Stroke-2003-Bhogal-987-93
-
Upload
paula-quezada -
Category
Documents
-
view
215 -
download
0
Transcript of Stroke-2003-Bhogal-987-93

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 1/8

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 2/8
Intensity of Aphasia Therapy, Impact on Recovery
Sanjit K. Bhogal, BA (Hon); Robert Teasell, MD; Mark Speechley, PhD
Background —It has been speculated that the conflicting results demonstrated across poststroke aphasia therapy studiesmight be related to differences in intensity of therapy provided across studies. The aim of this study is to investigate the
relationship between intensity of aphasia therapy and aphasia recovery.
Methods—A MEDLINE literature search was conducted to retrieve clinical trials investigating aphasia therapy after stroke.
Changes in mean scores from each study were recorded. Intensity of therapy was recorded in terms of length of therapy,
hours of therapy provided per week, and total hours of therapy provided. Pearson correlation was used to assess the
relationship between changes in mean scores of outcome measures and intensity of therapy.
Results—Studies that demonstrated a significant treatment effect provided 8.8 hours of therapy per week for 11.2 weeks
versus the negative studies that only provided 2 hours per week for 22.9 weeks. On average, positive studies provided
a total of 98.4 hours of therapy, whereas negative studies provided 43.6 hours of therapy. Total length of therapy time
was found to be inversely correlated with hours of therapy provided per week (P0.003) and total hours of therapy
provided (P0.001). Total length of therapy was significantly inversely correlated with mean change in Porch Index of
Communicative Abilities (PICA) scores (P
0.0001). The number of hours of therapy provided in a week wassignificantly correlated to greater improvement on the PICA (P0.001) and the Token Test (P0.027). Total number
of hours of therapy was significantly correlated with greater improvement on the PICA (P0.001) and the Token Test
(P0.001).
Conclusions—Intense therapy over a short amount of time can improve outcomes of speech and language therapy for
stroke patients with aphasia. (Stroke. 2003;34:987-993.)
Key Words: aphasia cerebrovascular accident therapy treatment outcome
The Agency for Health Care Policy and Research Post-
Stroke Rehabilitation Clinical Practice Guidelines1 de-
fine aphasia as “the loss of ability to communicate orally,
through signs, or in writing, or the inability to understandsuch communications; the loss of language usage ability.”
Darley2 noted that aphasia is generally described as an
impairment of language resulting from focal brain damage to
the language-dominant cerebral hemisphere. This serves to
distinguish aphasia from the language and cognitive-
communication problems associated with non–language-
dominant hemisphere damage, dementia, and traumatic brain
injury.3 However, defining aphasia as purely a disorder of
language may oversimplify a complex clinical entity.
Kertesz4 clinically described aphasia as a “neurologically
central disturbance of language characterized by paraphasias,
word finding difficulty, and variably impaired comprehen-
sion, associated with disturbance of reading and writing, attimes with dysarthria, non-verbal constructional and problem-
solving difficulty and impairment of gesture.”
The most effective means of treating aphasia after stroke
has yet to be determined, and studies investigating the
efficacy of speech and language therapy (SLT) for patients
See Editorial Comment, page 992
suffering aphasia after stroke have yielded conflicting results.
One possible explanation for the observed heterogeneity of findings across studies is a difference in intensity of thera-
py.5,6 We have noted that the failure to identify a consistent
benefit might have been due to the low intensity of SLT
applied in the negative studies, whereas higher intensities of
therapy were present in positive studies.7 A meta-analysis that
included all patients suffering from aphasia, not just stroke
patients, revealed that the more intensive the therapy, the
greater the improvement.8
The objective of the present study is to investigate the
relationship of intensity of aphasia therapy and aphasia
recovery after stroke. Using published studies of SLT, this
study attempts to quantify treatment intensity and determine
whether, in fact, intensity correlates with outcome results.
