STANISLAS LIMOUSIN, PHARMACAL · Cover picture STANISLAS LIMOUSIN, PHARMACAL INVENTOR (About 1886)...
Transcript of STANISLAS LIMOUSIN, PHARMACAL · Cover picture STANISLAS LIMOUSIN, PHARMACAL INVENTOR (About 1886)...


Cover picture
STANISLAS LIMOUSIN, PHARMACALINVENTOR (About 1886)
The French retail pharmacist, Stanislas Limousin,introduced many devices to Pharmacy and Medicine.His greatest contributions were invention of glassampoules; the medicine dropper; and apparatus forinhalation of oxygen.
One of a series: A History of Pharmacy in Pictures, presented by Parke, Davis& Company.George A. Bender, Director © 1957 Robert A. Thom, Artist
The Sri Lanka
PrescriberEditorsProfessor Gita Fernando MBBS, FRCP, FCCP
Professor Colvin Goonaratna MBBS, FRCP, FRCPE, FCCP, PhD, DSc
Professor Laal Jayakody MBBS, MRCP, PhD
Editorial BoardChinta Abayawardana Diploma in Pharmacy
Professor Anuja Abayadeera MBBS, FRCA, MD
Dr Nanda Amarasekara MBBS, MD, FRCP, FCCP, FRACP
Professor Kusum de Abrew MBBS, MD, FCCP, MRCP
Professor Shamya de Silva MBBS, DCH, MD
Professor Priyadarshani Galappatthy MBBS, MD, MRCP, DMT
Dr A M O Peiris BDS, FDSRCPS, FFDRCS
Professor Hemamali Perera MBBS, MRCPsych, MD
Dr Priyanga Ranasinghe MBBS
Professor Harshalal Seneviratne MBBS, FRCOG, DM
Dr Chamari Weeraratne MBBS, MD
Professor Anura Weerasinghe MBBS, MD, FRCP, DCH, DTM&H, PhD, FCCP
Copies of the Sri Lanka Prescriber and inquiries from M. P. Kuruppu,Deputy General Manager, Marketing, and Ms Anusha Gunatilleke,Manager Promotions and Publicity (Telephone 2338102), State Phar-maceuticals Corporation, P. O. Box 1757, 75, Sir Baron JayathilakeMawatha, Colombo 1.Price per copy Rs 50.00 (students Rs 25.00). Personal callers mayalso obtain copies from the Departments of Pharmacology atthe Medical Faculties in Colombo, Galle and Sri Jayewardenepura.
Published byDepartment of PharmacologyFaculty of Medicine271, Kynsey Road, Colombo 8, Sri Lanka.Telephone: + 94 11 2695300 Ext 315E-mail: [email protected] Pharmaceuticals Corporation75, Sir Baron Jayathilake Mawatha, Colombo 1.Telephones + 94 11 2320356-9Fax: + 94 11 447118E-mail: [email protected] Web site: www.spc.lk
Printed byAnanda Press82/5, Sir Ratnajothi Saravanamuttu Mawatha,Colombo 13.Telephone: + 94 11 2435975E-mail: [email protected]
(Secretary to Board and member)

1Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Management of acute bleeding in the uppergastrointestinal tract
IntroductionAcute upper gastrointestinal haemorrhage (bleedingproximal to the duodenojejunal flexure) is a commonmedical emergency (170 per 100 000 adults annually).Although its incidence may be declining, the mortalityrate of upper gastrointestinal haemorrhage remainshigh, approximately 6-8%.1 Depending on the site andrate of bleeding, a patient may present with melaena(black, tarry stool), haematemesis (vomiting ‘coffee-grounds’ or fresh blood), haematochezia (red bloodper rectum) or syncope. Melaena may also result frombleeding into the more distal small intestine or proximalcolon.
The majority of patients with upper gastrointestinalhaemorrhage require hospital management. Generalpractitioners have an important role in assessing andresuscitating patients and then managing themfollowing discharge to reduce the risk of recurrentbleeding.
SummaryAcute upper gastrointestinal haemorrhage is common.Patients require simultaneous resuscitation andclinical assessment followed by referral for endoscopy.There have been significant developments in termsof the acute endoscopic and medical treatment ofupper gastrointestinal haemorrhage, as well as thedevelopment of prognostic tools to help guidemanagement.
Preventing recurrent haemorrhage is also important.This requires an understanding of both the aetiologyand risk factors for recurrence, as well as the medicaland endoscopic treatments available to reduce theserisks
Key words: peptic ulcer, varices, endoscopy,haemorrhage
(Aust Prescr 2005; 28: 62-6)
Initial assessmentInitial clinical assessment is directed towards thehaemodynamic stability of the patient and therequirement for immediate resuscitation.
HistoryThe presenting symptom, past medical history andcurrent medications are important for establishing theaetiology (see box and Table 1) and severity ofhaemorrhage. A history of recent dyspepsia, or useof aspirin or another non-steroidal anti-inflammatorydrug (NSAID) may suggest a bleeding ulcer. Thepresence of chronic liver disease raises the possibilityof variceal haemorrhage. Haematemesis that followsprolonged vomiting or retching may be the result of aMallory-Weiss tear.
A history of syncope may reflect haemodynamicallysignificant bleeding. Vomiting frank blood suggestssevere haemorrhage from an arterial or varicealsource. In contrast, ‘coffee-grounds’ emesis isunlikely to reflect active bleeding.
Approximately 50 – 100 mL of blood is needed toproduce melaena. Haematochezia may occur withbrisk upper gastrointestinal haemorrhage and is usuallyaccompanied by haemodynamic compromise.
Common causes of upper gastrointestinalhaemorrhage
peptic ulcer disease
gastric erosions
oesophagitis
oesophageal or gastric varices
emetogenic injury (Mallory-Weiss tear)
malignancy
angiodysplasia

