St. Clair Hospital HouseCall_Vol V Issue 1
-
Upload
dymun-company -
Category
Documents
-
view
216 -
download
0
description
Transcript of St. Clair Hospital HouseCall_Vol V Issue 1

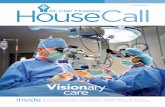
In Women’s Health CareOB-GYN surgeons Shannon H. McGranahan, M.D., and Stephanie S. Brown, M.D.
insideHeart Vest Saves Lives I Breast Care Center Offers 3D MammographyRenovations To First Floor Entrance And Lobby Complete I Ask The Doctor
HouseCall
VOLUME V ISSUE 1
Robotics Revolution

Volume V Issue 1 I HouseCall I 32 I HouseCall I Volume V Issue 1
PATIENT PROFILE
The women are among the first patients at
St. Clair Hospital to have gynecologic surgery
utilizing a breakthrough robotic technology
that is transforming the way that many
surgical procedures are performed.
The da Vinci Robotic Surgical System uses robotics and
computer technology to translate the real-time movements
of a surgeon’s hands into precise, micro-movements of
surgical instruments through tiny incisions. While the
da Vinci system uses robotics, it is not a robot. A robot
operates automatically, based on pre-set instructions.
With the da Vinci system, the surgeons are always in
control. The system cannot operate on its own. The
da Vinci represents a dramatic advance in surgical
science, making it possible for surgeons to perform
complex and delicate laparoscopic operations in the
safest and least invasive way possible. Robotic-assisted
surgery has numerous potential advantages for both the
surgeon and the patient, and is producing outstanding
clinical outcomes. At St. Clair, the system has been
in use since April 2011 for urologic surgery, and the
Hospital has gradually expanded its robotic-assisted
surgery program to include other surgical specialties,
including colorectal, general, thoracic and gynecologic.
Continued on page 4
Stephanie Brown, M.D. (left) and Shannon McGranahan, M.D. are using robotics technology in gynecologic procedures at St. Clair Hospital.
JUDITH GILLIAM, DEBRA CARSE AND AUDREY SMITH, ALL SOUTH HILLS RESIDENTS,
HAVE NEVER MET EACH OTHER, BUT THEY HAVE SEVERAL THINGS IN COMMON.
THEY ARE WOMEN WHO HAVE THE SHARED EXPERIENCE OF HAVING
UNDERGONE HYSTERECTOMY. THEY ARE ALSO MEDICAL PIONEERS.
ADVANCEDTECHNOLOGIES
Are Minimizing IncisionsAnd Speeding Recovery
For OB-GYN Surgery

Volume V Issue 1 I HouseCall I 32 I HouseCall I Volume V Issue 1
PAtient Profile
The women are among the first patients at
St. Clair Hospital to have gynecologic surgery
utilizing a breakthrough robotic technology
that is transforming the way that many
surgical procedures are performed.
The da Vinci Robotic Surgical System uses robotics and
computer technology to translate the real-time movements
of a surgeon’s hands into precise, micro-movements of
surgical instruments through tiny incisions. While the
da Vinci system uses robotics, it is not a robot. A robot
operates automatically, based on pre-set instructions.
With the da Vinci system, the surgeons are always in
control. The system cannot operate on its own. The
da Vinci represents a dramatic advance in surgical
science, making it possible for surgeons to perform
complex and delicate laparoscopic operations in the
safest and least invasive way possible. Robotic-assisted
surgery has numerous potential advantages for both the
surgeon and the patient, and is producing outstanding
clinical outcomes. At St. Clair, the system has been
in use since April 2011 for urologic surgery, and the
Hospital has gradually expanded its robotic-assisted
surgery program to include other surgical specialties,
including colorectal, general, thoracic and gynecologic.
Continued on page 4
Stephanie Brown, M.D. (left) and Shannon McGranahan, M.D. are using robotics technology in gynecologic procedures at St Clair Hospital.
Judith Gilliam, debra Carse and audrey smith, all south hills residents,
have never met eaCh other, but they have several thinGs in Common.
they are women who have the shared experienCe of havinG
underGone hystereCtomy. they are also mediCal pioneers.
ADVANCEDTECHNOLOGIES
Are Minimizing IncisionsAnd Speeding Recovery
For OB-GYN Surgery