Methods
Study Identification and SelectionA MEDLINE literature review was conducted to identify controlledtrials that investigated SLT for aphasia after stroke published
Received July 2, 2002; accepted October 22, 2002.From the Department of Physical Medicine and Rehabilitation (S.K.B., R.T.) and Department of Epidemiology and Biostatistics (M.S.), University of
Western Ontario, and St Joseph’s Health Care London (S.K.B., R.T.), Parkwood Hospital, London, Ontario, University of Western Ontario, London,
Ontario, Canada.Correspondence to Dr Robert Teasell, 801 Commissioners Rd East, London, Ontario N6C 5J1, Canada. E-mail [email protected]
© 2003 American Heart Association, Inc.Stroke is available at http://www.strokeaha.org DOI: 10.1161/01.STR.0000062343.64383.D0
987 by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 3/8
between January 1975 and May 2002. All searches used the limitterms human, adult , and English. The following MEDLINE searchwords were used: aphasia, stroke, speech therapy or languagetherapy or speech and language therapy, and treatment , as well asthe combined exploded key words stroke and aphasia and speechtherapy or language therapy or speech and language therapy andtreatment .
Articles identified in the MEDLINE literature search were in-
cluded in the present analyses if the study compared conventionalSLT with treatment of a comparative control group. If the compar-ative control group underwent an altered form of conventional SLT,then the duration of that therapy had to be of the same duration as theSLT. Articles were limited to stroke survivors suffering from aphasiaafter stroke, and studies that included patients with traumatic braininjury or any other disorders or illnesses were excluded. Studies thatprovided a drug and/or placebo as an adjunct to therapy were alsoexcluded from the present review.
After each citation was identified through the literature search, asingle investigator (R.T.) reviewed the corresponding abstract toassess the suitability for inclusion. All articles that appeared to betreatment based were considered. The article was examined a finaltime by the study coordinator to verify that at least 1 treatmentintervention had been assessed. Five studies were eventually deemedsuitable for inclusion. Studies cited in review articles and in retrieved
articles but not identified through the MEDLINE search were alsosought. Five more articles were found this way, bringing the totalnumber of articles meeting the inclusion criteria to 10.
Data AbstractionSeveral independent reviewers were used to extract data from theselected studies. Two abstractors, each blinded to the other’s results,reviewed each article independently. The review process consisted of the following 2 parts. (1) First, data were collected pertaining tostudy methodology, identification of outcome measures, results, andfinal conclusions. Data were typed into a computer-generated formto avoid identifying the abstractor via handwriting. (2) A qualityrating score was assigned. The quality rating scale used was thePhysiotherapy Evidence Database (PEDro) scale, developed by theCentre for Evidence-Based P hysiotherapy in A us tralia
(http://www.pedro.fhs.usyd.edu.au/).PEDro was developed for the purpose of accessing bibliographicdetails and abstracts of randomized controlled trials, quasirandom-ized studies, and systematic reviews in physiotherapy. Studiesincluded in this review using a nonexperimental design could not beassigned a PEDro score and were given a designation of no score.The PEDro Scale consists of 10 quality ratings, each receiving eithera yes or no score. The maximum score a study could receive was 10.Two independent raters reviewed each article, and a third reviewerresolved any scoring discrepancies between the 2 raters. The scoreprovided by the third reviewer constituted the final PEDro score.
Statistical AnalysisThe abstracted data (treatment type, length of therapy period in hoursand weeks, and mean change in scores for outcome measures) wereentered into SPSS 10.1 for Windows. An independent t test was usedto determine differences of mean scores and length of treatmentbetween the studies yielding positive results and those yieldingnegative results. Pearson bivariate correlation was used to determinethe association between mean change in scores for outcome mea-sures and the intensity of therapy (length of therapy period and hoursof therapy provided per week).
Several articles presented their results graphically. The graphsfrom these articles were scanned and entered into Microsoft Paint as.jpg files. The bitmap coordinates of the graphs were then recorded,and the individual values estimated relative to the bitmap coordinatesof the y axis.
Results
Summary of Individual Studies
Ten studies investigating the SLT for stroke patients sufferingfrom aphasia met criteria after being reviewed. These 10
studies represented 864 individual patients. A brief descrip-
tion of each article follows.