2 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
ExaminationIt is critical to assess the patient’s haemodynamicstatus by measuring heart rate, blood pressure andpostural changes. In haemodynamically compromisedpatients a fall in blood pressure may follow only aminor change in posture, for example from lying flatto sitting at a 45° incline. Variceal haemorrhage is morelikely if stigmata of chronic liver disease are present,particularly if there is evidence of portal hypertension,for example ascites and splenomegaly. An ulcer maycause epigastric tenderness. Digital rectal examinationis important to confirm the presence of true melaena.
InvestigationsHaemoglobin needs to be measured in all patientsbut may initially underestimate true blood loss, due todelayed haemodilution of the vascular space. Bloodshould be sent urgently to transfusion services forcross-matching. Other important tests include plateletcount, urea:creatinine ratio, coagulation indices andliver function tests including albumin. Patients with endstage liver disease may have normal liver enzymes,yet have impaired synthetic liver function as evidencedby low albumin, or reduced clotting factors.
Risk assessment scoresThe Blatchford score predicts the need for therapyand thus admission. Patients are unlikely to needtreatment and therefore may not require admission ifthey satisfy the following criteria:
• urea less than 6.5 mmol/L
• haemoglobin greater than 130 g/L (men) or 120 g/L(women)
• systolic blood pressure greater than 110 mmHg
• pulse less than 100 beats per minute (excludingthose with syncope).
This ‘fast-track’ triage could be used in an emergencydepartment to avoid unnecessary admissions.2
Likewise in regional areas, such a scoring systemcould help the general practitioner decide if a patientrequires immediate transfer to a tertiary referralcentre, or whether it is reasonable to discharge thepatient with a view to arranging an early outpatientendoscopy at the closest facility. The safety of usingthe management algorithm in this way is yet to beformally evaluated, and thus patients should continueto be managed on a case by case basis.
The Rockall score is frequently used for riskcategorisation (Table 2). The score is the sum of eachcomponent, calculated before and after endoscopy.This predicts rates of re-bleeding and mortality andcan be used in management algorithms, for examplewhether to admit a patient to an intensive care unit.Post-endoscopy risk scores of 2 or less are associatedwith a 4% risk of re-bleed and 0.1% mortality. In onestudy about 30% of patients had post-endoscopy riskscores of 2 or less and thus significant health savingscould be achieved by early endoscopy and discharge.3
Resuscitation
Until cross-matched blood is available, resuscitationproceeds with crystalloid or colloid solutions aimingfor a systolic blood pressure of greater than 100mmHg. Thiamine replacement should be consideredwhen there is a history of alcohol abuse.
Table 1. Drugs associated with gastrointestinal haemorrhage
Drugs Mechanism
Aspirin and non-steroidal Mucosal toxicityanti-inflammatory drugs,including COX-2 inhibitors
Prednisolone
Warfarin Impaired haemostasisClopidogrel and other antiplatelet drugsAspirinHeparin (both fractionated and unfractionated)Selective serotonin reuptake inhibitors

3Sri Lanka Prescriber, Vol. 23, No. 2, 2015
guide management and to facilitate the early dischargeof patients with a low risk of recurrent bleeding.
When high-risk lesions are seen (ulcers with activespurting vessel or non-bleeding visible vessel)endoscopic therapy significantly reduces re-bleedingrates and mortality.1 A dual-modality endoscopicapproach is currently recommended, with a com-bination of (1:10 000) adrenaline injection and thermalcoagulation. Band ligation and sclerotherapy are thetwo main endoscopic techniques for treating acuteoesophageal varices.5 These procedures are lesssuccessful in gastric varices, although injection withtissue adhesive may be effective.
The target haemoglobin concentration is contentious.Some advocate 70-80 g/L for otherwise healthyindividuals, without active bleeding, who arehaemodynamically stable.4 In patients older than 65or those with cardiovascular disease a targetconcentration of 90-100 g/L may be more appropriate.
Endoscopy – diagnosis and managementAfter resuscitation an endoscopy is arranged. Somepatients with profuse haemorrhage require emergencyendoscopy, however the majority can be scheduledon the next routine list. The endoscopy should, how-ever, take place within 24 hours of presentation, both to
Table 2. Rockall score for the prognostication of upper gastrointestinal bleeding3
Score
0 1 2 3
Pre-upper gastrointestinalendoscopy
Age <60 years 60-79 years 80 years
Shock No shock Tachycardia HypotensionBP >100 mmHg BP >100 mmHg BP < 100 mmHgand pulse <100 and pulse > 100
Comorbidity No major Ischaemic heart Renal or livercomorbidity disease, cardiac failure
failure, any major Disseminatedcomorbidity malignancy
Post-uppergastrointestinal endoscopy Diagnosis Mallory-Weiss or All other diagnose Gastrointestinal
no lesion found, malignancyand no majorstigmata of recenthaemorrhage
Major stigmata of recent None or dark Blood in upperhaemorrhage spot only gastrointestinal tract,
non-bleeding visiblevessel, spurting vesselor adherent clot
BP systolic blood pressurePatients with a score of 0, 1 or 2 have a lower risk of haemorrhage, whereas approximately 50% of patientswith a post-endoscopy score of 8 or more will re-bleed

