static-content.springer.com10.1007... · Web viewGeneral ICU , new onset hypotension (MAP < 60...
Transcript of static-content.springer.com10.1007... · Web viewGeneral ICU , new onset hypotension (MAP < 60...

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
ESM_2: Summary Tables
Table S2: Large randomized controlled trials investigating the effect of crystalloids in critically ill patients.AuthorYear
Study DesignLevel (A=C)
Clinical setting Intervention Nr trials or patients
Endpoints Results Comments
Young P 2015 SPLIT [1]
RCTA
ICU patients PlasmalyteNS
11621116
AKIHospital mortalityRRT
9.6% vs 9.2%, p=0.777.6% vs 8.6%, p=0.403.3% vs 3.4%, p=0.91
Double-blind, cluster randomized, double-crossover trialMedian of 1.5 l fluids received
Semler MW 2016 SALT [2]
RCTA
ICU patients Balanced crystalloidsNS
520
454
MAKE 30d (death, dialysis, persistent renal dysfunction)
24.7% vs 24.6%, p=0.98 Median of 1.5 l fluids received
Incidence of MAKE 30d was increasing with total amount of infusion volume in the NS but not in the balanced crystalloids group (p=0.026)
RCT = randomised controlled trial, HA = Human serum albumin, AKI = acute kidney injury, RRT = renal replacement therapy, RL = ringer´s lactate, NS= normal saline

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S3: Large randomised controlled trials and meta-analyses investigating colloids in critically ill patients.
AuthorYear
Study DesignLevel (A-C)
Clinical setting
Time of study/search
Intervention Nr trials or patients
Endpoints Results Comments
Stockwell MA 1992 [3]
RCTA
ICU patients 4.5% HA 3.5% gelatine
226249
AKI 1.3% vs. 2.0%, NS no
Schortgen F 2001 [4]
RCTB
Severe sepsis, septic shock
1998-199 6% HES 200/0.63% gelatine
6565
AKI (twofold increase in s-crea or RRT)Oliguria
42% vs 23%, p=0.028OR 2.57 (95%CI 1.13-5.83)
56% vs. 37%, p=0.025
differences in serum creatinine at baseline
Finfer S 2004 SAFE [5]
RCTA
ICU patients requiring fluid resuscitation
2001-2003 4% HANS
34973500
28 day mortalityDuration RRT
20.9% vs 21.1%, p=0.870.5+2.3 vs. 0.4+2.0, p=0.41
Brunkhorst FM 2008 [6]
RCTA
Severe sepsis 2003-2005 10% HES 200/0.5modified RL
262275
28 day mortalityAKI (twofold increase in s-crea or RRT)RRT
26.7% vs. 24.1%, p=0.4834.9% vs. 22.8%, p=0.002
31.0% vs. 18.8%, p=0.001
harm by HES
Guidet B 2012CRYSTMAS [7]
RCTB
Severe sepsis 2007-2010 6% HESNS
10096
Amount to reach hemodynamic stabilisationMortalityAKI (AKIN)
1.37 vs. 1.71 P=0.019
31% vs. 25.3% P=0.5948% vs. 45,8% p=0.37
Perner A 2012 6S [8]
RCT A
Severe sepsis 2009-2011 6% HES Ringer´s Acetate
398400
90 d mortalityAKI (twofold increase in s-crea)RRT
51% vs 43%, p=0.0341% vs 35%, p=0.08
22% vs 16% p=0.04
harm by HES (mortality, AKI,RRT)
Myburg, J.A. 2012 CHEST [9]
RCT A
ICU patients, fluid resuscitation
2009-2012 6% HES NS
33363315
90 d mortalityAKI (RIFLE F)RRT
18% vs 17%, p=0.2610.4% vs 9.2%, p=0.127% vs 5.8%, p=0.26
harm by HES (RRT)increased rates of itching

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Caironi P 2014 ALBIOS [10]
RCTA
Severe sepsis 2008-2012 20% HAcrystalloid
903907
28d mortalityAKIRRT
31.8% vs. 32 % p=0.9421.9% vs.22.7 % p=0.7124.6% vs. 21.4 % p=0.11
decreased mortality in subgroup with septic shock (n=1121), RR=0.87, 95%CI 0.77-0.99, less positive fluid balance
Zarychanski R 2013[11]
Meta-analysis A
ICU , surgical patients
1966-2012 HEScrystalloids, albumin or gelatine
31 RCTs including10290 patients
mortalityAKI RRT
RR 1.09 (95% CI 1.02-1.17)RR 1.27 (95% CI 1.09-1.47)RR 1.32 (95% CI 1.15-1.50)
retracted studies by J. Boldt excludedharm by HES (mortality, AKI,RRT)
Haase N 2013 [12]
Meta-analysis A
Sepsis 1966-2012 HEScrystalloids, or albumin
9 RCTs including3456 patients
mortalityAKI RRT
RR 1.04 (95% CI 0.89-1.22)RR 1.18 (95% CI 0.99-1.40)RR 1.36 (95% CI 1.08-1.72)
mortality in 4 trials with low risk of bias, 3016 patients RR 1.11 (95% CI 1.00-1.23)
Gattas DJ 2013 [13]
Meta-analysis A
ICU patients 1966-2012 6% HES resuscitation fluids
35 RCTs including10391 patients
mortalityRRT
RR 1.08 (95% CI 1.00-1.17)RR 1.25 (95% CI 1.08-1.44)
harm by HES (mortality RRT)
Rochwerg B 2015 [14]
Network meta-analysis A
Sepsis 1966-2014 HESalbumincrystalloidbalanced crystalloids
10 RCTs including6664 patients
RRT Starch vs. crystalloidsRR 1.39 (95% CI 1.17-1.66)Albumin vs. crystalloidsRR 1.04 (95% CI 0.78-1.38)
harm by HES (RRT)
Moeller C 2016 [15]
Meta-analysis C
Acutely ill patients
1966-2015 gelatine crystalloid or albumin
60 Studies30 RCTs8 non-randomised studies22 animal studies
MortalityAKI
RR 1.15 (95% CI 0.96-1.38)RR 1.35 (95% CI 0.58-3.14)
Increased risk of anaphylaxis by gelatine
RCT= randomised controlled trial, HA = Human serum albumin, AKI = acute kidney injury, RRT =renal replacement therapy, RL = ringer´s lactate, NS = normal saline

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S4: Meta-analyses and randomised controlled trial s not included in the meta-analyses evaluating the effects of loop diuretics on renal function and/or mortality
Authoryear
Study designEvidence (A-C)
Clinical setting Intervention Number of patients included
Endpoints Results Renal protection
Comments
Sampath S et al. 2007 [16]
Meta-analysisA
Patients with or at risk of AKI
Loop diuretics versus placebo
5 RCTs Mortality RRT
RR 1.12 (95% CI 0.92-1.35)RR 0.76 (95% CI 0.53-1.00)
No
Bagshaw SM et al. 2007 [17]
Meta-analysisA
Critically ill and non-critically ill patients with AKI
Frusemide versus placebo
5 RCTs including 555 patients
renal recovery hospital mortality
OR 0.88 (95% CI 0.59-1.31)OR 1.28 (95% CI 0.89-1.84)
No
Ho KM et al. 2010 [18]
Meta-analysis A
Adults with or at risk of AKI
Frusemide versus placebo
11 RCTs including 962 patients
RRT hospital mortality
RR 1.02 (95% CI 0.90-1.16)RR 1.12 (95% CI 0.93–1.34)
No more side effects
Wu MY et al. 2014 [19]
Meta-analysisA
Patients with acutely decompensated heart failure
Continuous loop diuretic infusion versus bolus treatment
10 RCTs including 518 patients
change in creatinine
mortality
No significant difference
RR 1.13 (95% CI 0.61-2.10)
No
Hager B et al. 1996 [20]
RCT B
Patients post major thoraco-abdominal or vascular surgery
Frusemide infusion versus placebo
121 patients creatinine clearance
Decrease of creatinine clearance by 83% in frusemide group and by 81% in placebo group
No more hypokalaemia in frusemide group
Lassnigg A et al. 2000 [21]
RCTB
Patients with normal renal function having cardiac surgery
Dopamine versus frusemide infusion versus placebo
n=42 (dopamine)n=41 (frusemide_n=40 placebo
change in creatinine
Significant rise in creatinine in frusemide group
No
Sirivella S et al. 2000 [22]
RCTC
Patients with oliguric or anuric AKI after cardiac surgery
Intermittent diuretics versus continuous infusion of mannitol, frusemide and dopamine
n=40 (intermittent)n=60 (continuous)
RRT 90% vs 6.7% Yes

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Smith MN et al. 2008 [23]
RCTC
Patients with creatinine 130 – 250 μmol/L having cardiac surgery
Mannitol versus Hartmann’s solution
n=25 (mannitol)n=25 (Hartmann’s)
change in creatinine
RRT
No difference in creatinine changesNo difference
No
Kunt AT et al. 2009 [24]
RCTB
Elective CABG surgery patients with creatinine <1.4mg/dl
Continuous frusemide infusion versus bolus treatment
n=50 (infusion)n=50 (bolus)
RRT creatinine
clearance 30-day mortality
0 vs 5% ; p=0.028significant fall in bolus group
0 vs 5% ; p=0.028
Yes (infusion)
Majumdar SR et al. 2009 [25]
RCTB
Adults with creatinine >1.7mg/dl undergoing coronary angiography
Saline + frusemide + mannitol versus saline hydration
n=46 (combination)n=46 (saline)
contrast induced nephropathy (≥25% or ≥0.5mg/dL rise in creatinine)
mortality
50% vs 28% ; p=0.03
no difference
No
Marenzi G et al. 2012 [26]
RCTB
Patients with CKD undergoing contrast coronary procedures
Frusemide with matched hydrationversus isotonic saline hydration
n=87 (furosemide)n=83 (saline)
Contrast induced nephropathy (≥25% or ≥0.5mg/dL rise in creatinine)
4.6% vs 18% ; p=0.005 Yes less in-hospital complications
Palazzuoli A et al. 2014 [27]
RCTB
Patients with acutely decompensated heart failure
Continuous frusemide infusion versus frusemide boluses
n=43 (infusion)n=39 (boluses)
AKIestimated GFR
22% vs 15% ; p=0.3 -9 vs +5 ; p<0.05
No
AKI = acute kidney injury; CABG = coronary artery bypass graft; CCF = congestive cardiac failure; CKD = chronic kidney disease; GFR = glomerular filtration rate; RCT = randomised controlled trial; RRT = renal replacement therapy; RR = relative risk; OR = odds ratio; CI = confidence interval;