Meikle et al9 compared the progress of 31 acute stroke
patients with dysphasia receiving conventional speech ther-
apy from either a qualified speech therapist or a nonprofes-
sional volunteer. Patients received a minimum of 3 and a
maximum of five 45-minute sessions per week. Length of
treatment was not defined, and therapy sessions were discon-
tinued when the therapist felt that the patient had not
improved in 2 consecutive sessions. There were no significant
differences in treatment results between the 2 groups. Both
treatment regimes appeared to provide the same benefits.
David et al10 compared the effects of speech therapists and
untrained volunteers on recovery from aphasia in the acute
phase after stroke. One hundred fifty-five patients received 30
hours of therapy over 15 to 20 weeks. Although patients in
both treatment groups improved, there was no overall differ-
ence in the amount of progress between the groups. However,
patients who were referred to treatment late (the median
interval between onset of stroke and starting treatment was 20weeks) began treatment at a level similar to that of the other
patients and showed an identical recovery pattern. This
suggested that treatment, and not spontaneous remission, was
responsible for the majority of the improvement experienced
in these patients.
Lincoln et al11 examined whether speech therapy produced
a better language outcome than natural recovery alone in 327
acute stroke patients with aphasia. Patients in the treatment
group received two 1-hour sessions of therapy per week for
24 weeks. Comparison of group results on the Porch Index of
Communicative Abilities (PICA) and the Functional Com-
munication Profile (FCP) revealed no significant difference
between treated and nontreated patients. Thus, speech therapydid not improve language functioning more than what was
achieved by spontaneous recovery. The treatment regime that
was used, which was representative of clinical practice, was
determined not to be effective for aphasic patients.
Shewan and Kertesz12 investigated 3 types of speech
therapy and compared its effects in 100 acute aphasic stroke
patients who received no speech or language therapy. Patients
who recovered their language skills within 2 to 4 weeks after
onset were excluded from the study. Treatment was provided
in three 1-hour sessions per week for 1 year. Shewan and
Kertesz12 noted no difference in Western Aphasia Battery
scores, its subsets Language Quotient (LQ) and Cortical
Quotient (CQ) scores, or the Auditory Comprehension Test
for Sentences scores, between groups. When treated patients
were compared with controls, Language Quotient scores of
patients in the treatment groups were significantly higher
compared with the control groups. Individually, the language-
oriented therapy and stimulation-facilitation therapy patients
significantly improved compared with the control patients,
but no significant differences were observed between the
unstructured-settings group and the control group. In addi-
tion, the CQ scores of the treatment groups were significantly
higher compared with patients in the control group. Individ-
ually, stimulation-facilitation therapy patients had higher CQ
scores than the controls, but the language-oriented therapyand unstructured-settings groups were not significantly dif-
988 Stroke April 2003
by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 4/8
ferent from the controls. The authors of this study suggested
that comparisons of treated patients with untreated aphasic
patients demonstrated that treatment was a significant factor
in improvement.Wertz et al13 compared the efficacy of clinic, home, and
deferred language treatment for aphasia in 121 patients
between 2 and 24 weeks after onset. Patients received 8 to 10
hours of therapy a week for 12 weeks. The authors noted that
at 12 weeks, clinic-treated patients made significantly more
improvement on the PICA than did the deferred patients,
whereas improvement in the home-treated patients did not
differ significantly from either the clinic-treated or deferred-
treatment patients. At 24 weeks, no differences were noted on
the PICA between all groups. On the basis of these results,
Wertz et al13 concluded that clinic treatment for aphasia was
efficacious, and delaying treatment for 12 weeks did not
compromise the ultimate improvement in aphasic patients.Hartman and Landau14 compared conventional speech
therapy provided by professional speech pathologists with
emotional supportive counseling therapy in 60 stroke patients
1 month after onset. Therapy was provided twice a week for
6 months. Change scores on the PICA revealed no significant
differences between the groups. Hartman and Landau14 as-
serted that conventional speech therapy was no more effec-
tive than emotional support.