4 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
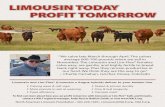
Figure 1. Management of acute upper gastrointestinal haemorrhage
Acute upper gastrointestinal bleedingResuscitation/transfer to hospital
Blatchford score low-risk forall parameters
Possible discharge withearly investigation
as an outpatient
YES
NO
Upper gastrointestinalendoscopy
Non-variceal
Rockall score
Variceal
Endoscopic haemostasisplus medical therapy
(octreotide/teripressin)
Early discharge.If ulcer, treat withusual dose PPI for
6 weeksStop NSAID & eradicate
H. pyloriStop smoking
If high-risk ulcer stigmatathen PPI infusion 72 hrs
usual dose PPI for6 weeks
Stop NSAID & eradicateH. pylori
Stop smoking
Reduce portal pressurewith medical therapy
(beta blocker +/- ISMN)with or without
endoscopic techniques(band ligation/sclerotherapy)
Re-bleeding may requirerepeat endoscopy +/-
surgical or radiologicalintervention
PPI proton pump inhibitorISMN ososorbide mononitrateNSAID non-steroidal anti-inflammatory
drug (including aspirin)
2 > 2

5Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Medical management of upper gastrointestinalbleeding (Fig. 1)Non-variceal
In gastrointestinal haemorrhage there is enhancedmucosal fibrinolytic activity, impairing haemostasis.6
Suppressing acid secretion blunts this escalation infibrinolysis. In this setting high-dose proton pump inhi-bitor therapy reduces the risk of recurrent bleeding.7
Proton pump inhibitor therapy can be administeredparenterally (either intermittently or by infusion) or orally.When high-risk features are present at endoscopy itmay be advisable to administer high dose intravenousproton pump inhibitor therapy, that is omeprazole 80mg (or equivalent) bolus followed by an infusion rateof 8 mg/hour for 72 hours. Where the cost of intra-venous proton pump therapy is prohibitive andespecially when there are no high-risk ulcer features,an oral proton pump inhibitor may be satisfactory.7
VaricealMedical therapy reduces variceal bleeding bylowering portal venous pressure. The available drugsinclude vasopressin and its synthetic analogueterlipressin, as well as somatostatin and its syntheticanalogues octreotide and vapreotide. The relativemerits of these drugs are unclear. The addition of anoctreotide infusion to endoscopic therapy improvesbleeding control and reduces transfusion require-ments5, therefore a combination of endoscopic andmedical treatment is probably the best approach.However, only terlipressin has been shown to reducemortality rates following variceal bleeding8, but it iscurrently only available in Australia under the SpecialAccess Scheme.*
* http://www.tga.gov.au/docs/html/sasinfo.htm [cited2005 May 10]
Prevention of recurrent bleedingNon-variceal
Prevention of recurrent bleeding in ulcer diseaseshould be directed towards the underlying cause. Allpatients should be asked about aspirin and otherNSAID use and be tested for Helicobacter pylori.Patients who smoke should be advised to stop.
NSAID-induced ulcers
NSAIDs should be discontinued where possible. Theulcer may then be healed with an H2-receptor
antagonist or a proton pump inhibitor over a period ofsix weeks.9 Current clinical practice favours protonpump inhibitor therapy over H2-receptor antagonistfor ulcer healing. No further endoscopy is requiredfor duodenal ulcers, but repeat endoscopy at eightweeks is advisable for gastric ulcers to ensure healingand exclude malignancy.
In patients requiring ongoing NSAID therapy, aconcomitant proton pump inhibitor achieves a greaterrate of ulcer healing than H2-receptor antagonists.10
An alternative approach is to substitute paracetamol ora COX-2 selective drug for the conventional NSAID.In terms of the rate of recurrent bleeding, this strategyis comparable to taking a conventional NSAID witha proton pump inhibitor.11 The rate of recurrenthaemorrhage in this group, however, is still relativelyhigh. It is important to remember that the gastro-intestinal advantages of COX-2 selective inhibitorsare negated by concomitant aspirin therapy, and thatthere has been recent concern about the cardio-vascular safety of this class of drug. A proton pumpinhibitor reduces the risk of recurrent bleeding whenlong-term aspirin therapy is required. The timing ofthe resumption of a medication which may havecontributed to the gastrointestinal haemorrhage shouldbalance the likelihood of re-bleeding, the indication forthe drug and whether safer alternatives are available.
H. pylori-associated ulcers
All patients with ulcer disease should be tested forH. pylori12 and the bacteria eradicated if found.Successful eradication, usually a seven day regimenof triple therapy, significantly reduces the risk of ulcerrecurrence.13 Once H. pylori eradication is confirmedand the ulcer has been healed by six weeks oftreatment with an H2-receptor antagonist or protonpump inhibitor, no further therapy is required.
Idiopathic ulcer
A number of patients have ulcers without a clearaetiology. These patients should have their ulcershealed with either an H2-receptor antagonist or aproton pump inhibitor for 6-8 weeks.9 However, theymay require long-term acid suppression.
Variceal
Variceal bleeding recurs in approximately two-thirdsof patients.5 Both endoscopic and medical strategiesare used in an attempt to reduce recurrent oeso-phageal variceal bleeding. Regular endoscopic

