Superior management of oblique dysfunctiontion and superior oblique palsy.13 15 Theinci-dence of...
Transcript of Superior management of oblique dysfunctiontion and superior oblique palsy.13 15 Theinci-dence of...

British Journal of Ophthalmology 1995; 79: 661-663
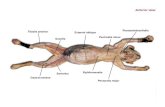
Superior oblique tendon expansion in themanagement of superior oblique dysfunction
M P Clarke, L C Bray, T Manners
AbstractTraditional superior oblique weakeningprocedures may be unpredictable andlead to superior oblique underaction. Theuse of 240 retinal band as a spacer tolengthen the superior oblique tendon hasbeen proposed as a more controlledapproach than superior oblique tenotomyand related procedures. The use of thistechnique is reported in a patient withdiplopia following an orbital floor blowout fracture, and in a child with Brown'ssuperior oblique tendon sheath syndrome.(BrJ7 Ophthalmol 1995; 79: 661-663)
Department ofOphthalmology, RoyalVictoria Infirmary,
Newcastle upon TyneNE1 4LPM P ClarkeL C BrayT Manners
Correspondence to:MrM P Clarke.Accepted for publication14 February 1995
Superior oblique weakening procedures usedin the treatment of superior oblique overactionand Brown's syndrome may be unpre-dictable.l Superior oblique tenotomy is vari-able in its efficacy and may be complicated bysuperior oblique paresis and inferior obliqueoveraction.35 Patients with fusion may sufferhead tilt, vertical or torsional diplopia, or lossof stereopsis following surgery.4To overcome some of these problems,
Wright5 has developed a new technique forweakening the superior oblique muscle bylengthening the superior oblique tendon usinga segment of 2 mm silicone retinal band.Manners et al have described its use in skewdeviation and superior oblique overaction.6We report two cases in which this technique
has been successfully employed. The firstpatient had an orbital blowout fracture, andthe second was a child with Brown's superioroblique tendon sheath syndrome.
~~~~~~~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ ~ AI
Figure Case 1. Preoperative nine gaze composite photograph. Note the marked rightsuperior oblque overaction.
Versions were quantified using a nine pointscoring system7 (-4 to +4). The amount ofAor V pattern was determined by comparing dis-tance alternate cover test measurements in 200upgaze and 200 downgaze.
Patients and methods
CASE 1A 46-year-old woman was seen in the eyedepartment 2 days after sustaining a left orbitalblowout fracture. Initial examination revealeda chin up head posture and restriction of leftelevation with a 20 dioptre right hypertropia inthe primary position. Two weeks after theinjury, there was no improvement in elevationof the left eye, and in addition restriction ofdepression of the left eye was apparent. A com-puted tomography (CT) scan demonstrated alarge orbital floor fracture, with herniation oforbital contents into the maxillary antrum. Theorbital floor was explored 1 month after theinjury, entrapped tissue was freed, and thedefect repaired with Silastic. There was littlechange in ocular motility following this pro-cedure, and a subsequent CT scan demon-strated persistent herniation of tissue throughthe fracture site. A further operation was per-formed 9 months after the original injury, anda bony defect was found posterior to the limitof the original Silastic sheet which wasreplaced.Three months after the second orbital pro-
cedure, there was no diplopia in the primaryposition, but there was limitation of verticalductions of the left eye with a small field ofbinocular single vision (Figs 1 and 2). Therewas a right superior oblique overaction of +3.A forced duction test showed limitation ofupward movement of the left eye, and a forcegeneration test demonstrated inferior rectusfunction. Diplopia in downgaze was particu-larly troublesome.To improve the field of binocular single
vision in downgaze, a right superior obliquetendon expansion of 6 mm was performed.The outcome is discussed in the resultssection.