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S5: Randomised controlled trials evaluating the renal protective effects of vasopressors
AuthorYear publication
Study DesignEvidence (A-C)
Clinical setting
Year of study Intervention Nr trialspatients
Endpoints Results Comment
Arterial pressure targetAsfar P2014 [28]
RCTA
Sepsis 2010-2011 MAP 65-70 mm HgMAP 80-85 mmHg
388388
AKIN II Renal SOFA RRT RRT free days Mortality 90-d
41.6% vs. 38.6%, p=0.421.0±1.4 vs. 0.8±1.3, p=0.07635.8% vs. 33.5%, p=0.521±11 vs. 19±11, p=0.3642.3% vs. 43.8%, p=0.74
High target: more new atrial fibrillation
Chron. hypertension subgroup
MAP 65-70 mm HgMAP 80-85 mmHg
173167
AKIN II Renal SOFA RRT
52.3% vs. 38.9%, p=0.021.1±1.4 vs. 0.7±1.2, p=0.00542.2% vs. 31.7%, p=0.046
Quereshi AI2016 [29]
RCTA
Acute Cerebral Hemorrhage
2011-2015 Systolic Pressure 110-139 mmHgSystolic Pressure 140-179 mmHg
500500
Renal adverse events c
9.0%4.0% p=0.002
VasopressorsRussell JA2008VASST [30]
RCTA
Septic shock b 2001-2006 vasopressin (0.01 to 0.03 U/min)noradrenaline(5 to15 μg/min)
besides open label vasopressors
396382
Mortality 90-d
RRT
44.2 vs. 49.5, p=0.11In less severe septic shock
26.5% vs. 35.7%, p = 0.05
Gordon AC2010PosthocVASST [31]
PosthocRCTB
Septic shock b
+ AKI RIFLE risk
2001-2006 vasopressin (0.01 to 0.03 U/min)noradrenaline(5 to15 μg/min) besides open label vasopressors
53 53
Worsening renal function
RRT mortality
20.8 vs. 39.6%, p=0.03
17.0 vs. 37.7%, p=0.0230.8 vs. 54.7%, p=0.01
De Backer D2010 [32]
RCTA
Shock 2003-2007 DopamineNorepinephrine
858821
Mortality RRT free days
arrhythmia
52.5% vs. 48.5%, p=0.1012.8±12.4 vs. 14.0±12.3, p=0.0124.1% vs. 12.4%, p<0.01

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Subgroup Cardiogenic shock
135145
Mortality Higher in the dopamine group, P=0.03
Gordon ACVANISH2016 [33]
RCTA
Septic shock 2013-2015 vasopressina norepinephrine
205204
Kidney failure free days
% patient without kidney failure
RRT
RRT in survivors
Mortality
V vs. N: 9 (1-24) vs 13 (1-25)Diff -4 (-11 to 5)
V vs. N: 57.0% vs. 59.2%Diff: -2.3% (-13.0 to 8.5%)
V vs. N: 25.4% v. 35.3%Diff:-9.9% (-19.3 to -0.6%)*
V vs. 19.9% vs. 22.3% Diff: -2.4 (-12.5 to 7.7)
V vs.N:10.7% vs.8.3%Diff: 2.5% (-3.3 to 8.2%)
Hajjar LAVANCS2017 [34]
RCTBd
Vasoplegic shock after Cardiac Surgery
2012-2014 vasopressin (0.01 to 0.06 U/min
noradrenalin 10 to 60 μg/min
149
151
mortality orseverecomplications e
within 30 days AKIN 1
AKIN 2
AKIN 3
RRT
Mortality 90d
.V vs., N: 32% vs. 49%HR 0.55 (0.38 to 0.80)
V vs. N: 20.0% vs. 18.5% OR 1.64 (0.889 to 3.03)
V vs. N: 6.2% vs. 11.9% OR 3.39 (1.43 to 8.06)
V vs. N: 8.3% vs. 32.5%6.93 (3.4 to 14.12)
V vs N: 2.7% vs. 13.9%OR 0.17 (0.06 to 0.51)
V vs N: 16.1% vs. 17.2%OR 0.92 (0.5-1.69)..
No difference in mortality
Single-centre studyhigh mortalityhigh incidence of RRT, possibly related to the inclusion criteria
a titrated up to 0.06 U/min, RRT renal replacement therapy, ND not differentb patients with septic shock needing s minimum of 5 μg of norepinephrine per minute .c Renal adverse events according to Medical Dictionary for Regulatory Activities (MEDDRA) definitionsd Monocenter study, high mortality and high incidence of AKIN and RRT possibly related to the inclusion criteria e stroke, requirement for mechanical ventilation for longer than 48h, deep sternal wound infection, reoperation, or acute renal failure

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S6: Meta-analysis evaluating the renal protective effect of low dose dopamine
AuthorYear publication
Study DesignEvidence (A-D)
Clinical setting
Year of study Intervention Nr trialspatients
Endpoints Results Comments
Meta-analysisFriedrich2005 [35]
Meta-analysisA
Major surgeryCritically ill
1966-2005 Low dose dopamine 613359
Need for RRT
Urine Output d-1Urine Output d 2Urine Output d 3
Creat Clearance d1Creat Clearance d2Creat Clearance d3
Mortality
RR 0.96 (0.78-1.19)
RM 1.24 (1.14-1.35), , p<0.01RM 1.09 (0.99-1.20)RM 1.02 (0.87-1.20)
RM 1.06 (1.01-1.11) , p=0.02RM 1.02 (0.90-1.15)RM 1.09 (0.96-1.24
RR 0.96 (0.78-1.19)RR = relative risk, RM = ratio of means

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S7. Meta-analyses and RCT not included in the meta-analyses evaluating the renal protective effect of fenoldopam Authoryear
Study DesignLevel (A-C)
Clinical settingInclusion
Time of study/search
Intervention Nr trials or patients
Endpoints Results Comments
Meta-analysesLandoni G a
2007 [36]Meta-analysisB *
Critically ill andCardiovascular surgery
Up to 2005 fenoldopam placebo/dopamine
or dobutamine /control
16 a
1290Risk for AKINeed for RRTHosp. mortality
OR 0.44 (CI0.32-0.59)OR 0.54 (0.34-0.84)OR 0.64 (0.45-0.91)
Small and non-RCT
Landoni G b
2008 [37]Meta-analysisB *
Cardiovascular surgery
Up to 2006 fenoldopam placebo/
dopamine/control
13 b
1059Need for RRTHosp. mortality
OR 0.37 (0.23-0.59)OR 0.46 (0.29-0.75)
Small and biased trials
Zangrillo A c
2012 [38]Meta-analysisB *
Cardiac surgery Up to 2012 fenoldopam placebo
6 c
440Risk for AKINeed for RRTHosp. mortality
OR 0.41 (0.23-0.74)No effectNo effect
SmallMore hypotension
Gillies MA c
2015 [39]Meta-analysisB *
Major surgery NR fenoldopam placebo
6 c
507New AKINeed for RRTHosp. mortality
OR 0.46 (0.27-0.79)OR 0.27 (0.06-1.19)OR 1.0 (0.14-7.37)
SmallHigh risk of biasMore hypotension
RCTBove T2014 [40]
RCTA
Post cardiac surgeryAKI RIFLE Risk
2008-2013 fenoldopam0.1μg/kg/min (0.025-0.3μg).
Placeboup to 4-days
338
329
Need for RRT
Mortality
69/338 (20%)60/329 (18%), p=0.8678/338 (23%)74/329 (22%), p=0.47
No protectionMore hypotension
AKI = acute kidney injury, RRT= renal replacement therapy, RCT = randomised controlled trial, CrCl = creatinine clearance, SCr = serum creatinine, * Small studies, some heterogeneity, different definitions of AKI, outcome reported bias
a In this meta-analysis, all included studies were RCTs; 5 RCTs included ICU patients, 5 cardiac surgery, 3 vascular surgery, 2 liver and 1 renal transplantationb In this meta-analysis, 4/13 studies including 386/1059 patients were non-randomised (case control, propensity matched)c The included RCTs in the meta-analysis of Gilles et al. differ from those in the meta-analysis of Zangrillo et al.. Gilles at al. also included a RCT in patients with a solitary kidney undergoing partial nephrectomy and in patients undergoing liver transplantation , but did not include a RCT in critically ill patient with early acute tubular necrosis and a RCT in cardiac surgery comparing fenoldopam to dopexamine

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S8: Meta-analysis and RCT not included in the meta-analyses evaluating the renal protective and or mortality effects of natriuretic peptides
Authoryear
Study DesignEvidence
Clinical setting Time of study/search
Intervention Nr trialspatients
Endpoints Results Renal protection
Comments
Meta-analysesNigwekar SU2009 [41]
Meta analysisB
Prevention AKI 1966-2007 ANPPlacebo
11818
Need for RRT
Mortality
OR 0.45 (0.21-0.99)P=0.05OR 0.67 (0.19-2.35)
Yes LOS
Treatment AKI 8 1043
Need for RRT Mortality
OR 0.59 (0.32-1.08)OR 0.34 (0.12-0.96) b
OR 1.01 (0.72-1.43)Yes b
Hypotension b
Arrhythmias b
Subgroup major surgery a
14817
Need for RRTMortality
OR 0.49 (0.27-0.88)NS
Subgroup CV surgery
8 Need for RRT OR 0.24 (0.10-0.58) Yes
Oliguric AKI Need for RRTMortality
OR 0.46 (0.19-1.12)OR 0.94 (0.62-1.43)
No
Mitaka C2011[42]
MetaAnalysisB
Cardiac and CV surgery
1994-2011 ANP or BNPPlacebo
6 ANP1041
Peak seCr
RRT
Mortality
-0.13 (-0.130-0.126) p<0.00016/280 vs. 18/283OR 0.261 (0.090-0.761)OR 0.62 (0.22 – 1.75)
Yes LOS Arrhythmias
3 BNP425
seCr / RRTMortality
NSOR 0.72 (0.24 - 2.12)
No LOS
Xiong B2015 [43]
Meta-analysisB
Acute decompensated heart failure
1999-2014 BNP nesiritide)Control or placebo
Subgroup high dose> 0.01 μg/kg/minSubgroup standard dose< 0.1 + bolus 2 μg/kg Subgroup low dose
159623
1269
7698
503
Worsening renal function
RR 1.08 (1.01–1.15) p=0.023
RR 1.54,9 (1.19-2.00 p=0.001RR 1.04 (0.98–1.12) p=0.213 RR 1.01 (0.74–1.37)