Brindley et al5 investigated the speech of 10 patients with
chronic Broca’s aphasia after intensive speech therapy. Pa-
tients were provided 5 hours of therapy over 5 days a week
for 12 weeks. There was significant improvement on the FCP
subscales in movement, speech, reading, and overall score
during the intensive period. There was a significant ratio of
improvement (ratio of the score at the end of a period to that
at the start) on FCP between the intensive period and a second
nonintensive period in movement, speech, and overall score.
In addition, the Language Assessment Remediation and
Screening Procedure showed significant improvement during
the intensive period on sentence length increase, a reduction
in element omission, and an increase in percentage of full
utterances. Thus, the authors of the study concluded that
intensive therapy improves speech recovery 1-year after onset
of aphasia for some patients.
Marshall et al15
investigated the impact of home treatmentfor 121 aphasic patients between 2 to 24 weeks after onset by
trained nonprofessionals. Patients received 8 to 10 hours of
therapy a week for 12 weeks at 2 to 24 weeks after onset. The
authors observed that at 12 weeks the SLT group showed
significantly more improvement than the deferred-treatmentgroup. However, improvements noted in the home-treatment
group did not differ from those in the SLT group. The authors
further noted that at 24 weeks, the deferred-treatment group
caught up to the other 2 groups and no significant differences
between the groups were observed.
Poeck et al6 evaluated the outcome of intensive language
treatment in 160 acute and chronic aphasic inpatients. Patients
undertook 9 hours of therapy a week for 6 to 8 weeks. These
patients were compared with a group of aphasic stroke patients
who received no aphasia therapy. The authors of the study
observed that the mean gain on each measure of the Aachen
Aphasia Test improved substantially for both the treated and the
control group. However, with intensive therapy, 78% of the
patients treated up to 4 months after onset versus 46% of the
patients treated from 4 to 12 months after onset improved
beyond that expected with spontaneous recovery.
Prins et al16 compared the effectiveness of systematic
aphasia therapy that was organized on 4 levels (nonverbal,
phonology, lexical semantics, and morphosyntax) with the
effectiveness of conventional therapy. Thirty-two stroke pa-
tients exhibiting aphasia for at least 3 months were included
in the study. Patients receiving systematic aphasia therapy
were compared with aphasic stroke patients receiving con-
ventional SLT and with patients receiving no aphasia therapy.
Patients in this study received only 2 therapy sessions perweek for 5 months. Multiple regression analysis revealed that
there were no significant differences between the groups on
all evaluations. Moreover, neither the systematic aphasia
therapy nor the conventional therapy had any effect on the
recovery progress of the study patients.
Of the 10 studies reviewed, 5 were positive studies and 5
were negative studies (see Table 1). When examining the
outcomes related to the amount of therapy provided, it
appears the positive studies provided an average of 7.8 (5 to
10) hours of therapy per week for 18 (8 to 12) weeks
compared with the negative studies that only provided 2.4
(2 to 3.8) hours per week for 22.9 (20 to 26) weeks.Moreover, total number of hours of therapy was, on average
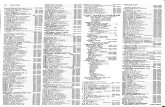
TABLE 1. Intensity of Aphasia Therapy Poststroke and Its Impact
Authors, Year PEDro Score
n at
Randomization Intensity of Therapy
Impact of Aphasia
Therapy vs Control
Lincoln et al, 1984 6 327 Two 1-hour sessions per week for 34 weeks
Wertz et al, 1986 6 121 8 to 10 hours a week for 12 weeks
Marshall et al, 1989 6 121 8 to 10 hours a week for 12 weeks
Hartman and Landau, 1987 6 60 2 times a week for 6 months
David et al, 1982 5 155 30 hours over 15 to 20 weeks
Shewan and Kertesz, 1984 5 100 Three 1-hour sessions a week for 1 year
Prins et al, 1989 5 32 2 sessions a week for 5 months
Meikle et al, 1979 4 31 Minimum of 3 and maximum of 5 sessions a week of 45 minutes
Brindley et al, 1989 4 10 5 hours over 5 days a week for 12 weeks
Poeck et al, 1989 Not scored 160 9 hours a week for 6 to 8 weeks
Bhogal et al Intensity of Aphasia Therapy 989
by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 5/8
108 (60 to 156) hours in the positive studies versus only 43.6
(30 to 52) hours in the negative trials.
