poromandibular joint: long-term post-operative follow-up of the residualcalcification. J Med Dent Sci 2003: 50:133–137.
27. Kademani D, Bevin C. A mass in thetemporomandibular joint. J Am DentAssoc 2008: 139: 301–303.
28. Karlis V, Glickman RS, Zaslow M.Synovial chondromatosis of the tempor-omandibular joint with intracranialextension. Oral Surg Oral Med OralPathol Oral Radiol Endod 1998: 86:664–666.
29. Koyama J, Ito J, Hayashi T, Kobaya-
shi F. Synovial chondromatosis in thetemporomandibular joint complicated
by displacement and calcification ofthe articular disk: report of two cases.Am J Neuroradiol 2001: 22: 1203–1206.
30. Lieger O, Zix J, Stauffer-Brauch EJ,Iizuka T. Synovial chondromatosis ofthe temporomandibular joint with cranialextension: a case report and literaturereview. J Oral Maxillofac Surg 2007:65: 2073–2080.
31. Louis PJ, West WF, Tilley MS, Waite
PD, Cuzalina LA. A case report, chon-dromatosis of the temporomandibularjoint. J Am Dent Assoc 1998: 129:1010–1013.
32. Lustman J, Zelster R. Synovial chon-dromatosis of the temporomandibularjoint. Review of the literature and casereport. Int J Oral Maxillofac Surg 1989:18: 90–94.
33. Mandrioli S, Polito J, Denes SA,Clauser L. Synovial chondromatosisof the temporomandibular joint. J Cranio-fac Surg 2007: 18: 1486–1488.
34. Martin-Granizo R, Sanchez JJ, Jour-
queira M, Ortega L. Synovial chondro-matosis of the temporomandibular joint: aclinical, radiological and histologicalstudy. Med Oral Patol Oral Cir Bucal2005: 10: 272–276.
35. Milgram JW. Synovial osteochondroma-tosis: a histopathological study of thirtycases. J Bone Joint Surg Am 1977: 59:792–801.
36. Milgram JW. The classification of loosebodies in human joints. Clin Orthop 1977:124: 282–291.
37. Miyamoto H, Sakashita H, Wilson
DF, Goss AN. Synovial chondromatosisof the temporomandibular joint. Br J OralMaxillofac Surg 2000: 38: 205–208.
38. Mullins F, Beard CW, Eisenberg SH.Chondrosarcoma following synovialchondromatosis. A case study Cancer1965: 18: 1180–1188.
39. Mupparapu M. Synovial chondromato-sis of the temporomandibular joint withextension to the middle cranial fossa. JPostgrad Med 2005: 51: 122–124.
40. Norman JE, Stevenson RL, Painter
DM, Sykes DG, Feain LA. Synovialchondromatosis of the temporomandibu-lar joint. An historical review with pre-sentation of three cases. JCraniomaxillofac Surg 1988: 16: 212–220.
41. O’Connell JX. Pathology of the syno-vium. Am J Clin Pathol 2000: 114: 773–779.
42. Peng LW, Yan DM, Wang YG, Li YD.Synovial chondromatosis of the tempor-omandibular joint: a case report withbilateral occurrence. J Oral MaxillofacSurg 2009: 67: 893–895.
43. Petito AR, Bennett J, Assael LA,Carlotti Jr AE. Synovial chondroma-tosis of the temporomandibular joint:varying presentation in 4 cases. OralSurg Oral Med Oral Pathol Oral RadiolEndod 2000: 90: 758–764.
44. Reddy PK, Vannemreddy PS, Gonza-
lez E, Nanda A. Synovial chondroma-tosis of the temporomandibular joint withintracranial extension. J Clin Neurosci2000: 7: 332–334.
45. Reyes Macias JF, Sanchez Prieto M.Synovial chondromatosis of the tempor-omandibular joint. Med Oral Patol OralCir Bucal 2007: 12: E26–E29.
46. Rootkin-Gray VF, Fryer L, Robinson
PD. ‘Mice’ in the joint. Br J Oral Max-illofac Surg 2003: 41: 199–200.
47. Sarlani E, Nikitakis NG, Papadimi-
triou JC, Ord RA. Synchronus occur-rence of ipsilateral synovialchondromatosis of the temporomandib-ular joint and pleomorphic adenoma ofthe parotid gland. Oral Surg Oral MedOral Pathol Oral Radiol Endod 2004:98: 69–75.
48. Sessana E, Tullio A, Ferrani S. Chon-drosarcoma of the temporomandibularjoint: a case report and review of theliterature. J Oral Maxillofac Sug 1997:55: 1348–1352.
49. Sembronio S, Albiero AM, Toro C,Robiony M, Politi M. Arthroscopy withopen surgery for treatment of synovialchondromatosis of the temporomandibu-lar joint. Br J Oral Maxillofac Surg 2008:46: 582–584.
50. Shibuya T, Kino K, Kitamura Y,Takahashi T. Synovial chondromatosisaccompanying an ossified articular disk inthe temporomandibular joint: a casereport. J Oral Pathol Med 2003: 32:441–442.
51. Shibuya T, Kino K, Okada N, Ama-
gasa T. Synovial chondromatosis of theleft temporomandibular joint superfi-cially resembling chondrosarcoma: acase report. Cranio 2000: 18: 286–288.
52. Shibuya T, Kino K, Yoshida S, Ama-
gasa T. Arthroscopic removal of nodulesof synovial chondromatosis of the tem-poromandibular joint. Cranio 2002: 20:304–306.
53. Stern D. Benign and malignant tumors.In: Laskin DM, Greene CS, Hylander
WL, eds: TMDs. An Evidence-basedApproach to Diagnosis and Treatment.Chicago, USA: Quintessence Publishing2006: 319–334.
54. Von Arx DP, Simpson MT, Batman P.Synovial chondromatosis of the tempor-omandibular joint. Br J Oral MaxillofacSurg 1988: 26: 297–305.
55. Von Lindern JJ, Theuerkauf I, Nie-
derhagen B, Berge S, Appel T, Reich
RH. Synovial chondromatosis of the tem-poromandibular joint: clinical, diagnosticand histomorphologic findings. Oral SurgOral Med Oral Pathol Oral Radiol Endod2002: 94: 31–38.
56. Xu WH, Ma XC, Guo CB, Yi B, Bao
SD. Synovial chondromatosis of the tem-poromandibular joint with middle cranialfossa extension. Int J Oral MaxillofacSurg 2007: 36: 652–655.

Synovial chondromatosis of the TMJ 755
57. Yildiz ST, Demir A, Kaya A. Synovialchondromatosis of the temporomandibu-lar joint extending to temporalis, masti-cator, and parotid spaces. J Comput AssitTomogr 2001: 25: 126–129.
58. Yokota N, Inenaga C, Tokuyama T,Nishizawa S, Miura K, Namba H.Synovial chondromatosis of the tempor-omandibular joint with intracranial exten-
sion. Neurol Med Chir (Tokyo) 2008: 48:266–270.
59. Zha W, Zhao YF, Liu Y, Jiang L. Acase of synovial chondromatosis of thetemporomandibular joint secondary topreauricular trauma. Int J Oral MaxillofacSurg 2009. 10.1016/j.ijom.2009.05.005(EPub ahead of print).
Address:Daniele ManfrediniViale XX Settembre 29854036 Marina di Carrara (MS)ItalyTel: +39 0585 630964E-mail: [email protected]