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
< 0.01 μg/kg/min Subgroup non-CKD
Subgroup CKD
Subgroup 1030 Weighted mean SeCreat
p=0.968RR 1.08 (1.02–1.16) p=0.016RR 0.94 (0.70–1.27) p=0.680-2.54 (-5.76–0.67) p=0.121
Randomised controlled trialsMori Y2014 [44]
RCTC
Aortic arch surgery
ANP 0.0125 μg/kg/min Placebo
2022
AKI
RRTmortality
6/20 (30%) vs. 16/22(72%), p=0.0140/20 vs. 0/22, NS0/20 vs. 1/22, NS
Yes
Sezai A2013 [45]
RCTB
High risk CABG+CPBEuroscore ≥ 6
hANP (carperitide) placeboduring CPB until oral intake
183184
RRT
Mortality
0/183 vs. 7/184 (p=0.015)14/183 vs. 22/184 (p=0.22)
Yes less MACCE Fragility 1
OR = odds ratio; CV = cardiovascular; RCT = randomised controlled trial; ANP = atrial natriuretic factor; seCr = serum creatinine; RRT = renal replacement therapy; LOS = length of stay; CPB = cardiopulmonary bypass; MACCE = major adverse cardiovascular and cerebrovascular events. CKD = chronic kidney diseasea including 3 RCT in liver transplantation and 1 RCT in heart transplantationb low dose ANP; no benefit for high dose ANP ; c non inotrope control; d any control; e low dose

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S9: Meta-analysis and RCT not included in the meta-analyses evaluating the renal protective effects of levosimendanAuthorYear
Study DesignEvidence (A-C)
Clinical setting Time of study/search
Intervention Nr trialspatients
Endpoints Results Comments
Bove T 2015 [46]
Meta-analysisB**
Critically ill with or at risk for AKI
High quality studies
1999-2013 levosimendanplacebo/dobutamine/
PGE2milrinone/ fur-osemide/ standard inotrop-ics
333867
6
AKI
RRT
RRT
L: 7.3% vs. C: 9.3%RR 0.79 (0.63 to 0.99) L: 3.5% vs. C: 8.7%RR 0.52 (0.32 to 0.86)
RR 0.41 ( 0.15 to 1.12) p=0.08
Zhou C 2016 [47]
Meta-analysisB**
Cardiac Surgeryperioperatively
1990-2015 levosimendanplacebo (9)/other inotropic
(4)
131345
AKI
RRT
Mortality
L: 8.7% vs. C: 15.1%OR 0.51 (0.24-0.79)L: 4.5% vs. C: 10%OR 0.43 (0.25-0.76)L: 5.3% vs. C: 14.3%OR 0.41 (0.27 -0.62)
Randomised controlled trialsGordon AC2016 [48]
RCTdouble blindA
Sepsis 2014-2015 levosimendan0.1 g/kg/min (0.5-2) for 24h
placebo
258
257
Renal SOFA
Need of RRT
Mortality 28-d
Mean diff0.61 (−0.07 to 1.29)L: 24.1% vs. C: 24.1% OR 0.99 (0.66 – 1.49)L: 34.5% vs. P: 30.9% OR 1.19 (0.82 – 1.72)
Trend to worse outcome,no renal protection,longer weaning,more arrhythmia
Mehta RH2017 [49]
MulticentreRCTnon-blindedA
Cardiac surgeryLV ejection fraction < 35%
2014-2016 levosimendan 0.2 μg/kg/min for 1 hour,
followed by 0.1 μg/kg/min for 23 hours
placebo
Per protocol428
421
Composite: 30-d mortality, RRT, MI, 5-d mechanical assist RRT at 30-d
24.3% vs. 24.4%OR 1.00 (0.66–1.54)
2.1% vs. 3.8%OR 0.54 (0.24–1.24)

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Landoni G2017 [50]
MulticentreRCTdouble-blindA
Cardiac surgeryNeeding HD support
2009-2016 levosimendan 0.025 to 0.2 μg/kg/min for 48-h
placebo
248
258
30-day mortality
AKI risk
AKI injury
AKI failure
RRT
12.9% vs. 12.8%OR 0.1 (−5.7 to 5)16.6% vs. 21.3% OR −4.7 (−11.5 to 2.1)10.5% vs. 10.5%OR 0.1 (−5.3 to 5.4)6.9% vs. 8.5%OR −1.6 (−6.3 to 3.0)9.7% vs. 12.8%OR −3.1 (−8.6 to 2.4)
RCT = randomised controlled trial, CABG = coronary artery bypass grafting, PCI = percutaneous coronary intervention, RRT = renal replacement therapy, SOFA = Sequential Organ Failure Assessment, GFR = glomerular filtration rate; * cardiac surgery OR 0.52 (0.35-0.75), cardiology OR 0.75 (0.63-0.91), LV left ventricular, MI myocardial infaction, HD hemodynamic** Small studies, some heterogeneity, AKI was not always a predefined endpoint, different definitions of AKI, outcome reported bias

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S10: Randomised controlled trials evaluating the renal protective effects of dexmedetomidine
AuthorYear publication
Study DesignEvidence (A-C)
Clinical setting
Year of study Intervention Nr trialspatients
Endpoints Results Comments
Leino 2011[51]
RCT B
Coronary Artery Bypass Surgey
1994-1997 -dexmedetomidine-placebo
4443
Diuresis in the first 4 hours after insertion of urinary catheterPeri-operative serum creatinine
74 % increase in diuresis in the dexmedetomidine group (P < 0.001)
No differences between the two groups (P> 0.05) regarding creatinine
Balkanay2015 [52]
RCTB
Coronary Artery Bypass Surgey
2009-2011-dexmedetomidine < 8 mcg/kg-dexmedetomidine > 8 mcg/kg-placebo
312928
NGAL at 24 h
serum creatinine, diuresis
NGAL 24h [ng/ml]97.767.3176.8(P < 00.1)
no differences in serum creatinine or diuresis
Cho 2016 [53]
RCTA
Valvular Hart Surgery Patients
2013-2015 Groups- placebo - dexmedetomidine 0.4 mcg/kg
100100
AKI at 48h
ICU length of Stay in days
AKI at 48 h 33%14 %P < 0.05
placebo: 2.4 ddexmedetomidine: 2.3 dP < 0.05
RCT = randomised controlled trial, AKI = acute kidney injury, NGAL= Neutrophil gelatinase-associated lipocalin

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S11: Randomised controlled studies evaluating the renal protective effect of tight glycaemic control
Author
Year [ref]
Design
Evidence
(A-C)
Clinical
setting
Year of
study
Intervention Targets
(mg/dL)
N patients
(N trials)
endpoints Results
(TGC vs control)
RR Comments
Van den Berghe G
2001 [54]
RCT
A
Surgical ICU 2000-
2001
TGC
control
80-110R/ if >215Stop if <180
765
783
mortality
RRT
AKI1
7.2% vs 10.9% (p=0.01)
4.8% vs 8.2% (p=0.007)
9.0% vs 12.3% (p=0.04)
0.66 (0.48-0.92)
0.59 (0.4-0.88)
Van den Berghe G
2006 [55]
RCT
A
Medical ICU 2002-
2005
TGC
control
80-110R/ if >215Stop if <180
595
605
mortality
RRT
AKI2
37.3% vs 40% (p=0.33)
19.8 vs 19.8% (NS)
5.9 vs 8.9% (p=0.04)
0.93 (0.81-1.08)
0.92 (0.74-1.14)
Brunkhorst F
2008 [6]
RCT
A
Severe sepsis/
septic shock
2003-
2005
TGC
control
80-110
180-200
247
290
mortality
RRT
AKI4
24.7% vs 26% (p=0.74)
27.5% vs 22.5% (p=0.19)
31.1% vs 26.6% (p=0.25)
0.95 (0.71-1.27)
1.21 (0.9-1.63)
Arabi YM
2008 [56]
RCT
A
Mixed ICU 204-
2006
TGC
control
80-110
180-200
266
257
mortality
RRT
27.1% vs 32.3% (p=0.19)
11.7% vs 12.4% (p=0.54)
0.84 (0.64-1.09)
0.97 (0.61-1.54)
De Le Rosa G
2008 [57]
RCT
A
Mixed ICU 2003-
2005
TGC
control
80-110
180-200
254
250
mortality
RRT
AKI
40% vs 38.4% (NS)
10.8 vs 13% (p=0.45)
12.6 vs 10% (p0.36)
1.13 (0.89-1.44)
0.81 (0.50-1.3)
Large overlap achieved blood
glucose levels
Preiser
2009 [58]
RCT
A
Mixed ICU 2004-
2006
TGC
control
80-110
140-180
536
542
mortality
Days of RRT
23.3% vs 19.4% (p=0.11)
519 vs 523 (p=0.75)
1.21 (0.93-1.57) Stopped early
Large overlap achieved blood
glucose levels
Finfer S
2009 [59]
RCT
A
Mixed ICU 2004-
2008
TGC
control
81-108
<180
3010
3012
mortality3
mortality6
RRT
22.3% vs 20.8% (p=0.17)
27.5% vs 24.9% (p=0.02)
15.4% vs 14.5% (p=0.34)
1.07 (0.97-1.18)
1.14 (1.02-1.28)
1.06 (0.94-1.2)
Strict vs. intermediate level
Unreliable glucose meters

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Arabi YM
2011 [60]
RCT
A
Mixed ICU ?? TGC
control
80-110
180-200
120
120
mortality
RRT
35% vs 37.5%
16.7% vs 15% (p=0.72) 1.11 (0.62-1.91)
Wiener
2008 [61]
Meta-
analysis
A
TGC
Control
1790
1839 (9)
mortality
RRT
0.93 (0.85-1.03)
0.96 (0.76-1.2)
Ling Y
2012 [62]
Meta-
analysis
A
TGC
control
5368
5417 (8)
mortality
RRT
1.02 (0.95-1.10)
0.96 (0.83-1.11)
RCT = randomised controlled trial, TGC = tight glycemic control, RRT = need for renal replacement therapy, AKI = acute kidney injury mortality = hospital mortality unless otherwise reported1 peak Screat <2.5mg/dL, 2 doubling of admission Screat or peak >2.5mg/dL 3 28-day mortality, 4 doubling of Screat or RRT, 5 30d mortality, 6 90d mortality