the DoctorsThe application of da Vinci technology to gynecologic procedures
represents a clinical advancement that may dramatically change the
way that women experience hysterectomies and other surgeries. And,
according to the three St. Clair OB-GYNs — Stephanie Brown, M.D.,
Shannon McGranahan, M.D., and Sandor Mecs, M.D. — who perform
robotic-assisted gynecologic surgery, it can even be said that da Vinci
technology may revolutionize women’s health care.
Stephanie Brown, M.D., is an obstetrician-gynecologist who
performs robotic-assisted gynecologic surgery at St. Clair. She
describes the da Vinci system as a form of minimally invasive
surgery that improves upon conventional laparoscopy. The surgeon,
she explains, sits at a console that is in the operating room but
several feet away from the patient. Using hand and foot controls,
she manipulates a machine with four robotic arms that are positioned
over the patient. Three of the arms hold miniaturized surgical
instruments, such as a grasper or scissors, and one holds an
endoscopic camera. At the console, the surgeon looks through
lenses that give her a three-dimensional image and the capability
of magnification up to 10 times.
“The biggest advantage is that the da Vinci system enables the
surgeon to see so well,” Dr. Brown says. “You have extraordinary
visualization; you can zoom in and the three-dimensional camera
provides great depth perception. You can magnify and see the anatomy
so closely. The wristed instruments can get at angles in the pelvis that
you can’t otherwise achieve and the instruments move just like your
hands. It’s amazing.”
In addition to superior visualization, the da Vinci system provides
the surgeon with enhanced dexterity and increased precision.
Nevertheless, Dr. Brown acknowledges some initial skepticism.
“I was a skeptic at first. I didn’t like the idea of my hands not feeling
that tissue. As a surgeon, you feel it, respect it and know it. Especially
with tough cases, I felt that I had to be in there physically, feeling
the organs and arteries. With the robotic-assisted system, you are
not in direct physical contact with the patient, but what you gain in
visualization compensates.”
Dr. Brown says that some patients believe their surgery will be
performed by a robot. “When patients are first approached, some are
taken aback. I tell patients that I do the procedure with the assistance
of this instrument — it’s still laparoscopic surgery.”
Dr. Brown completed her comprehensive da Vinci training program
at an “epicenter” in Houston, Texas. An epicenter is a hospital where
there is a well-established da Vinci program with experienced surgeons
4 I HouseCall I Volume V Issue 1
Assistant
Video screen
Nurse
Surgeon uses open-surgeryhand movements, whichare precisely replicatedin the operative field bythe instruments
Surgeon at operative console
Anesthesiologist
Interchangeable instrumentswith EndoWrist™ technologysimultaneously followsurgeon’s hand andwrist movements
Volume V Issue 1 I HouseCall I 5
The surgeon uses hand controls on the da Vinci console tomanipulate the surgical instruments inside the patient.
“The biggest advantage is that the da Vinci system
enables the surgeon to see so well. … With the robotic-assisted system,
you are not in direct physicalcontact with the patient,
but what you gain in visualization compensates.
It’s amazing.”–Stephanie Brown, M.D.
An overhead view of the state-of-the-art da Vinci robotic surgical system.
the system provides surgeons with extraordinary visualization
and depth perception of the patient.
who offer their expertise to help other surgeons and surgical teams
master the technology. St. Clair has a special robotics surgical team,
which Dr. Brown calls “a well-oiled machine,” in a state-of-the-art
operating room that features wide-screen, high-definition monitors
and sophisticated equipment. Shannon McGranahan, M.D., Dr. Brown’s
partner in the OB-GYN group of Dr. Patricia Bulseco, M.D., PC, also
has completed da Vinci training at the Houston epicenter and the
two surgeons often operate together.
PAtient ProfileContinued from page 3
Continued on page 6

