Stomach Pathology.ppt
description
Transcript of Stomach Pathology.ppt

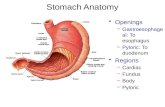
STOMACHSTOMACH

CONGENITAL ABNORMALITIESCONGENITAL ABNORMALITIES
• Pyloric stenosisa) males 3:1 vs. femalesb) may occur with Turner
syndrome, trisomy 18, esophageal atresiac) clinical:
i) narrowing of pyloris- hypertrophy and possibly hyperplasia (muscularis)
ii) regurgitation (projectile !!)- dehydration of concern

iii) oval (“olive”) palpable massiv) surgical splitting is curative

DIAPHRAGMATIC HERNIADIAPHRAGMATIC HERNIA
• Bochdalek herniaA Bochdalek hernia involves an opening on the left side of the diaphragm. The stomach and intestines usually move up into the chest cavity.•Morgagni herniaA Morgagni hernia involves an opening on the right side of the diaphragm. The liver and intestines usually move up into the chest cavity.


ACUTE GASTRITISACUTE GASTRITIS• Gastritis (inflammation of gastric mucosa)• transient inflammation (usually)
a) bleeding and erosion i) sloughing of mucosa
• Pathogenesis not clear: associationsa) NSAID (e.g., aspirin)b) alcoholc) smokingd) stress (trauma, burns, surgery)e) uremia, infections

• Several factors involved: (1 or more)
a) acid secretion with back diffusion
b) HCO3- buffer
c) blood flowd) disruption of mucus layere) damage to epitheliumf) lots of patients have idiopathic acute gastritis without any
of the listed disorders !!g) neutrophils above basement membrane active
inflammation

• Clinical:a) may be asymptomaticb) nausea, vomitingc) variable epigastric paind) in severe cases:
i) hemorrhage- may be fatal
ii) severe hematemesis- alcoholics
iii) melena

CHRONIC GASTRITISCHRONIC GASTRITIS
• presence of chronic mucosal inflammation
a) leading to mucosal atrophyb) intestinal metaplasiac) usually no erosiond) epithelial changes may
dysplasiai) basis for CA

• Pathogenesis:a) chronic infection (H. pylori)b) autoimmune (pernicious
anemia)c) alcohol, smokingd) post surgery (i.e., gastric)e) radiation
1. Helicobacter 1. Helicobacter pyloripylori• most important etiologic
association with chronic gastritis

• plays role in other diseases:a) peptic ulcerb) gastric carcinomac) gastric MALT lymphoma
i) “mucosa-associated lymphoid tissue”
• characteristics:a) flagellated (swim through
mucus)b) urease +
i) produces NH3 and CO2 from urea
- buffers H+

c) H. pylori-induced gastritisi) antral-type
- high H+ production- risk of peptic ulcer
ii) pangastritis- multifocal gastric
atrophy- lower H+ production- risk of adenocarcinoma
d) IL-1β (inflammatory cytokine)i) inhibits gastric acid ii) IL-1β pangastritisiii) IL-1β antral-type

e) clinical:i) serologic test for Abii) fecal bacteria detectioniii) urea breath testiv) gastric biopsy (culture)
- histology visualization

2. Autoimmune gastritis2. Autoimmune gastritis
• < 10% of gastritis cases
• Ab against H+-K+-ATPase , gastrin and IF
a) mucosal atrophyi) loss of acid production
b) pernicious anemia• seen with other autoimmune diseases
a) type 1 diabetesb) Addison's diseasec) Hashimoto thyroiditis

• high risk of gastric CA and endocrine tumors (carcinoid tumors)• diffuse mucosal damage
a) fundus and bodyb) lymphocytes and plasma cellsc) active inflammation
neutrophils !d) atrophy is frequently
associated; and with pangastritis (H. pylori)e) hyperplasia of G cells ( gastrin)
i) due to H+ productionii) gastremia

f) dysplasia with long standing gastritis CA in-situ
i) atrophic forms of chronic gastritis- H. pylori- pernicious anemia
g) clinical:i) few symptoms
- only with severe casesii) peptic ulcer disease
- H.pylori(gastric CA and
lymphoma)

3. Special forms3. Special forms
• Eosinophilica) antral, pyloric regionb) middle aged womenc) abdominal paind) steroids effective
• allergica) childrenb) diarrhea, vomitingc) antral eosinophils

• lymphocytica) T-lymphocytes (CD8+ mostly)b) body of stomachc) ~ 50% associated with celiac
disease• granulomatous
a) granulomasb) Crohn diseasec) sarcoidosisd) infection (TB, histoplasmosis)

• reactive gastropathy a) absence of active inflammation
i) no neutrophilsb) common gastritisc) causes:
i) chemical (NSAID)ii) bile refluxiii) mucosal trauma from
prolapse- “gastric antral vascular “gastric antral vascular
ectasia”ectasia”
(dilated capillaries with fibrin thrombi; longitudinal erythematous stripes)