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S12: Randomised controlled studies evaluating the renal protective effect of erythropoietin
AuthorYear [ref]
DesignEvidence (A-C)
Clinical setting Interventionin U rHuEPO
N patients(N trials)
endpoints ResultsEPO vs placebo
RR for AKI Comments
Endre 2010 [63]
RCTC
ICU + increased biomarker
500U/kgplacebo
8479
RRT in 30dAKI in 7d
6% vs 3.8% (p=0.72)48.8% vs 48.7% (p=1)
Shema-Didi2016 [64]
RCTC
Contrast in diabetics
50,000IUcontrol
7266
Scr increase of 0.5mg/dL in 48h
9.7% vs 7.6% (p=0.65)
Song2009 [65]
RCTC
Elective CABG 300U/kgplacebo
3635
AKI in 5d 8% vs 29% (p=0.035) Fragility index 1
Yoo2011 [66]
RCTC
Valvular heart surgery
500U/kgplacebo
3737
AKI in 48h 24.3% vs 54.3% (p=0.017) Fragility index 3
De Seigneux2012 [67]
RCTC
Cardiac surgery 20000U40000Uplacebo
202040
AKI in 7d 25% vs 30% vs 17.5% (NS)
Tasanarong2013 [68]
RCTC
Cardiac surgery 200U/kgplacebo
5050
AKI in 48h 14% vs 38% (p<0.01) Fragility index 4
Kim2013 [69]
RCTC
Cardiac surgery 300U/kgplacebo
4949
AKI in 48h 33% vs 35% (p=0.83)
Dardashti2014 [70]
RCTC
Cardiac surgery 400U/kgplacebo
3535
AKI in 48h 34% vs 29% (p?)
Kim2016 [71]
RCTC
Aortic surgery 500U/kgplacebo
3030
AKI in 7dStage 3 AKI
58% vs 62% (p=0.75)16% vs 14% (p>0.99)
Tie2015 [72]
Meta-analysisB
Cardiac surgery All patientsLow AKI riskHigh AKI risk
321 (5)143 (3)178 (2)
AKI 0.64 (0.35-1.16)0.38 (0.24-0.61)1.22 (0.77-1.94)
heterogeneity
Penny-Dimri2016 [73]
Meta-analysisB
Cardiac surgery All patientsLow AKI riskPre anaesthetic administration
531 (6)171 (2)172 (2)
AKI 0.69 (0.35-1.36)0.25 (0.11-0.56)0.27 (0.13-0.54)
heterogeneity

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Zhao2015 [74]
Meta-analysisC
ICU or peri-operative care
All patients 13911368 (10)
mortalityRRTAKI
0.96 (0.78-1.18)0.72 (0.31-1.70)0.97 (0.79-1.19)
EPO = erythropoietin, RCT = randomised controlled trial, RRT = need for renal replacement therapy, AKI = acute kidney injury. The fragility index refers to the numbers of events that is required to change a statistically significant result into a non-significant result.

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S13. Randomised controlled studies evaluating the renal protective effect of N-acetyl cysteine in ICU patients
Authoryear
Study DesignEvidence (A-C)
Clinical setting Intervention Nr of patients
Endpoints Results Comments
Burns KE2005 [75]
RCTB
At risk patients (CRF, ≥70 yrs, DM, poor LV) undergoingcardiopulmonary bypass
IV NAC (600mg x 4 doses)
placebo or control
295 Increase in SCr > 44μmol/l or > 25% baseline
29.7 vs. 29% (OR 1.03 (0.72-1.46) p = 0.89
Macedo E2006 [76]
RCTC
Elective AAA repairStable renal function
NAC 2x1200mg po starting day before surgery , then Iv NaC 600mg x 4placebo
42 Increase in SCr > 44μmol/l or > 25% baselineICU MortalityICU LOS
50% vs. 27.3% p = 0.16
p = 0.29p = 0.4
Komisarof JA2007 [77]
RCTB
> 30 minutes new onset hypotension
oral/NG NAC 3.0g bolus, then 1.5g x 8 doses, then 1.2g x 8 doses
placebo
142 Increase in SCr > 0.5mg/dl
ICU MortalityNeed for RRT
15.5 vs 16.9% p = 0.82
NoneNone
Sisillo E2008 [78]
RCTB
Patients with CrCl < 60 ml/min undergoingcardiopulmonary bypass
IV NAC 1.2 g x 4 doses
placebo
254 Increase in SCr > 44μmol/l or > 25% baseline
ICU MortalityNeed for RRT
40 vs 52% p = 0.06
NoneNone
Decreased need for prolonged MV in NAC group ( 3 vs. 18% p = 0.001)ICU stay > 4 days reduced (13 vs. 33% p = 0.001)
Adabag AS2008 [79]
RCTB
Patients with chronic kidney disease undergoing cardiac surgery
IV NAC 600mg bd for 7 days
placebo
102 Maximum change in SCr from baseline
ICU MortalityNeed for RRT
0.45 +/- 0.7 mg/dL (NAC) vs. 0.55 +/- 0.9 mg/dL (placebo) p = 0.53p = 1.0p = 0.68

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Wijeysundera DN 2007 [80]
RCTB
Patients with CrCl < 60 ml/min undergoingCardiopulmonary bypass
IV NAC 100mg/kg bolus followed by 20mg/kg/hr for 4 hours
placebo
177 %age change in GFR during first 72 hours
Increase in SCr > 44μmol/l or > 25% baselineNeed for RRTICU Mortality
5.2% improved in NAC group (CI 2.4-12.1%)
28 vs. 32% p = 0.59OR 0.84 (0.42-1.68)p = 0.370 vs 8%, p = 0.007
Song JW2015 [81]
RCTB
At risk patients undergoing off-pump coronary bypass surgery (i) preoperative serum creatinine >1.4 mg/dL; (ii) left ventricular ejection fraction <35% or congestive heart failure (iii) age >70 years (iv) diabetes (v) re-operation
IV NAC 150 mg/kg bolus followed by 24 hours of 150 mg/kg NAC
placebo
117 AKI (AKIN)
Urine output
35% (NAC) vs 32% (placebo) (p = 0.695)4982 ± 1185 mL (NAC) vs. 5528 ± 1247 mL (placebo) (p=0.017)
Fraga CM 2016 [82]
RCTC
General ICU , new onset hypotension (MAP < 60 mmHg)
IV NAC 50 mg/kg over 4h followed by 48h of 100 mg/kg/d NAC + deferoxamine (DFX) 1000mg
placebo
80 AKI
AKI duration
RRT
Mortality
NAC/DFX vs. placebo: 65% vs. 67%; adjusted RR 1.1 (95% CI: 0.37-3.2) 1d (NAC(DFX) vs. 0.5d (p=0.04)15% vs. 15%; adjusted RR 1.1 (95% CI: 0.3-4.2) 60% vs. 57% adjusted RR 1.3 (95% CI: 0.51-3.7)
NAC effect indistinguishable from DFX effect, thus level of evidence downgraded
RCT = randomised controlled trial, NAG = Urine N-acetyl-β-D-glucosaminidase, SCr = serum creatinine, NAC = N-acetylcysteine, DFX= deferoxamine, MV = mechanical ventilation, LOS = length of stay, ICU = intensive care unit.

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S14: Recent meta-analyses evaluating the renoprotective effect of statins following coronary angiography / interventionsAuthorYear
Study designEvidence (A-C)
Clinical setting Intervention Number of patients included
Endpoints Results Comments
Navarese EP 2017
[83]
Network Meta-
analysis
A
Patients undergoing
cardiovascular
procedures with
contrast
Statin versus
Saline / sodium
bicacarbonate /
saline + NAC /
prostaglandin
2951 patients AKI RR 0.36 – 0.51
Su X 2016 [84] Bayesian network
meta-analysis
A
Patients undergoing
procedures with
contrast
High dose statins
Placebo / control
Low dose statin
Placebo / control
13 RCTs including
2612 patients
AKI OR 0.37 (95% CI 0.17-0.72)
OR 0.98 (95% CI 0.41 – 2.07) low dose statins
not effective
Li H 2016 [85] Meta-analysis
A
Patients undergoing
procedures with
contrast
Statin
Placebo
21 RCTs including
7746 patients
AKI RR 0.57 (95% CI 0.47-0.69)
Wang N 2016 [86] Meta-analysis
A
Patients undergoing
coronary
catheterisation
Statin
Placebo
14 RCTs including
6033 patients
AKI 3.7% vs 8.3% ; p<0.00001
Thompson K 2016
[87]
Meta-analysis
A
Patients undergoing
angiography
Statin
Placebo
19 RCTs including
7161 patients
AKI RR 0.52 (95% CI 0.40-0.67)
Yang Y 2015 [88] Meta-analysis
A
Patients undergoing
coronary
Statin
Placebo
5 RCTs including
4045 patients
AKI OR 0.49 (95% CI 0.37-0.66)

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
catheterisation
Marenzi G 2015
[89]
Meta-analysis
A
Patients undergoing
coronary
catheterisation
Statin
Placebo
9 RCTs including
5212 patients
AKI RR 0.50 (95% CI 0.39-0.64)
Wu H 2015 [90] Meta-analysis
A
Patients undergoing
coronary angiography
High dose statin
versus low dose
statin
14 RCTs including
1689 patients
AKI RR 0.41 (95% CI 0.29-0.56)
Liu YH 2015 [91] Meta-analysis
A
Patients undergoing
coronary
catheterisation
Statin versus
placebo
9 RCTs including
5143 patients
AKI
RRT
mortality
RR 0.47 (95% CI 0.37-0.60)
OR 0.14 (95% CI 0.03-0.60)
RR 0.77 (95% CI 0.28-2.12)
Briasoulis A 2015
[92]
Meta-analysis
A
Patients undergoing
interventions which
require contrast
Statin versus
placebo/control
9 RCTs including
4984 patients
AKI OR 0.45 (95% CI 0.34-0.58)
Ukaigwe A 2014
[93]
Meta-analysis
A
Patients undergoing
coronary angiography
High dose statin
versus low dose
statin or placebo
12 RCTs including
5564 patients
AKI OR 0.43 (95% CI 0.33-0.55)
Lee JM 2014 [94] Meta-analysis
A
Patients undergoing
coronary angiography
Statin
Placebo
13 RCTs including
5825 patients
AKI High dose statins:
RR 0.45 (95% CI 0.35-0.57)
Singh N 2014 [95] Meta-analysis
A
Patients exposed to
contrast
Statin
Placebo
9 RCTs including
5143 patients
AKI RR 0.47 (95% CI 0.34-0.64)
Peruzzi M 2014
[96]
Network
Meta-analysis
A
Patients exposed to
contrast
Statin
Placebo
14 RCTs including
6160 patients AKI
RRT
High dose statins:
OR 0.47 (95% CI 0.37-0.60)
OR 0.27 (95% CI 0.07-1.09)

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
90-day mortality OR 0.80 (95% CI 0.31-2.10)
Barbieri L et al.
2014 [97]
Meta-analysis
A
Patients undergoing
contrast angiography /
angioplasty
Statin
Placebo
8 RCTs including
4734 patients
AKI OR 0.50 (95% CI 0.38–0.66)
RCT = randomised controlled trial, RRT = renal replacement therapy, AKI = acute kidney injury; OR = odds ratio, RR = relative risk, CI = confidence interval