Relationship Between Intensity of TherapyProvided and Outcome of StudyWe next wanted to determine whether there was in fact a
correlation between intensity of therapy provided and the
outcome of a study. The target outcome measures were the
Token Test, PICA, and FCP, which were the scales most
often used by the reviewed studies. The Token Test, PICA,
and FCP were used in 3, 4, and 3 studies respectively. As
such, Shewan and Kertesz,12 a positive study, was excluded
from the analysis because this study did not use any of the
targeted outcome measures. Although Meikle et al,9 a nega-
tive study, did use the PICA, the authors did not provide point
measures or measures of variability of their results; therefore,this study was excluded from our analysis. Two studies
provided their results in graph format.10,11 The bitmap coor-
dinates of the mean scores from these studies were recorded
and their values calculated relative to the bitmap coordinates
of the y axis.
Eight studies, therefore, provided the appropriate data to
allow determination of the relationship between intensity of
therapy provided and outcome (see Table 2). Four studies
yielded positive results,5,6,13,15 and 4 yielded negative
outcomes.10,11,14,16
Of the 4 positive trials analyzed,5,6,13,15 intensive practice
(mean, 8.8 hours a week) was provided over a short amount
of time (mean, 11.2 weeks), thereby accumulating an averageof 98.4 hours of total therapy time. In the 4 negative studies
analyzed,10,11,14,16 less intense practice (mean, 2.0 hours a
week) was provided for a longer duration (mean, 22.9 weeks),
accumulating an average of 43.6 hours of total therapy time
(see Table 3). In the positive studies, significantly more hours
of therapy per week and significantly more total therapy
hours in a significantly shorter period of time were provided,
as compared with the negative studies.
Total length of therapy time was inversely correlated with
hours of therapy provided per week (r 0.639, P0.003,
n19). Moreover, hours of therapy provided in a week was
significantly correlated to total hours of therapy provided
(r 0.542, P0.016). In other words, the shorter the overall
therapy period was, the more hours of therapy provided in a
week. The more hours of therapy provided per week, the
greater the total hours of therapy provided over the study’s
duration. Stated differently, in studies in which the overall
length of treatment was shorter, the therapy was more
intensive. As such, the positive studies, which were signifi-cantly shorter in duration, were more intensive than the
negative studies, which were longer in duration.
The positive studies demonstrated a mean improvement in
both the PICA13,15 and Token Test6,15 scores of 15.13 (SD,
3.06) and 13.74 (SD, 8.67), respectively. The negative studies
demonstrated mean improvement on the PICA11,15 and Token
Test16 scores of 1.37 (SD, 0.52) and 0.59 (SD, 0.78),
respectively (see Table 3). The mean improvements in both
PICA and Token Test scores were significantly different
between the positive and negative resultant studies (see Table 3).