PEPTIC ULCER DISEASEPEPTIC ULCER DISEASE
• chronic, most often solitary lesionsa) duodenum (initial portion) 4:1b) stomach (antrum)c) gastroesophageal junction
i) Barrett esophagusd) duodenum, stomach and/or jejunum
i) Zollinger-Ellison syndrome• in USA, ~ 4 million; 3:1 male:female• middle age to older adults


• relapsing lesionsa) in part due to H. pylori infection
• peptic ulcers occur:a) imbalance between defense
and damaging forcesi) most due to defense failure
- H. pylorib) H. pylori
i) ~ 100% in duodenal ulcersii) ~ 75% in gastric ulcersiii) antibiotic Tx healing and prevents recurrence

iv) severe inflammation- IL-1, IL-6, IL-8,TNF- IL-8 recruits neutrophils
v) produces proteases and phospholipases
- break down protective actions of mucus
vi) HCO3- in duodenum
v) H+ secretion in stomachvi) damage to mucosa and epithelial cells leakage of nutrients (sustain H. pylori)

c) clinical: (table 17-3)i) epigastric pain, burning
- worse at night and- 1-3 hours after meal- relieved with food or antacids
ii) iron deficiency anemiaiii) penetrating ulcers refer
pain to back, left upper quadrant or chest (MI ?)
iv) NO progression to CA (duodenal or gastric)


ACUTE GASTRIC ULCERATIONACUTE GASTRIC ULCERATION
• well known complication of Tx with NSAID• following severe stress (“stress ulcers”)• many lesions in stomach and occasionally in the duodenum• range from
a) erosion – sloughing of mucosal epitheliumb) entire mucosal thickness (ulcer)

• stress ulcers:a) shock/traumab) sepsisc) severe burnsd) intracranial injury with ICPe) intracranial surgery

MISCELLANEOUSMISCELLANEOUS
• Hypertropic gastropathya) Ménétrier disease: extensive
hyperplasia of gastric mucosa with glandular atrophy
b) clinical:i) epigastric painii) diarrheaiii) weight loss
c) body/fundus, antrum or entire stomach regions

d) gastric secretions i) excessive mucusii) hypo- or achlohydria
- due to glandular atrophye) protein loss
i) hypoalbuminemia and edema
f) risk of gastric CA

BENIGN TUMORSBENIGN TUMORS• In alimentary tract “polyp” is a mass extending above mucosa

• hypereplastic in nature• 10% of polyps are neoplastic
a) dysplasia are are pre-CAb) adenomatous polyps more
common in colon• clinical:
a) hyperplastic polypsi) often seen in chronic
gastritisii) NO malignant potential

GASTRIC CARCINOMAGASTRIC CARCINOMA
• most common malignancy in stomach• next are lymphomas (4%) then• mesenchymal tumors (2%)
a) Leiomyosarcomab) schwannoma
• second most common tumor worldwide•High incidence in Japan, Chile, China, Portugal, etc compared to USA, Europe, Canada

• WHO classification (table 17-4)
• Pathogenesis (table 17-5)a) H. pylori risk 6X for
developing gastric carcinoma (intestinal type)
i) chronic gastritis atrophy metaplasia dysplasia carcinomaii) not all patients with H.
pylori or chronic gastritis develop cancer

b) environmental factorsi) diet suspected as 1o
ii) NO link with alcohol and smoking as causative as
well as antacid use
• most important determinant of outcome is the depth of invasion
a) mucosa and submucosa better prognosis that invasion of the muscularis

• types:a) exophylic
i) protrusion into lumenb) flat
i) NO protrusionsc) excavated
i) crater in wall of stomach
Early
Advanced


• metastasesa) supraclavicular nodeb) periumbilical region to form subcutaneous nodule
i) “Sister Mary Joseph nodule”
c) Krukenberg tumor to ovary clinical:
a) asymptomatic until advanced stage
i) nonspecific CA symptomsb) diffuse area covered with malignancy
i) “linitis plastica” leather bottle

Krukenberg tumor to ovaryKrukenberg tumor to ovary
•Usually large and associated with poor prognosis

Gross: Linitis plastica carcinoma diffusely infiltrates the entire gastric wall without forming an intraluminal mass. The wall of the stomach is typically thickened to about 2-3 cm. and has a leathery, inelastic consistency.

c) metastasis from breast or lung can cause linitis plastica (diffuse)• gastric lymphoma
a) > 80% associated with H. pylori and chronic gastritis
i) 50% Tx with antibiotics• GI stromal tumor
a) originate in interstitial cells of Cajal (regulate peristalsis)
i) 95% stain with Ab against c-KIT (CD117)ii) 70% stain for CD34












![Basic Plant Pathology.ppt [Repaired] - UGA Extensionextension.uga.edu/content/dam/extension-county-offices/bartow... · ORGANISM! Biotic (pathogenic) ... Black spot on Rose Prune](https://static.fdocuments.in/doc/165x107/5ab5dd477f8b9a2f438d15e5/basic-plant-repaired-uga-extensionextensionugaeducontentdamextension-county-officesbartoworganism.jpg)