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S15: Recent meta-analyses and randomised controlled studies not included in the meta-analyses evaluating the renoprotective
effect of statins in cardiac surgeryAuthoryear
Study designEvidence (A-C)
Clinical setting Intervention Number of patients included
Endpoints Results Comments
Park JH 2016 [98] RCT
B
Patients undergoing
valvular surgery
Statin
Placebo
200 patients AKI 21% versus 24%; p=0.40
Xiong B 2017 [99] Meta-analysis
A
Patients requiring
cardiac bypass
surgery
Statin
Placebo
9 RCTs including
3201 patients
AKI
RRT
RR 1.12 (95% CI 0.97 – 1.29)
RR 1.13 (95% CI 0.45 – 2.85)
Yuan X 2017
[100]
Meta-analysis
A
Patients requiring
cardiac bypass
surgery
Statin
Placebo / control
8 RCTs including
3204 patients
AKI OR 1.01 (95% CI 0.75 – 1.36)
Putzu A 2016
[101]
Meta-analysis
A
Patients requiring
cardiac bypass
surgery
Statin
Placebo or no
treatment
23 RCTs including
5102 patients
AKI OR 1.26 (95% CI 1.05 – 1.52)
Li M
2016 [102]
Meta-analysis
C
Patients requiring
cardiac bypass
surgery
Statin
Control
17 studies
41717 patients
AKI
mortality
OR 0.72 (95% CI 0.55 – 0.94)
OR 0.40 (95% CI 0.22 – 0.72)
Lewicki M 2015
[103]
Meta-analysis
A
Patients requiring
cardiac bypass
surgery
Statin
Placebo
7 RCTs including
662 patients
AKI
RRT
mortality
RR 0.76 (95% CI 0.46-1.28)
RR 0.80 (95% CI 0.23-2.81)
RR 3.86 (95% CI 0.43-34.4)
RCT= randomised controlled trial, RRT = renal replacement therapy, AKI = acute kidney injury

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Table S16: Randomised controlled studies and meta-analyses evaluating the renal protective effect of remote ischaemic preconditioning Author/year Study design
Evidence (A-C)
Clinical setting Intervention
Number of patients included
Endpoints Results Comments
Li 2013 [104] Meta-analysisB
Cardiac and vascular interventions
RIPC 924 AKI RR 0.73 (0.50, 1.06), p = 0.10
Yang 2014 [105]
Meta-analysisB
Cardiac and vascular interventions
RIPC 13 studies, 1334 patients
AKI, RRT, kidney biomarkers, in-hospital mortality, length of stay in the ICU and in-hospital
AKI: RR 0.70 (0.48, 1.02), p = 0.06. All other endpoints also similar
Pei 2014 [106]
Meta-analysis B
Coronary intervention
RIPC 11 studies, 1713 patients
CA-AKI OR 0.61 (0.38, 0.98), p = 0.04 Reduction of myocardial infarction OR0.68 (0.51, 0.91), p = 0.01
Li 2017 [107] Meta-analysis B
Cardiac and vascular interventions
RIPC 26 studies, 699 patients
AKI, RRT AKI: RR 0.79 (0.66, 0.95), p = 0.01RRT: RR 1.02 (0.45, 2.30), p = 0.96
Reduced length of ICU stay, similar length of hospital stay
Hu 2016 [108]
Meta-analysisB
Cardiac or aortic surgery (IR) and contrast administration (CA)
RIPC 30 studies, 7244 patients
AKI AKI: RR 0.834 (0.728, 0.955)IR-AKI: RR 0.905 (0.783, 1.045)CA-AKI: RR 0.430 (0.286, 0.648)
No effect on RRT, change in serum creatinine and eGFR, mortality (hospital and d30), or length of hospital stay
Zhang 2016 [109]
Meta-analysis B
On-pump cardiac surgery
RIPC 19 studies, 5100 patients
AKI, RRT, postop creatinine
AKI: OR 0.84 (0.73, 0.98)RRT: OR 0.76 (0.46, 1.24)
Similar postop. creatinine on day 1 and 2Similar hospital mortality
Zhou 2016 [110]
Meta-analysis B
Elective coronary revascularization; PCI and CABG
RIPC 20 studies, 4858 patients
AKI PCI AKI: OR 0.51 (0.31, 0.82)CABGAKI: OR 0.94 (0.73, 1.19)RRT: OR 1.04 (0.62, 1.76)
CABG: Similar hospital mortalityNo effct on AKI.

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Zhang 2016 [111]
Meta-analysis B
PCI and CABG RIPC 37 studies, 81668 patients
AKI Investigator defined AKIRR 0.84 (0.73, 0.96)PCIRR 0.64 (0.46, 0.87)CABGRR 0.93 (0.82, 1.06)KDIGO variant AKIRR 0.87 (0.74, 1.02)
Uncertainty of effect due to use of non-standardized AKI definition
Yi 2016 [112] Meta-analysis B
PCI and cardiac surgery with CPB
RIPC 13 studies4370 patients
AKI RRT
AKI: RR 0.81 (0.66, 0.99)RRT: RR 0.82 (0.20, 3.39)
Sukkar 2016 [113]
Meta-analysis B
Invasive procedures
RIPC 85 studies13800 patients
AKI AKI: RR 0.83 (0.71, 0.97) Beneficial effect on AKI was predominantly in AKIN 1, and attenuated in AKIN stage 2 and 3.Low event rate!No effect on mortality, myocardial infarction, stroke, major adverse cardiovascular events
Zhou 2017 [114]
Meta-analysis B
Cardiac surgery RIPC 21 studies6302 patients
AKI AKI: OR 0.79 (0.65, 0.96)AKI stage 1: OR 0.65 (0.47, 0.89)
Shorter duration of mechanical ventilation and ICU stayMeta-regression showed benefit in younger patients undergoing non-complex surgery
Pierce 2017 [115]
Meta-analysis B
Cardiac surgery RIPC 21 studies, 5262 patients
AKI
mortality
AKI: 24.7% vs. 27.2%, RR 0.839 (0.703, 1.001)Only studies with propofol free anaesthesiaAKI: 32.7% vs. 47.5%, RR 0.700 (0.527, 0.930)
Effect on AKI only if analysis was restricted to studies with propofol free anesthesia
No difference in mortality and myocardial infarction

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
Menting 2017 [116]
Meta-analysis B
Surgery (kidney transplantation excluded)
RIPC 28 studies6851 patients
serum-creatinine d1, d2, d3
AKI (RIFLE)
AKI (AKIN)
RRT
Creatinine d1: mean diff 0. 02 mg/dL (-0.05, 0.02)Creatinine d2: mean diff -0.04 (-0.09, 0.02)Creatinine d3: mean diff –0.05 (-0.19, 0.10)AKI (RIFLE): RR 0.91 (0.75, 1.12)AKI (AKIN): RR 0.76 (0.57, 1.00)RRT: RR 0.85 (0.37, 1.9)
No difference in adverse effects, length of hospital stay
Effect on AKI depending on AKI definition used (AKIN or RIFLE)
Randomised controlled trialsWalsh 2016 [117]
RCT A
High risk cardiac surgery
RIPC 258 serum-creatinine
AKIRRT
Creatinine: mean diff 0.06 (-0.10, 0.23)AKI: RR 1.10 (0.68, 1.78)RRT: 4.8% vs. 0.8%
CK-MB myocardial infarction, stroke, and death were similar in both groups
Kim 2017 [118]
RCT B
Cardiac surgery on CPB
RIPC delayed (24-48h prior surgery)Sham
160 serum-creatinineAKI
Creatinine: p=0.615AKI: 30.0% vs. 47.5%, RR 0.768 (0.599, 0.985)
Lower rate of complications Troponin I (72h AUC) 743.5 vs. 530.8, p=0.662
Zarbock 2017 [119]
RCT A
High risk cardiac surgery
RIPC 240 90-day outcomes:MAKE90, RRT,
Non-recovery of AKI
MAKE90:14.2% vs. 25.0%, ARR 10.8% (0.9%, 20.8%)RRT d90: 14.3% vs. 2.6%, ARR 11.7% (1.2%, 22.1%)Non-recovery d90: 5.3% vs. 23.2%, ARR 17.9% (4.8%, 31.1%)
RIPC= remote ischaemic preconditioning, RCT= randomised controlled trial, RRT = renal replacement therapy, AKI = acute kidney injury, CA-AKI = conrast media associated AKI, MAKE= major adverse kidney events

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
References
1. Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, McGuinness S, Mehrtens J, Myburgh J, Psirides A, Reddy S, Bellomo R, (2015) Effect of a Buffered Crystalloid Solution vs Saline on Acute Kidney Injury Among Patients in the Intensive Care Unit: The SPLIT Randomized Clinical Trial. Jama 314: 1701-1710
2. Semler MW, Wanderer JP, Ehrenfeld JM, Stollings JL, Self WH, Siew ED, Wang L, Byrne DW, Shaw AD, Bernard GR, Rice TW, Investigators S, the Pragmatic Critical Care Research G, (2016) Balanced Crystalloids versus Saline in the Intensive Care Unit: The SALT Randomized Trial. Am J Respir Crit Care Med
3. Stockwell MA, Scott A, Day A, Riley B, Soni N, (1992) Colloid solutions in the critically ill. A randomised comparison of albumin and polygeline 2. Serum albumin concentration and incidences of pulmonary oedema and acute renal failure. Anaesthesia 47: 7-9
4. Schortgen F, Lacherade JC, Bruneel F, Cattaneo I, Hemery F, Lemaire F, Brochard L, (2001) Effects of hydroxyethylstarch and gelatin on renal function in severe sepsis: a multicentre randomised study. Lancet 357: 911-916
5. Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, Investigators SS, (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350: 2247-2256
6. Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K, German Competence Network S, (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358: 125-139
7. Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, Forceville X, Feissel M, Hasselmann M, Heininger A, Van Aken H, (2012) Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care 16: R94
8. Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J, Group ST, Scandinavian Critical Care Trials G, (2012) Hydroxyethyl starch 130/0.42 versus Ringer's acetate in severe sepsis. N Engl J Med 367: 124-134
9. Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SA, Investigators C, Australian, New Zealand Intensive Care Society Clinical Trials G, (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367: 1901-1911