6 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
treatment, usually 3-4 sessions (initially weekly, thenevery 2-3 weeks), with either sclerotherapy orbanding can obliterate oesophageal varices. Bandligation is preferred because of greater efficacy anda lower incidence of oesophageal strictures. 5
Alternatively, reducing portal pressure with a non-selective beta blocker (propranolol, nadolol (notapproved in Australia) with or without a long-actingnitrate has proven effective. The combination ofnadolol and isosorbide mononitrate therapy wassuperior to band ligation alone in preventing recurrentvariceal bleeding.14 It is possible, however, thatcombination endoscopic and medical therapy (in thisstudy the medical treatment was nadolol andsucralfate) may be more effective than either alone.15
Some patients require specialist techniques such asporto-systemic shunting by surgery or by a trans-jugular intrahepatic porto-systemic shunt. Otherpatients may not be able to have optimal medicaltreatment because of contraindications or adverseeffects. In the case of alcoholic liver disease, failureto stop drinking increases the risk for recurrenthaemorrhage, so abstention from alcohol is critical.
ConclusionManagement of acute upper gastrointestinalhaemorrhage begins with clinical assessment andresuscitation. Endoscopy is required for diagnosis andinitial therapy. A combination of medical andendoscopic strategies are used to reduce the risk ofrecurrent bleeding.
References1. Barkun A, Bardou M, Marshall JK. Consensus
recommendations for managing patients withnonvariceal upper gastrointestinal bleeding. AnnIntern Med 2003;139:843-57.
2. Blatchford O, Murray WR, Blatchford M. A risk scoreto predict need for treatment for upper-gastrointestinalhaemorrhage. Lancet 2000;356:1318-21.
3. Rockall TA, Logan RF, Devlin HB, Northfield TC.Selection of patients for early discharge or outpatientcare after acute upper gastrointestinal haemorrhage.Lancet 1996;347:1138-40.
4. Ghosh S, Watts D, Kinnear M. Management ofgastrointestinal haemorrhage. Postgrad Med J2002;78:4-14.
5. Sharara AI, Rockey DC. Gastroesophageal varicealhemorrhage. N Engl J Med 2001;345:669-81.
6. Vreeburg EM, Levi M, Rauws EA, Deventer SJ, Snel P,Bartelsman JW, et al. Enhanced mucosal fibrinolyticactivity in gastroduodenal ulcer haemorrhage and thebeneficial effect of acid suppression. AlimentPharmacol Ther 2001;15:639-46.
7. Leontiadis GI, McIntyre L, Sharma VK, Howden CW.Proton pump inhibitor treatment for acute peptic ulcerbleeding. The Cochrane Database of SystematicReviews 2004,Issue 3. Art. No.: CD002094.pub2. DOI:10.1002/14651858.CD002094.pub2.
8. Ioannou GN, Doust J, Rockey DC. Systematic review:terlipressin in acute oesophageal varicealhaemorrhage. Aliment Pharmacol Ther 2003;17:53-64.
9. Yeomans ND. Management of peptic ulcer disease notrelated to Helicobacter. J Gastroenterol Hepatol2002;17:488-94.
10. Yeomans ND, Tulassay Z, Juhasz L, Racz I, HowardJM, van Rensburg CJ, et al. A comparison ofomeprazole with ranitidine for ulcers associatedwith nonsteroidal antiinflammatory drugs. AcidSuppression Trial: Ranitidine versus Omeprazole forNSAID-Associated Ulcer Treatment (ASTRONAUT)Study Group. N Engl J Med 1998;338:719-26.
11. Chan FK, Hung LC, Suen BY, Wu JC, Lee KC, LeungVK, et al. Celecoxib versus diclofenac and omeprazolein reducing the risk of recurrent ulcer bleeding inpatients with arthritis. N Engl J Med 2002;347:2104-10.
12. Lambert J, Badov D. Abnormal laboratory results.Testing for Helicobacter pylori. Aust Prescr 1997;20:96-8.
13. Ford A, Delaney B, Forman D, Moayyedi P. Eradicationtherapy for peptic ulcer disease in Helicobacter pyloripositive patients. The Cochrane Database of SystematicReviews 2003, Issue 4. Art. No.: CD003840.pub2. DOI:10.1002/14651858.CD003840.pub2.
14. Villanueva C, Minana J, Ortiz J, Gallego A, Soriano G,Torras X, et al. Endoscopic ligation compared withcombined treatment with nadolol and isosorbidemononitrate to prevent recurrent variceal bleeding. NEngl J Med 2001;345:647-55.
15. Lo GH, Lai KH, Cheng JS, Chen MH, Huang HC, HsuPI, et al. Endoscopic variceal ligation plus nadolol andsucralfate compared with ligation alone for theprevention of variceal rebleeding: a prospective,randomized trial. Hepatology 2000;32:461-5.
Daniel L. Worthley, Registrar, and Robert J. Fraser, Associate Professor and Director of Gastroenterology,Repatriation General Hospital, Daw Park, South Australia
Associate Professor Fraser has received unrestricted grants from AstraZeneca, Pfizer, Lederle, and Altana, and acts asa consultant to Pfizer. Dr Worthley has received travel grants from AstraZeneca.
This article is reproduced from the Australian Prescriber 2005; 36: 62-6 by prior arrangement, courtesy of Australian Prescriber.

7Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Management of gastro-oesophageal reflux disease
Gastro-oesophageal reflux disease (GORD) occursdue to chronic reflux of gastric contents into theoesophagus. It is one of the commonest conditionspresenting to primary care physicians and specialistsin the field of gastroenterology.
The diagnosis of GORD is primarily clinical in themajority of patients who present with the typicalsymptoms of heartburn and regurgitation. Uppergastrointestinal endoscopy (UGIE) is warranted inthe following circumstances:
• In the elderly• In those with alarm symptoms (i.e. anorexia,
weight loss, melaena, anaemia, dysphagia, andodynophagia)
• When complications (eg. strictures) aresuspected
• Follow up after proton pump inhibitor (PPI)therapy in those with severe erosive oesophagitisat initial endoscopy
• Persistent symptoms despite 4-8 weeks of PPItherapy
Endoscopic examination enables the differentiationof GORD into erosive oesophagitis (EO) or non-erosive reflux disease (NERD), based on the presenceor absence of mucosal erosions in the distaloesophagus. Cardiac investigation may be requiredwhen chest pain is the primary presentation. Thisreview focuses on the management of patients wherea diagnosis of GORD has been established. The mainobjectives of treatment in GORD include:
• symptomatic relief• healing and prevention of recurrent mucosal
lesions, ie. reflux oesophagitis• prevention of complications such as strictures,
bleeding and columnar metaplasia (ie. Barret'soesophagus)
The management strategy of GORD is determinedby the:
• frequency of symptoms• severity of symptoms• presence of erosive oesophagitis on UGIE
Symptomatic relief is the most important reason forpatients seeking medical attention and is achieved bya combination of lifestyle modification and drugtherapy
Lifestyle and dietary modificationThe following lifestyle modifications are recommendedas the first line of management in patients withGORD.
• Weight loss in those who are overweight or haverecently gained weight
• Elevation of the head of the bed where nocturnalor laryngeal symptoms (eg. cough, hoarseness,throat clearing) are predominant
• Avoidance of large meals and consumption ofsmall frequent meals
• Avoidance of the supine position soon aftermeals, and avoidance of meals two to three hoursbefore bedtime
• Avoidance of specific foods (oily food, caffeine,chocolate, spicy food, carbonated beverages, andpeppermint) that trigger GORD symptoms
• Avoidance of tight fitting garments that raiseintra-gastric pressure
• Promotion of salivation through oral lozenges orchewing gum to neutralise refluxed acid andenhance oesophageal acid clearance
• Avoidance of tobacco and alcohol, as both reducelower oesophageal sphincter (LOS) tone, andsmoking also diminishes salivation
• Abdominal breathing exercises to strengthen theanti-reflux barrier of the LOS
Drug therapyTwo strategies are described for the treatment ofpatients with GORD.• Step up – this involves an incremental increase
in the potency of therapy until symptomaticcontrol is achieved
• Step down – this begins with potent anti-secretoryagents and a gradual reduction in the potency oftherapy until breakthrough symptoms define thetreatment necessary for symptom control

8 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
The former, recommended for patients with mild andintermittent symptoms, minimizes the use of protonpump inhibitors (PPIs) and its associated costs andside-effects, whereas the latter provides rapid symp-tomatic relief to those with severe symptoms or EO.
AntacidsAntacids are limited to on-demand use forsymptomatic relief, especially when the symptomsare mild and infrequent ie. less than once a week.They usually contain a combination of magnesiumtrisilicate, aluminum hydroxide, or calcium carbonate.These neutralise gastric acidity and reduce the acidexposure of the oesophageal mucosa during episodesof reflux. They are taken after a meal and at bedtime,and provide relief from heartburn within 5 minutesbut have a short duration of effect of 30 to 60 minutes.
Surface agents and alginatesSucralfate is a surface agent that adheres to the mucosalsurface and induces healing and protects from pepticinjury. However, its short duration of action and limitedefficacy compared to PPIs limits its use mainly tothe management of GORD in pregnancy.
Sodium alginate is a polysaccharide derived fromseaweed that forms a viscous gum that floats withinthe stomach and reduces the postprandial acid pocketin the proximal stomach. Its role in the managementof GORD is not established.
Acid suppression therapyAcid suppressionis the cornerstone of medical therapyand includes the H2 receptor-antagonists (H2RAs)and proton pump inhibitors (PPIs). Symptomatic reliefis achieved in more than 75% of patients, especiallywith the latter.
Histamine 2 receptor antagonists (H2RAs)H2RAs decrease acid secretion by inhibiting hista-mine-2 receptors on gastric parietal cells. However,the development of tachyphylaxis within 2-6 weeksof initiation of H2RAs limits their use as maintenancetherapy. They also have limited efficacy in patientswith EO, especially when severe.
Proton pump inhibitorsPPIs are the most potent inhibitors of gastric acidsecretion by irreversibly binding to and inhibiting thehydrogen-potassium ATPase pump. PPIs are used inpatients,
• who fail twice daily H2RA therapy• with EO and/or frequent (two or more episodes
per week) symptoms• with severe symptoms that impair quality of life
PPIs are administered daily and are most effectivewhen taken 30 minutes before the first meal of theday, because the amount of H-K-ATPase present inthe parietal cell is greatest after a prolonged fast.PPIs at standard doses for 8 weeks relieve symptomsof GORD and heal oesophagitis in most patientswith EO. There are no major differences in efficacyamong PPIs, different dosages or dosing regimens.Limitations include a higher cost and potential side-effects such as interference with calcium homeo-stasis, aggravation of cardiac conduction defects andhip fractures in postmenopausal women.
Prokinetic medications and reflux inhibitorsProkinetic agents may be effective in patients withmild symptoms and are usually prescribed along withPPIs. The usual adult regimen is metoclopramide ordomperidone 10 mg/day. Long-term use of prokineticagents is discouraged since they have seriouscomplications.
Treatment of Helicobacter pylori infectionIt is unclear whether chronic acid suppression withPPIs increases the risk of atrophic gastritis in patientswith H. pylori. Hence, routine screening for H.pylori infection and empirical eradication of H. pyloriare not recommended in patients with GORD.However, for H. pylori diagnosed in the setting ofGORD, eradication has been associated with animprovement of symptoms in patients with antralgastritis.
Healing of oesophagitisThe healing of acute reflux oesophagitis usuallyrequires marked acid suppression for a long period,and is dependent on the severity of the initialoesophagitis. Most such patients will requiremaintenance PPI therapy at a dosage of 20 mg/day,while a smaller group will require at least 40 mg/day.
Refractory symptomsPatients who fail to respond to once daily PPI therapyare considered to have refractory GORD.Twice dailyPPI therapy should be used to improve symptom reliefin these patients.

9Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Management of recurrent symptoms andmaintenance therapyCessation of medication should be considered in allpatients with GORD whose symptoms resolve withacid suppression. Exceptions include those patientswith severe OE and Barrett’s oesophagus, who shouldremain on long-term maintenance acid suppressionwith a PPI.
Up to 60% of patients with NERD and most patientswith OE will relapse within 6 to 9 months when acidsuppression is discontinued. Patients with recurrentsymptoms should be managed with acid suppressivetherapy, with incremental dose adjustment to controlsymptoms if required.
When symptom recurrence occurs three or moremonths after discontinuing therapy repeated, 8-weekcourses of acid suppressive therapy is recommended.However, if symptoms recur within 3 months, an UGIEis done to rule out complications of GORD and long-term maintenance acid suppression (PPI) therapy atthe lowest effective dose is recommended. Althoughintermittent (on-demand) therapy is an alternative inthe management of recurrent GORD, continuoustherapy appears to provide better symptom control,quality of life, and higher endoscopic remission rates.
Prevention of complicationsAggressive medical therapy heals oesophageal ulcersand prevents recurrent bleeding. Barrett’s oesophagusshould be prevented owing to its malignant potential.Evidence suggests that it rarely develops de novo orprogresses after effective control of oesophagitis.This supports the use of aggressive acid suppressionin patients with severe oesophagitis. It appearsunlikely that PPIs or surgery cause regression ofestablished Barrett’s oesophagus.
Pregnancy and lactationThe initial management of GORD in pregnancyconsists of lifestyle and dietary modification. Inpatients with persistent symptoms, pharmacologictherapy should begin with antacids followed bysucralfate. In those who fail to respond, H2RAs andPPIs could be used.
While most antacids are safe during pregnancy andbreast-feeding those containing sodium bicarbonateand magnesium trisilicate should be avoided. WhereUGIE is indicated, it should be postponed to the secondtrimester or post-partum.
Indications for surgeryThe Nissen fundoplication, a 360° transabdominalfundoplication is the most widely practiced procedurefor GORD. It is increasingly done laparoscopically.Ambulatory pH studies and oesophageal manometryon or off therapy should be considered prior tosurgery.
Indications for fundoplication include:• patients with symptoms not completely controlled
by PPI therapy• patients with well-controlled GORD who desire
definitive, one-time treatment• presence of Barrett oesophagus• presence of extra-oesophageal manifestations of
GORD: ie. respiratory (eg. cough, wheezing,aspiration), ear, nose, and throat (eg. hoarseness,sore throat, otitis media) and dental (eg. enamelerosion)
• young patients• poor patient compliance with medications• postmenopausal women with osteoporosis• patients with cardiac conduction defects• costs of prolonged medical therapy
Further reading1. Philip OK, Lauren BG, Marcelo FV. Guidelines for the
diagnosis and management of gastroesophageal refluxdisease. American Journal of Gastroenterology 2013;108: 308.
2. Kahrilas PJ, Shaheen NJ, Vaezi MF. AmericanGastroenterological Association Institute technicalreview on the management of gastroesophageal refluxdisease. Gastroenterology 2008; 135: 1392.
3. Guideline: The role of endoscopy in the managementof GERD. Gastrointestinal Endoscopy 2007; 66: 219.
4. Kahrilas PJ, Nicholas JT, Shilpa G. Up To Date: Medicalmanagement of gastroesophageal reflux disease inadults. http://www.uptodate.com/contents/medical-management-of-gastroesophageal-reflux-disease-in-adults. (cited: April 2015)
Dr Sivasuriya Sivaganesh, MBBS (Colombo), MS (Colombo), MRCS (Eng), PhD, Senior Lecturer in Surgery,Faculty of Medicine, University of Colombo.
Email <[email protected]>.

10 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Some key points in the new National MedicinesRegulatory Authority (NMRA) Act
IntroductionThe Government of Sri Lanka published its NationalMedicinal Drug Policy (NMDP) in 2005. Since then,attempts that were made to get it through as an Actof Parliament ran into various difficulties, and theNMDP remained as yet another inactive governmentdocument. Attempts to operationalize it got a boostwhen the NMDP became an election slogan in thelast few years. In June 2014, the then Minister ofHealth, appointed a committee to draft a NationalMedicines Regulatory Authority (NMRA) Act. Thiscommittee used the existing draft of an Act developedby a previous committee and modified it toaccommodate the objectives of the NMDP as far aspossible. The implementation of the NMDP wasincluded in the “100 day programme” of the presentgovernment. The drafting committee had to workovertime to develop the NMRA Act in quick time.The proposed NMRA Act was presented to theCabinet in February, and was approved by Parliamentin March 2015. Salient points in the proposed NMRAAct are summarised in this article.
Throughout the Act the term medicine orpharmaceutical is used instead of the word ‘drug’.This Act proposes to regulate medicines, medicaldevices and borderline medicinal products. However,the acronym NMRA is usedfor short. Cosmetics withmedicinal claims are regulated under this Act asborderline products. Products which get classified aspure cosmetics which do not have any medicinalclaims, such as simple soaps and toothpastes, will notbe regulated under this Act. The government will haveto develop a new mechanism to regulate suchcosmetics.
Establishment of an independent “Authority”Under the repealed Cosmetics Devices and DrugsAct No. 27 of 1980 (CDD Act), the Drug RegulatoryAuthority (DRA) of Sri Lanka came under thepurview of the Department of Health Services andthe Director General of Health Services (DGHS)functioned as the “Drugs Authority”. With delegatedauthority, the Director, Medical Technology andSupplies (D, MT & S) functioned as the local DRA.
Under the proposed Act a National MedicinesRegulatory Authority (“Authority”) will be establishedoutside the Department of Health Services, butanswerable to the Minister of Health. This Authoritywill have 13 members, including a Chairman and thechief executive officer (CEO). The DGHS will be amember. Others include persons with training inpharmacology, pharmacy, medical specialists andother professionals. The Minister will make theappointments. It is expected that the responsibility ofall aspects of medicines regulation will be with theAuthority, and not on any single individual.
Some key objects of the Authority are as follows.(a) Ensure the availability of efficacious, safe
and good quality medicines, medical devicesand borderline products to the general publicat affordable prices
(b) Function as the central regulator of allmatters connected with regulation andlicensing of medicines, medical devices andborderline products
(c) Ensure that activities pertaining to objective(b) are carried out in a transparent, sus-tainable and equitable manner
(d) Encourage local manufacture of goodquality medicines with a view to assuringavailability of essential medicines ataffordable prices
(e) Promote safe and rational use of medicinesto health care professionals and toconsumers
(f) Regulate the availability of medicines,medical devices and borderline products
Divisions of the AuthorityThe Authority will have different divisions in it includingthe National Medicines Quality Assurance Laboratory(NMQAL), which will be one such division. Othersinclude the Medicines Regulatory Division, MedicalDevices Regulatory Division, Borderline ProductsRegulatory Division, Clinical Trials RegulatoryDivision (CTRD), Pharmacy Regulatory Division,Organization Development Division (dealing with