CASE 2A 7-year-old boy was seen in the eye depart-ment from the age of 3 years with a rightBrown's syndrome. There was a rightesotropia of 30 prism dioptres in the primaryposition and a -4 limitation of elevation inadduction of the right eye (Fig 5, preopera-tive). There was no spontaneous improve-ment over the subsequent 4 years, and his
661
on July 4, 2020 by guest. Protected by copyright.
http://bjo.bmj.com
/B
r J Ophthalm
ol: first published as 10.1136/bjo.79.7.661 on 1 July 1995. Dow
nloaded from

Clarke, Bray, Manners
NusCaUNCHANT
DIGNOSIS Gnb lsh Ey
Figure 2 Case 1. Preoperative Hess chart.
Figure 3 Case 1. Postoperative nine gaze composite photograph taken 10 days aftersurgery. Note the significant reduction in right superior oblique overaction.
Figure 4 Case 1. Postoperative Hess chart recorded 10 days after surgery.
parents requested surgery because the boywas teased at school about his appearance.Under general anaesthesia, forced duction
testing confirmed the diagnosis of Brown'ssyndrome. The right superior oblique tendonwas lengthened 7 mm using a 40 retinaldetachment band. After this procedure, eleva-tion of the right eye was improved, but thehorizontal deviation was increased. At a
second procedure, both medial recti were
recessed 4 mm.
SURGICAL TECHNIQUE FOR SUPERIOR OBLIQUETENDON EXPANSIONThe surgical technique described by Wright5uses a modified Park's temporal approach8through which the superior oblique muscle isisolated. The tendon is exposed through asmall incision in the roof of the superioroblique capsule, while preserving the floor ofthe capsule. The segment of silicone is suturedbetween the cut ends of the tendon withdouble armed 5-0 Mersilene suture placed 2 to3 mm nasal to the superior rectus muscle.The length of silicone expander used was
determined by the degree of superior obliqueoveraction, thus 3 to 4 mm for +2, 5 mm for+2, 6 mm for +3, and 7 mm for +4. A 6 or 7mm expander was used in patients with Brownsyndrome and intraoperative forced ductiontests performed to verify that restriction hadbeen adequately relieved.
ResultsIn case 1, superior oblique overaction waseliminated, resulting in a marked sympto-matic improvement and increased comitance.Figure 3 shows the appearance 2 months aftersurgery, and Figure 4 shows the Hess chart1 year after superior oblique tendon expansion,and 2 years following the original injury.The field of binocular single vision was
scored for complete, superior, and inferior halffields, using the method described byWoodruff et al.9 The complete field score wasimproved from 66% preoperatively to 81% at6 months after surgery. These overall scoresmasked the dramatic effect of the surgery onthe inferior half field which improved from67% preoperatively to 97% at 6 months aftersurgery. The scores for superior half fields were64% preoperatively and 53% 6 months aftersurgery. This overall improvement has beenmaintained over the 2 year follow up.The marked improvement in cosmetic
appearance 1 year after surgery in case 2 is seenwhen comparing Figures 5 and 6. There was asmall right hypertropia and right esotropia inall gaze positions, but the cosmetic appearancewas much improved and considered satisfac-tory by the parents.
DiscussionThe technique of superior oblique tendonexpansion described by Wright allows a gradedreduction in superior oblique overaction to beachieved thereby reducing the incidence ofpostoperative palsy or residual overaction.8The two cases reported illustrate some of theadvantages of the technique.
In case 1, orbital blowout fracture was com-plicated by diplopia which persisted despiteearly repair of the orbital floor. Diplopia islikely to have been the result of either directmuscle or nerve damage, or scarring and fixa-tion of previously entrapped tissue.10The surgical options were an inverse Knapp
procedure on the affected eye or a contralateralsuperior oblique weakening procedure. Ainverse Knapp procedure may improve both
662
GC_E1w-RiMy
on July 4, 2020 by guest. Protected by copyright.
http://bjo.bmj.com
/B
r J Ophthalm
ol: first published as 10.1136/bjo.79.7.661 on 1 July 1995. Dow
nloaded from

Superior oblique tendon expansion in the management ofsuperior oblique dysfunction
I
Figure 6 Postoperative eye movements case 2
superior and inferior fields of binocular singlevision in patients with inferior rectus paresis, 11
but risks aggravating diplopia in the primaryposition. A weakening procedure on the con-tralateral superior oblique muscle was felt to bethe best method of reducing incomitance indowngaze and as the patient had fusion, thesilicone expander procedure was felt to be
most appropriate. There was no diplopia dueto excyclotorsion postoperatively. We recom-mend that it is considered as a surgical optionin patients with persistent diplopia followinginferior orbital wall blowout fractures.