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
10. Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, Iapichino G, Antonelli M, Parrini V, Fiore G, Latini R, Gattinoni L, Investigators AS, (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370: 1412-1421
11. Zarychanski R, Abou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, Fergusson DA, (2013) Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. Jama 309: 678-688
12. Haase M, Haase-Fielitz A, Plass M, Kuppe H, Hetzer R, Hannon C, Murray PT, Bailey MJ, Bellomo R, Bagshaw SM, (2013) Prophylactic perioperative sodium bicarbonate to prevent acute kidney injury following open heart surgery: a multicenter double-blinded randomized controlled trial. PLoS medicine 10: e1001426
13. Gattas DJ, Dan A, Myburgh J, Billot L, Lo S, Finfer S, Committee CM, (2013) Fluid resuscitation with 6 % hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Med 39: 558-568
14. Rochwerg B, Alhazzani W, Gibson A, Ribic CM, Sindi A, Heels-Ansdell D, Thabane L, Fox-Robichaud A, Mbuagbaw L, Szczeklik W, Alshamsi F, Altayyar S, Ip W, Li G, Wang M, Wludarczyk A, Zhou Q, Annane D, Cook DJ, Jaeschke R, Guyatt GH, (2015) Fluid type and the use of renal replacement therapy in sepsis: a systematic review and network meta-analysis. Intensive Care Med 41: 1561-1571
15. Moeller C, Fleischmann C, Thomas-Rueddel D, Vlasakov V, Rochwerg B, Theurer P, Gattinoni L, Reinhart K, Hartog CS, (2016) How safe is gelatin? A systematic review and meta-analysis of gelatin-containing plasma expanders vs crystalloids and albumin. Journal of critical care 35: 75-83
16. Sampath S, Moran JL, Graham PL, Rockliff S, Bersten AD, Abrams KR, (2007) The efficacy of loop diuretics in acute renal failure: assessment using Bayesian evidence synthesis techniques. Crit Care Med 35: 2516-2524
17. Bagshaw SM, Delaney A, Haase M, Ghali WA, Bellomo R, (2007) Loop diuretics in the management of acute renal failure: a systematic review and meta-analysis. Crit Care Resusc 9: 60-68
18. Ho KM, Power BM, (2010) Benefits and risks of furosemide in acute kidney injury. Anaesthesia 65: 283-29319. Wu MY, Chang NC, Su CL, Hsu YH, Chen TW, Lin YF, Wu CH, Tam KW, (2014) Loop diuretic strategies in patients with acute
decompensated heart failure: a meta-analysis of randomized controlled trials. Journal of critical care 29: 2-920. Hager B, Betschart M, Krapf R, (1996) Effect of postoperative intravenous loop diuretic on renal function after major surgery. Schweiz
Med Wochenschr 126: 666-67321. Lassnigg A, Donner E, Grubhofer G, Presterl E, Druml W, Hiesmayr M, (2000) Lack of renoprotective effects of dopamine and
furosemide during cardiac surgery. J Am Soc Nephrol 11: 97-104

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
22. Sirivella S, Gielchinsky I, Parsonnet V, (2000) Mannitol, furosemide, and dopamine infusion in postoperative renal failure complicating cardiac surgery. Ann Thorac Surg 69: 501-506
23. Stafford-Smith M, Patel UD, Phillips-Bute BG, Shaw AD, Swaminathan M, (2008) Acute kidney injury and chronic kidney disease after cardiac surgery. Adv Chronic Kidney Dis 15: 257-277
24. Kunt AT, Akgun S, Atalan N, Bitir N, Arsan S, (2009) Furosemide infusion prevents the requirement of renal replacement therapy after cardiac surgery. Anadolu Kardiyol Derg 9: 499-504
25. Majumdar SR, Kjellstrand CM, Tymchak WJ, Hervas-Malo M, Taylor DA, Teo KK, (2009) Forced euvolemic diuresis with mannitol and furosemide for prevention of contrast-induced nephropathy in patients with CKD undergoing coronary angiography: a randomized controlled trial. Am J Kidney Dis 54: 602-609
26. Marenzi G, Ferrari C, Marana I, Assanelli E, De Metrio M, Teruzzi G, Veglia F, Fabbiocchi F, Montorsi P, Bartorelli AL, (2012) Prevention of contrast nephropathy by furosemide with matched hydration: the MYTHOS (Induced Diuresis With Matched Hydration Compared to Standard Hydration for Contrast Induced Nephropathy Prevention) trial. JACC Cardiovasc Interv 5: 90-97
27. Palazzuoli A, Pellegrini M, Ruocco G, Martini G, Franci B, Campagna MS, Gilleman M, Nuti R, McCullough PA, Ronco C, (2014) Continuous versus bolus intermittent loop diuretic infusion in acutely decompensated heart failure: a prospective randomized trial. Crit Care 18: R134
28. Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, Dequin PF, Gergaud S, Weiss N, Legay F, Le Tulzo Y, Conrad M, Robert R, Gonzalez F, Guitton C, Tamion F, Tonnelier JM, Guezennec P, Van Der Linden T, Vieillard-Baron A, Mariotte E, Pradel G, Lesieur O, Ricard JD, Herve F, du Cheyron D, Guerin C, Mercat A, Teboul JL, Radermacher P, Investigators S, (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370: 1583-1593
29. Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, Moy CS, Silbergleit R, Steiner T, Suarez JI, Toyoda K, Wang Y, Yamamoto H, Yoon BW, Investigators A-T, the Neurological Emergency Treatment Trials N, (2016) Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med 375: 1033-1043
30. Russell JA, Walley KR, Singer J, Gordon AC, Hebert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D, Investigators V, (2008) Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 358: 877-887
31. Gordon AC, Russell JA, Walley KR, Singer J, Ayers D, Storms MM, Holmes CL, Hebert PC, Cooper DJ, Mehta S, Granton JT, Cook DJ, Presneill JJ, (2010) The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med 36: 83-91
32. De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, Brasseur A, Defrance P, Gottignies P, Vincent JL, Investigators SI, (2010) Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 362: 779-789

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
33. Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, Pogson DG, Aya HD, Anjum A, Frazier GJ, Santhakumaran S, Ashby D, Brett SJ, Investigators V, (2016) Effect of Early Vasopressin vs Norepinephrine on Kidney Failure in Patients With Septic Shock: The VANISH Randomized Clinical Trial. JAMA 316: 509-518
34. Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, Rhodes A, Landoni G, Osawa EA, Melo RR, Sundin MR, Grande SM, Gaiotto FA, Pomerantzeff PM, Dallan LO, Franco RA, Nakamura RE, Lisboa LA, de Almeida JP, Gerent AM, Souza DH, Gaiane MA, Fukushima JT, Park CL, Zambolim C, Rocha Ferreira GS, Strabelli TM, Fernandes FL, Camara L, Zeferino S, Santos VG, Piccioni MA, Jatene FB, Costa Auler JO, Jr., Filho RK, (2017) Vasopressin versus Norepinephrine in Patients with Vasoplegic Shock after Cardiac Surgery: The VANCS Randomized Controlled Trial. Anesthesiology 126: 85-93
35. Friedrich JO, Adhikari N, Herridge MS, Beyene J, (2005) Meta-analysis: low-dose dopamine increases urine output but does not prevent renal dysfunction or death. Ann Intern Med 142: 510-524
36. Landoni G, Biondi-Zoccai GG, Tumlin JA, Bove T, De Luca M, Calabro MG, Ranucci M, Zangrillo A, (2007) Beneficial impact of fenoldopam in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Am J Kidney Dis 49: 56-68
37. Landoni G, Biondi-Zoccai GG, Marino G, Bove T, Fochi O, Maj G, Calabro MG, Sheiban I, Tumlin JA, Ranucci M, Zangrillo A, (2008) Fenoldopam reduces the need for renal replacement therapy and in-hospital death in cardiovascular surgery: a meta-analysis. J Cardiothorac Vasc Anesth 22: 27-33
38. Zangrillo A, Biondi-Zoccai GG, Frati E, Covello RD, Cabrini L, Guarracino F, Ruggeri L, Bove T, Bignami E, Landoni G, (2012) Fenoldopam and acute renal failure in cardiac surgery: a meta-analysis of randomized placebo-controlled trials. J Cardiothorac Vasc Anesth 26: 407-413
39. Gillies MA, Kakar V, Parker RJ, Honore PM, Ostermann M, (2015) Fenoldopam to prevent acute kidney injury after major surgery-a systematic review and meta-analysis. Crit Care 19: 449
40. Bove T, Zangrillo A, Guarracino F, Alvaro G, Persi B, Maglioni E, Galdieri N, Comis M, Caramelli F, Pasero DC, Pala G, Renzini M, Conte M, Paternoster G, Martinez B, Pinelli F, Frontini M, Zucchetti MC, Pappalardo F, Amantea B, Camata A, Pisano A, Verdecchia C, Dal CE, Cariello C, Faita L, Baldassarri R, Scandroglio AM, Saleh O, Lembo R, Calabro MG, Bellomo R, Landoni G, (2014) Effect of fenoldopam on use of renal replacement therapy among patients with acute kidney injury after cardiac surgery: a randomized clinical trial. JAMA 312: 2244-2253
41. Nigwekar SU, Navaneethan SD, Parikh CR, Hix JK, (2009) Atrial natriuretic peptide for management of acute kidney injury: a systematic review and meta-analysis. Clin J Am Soc Nephrol 4: 261-272
42. Mitaka C, Kudo T, Haraguchi G, Tomita M, (2011) Cardiovascular and renal effects of carperitide and nesiritide in cardiovascular surgery patients: a systematic review and meta-analysis. Crit Care 15: R258