11Sri Lanka Prescriber, Vol. 23, No. 2, 2015
human resources, finance, administration and audit),Information Education Communication and ResearchDivision (IECRD) and Vigilance and InspectorateDivision. The Authority shall have its own fund.Provision is provided to address conflict of interestissues of the members of the Authority and thecommittees. It is expected that most of the workpertaining to implementation of the NMRA Act willhave to be done by qualified pharmacists. Theirrepresentation is provided in the appropriatecommittees.
The National Standing CommitteeA National Standing Committee (NSC) consistingof 21 members is appointed to supervise theimplementation of the NMDP and the NMRA Actby the Authority. The technical advisory committee(TAC) of the CCD Act is extinct, and some of thefunctions of the TAC will be vested with the NationalAdvisory Committee.
Aspects of regulationAreas of registration, import, local manufacture,wholesale sale, retail sale, storage, transport,advertising and promotion pertaining to medicines,medical devices and borderline products will beregulated through a process of registration, licensing,scheduling and listing.
Technical evaluation of the products will be done by3 committees (Medicines Evaluation Committee,MEC; Medical Devices Evaluation Committee, MDEC,and Borderline Products Evaluation Committee,BPEC) whose membership is specified in the Act.In addition to the specified members there will bepanels of experts to each committee and also theoption to co-opt members. Criteria to be consideredduring evaluation of the products are efficacy, safety,quality, need and cost. In addition, provision has alsobeen made to consider pharmacoeconomic aspectswhere appropriate. Registering of generic medicineswould be subjected to evaluation of bioequivalenceand biowaiver data.
With stringent criteria used during the registrationprocess it is expected that only products which meetquality standards will be registered. With theoperation of the “need clause” it is expected that theNMRA will be able to reduce the number of brandsin the market.
Where relevant, compliance with various international
guidelines is incorporated in the Act for differentaspects of regulation. These include the WHO GoodManufacturing Practices (GMP), Good PharmacyPractice, Good Distribution Practice, Good ReviewPractice guidelines etc.
All new applications will be granted registration initiallyfor a period of one year. The Authority may renewthe registration for a further period of 1 year or 5years. In the case of new chemical entities theregistration and renewal shall be granted for periodsof 1 year each, up to a period of 3 years.
National Medicines Quality AssuranceLaboratory (NMQAL)Under the CCD Act the NDQAL was not under theAuthority. In the NMRA Act the laboratory will be adivision of the Authority, and function as its laboratory.The main function of the NMQAL is to test the qualityof medicines, medical devices and borderline productssubmitted by the Authority, including articles submittedfor registration, those collected at ports of entry tothe country, complaint samples, post-marketingsurveillance samples and others. Provision for testingat different points during the life-cycle of a medicineis provided. It is expected that the resources and thecapacity of the laboratory will be increased enablingit to carry out these functions.
Clinical trialsProvision is made to establish a Clinical TrialsRegulatory Division (CTRD) under the Authority.Reference is made to the new Clinical Trials Act forregulation of clinical trials, which is already draftedas a separate Bill to be passed by Parliament in thenear future.
Pharmacies and prescribingThere is a separate division in the Authority to regulatepharmacies. Dispensing of drugs has to be done bythe pharmacist or by an apprentice pharmacist, underthe direct supervision of a pharmacist.
Prescriptions shall be written in the generic name ofthe medicine. If the prescriber wishes, he may, inaddition to the generic name write a particular brandname, for the medicine prescribed. Where the brandof the medicine in the prescription is not available inthe pharmacy, or is not affordable to the customer,the pharmacist may dispense any other genericmedicine with the consent of the customer. The