Brown's syndrome often requires no surgicalintervention and spontaneous resolution isreported in 10% of cases.12 However, whensurgical treatment is required, results areunpredictable. 13-15 Superior oblique tenotomyis frequently associated with both undercorrec-tion and superior oblique palsy.13 15 The inci-dence of palsy can be reduced by ipsilateralinferior oblique recession but this may furtherreduced elevation in adduction.15 When thesilicone expander technique is used, inferioroblique weakening is unnecessary. The goodand stable cosmetic result achieved by the useof a silicone expander is matched by reports inthe literature.13The authors thank Mrs A Smith for secretarial help.
1 Urist MJ. Complications following bilateral superior obliqueweakening surgical procedures for A-pattern horizontaldeviations. Am J Ophthalmol 1970; 70: 583-7.
2 Souza-Dias C, Uesugui CF. Efficacy of different techniquesof superior oblique weakening in the correction of 'A'anisotropia. J Pediatr Ophthalmol Strabismus 1986; 23:82-6.
3 Scott WE, Jampolsky AJ, Redmond MR. Superior obliquetenotomy: indications and complications. Int OphthalmolClin 1976; 16: 151-9.
4 Parks MM. Commentary on superior oblique tenotomy forA-pattem strabismus in patients with fusion. BinocularVision 1988; 3: 39.
5 Wright KW. Color atlas of ophthalmic surgery: strabismus.Philadelphia: JB Lippincott, 1991: 201-16.
6 Manners RM, O'Flynn E, Morris RJ. Superior obliquetendon lengthening for acquired superior oblique over-actions. BrJ Ophthalmol 1994; 78: 280-4.
7 Doughty DD, Lennarson LW, Scott WE. A graphicportrayal of versions. Perspect Ophthalmol 1978; 2:55-9.
8 Parks MM. Atlas of strabismus surgery. Philadelphia: Harper& Row, 1983: 191.
9 Woodruff G, O'Reilly C, Kraft SP. Functional scoring ofthe field of binocular single vision in patients withdiplopia. Ophthalmology 1987; 94: 1554-61.
10 Koomeef L. Current concepts on the management oforbital blow-out fractures. Ann Plast Surg 1982; 9:185-200.
11 Lipton JR, Page AB, Lee JP. Management of diplopia ondowngaze following orbital trauma. Eye 1990; 4: 535-7.
12 Kaban TIJ, Smith K, Orton RB, Noel LP, Clarke W, CaderaW. Natural history of presumed congenital Brown syn-drome. Arch Ophthalmol 1993; 111: 943-6.
13 Wright KW, Min B-M, Park C. Comparison of superioroblique tendon expander to superior oblique tenotomy forthe management of superior oblique overaction andBrown syndrome. Jf Pediatr Ophthalmol Strabismus 1992;2: 92-7.
14 Crawford JS. Surgical treatment of true Brown's syndrome.AmJ Ophthalmol 1976; 81: 289-95.
15 Parks MM, Eustis HS. Simultaneous superior obliquetenotomy and inferior oblique recession in Brown's syn-drome. Ophthalmology 1987; 94: 1043-8.
663
:40%
on July 4, 2020 by guest. Protected by copyright.
http://bjo.bmj.com
/B
r J Ophthalm
ol: first published as 10.1136/bjo.79.7.661 on 1 July 1995. Dow
nloaded from














![EfficacyofManipulativeAcupunctureTherapyMonitoredbyLSCI ...Bell’s palsy is an acute peripheral facial nerve palsy of un-knowncauseandaccountsfor50%ofallcasesoffacialnerve palsy [1].](https://static.fdocuments.in/doc/165x107/60a4deb9e0003e748e568e41/efficacyofmanipulativeacupuncturetherapymonitoredbylsci-bellas-palsy-is-an.jpg)