Brindley et al5 provided their results in terms of ratio of
improvement (ratio of the FCP scores at the end of treatment
period to the FCP at the start). A ratio of 1 indicates animprovement, whereas a ratio of 1 indicates decline over
time. Because change scores could not be retrieved from this
article,5 we decided to convert the FCP scores of David et al10
TABLE 2. The 8 Studies Analyzed for Association Between Intensity of Therapy
and Aphasia Recovery
Study
Hours per
Week
Therapy Length
(weeks)
Total Hours
of Therapy
Measures
Used
Impact of
Therapy
David et al10 20 30 FCP
Lincoln et al11 2 24 48 PICA
FCP
Wertz et al13 10 12 120 PICA
Hartman and Landau14 2 26 52 PICA
Brindley et al5 5 12 60 FCP
Marshall et al15 10 12 120 PICA
Token Test
Poeck et al6 9 8 72 Token Test
Prins et al16 2 22 44 Token Test
TABLE 3. Comparing Intensity of Therapy Between Positive and Negative Resultant Studies
Therapy Measures Mean (SD) Outcome Measures Mean (SD)
Length (weeks) Hours (per week) Total (hours) PICA Token Test
Positive studies n259 11.2 (1.7) 8.8 (2.0) 98.4 (28.2) 15.1 (3.1) 13.74 (6.67)
Negative studies n574 22.9 (2.3) 2.0 43.6 (8.3) 1.37 (1.37) 0.59 (0.79)
t statistic 12.80 8.72 5.61 8.79 2.561
P value 0.001 0.001 0.001 0.001 0.05
990 Stroke April 2003
by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 6/8
and Lincoln et al11 to ratio factors as well. Brindley et al5
noted a significant ratio of improvement on overall FCP
scores between groups (1.10 versus 0.97, P0.01), whereas
the ratio of improvement on FCP scores was not significant
between groups in the David et al10 (1.54 versus 1.53) and
Lincoln et al11 (1.14 versus 1.14) studies. As such, the mean
ratio of improvement in FCP for group in the negative
trials10,11 was 1.34 (SD, 0.23), whereas for the positive trial5
it was 1.04 (SD, 0.09). The difference in scores between the
negative and positive trials was not statistically significant(P0.16). Because no significant differences in FCP scores
were noted between the negative and positive trials, no
further analysis using the FCP was attempted.
Analysis revealed that the total length of therapy was
significantly inversely correlated with mean change in
PICA11,13,14,15 scores (r 0.948, P0.0001, n9). That is,
the shorter the therapy period, the greater the change in PICA
scores. This trend was also evident when we looked at the
Token Test6,15,16 change scores, (r 0.581, P0.17, n7),
although it failed to achieve statistical significance (see Table
4). In addition, the hours of therapy provided in a week was
significantly correlated to greater improvement on the PICA
(r 0.957, P0.001, n9) and on the Token Test (r 0.811,P0.027, n7).
As noted earlier, total hours of therapy received was
significantly greater in the shorter, more intense studies that
provided positive results compared with the negative result-
ant studies. Total hours of therapy were significantly corre-
lated with mean change in PICA (r 0.958, P0.0001, n9)
and Token Test scores (r 0.963, P0.0001, n7). As such,
the more hours of therapy provided, the greater the improve-
ment in PICA and Token Test scores noted.
DiscussionFour of the 8 reviewed studies that reported significantly
positive results5,6,13,15 provided an average of 8.8 hours of
therapy per week for 11.2 weeks compared with the 4
negative studies10,11,14,16 that only provided approximately
two 1-hour sessions per week for 22.9 weeks. Analysis
revealed that the more intensive therapies (those that pro-
vided greater hours of therapy per week) resulted in the
improved outcomes. Significant improvement in PICA and
Token Test scores was associated with more intense therapy.
Unfortunately, analysis using the FCP did not yield a
similar pattern. Although Brindley et al5 noted significant
between-group differences in their study, there was no sig-
nificant difference in groups’ scores of the negative trials
versus the positive study. It should be noted that although theFCP is a widely used assessment of functional language, it is
a rather subjective instrument consisting of interviews and
observations of patients.
Constraint-induced (CI) aphasia therapy has as its hallmark
feature intense therapy for patients suffering from aphasia.
The use of intensive practice for short time intervals is
preferred over long-term, less frequent training in CI aphasia
therapy. The impact of intense therapy using the CI paradigm
was demonstrated by the Pulvermuller et al17 study, in which
patients receiving CI therapy (3 hours of therapy per day for
2 weeks) significantly improved on all outcome measures
compared with the patients receiving conventional therapy
who showed no significant improvement.