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
43. Xiong B, Wang C, Yao Y, Huang Y, Tan J, Cao Y, Zou Y, Huang J, (2015) The dose-dependent effect of nesiritide on renal function in patients with acute decompensated heart failure: a systematic review and meta-analysis of randomized controlled trials. PLoS One 10: e0131326
44. Mori Y, Kamada T, Ochiai R, (2014) Reduction in the incidence of acute kidney injury after aortic arch surgery with low-dose atrial natriuretic peptide: a randomised controlled trial. Eur J Anaesthesiol 31: 381-387
45. Sezai A, Nakata K, Iida M, Yoshitake I, Wakui S, Hata H, Shiono M, (2013) Results of low-dose carperitide infusion in high-risk patients undergoing coronary artery bypass grafting. Ann Thorac Surg 96: 119-126
46. Bove T, Matteazzi A, Belletti A, Paternoster G, Saleh O, Taddeo D, Dossi R, Greco T, Bradic N, Husedzinovic I, Nigro Neto C, Lomivorotov VV, Calabro MG, (2015) Beneficial impact of levosimendan in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Heart, lung and vessels 7: 35-46
47. Zhou C, Gong J, Chen D, Wang W, Liu M, Liu B, (2016) Levosimendan for Prevention of Acute Kidney Injury After Cardiac Surgery: A Meta-analysis of Randomized Controlled Trials. Am J Kidney Dis 67: 408-416
48. Gordon AC, Perkins GD, Singer M, McAuley DF, Orme RM, Santhakumaran S, Mason AJ, Cross M, Al-Beidh F, Best-Lane J, Brealey D, Nutt CL, McNamee JJ, Reschreiter H, Breen A, Liu KD, Ashby D, (2016) Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis. N Engl J Med 375: 1638-1648
49. Mehta RH, Leimberger JD, van Diepen S, Meza J, Wang A, Jankowich R, Harrison RW, Hay D, Fremes S, Duncan A, Soltesz EG, Luber J, Park S, Argenziano M, Murphy E, Marcel R, Kalavrouziotis D, Nagpal D, Bozinovski J, Toller W, Heringlake M, Goodman SG, Levy JH, Harrington RA, Anstrom KJ, Alexander JH, Investigators L-C, (2017) Levosimendan in Patients with Left Ventricular Dysfunction Undergoing Cardiac Surgery. N Engl J Med
50. Landoni G, Lomivorotov VV, Alvaro G, Lobreglio R, Pisano A, Guarracino F, Calabro MG, Grigoryev EV, Likhvantsev VV, Salgado-Filho MF, Bianchi A, Pasyuga VV, Baiocchi M, Pappalardo F, Monaco F, Boboshko VA, Abubakirov MN, Amantea B, Lembo R, Brazzi L, Verniero L, Bertini P, Scandroglio AM, Bove T, Belletti A, Michienzi MG, Shukevich DL, Zabelina TS, Bellomo R, Zangrillo A, Group CS, (2017) Levosimendan for Hemodynamic Support after Cardiac Surgery. N Engl J Med
51. Leino K, Hynynen M, Jalonen J, Salmenpera M, Scheinin H, Aantaa R, Dexmedetomidine in Cardiac Surgery Study G, (2011) Renal effects of dexmedetomidine during coronary artery bypass surgery: a randomized placebo-controlled study. BMC anesthesiology 11: 9
52. Balkanay OO, Goksedef D, Omeroglu SN, Ipek G, (2015) The dose-related effects of dexmedetomidine on renal functions and serum neutrophil gelatinase-associated lipocalin values after coronary artery bypass grafting: a randomized, triple-blind, placebo-controlled study. Interactive cardiovascular and thoracic surgery 20: 209-214
53. Cho JS, Shim JK, Soh S, Kim MK, Kwak YL, (2016) Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int 89: 693-700

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
54. van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R, (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345: 1359-1367
55. Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R, (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354: 449-461
56. Arabi YM, Dabbagh OC, Tamim HM, Al-Shimemeri AA, Memish ZA, Haddad SH, Syed SJ, Giridhar HR, Rishu AH, Al-Daker MO, Kahoul SH, Britts RJ, Sakkijha MH, (2008) Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med 36: 3190-3197
57. De La Rosa Gdel C, Donado JH, Restrepo AH, Quintero AM, Gonzalez LG, Saldarriaga NE, Bedoya M, Toro JM, Velasquez JB, Valencia JC, Arango CM, Aleman PH, Vasquez EM, Chavarriaga JC, Yepes A, Pulido W, Cadavid CA, Grupo de Investigacion en Cuidado intensivo G-H, (2008) Strict glycaemic control in patients hospitalised in a mixed medical and surgical intensive care unit: a randomised clinical trial. Crit Care 12: R120
58. Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R, (2009) A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 35: 1738-1748
59. Investigators N-SS, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ, (2009) Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360: 1283-1297
60. Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R, (2011) Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr 93: 569-577
61. Wiener RS, Wiener DC, Larson RJ, (2008) Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 300: 933-944
62. Ling Y, Li X, Gao X, (2012) Intensive versus conventional glucose control in critically ill patients: a meta-analysis of randomized controlled trials. Eur J Intern Med 23: 564-574
63. Endre ZH, Walker RJ, Pickering JW, Shaw GM, Frampton CM, Henderson SJ, Hutchison R, Mehrtens JE, Robinson JM, Schollum JB, Westhuyzen J, Celi LA, McGinley RJ, Campbell IJ, George PM, (2010) Early intervention with erythropoietin does not affect the outcome of acute kidney injury (the EARLYARF trial). Kidney Int 77: 1020-1030
64. Shema-Didi L, Kristal B, Eizenberg S, Marzuq N, Sussan M, Feldman-Idov Y, Ofir P, Atar S, (2016) Prevention of contrast-induced nephropathy with single bolus erythropoietin in patients with diabetic kidney disease: A randomized controlled trial. Nephrology (Carlton) 21: 295-300

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
65. Song YR, Lee T, You SJ, Chin HJ, Chae DW, Lim C, Park KH, Han S, Kim JH, Na KY, (2009) Prevention of acute kidney injury by erythropoietin in patients undergoing coronary artery bypass grafting: a pilot study. Am J Nephrol 30: 253-260
66. Yoo YC, Shim JK, Kim JC, Jo YY, Lee JH, Kwak YL, (2011) Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology 115: 929-937
67. de Seigneux S, Ponte B, Weiss L, Pugin J, Romand JA, Martin PY, Saudan P, (2012) Epoetin administrated after cardiac surgery: effects on renal function and inflammation in a randomized controlled study. BMC Nephrol 13: 132
68. Tasanarong A, Duangchana S, Sumransurp S, Homvises B, Satdhabudha O, (2013) Prophylaxis with erythropoietin versus placebo reduces acute kidney injury and neutrophil gelatinase-associated lipocalin in patients undergoing cardiac surgery: a randomized, double-blind controlled trial. BMC Nephrol 14: 136
69. Kim JH, Shim JK, Song JW, Song Y, Kim HB, Kwak YL, (2013) Effect of erythropoietin on the incidence of acute kidney injury following complex valvular heart surgery: a double blind, randomized clinical trial of efficacy and safety. Crit Care 17: R254
70. Dardashti A, Ederoth P, Algotsson L, Bronden B, Grins E, Larsson M, Nozohoor S, Zinko G, Bjursten H, (2014) Erythropoietin and protection of renal function in cardiac surgery (the EPRICS Trial). Anesthesiology 121: 582-590
71. Kim JE, Song SW, Kim JY, Lee HJ, Chung KH, Shim YH, (2016) Effect of a Single Bolus of Erythropoietin on Renoprotection in Patients Undergoing Thoracic Aortic Surgery With Moderate Hypothermic Circulatory Arrest. Ann Thorac Surg 101: 690-696
72. Tie HT, Luo MZ, Lin D, Zhang M, Wan JY, Wu QC, (2015) Erythropoietin administration for prevention of cardiac surgery-associated acute kidney injury: a meta-analysis of randomized controlled trials. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery 48: 32-39
73. Penny-Dimri JC, Cochrane AD, Perry LA, Smith JA, (2016) Characterising the Role of Perioperative Erythropoietin for Preventing Acute Kidney Injury after Cardiac Surgery: Systematic Review and Meta-Analysis. Heart, lung & circulation 25: 1067-1076
74. Zhao C, Lin Z, Luo Q, Xia X, Yu X, Huang F, (2015) Efficacy and Safety of Erythropoietin to Prevent Acute Kidney Injury in Patients With Critical Illness or Perioperative Care: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Journal of cardiovascular pharmacology 65: 593-600
75. Burns KE, Chu MW, Novick RJ, Fox SA, Gallo K, Martin CM, Stitt LW, Heidenheim AP, Myers ML, Moist L, (2005) Perioperative N-acetylcysteine to prevent renal dysfunction in high-risk patients undergoing cabg surgery: a randomized controlled trial. JAMA 294: 342-350
76. Macedo E, Abdulkader R, Castro I, Sobrinho AC, Yu L, Vieira JM, Jr., (2006) Lack of protection of N-acetylcysteine (NAC) in acute renal failure related to elective aortic aneurysm repair-a randomized controlled trial. Nephrol Dial Transplant 21: 1863-1869
77. Komisarof JA, Gilkey GM, Peters DM, Koudelka CW, Meyer MM, Smith SM, (2007) N-acetylcysteine for patients with prolonged hypotension as prophylaxis for acute renal failure (NEPHRON). Crit Care Med 35: 435-441

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
78. Sisillo E, Ceriani R, Bortone F, Juliano G, Salvi L, Veglia F, Fiorentini C, Marenzi G, (2008) N-acetylcysteine for prevention of acute renal failure in patients with chronic renal insufficiency undergoing cardiac surgery: a prospective, randomized, clinical trial. Crit Care Med 36: 81-86
79. Adabag AS, Ishani A, Koneswaran S, Johnson DJ, Kelly RF, Ward HB, McFalls EO, Bloomfield HE, Chandrashekhar Y, (2008) Utility of N-acetylcysteine to prevent acute kidney injury after cardiac surgery: a randomized controlled trial. Am Heart J 155: 1143-1149
80. Wijeysundera DN, Beattie WS, Rao V, Granton JT, Chan CT, (2007) N-acetylcysteine for preventing acute kidney injury in cardiac surgery patients with pre-existing moderate renal insufficiency. Can J Anaesth 54: 872-881
81. Song JW, Shim JK, Soh S, Jang J, Kwak YL, (2015) Double-blinded, randomized controlled trial of N-acetylcysteine for prevention of acute kidney injury in high risk patients undergoing off-pump coronary artery bypass. Nephrology (Carlton) 20: 96-102
82. Fraga CM, Tomasi CD, Damasio DC, Vuolo F, Ritter C, Dal-Pizzol F, (2016) N-acetylcysteine plus deferoxamine for patients with prolonged hypotension does not decrease acute kidney injury incidence: a double blind, randomized, placebo-controlled trial. Crit Care 20: 331
83. Navarese EP, Gurbel PA, Andreotti F, Kolodziejczak MM, Palmer SC, Dias S, Buffon A, Kubica J, Kowalewski M, Jadczyk T, Laskiewicz M, Jedrzejek M, Brockmeyer M, Airoldi F, Ruospo M, De Servi S, Wojakowski W, C OC, Strippoli GF, (2017) Prevention of contrast-induced acute kidney injury in patients undergoing cardiovascular procedures-a systematic review and network meta-analysis. PLoS One 12: e0168726
84. Su X, Xie X, Liu L, Lv J, Song F, Perkovic V, Zhang H, (2016) Comparative Effectiveness of 12 Treatment Strategies for Preventing Contrast-Induced Acute Kidney Injury: A Systematic Review and Bayesian Network Meta-analysis. Am J Kidney Dis
85. Li H, Wang C, Liu C, Li R, Zou M, Cheng G, (2016) Efficacy of Short-Term Statin Treatment for the Prevention of Contrast-Induced Acute Kidney Injury in Patients Undergoing Coronary Angiography/Percutaneous Coronary Intervention: A Meta-Analysis of 21 Randomized Controlled Trials. American journal of cardiovascular drugs : drugs, devices, and other interventions 16: 201-219
86. Wang N, Qian P, Yan TD, Phan K, (2016) Periprocedural effects of statins on the incidence of contrast-induced acute kidney injury: A systematic review and trial sequential analysis. Int J Cardiol 206: 143-152
87. Thompson K, Razi R, Lee MS, Shen A, Stone GW, Hiremath S, Mehran R, Brar SS, (2016) Statin use prior to angiography for the prevention of contrast-induced acute kidney injury: a meta-analysis of 19 randomised trials. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology 12: 366-374
88. Yang Y, Wu YX, Hu YZ, (2015) Rosuvastatin Treatment for Preventing Contrast-Induced Acute Kidney Injury After Cardiac Catheterization: A Meta-Analysis of Randomized Controlled Trials. Medicine 94: e1226