12 Sri Lanka Prescriber, Vol. 23, No. 2, 2015
pharmacist shall inform the range of products availablein the pharmacy of the generic medicine and theirprices, enabling the customer to buy the medicinesaccording to his choice.
PricingA Pricing Committee will be established in theAuthority. The Authority will decide on theintroductory price based on the submission by theapplicant and other relevant factors such as theprevailing market prices for similar products withinthe same therapeutic class, a pricing formula, theinternational reference prices and other factors. Pricerevisions, which were previously under the ConsumerAffairs Authority will also come now under theNMRA.
Local manufacturePromoting local manufacture is specifically mentionedin a separate section and clauses, to provide technicalassistance and other necessary assistance toprospective manufacturers. There is provision torestrict import of products which are manufacturedlocally.
Appeals committeeParties whose applications for registration have beenturned down can initially appeal to the Authority forreconsideration. After this step they could appeal toa 3-member Appeals Committee.
Miscellaneous areasClauses to regulate advertising and promotion ofproducts and giving samples is included. Provision ismade to import unregistered medicines in limitedquantities for personal use. Such medicines shouldnot be sold. As in most Acts, the NMRA also hassections on prohibitions, offences and punishments.
DefinitionsDefinitions for various terms such as medicines,medical devices and borderline products and other
terms used in this Act are provided. Ayurveda andHomeopathic products do not come under the purviewof the NMRA.
Comments and conclusions
This NMRA Authority will function outside theDepartment of Health Services. With appropriatefunding it will be able to establish itself and workindependently. According to the repealed CDD Actone person functioned as the Authority. In the NMRAa 13-member Authority will hold responsibility. Asthere is independence from the Department of HealthServices, it is hoped that decision making andoperation will be less bureaucratic. Up to now, in SriLanka the Authorities did not have provision to regulatethe initial price of medicines, medical devices andborderline products. With the provisions of the NMRAthe Authority will be able to have an influence on theprices of medicines. For effective implementation ofthe provisions of this Act, regulations have to bedrafted in several areas. The impact of the new Actwill be felt only after establishment of the NMRAand implementation of its activities effectively. It isour belief that people will be served better with thenew NMRA Act, with quality products being madeavailable in the market at affordable prices.
Further reading1. National Medicinal Drug Policy for Sri Lanka 2005,
Ministry of Healthcare and Nutrition “Suwasiripaya”Colombo 10.
2. National Medicines Regulatory Authority – A Bill,Parliament of the Democratic Socialist Republuc of SriLanka Bill No.335, (March 3, 2015).
3. Cosmetics Devices and Drugs Act No. 27 of 1980,Government of the Democratic Socialist Republic ofSri Lanka.
4. National Pharmaceutical Pricing Agency, India; TheGazette of India – Extraordinary Part II – Section 3 –Sub-Section (ii) Ministry of Chemicals and Fertilizers,Department of Chemicals and Petrochemicals, NewDelhi (January 6, 1995).
5. Alexandre Dolgui, Jean-Marie Proth. Pricing strategiesand models. Annual Reviews in Control 2010; 34:101-10.
Professor R. L. Jayakody, Professor of Pharmacology, Faculty of Medicine, University of Colombo,
Email <[email protected]>.
Professor P. Galappatthy, Professor in Pharmacology, Faculty of Medicine, University of Colombo

13Sri Lanka Prescriber, Vol. 23, No. 2, 2015
Self-assessment questionsSelect the best response in each question
Question 1
A 70-year old man who had a brief loss of consciousness at a bus halt was brought by ambulance to the ETUof a General Hospital. He was conscious but confused, and the only medical history he gave was that he hadtaken treatment for several years from a District Hospital for chronic abdominal pain. His BP was 105/72mmHg. The pulse was regular at 110 bpm and a 12-lead ECG was unremarkable. Initial biochemicalresults were.
Glucose 4.0 mmol/l (3.5 – 6.0 fasting)
Urea 22.0 mmo/l (2.5 – 6.5)
Na 122 mmol/l (135 – 145)
K 2.9 mmol/l (3.5 – 5.0)
Cl 85 mmol/l (95 – 105)
HCO3 42 mmol/l (22 – 30)
What is your interpretation of the initial biochemical data?
Question 2
A 62-year old woman stabilised on thyroxine 150 µg/day for hypothyroidism for 3 years, was seen at a routineclinic visit with the following biochemical results.
Hb 11.0g/dl (12.4 – 15.2)
WBC, DC, and platelets normal
TSH 21 mU/l (0.4 – 4.0)
Free T4 16 pmol/l (12.0 – 22)
She had no specific complaints. What is your interpretation of her thyroid status?
Question 3
A 69-year old woman taking hydrochlorothiazide 25 mg and losartan potassium 50 mg daily for hypertension isadmitted to the ETU, breathless at rest. Arterial blood gases on air and other biochemical results are as follows
pH 7.48 (7.35 – 7.45) Na 136 mmol/l (135 – 145)
Pa O2 8.2 kPa (10 – 13) K 3.3 mmol/l (3.5 – 5.0)
Pa CO2 5.3 kPa (4.5 – 6) Urea 4.6 mmol/l (2.5 – 6.7)
HCO3 32 mmol/l (22 – 30) Creatinine 84 µmol/l (60 – 120)
Base excess + 7.2 Glucose 8 mmol/l (3.5 – 6.0 fasting)
Oxgen saturation 93%
What is your interpretation of these data?

ISSN 1391-0736
Printed by Ananda Press, Colombo.
Answers to self-assessment questions
Question 1 This man has hyponatraemia and hypokalaemia. The high urea is consistent with dehydration(water deficiency), and the low chloride and high bicarbonate are compatible with metabolicalkalosis produced by copious vomiting. Full investigation showed later that he had a non-malignant pyloric stenosis, with episodic bouts of profuse vomiting.
Question 2 A high TSH with a normal free T4 in a hypothyroid patient on thyroxine treatment is indicativeof non-adherence to the regular daily replacement regimen. Commencing regular thyroxineagain will normalise free T4 level in a few weeks, but the raised TSH will take much longer toadjust to the normal free T4 level.
Question 3 This woman may have metabolic alkalosis consequent to hypokalaemia due to the diuretic, ora Type 1 respiratory failure (eg. pneumonia, pulmonary embolism).
Professor Colvin Goonaratna FRCP (Lond and Edin), FCCP, PhD, Hon DSc.Email: [email protected] I have no conflict of interest regarding these questions or answers.