Earlier researchers have observed the association between
intensive therapy and improved aphasia outcomes. Brindley
et al5 noted that “it is only by radically reorganizing current
provision or increasing the time allocated to speech therapists
that their expertise can be effective in the field of chronic
aphasia.” In support of that statement, Poeck et al6 noted that
aphasia improved even in the chronic phase with intensive
therapy.The impact of the intensity of SLT on aphasia recovery still
requires further study. Most of the limitations of the present
review stem, in part, from the limitations of the original
studies. Only 3 studies were rated to be of “good” quality
(PEDro score6), whereas the rest were either of fair quality
(PEDro scores4 and 5) or did not qualify for a PEDro
rating6 because of a lack of randomization of the groups. The
use of nonstandardized measures and lack of clarity regarding
therapy intensity and the nonreporting of overall mean
changes in scores for outcomes measures were noted in
several studies. In addition, many of the studies were under-
powered with small sample sizes. The largest trial, Lincoln etal,11 randomized 327 patients; however, only 161 completed
analyses were reported, and only 27 patients received 36
treatment sessions.
Given the association between intensity of SLT and apha-
sia recovery, greater attention needs to be given to structuring
the most appropriate treatment regime. Length of therapy and
hours of therapy provided per week that allow for maximum
recovery require further investigation. Most importantly, this
review underscores the importance of SLT to aphasia recov-
ery. Previous highly influential studies such as Lincoln et al11
have led to doubt as to the efficacy of SLT in aphasia
recovery. Our review confirms that lower-intensity therapy
provided over a longer period of time does not result in asignificant change in outcome. However, more intensive
SLT, delivered over a shorter period of time, results in
significant improvement in outcome. We conclude that inten-
sive aphasia therapy delivered over 2 to 3 months is critical to
maximizing aphasia recovery, and failure to provide it poten-
tially compromises individual outcomes.
AcknowledgmentsThis study was funded by the Heart and Stroke Foundation of
Ontario, the Ontario Ministry of Health and Long Term Care, the
Parkwood Hospital Foundation, and the Canadian Stroke Network.
We thank Norine Foley, project coordinator, for her help with article
selection and data abstraction, and James Fisher for reviewing thisarticle. The following individuals were involved in assessment of the
TABLE 4. Association Between Intensity of Therapy and
Improvement in PICA and FCP Scores
Length of
Therapy
Hours of
Therapy per Week
Total Hours
of Therapy
PICA r 0.948 r 0.957 r 0.958
P 0.0001 P 0.0001 P 0.0001
Token Test r 0.581 r 0.811 r 0.963
P 0.171 P 0.027 P 0.0001
Bhogal et al Intensity of Aphasia Therapy 991
by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 7/8

8/12/2019 Stroke-2003-Bhogal-987-93
http://slidepdf.com/reader/full/stroke-2003-bhogal-987-93 8/8
References1. Klein K. Aphasia Community Group Manual. New York, NY: National
Aphasia Association; 1995.
2. National Institute on Neurological Disorders and Stroke. Aphasia. hope
through research. Bethesda, MD: National Institute on Neurological Dis-
orders and Stroke; 1990. Publication 90-391.
3. Albert ML. Treatment of aphasia. Arch Neurol. 1998;55:1417–1419.
4. Robey R. The efficacy of treatment for aphasic persons: a meta-analysis.
Brain Lang. 1994;47:582– 608.5. Robey R. A meta-analysis of clinical outcomes in the treatment of
aphasia. J Speech Lang Hearing Res. 1998;41:172–187.
6. Holland A, Fromm D, DeRuyter F, Stein M. Treatment efficacy: aphasia.
J Speech Lang Hearing Res. 1996;39:S27–S36.
7. Tanaka Y, Miyazaki M, Albert ML. Effects of cholinergic activity on
naming in aphasia. Lancet . 1997;350:116 –117.
8. Bragoni M, Altieri M, DiPiero V, Padovani A, Mostardini C, Lenzi G.
Bromocriptine and speech therapy in non-fluent chronic aphasia after
stroke. Neurol Sci. 2000;21:19 –22.
9. Walker-Batson D, Curtis S, Natarajan R, Ford J, Dronkers N,
Salmeron E, Lai J, Unwin D. A double-blind, placebo-controlled studyof the use of amphetamine in the treatment of aphasia. Stroke. 2001;
32:2093–2098.
Bhogal et al Intensity of Aphasia Therapy 993
by guest on December 8, 2013http://stroke.ahajournals.org/ Downloaded from