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
89. Marenzi G, Cosentino N, Werba JP, Tedesco CC, Veglia F, Bartorelli AL, (2015) A meta-analysis of randomized controlled trials on statins for the prevention of contrast-induced acute kidney injury in patients with and without acute coronary syndromes. Int J Cardiol 183: 47-53
90. Wu H, Li D, Fang M, Han H, Wang H, (2015) Meta-analysis of short-term high versus low doses of atorvastatin preventing contrast-induced acute kidney injury in patients undergoing coronary angiography/percutaneous coronary intervention. Journal of clinical pharmacology 55: 123-131
91. Liu YH, Liu Y, Duan CY, Tan N, Chen JY, Zhou YL, Li LW, He PC, (2015) Statins for the Prevention of Contrast-Induced Nephropathy After Coronary Angiography/Percutaneous Interventions: A Meta-analysis of Randomized Controlled Trials. J Cardiovasc Pharmacol Ther 20: 181-192
92. Briasoulis A, Mallikethi-Reddy S, Sharma S, Briasouli AA, Afonso L, (2015) 3-Hydroxy-3-methylglutaryl-CoA reductase enzyme inhibitors for prevention of contrast-induced nephropathy: a meta-analysis of prospective randomized controlled studies. Am J Ther 22: e158-166
93. Ukaigwe A, Karmacharya P, Mahmood M, Pathak R, Aryal MR, Jalota L, Donato AA, (2014) Meta-analysis on efficacy of statins for prevention of contrast-induced acute kidney injury in patients undergoing coronary angiography. Am J Cardiol 114: 1295-1302
94. Lee JM, Park J, Jeon KH, Jung JH, Lee SE, Han JK, Kim HL, Yang HM, Park KW, Kang HJ, Koo BK, Jo SH, Kim HS, (2014) Efficacy of short-term high-dose statin pretreatment in prevention of contrast-induced acute kidney injury: updated study-level meta-analysis of 13 randomized controlled trials. PLoS One 9: e111397
95. Singh N, Lee JZ, Huang JJ, Low SW, Howe C, Pandit A, Suryanarayana P, Lee KS, (2014) Benefit of statin pretreatment in prevention of contrast-induced nephropathy in different adult patient population: systematic review and meta-analysis. Open Heart 1: e000127
96. Peruzzi M, De Luca L, Thomsen HS, Romagnoli E, D'Ascenzo F, Mancone M, Sardella G, Lucisano L, Abbate A, Frati G, Biondi-Zoccai G, (2014) A network meta-analysis on randomized trials focusing on the preventive effect of statins on contrast-induced nephropathy. BioMed research international 2014: 213239
97. Barbieri L, Verdoia M, Schaffer A, Nardin M, Marino P, De Luca G, (2014) The role of statins in the prevention of contrast induced nephropathy: a meta-analysis of 8 randomized trials. Journal of thrombosis and thrombolysis 38: 493-502
98. Park JH, Shim JK, Song JW, Soh S, Kwak YL, (2016) Effect of atorvastatin on the incidence of acute kidney injury following valvular heart surgery: a randomized, placebo-controlled trial. Intensive Care Med 42: 1398-1407
99. Xiong B, Nie D, Cao Y, Zou Y, Yao Y, Qian J, Rong S, Huang J, (2017) Preoperative Statin Treatment for the Prevention of Acute Kidney Injury in Patients Undergoing Cardiac Surgery: A Meta-Analysis of Randomised Controlled Trials. Heart, lung & circulation
100. Yuan X, Du J, Liu Q, Zhang L, (2017) Defining the role of perioperative statin treatment in patients after cardiac surgery: A meta-analysis and systematic review of 20 randomized controlled trials. Int J Cardiol 228: 958-966

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
101. Putzu A, Capelli B, Belletti A, Cassina T, Ferrari E, Gallo M, Casso G, Landoni G, (2016) Perioperative statin therapy in cardiac surgery: a meta-analysis of randomized controlled trials. Crit Care 20: 395
102. Li M, Zou H, Xu G, (2016) The prevention of statins against AKI and mortality following cardiac surgery: A meta-analysis. Int J Cardiol 222: 260-266
103. Lewicki M, Ng I, Schneider AG, (2015) HMG CoA reductase inhibitors (statins) for preventing acute kidney injury after surgical procedures requiring cardiac bypass. Cochrane Database Syst Rev: CD010480
104. Li L, Li G, Yu C, Li Y, (2013) The role of remote ischemic preconditioning on postoperative kidney injury in patients undergoing cardiac and vascular interventions: a meta-analysis. Journal of cardiothoracic surgery 8: 43
105. Yang Y, Lang XB, Zhang P, Lv R, Wang YF, Chen JH, (2014) Remote ischemic preconditioning for prevention of acute kidney injury: a meta-analysis of randomized controlled trials. Am J Kidney Dis 64: 574-583
106. Pei H, Wu Y, Wei Y, Yang Y, Teng S, Zhang H, (2014) Remote ischemic preconditioning reduces perioperative cardiac and renal events in patients undergoing elective coronary intervention: a meta-analysis of 11 randomized trials. PLoS One 9: e115500
107. Li B, Lang X, Cao L, Wang Y, Lu Y, Feng S, Yang Y, Chen J, Jiang H, (2017) Effect of remote ischemic preconditioning on postoperative acute kidney injury among patients undergoing cardiac and vascular interventions: a meta-analysis. Journal of nephrology 30: 19-33
108. Hu J, Liu S, Jia P, Xu X, Song N, Zhang T, Chen R, Ding X, (2016) Protection of remote ischemic preconditioning against acute kidney injury: a systematic review and meta-analysis. Crit Care 20: 111
109. Zhang Y, Zhang X, Chi D, Wang S, Wei H, Yu H, Li Q, Liu B, (2016) Remote Ischemic Preconditioning for Prevention of Acute Kidney Injury in Patients Undergoing On-Pump Cardiac Surgery: A Systematic Review and Meta-Analysis. Medicine 95: e3465
110. Zhou C, Jeon Y, Meybohm P, Zarbock A, Young PJ, Li L, Hausenloy DJ, (2016) Renoprotection by remote ischemic conditioning during elective coronary revascularization: A systematic review and meta-analysis of randomized controlled trials. Int J Cardiol 222: 295-302
111. Zhang L, Diao Y, Chen G, Tanaka A, Eastwood GM, Bellomo R, (2016) Remote ischemic conditioning for kidney protection: A meta-analysis. Journal of critical care 33: 224-232
112. Yi B, Chen X, Shi H, Lin T, Lin H, Xu Y, Rong J, (2016) Remote ischaemic preconditioning reduces acute kidney injury in adult patients undergoing cardiac surgery with cardiopulmonary bypass: a meta-analysis. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery
113. Sukkar L, Hong D, Wong MG, Badve SV, Rogers K, Perkovic V, Walsh M, Yu X, Hillis GS, Gallagher M, Jardine M, (2016) Effects of ischaemic conditioning on major clinical outcomes in people undergoing invasive procedures: systematic review and meta-analysis. Bmj 355: i5599

Prevention of Acute Kidney Injury and Protection of Renal Function in the Intensive Care Unit: Update 2017.
114. Zhou C, Bulluck H, Fang N, Li L, Hausenloy DJ, (2017) Age and Surgical Complexity impact on Renoprotection by Remote Ischemic Preconditioning during Adult Cardiac Surgery: A Meta analysis. Scientific reports 7: 215
115. Pierce B, Bole I, Patel V, Brown DL, (2017) Clinical Outcomes of Remote Ischemic Preconditioning Prior to Cardiac Surgery: A Meta-Analysis of Randomized Controlled Trials. Journal of the American Heart Association 6
116. Menting TP, Wever KE, Ozdemir-van Brunschot DM, Van der Vliet DJ, Rovers MM, Warle MC, (2017) Ischaemic preconditioning for the reduction of renal ischaemia reperfusion injury. Cochrane Database Syst Rev 3: Cd010777
117. Walsh M, Whitlock R, Garg AX, Legare JF, Duncan AE, Zimmerman R, Miller S, Fremes S, Kieser T, Karthikeyan G, Chan M, Ho A, Nasr V, Vincent J, Ali I, Lavi R, Sessler DI, Kramer R, Gardner J, Syed S, VanHelder T, Guyatt G, Rao-Melacini P, Thabane L, Devereaux PJ, Remote II, (2016) Effects of remote ischemic preconditioning in high-risk patients undergoing cardiac surgery (Remote IMPACT): a randomized controlled trial. CMAJ 188: 329-336
118. Kim TK, Min JJ, Cho YJ, Hausenloy DJ, Ahn H, Kim KH, Hwang HY, Hong DM, Jeon Y, (2017) Effects of delayed remote ischemic preconditioning on peri-operative myocardial injury in patients undergoing cardiac surgery - A randomized controlled trial. Int J Cardiol 227: 511-515
119. Zarbock A, Kellum JA, Van Aken H, Schmidt C, Kullmar M, Rosenberger P, Martens S, Gorlich D, Meersch M, (2017) Long-term Effects of Remote Ischemic Preconditioning on Kidney Function in High-risk Cardiac Surgery Patients: Follow-up Results from the RenalRIP Trial. Anesthesiology 126: 787-798




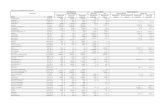

![SU PPLEMENTAR Y INFORMATION - Nature · General Information ... [6, 48] = 11.91 . p < 0.001 (S)-KET 1 mg/kg . vs (R)-KET 1 mg/kg. p > 0.05 (S)-KET 5 mg/kg . vs (R)-KET 5 mg/kg.](https://static.fdocuments.in/doc/165x107/5b38a1317f8b9abd438d7929/su-pplementar-y-information-nature-general-information-6-48-1191.jpg)





![Appendix F Examples · IT = the chemical intake (mg/kg-day) SF = the contaminant carcinogenic slope factor ([mg/kg-day]-1) Risk = 0.0107 mg/kg-day * 0.1 [mg/kg-day]-1 = 1.07 x 10-3](https://static.fdocuments.in/doc/165x107/600190ddec33f82cbe5ca5d7/appendix-f-examples-it-the-chemical-intake-mgkg-day-sf-the-contaminant-carcinogenic.jpg)