the DoctorsThe application of da Vinci technology to gynecologic procedures
represents a clinical advancement that may dramatically change the
way that women experience hysterectomies and other surgeries. And,
according to the three St. Clair OB-GYNs — Stephanie Brown, M.D.,
Shannon McGranahan, M.D., and Sandor Mecs, M.D. — who perform
robotic-assisted gynecologic surgery, it can even be said that da Vinci
technology may revolutionize women’s health care.
Stephanie Brown, M.D., is an obstetrician-gynecologist who
performs robotic-assisted gynecologic surgery at St. Clair. She
describes the da Vinci system as a form of minimally invasive
surgery that improves upon conventional laparoscopy. The surgeon,
she explains, sits at a console that is in the operating room but
several feet away from the patient. Using hand and foot controls,
she manipulates a machine with four robotic arms that are positioned
over the patient. Three of the arms hold miniaturized surgical
instruments, such as a grasper or scissors, and one holds an
endoscopic camera. At the console, the surgeon looks through
lenses that give her a three-dimensional image and the capability
of magnification up to 10 times.
“The biggest advantage is that the da Vinci system enables the
surgeon to see so well,” Dr. Brown says. “You have extraordinary
visualization; you can zoom in and the three-dimensional camera
provides great depth perception. You can magnify and see the anatomy
so closely. The wristed instruments can get at angles in the pelvis that
you can’t otherwise achieve and the instruments move just like your
hands. It’s amazing.”
In addition to superior visualization, the da Vinci system provides
the surgeon with enhanced dexterity and increased precision.
Nevertheless, Dr. Brown acknowledges some initial skepticism.
“I was a skeptic at first. I didn’t like the idea of my hands not feeling
that tissue. As a surgeon, you feel it, respect it and know it. Especially
with tough cases, I felt that I had to be in there physically, feeling
the organs and arteries. With the robotic-assisted system, you are
not in direct physical contact with the patient, but what you gain in
visualization compensates.”
Dr. Brown says that some patients believe their surgery will be
performed by a robot. “When patients are first approached, some are
taken aback. I tell patients that I do the procedure with the assistance
of this instrument — it’s still laparoscopic surgery.”
Dr. Brown completed her comprehensive da Vinci training program
at an “epicenter” in Houston, Texas. An epicenter is a hospital where
there is a well-established da Vinci program with experienced surgeons
4 I HouseCall I Volume V Issue 1
Assistant
Video screen
Nurse
Surgeon uses open-surgeryhand movements, whichare precisely replicatedin the operative field bythe instruments
Surgeon at operative console
Anesthesiologist
Interchangeable instrumentswith EndoWrist™ technologysimultaneously followsurgeon’s hand andwrist movements
Volume V Issue 1 I HouseCall I 5
The surgeon uses hand controls on the da Vinci console tomanipulate the surgical instruments inside the patient.
“The biggest advantage is that the da Vinci system
enables the surgeon to see so well. … With the robotic-assisted system,
you are not in direct physicalcontact with the patient,
but what you gain in visualization compensates.
It’s amazing.”–Stephanie Brown, M.D.
An overhead view of the state-of-the-art da Vinci robotic surgical system.
the system provides surgeons with extraordinary visualization
and depth perception of the patient.
who offer their expertise to help other surgeons and surgical teams
master the technology. St. Clair has a special robotics surgical team,
which Dr. Brown calls “a well-oiled machine,” in a state-of-the-art
operating room that features wide-screen, high-definition monitors
and sophisticated equipment. Shannon McGranahan, M.D., Dr. Brown’s
partner in the OB-GYN group of Dr. Patricia Bulseco, M.D., PC, also
has completed da Vinci training at the Houston epicenter and the
two surgeons often operate together.
PAtient ProfileContinued from page 3
Continued on page 6

the PAtientsFor Canonsburg resident Judy Gilliam, having
a hysterectomy was a matter of trust. The
68-year old retiree, wife and grandmother had
known for several years that she might eventually
need the operation, due to an ovarian cyst and
uterine fibroids. Gilliam wasn’t worried — she
knew that hysterectomy was a common surgical
procedure. Still, she was surprised when
Dr. Brown made a request: was she open to
undergoing robotic-assisted hysterectomy?
Indeed she was. Judy never hesitated.
“Dr. Brown is my doctor and I have all the faith
in the world in her. She’s a good doctor and the
nicest person. She said we could do it the ‘old
way’ if I wanted, but that I was a good candidate
for the robotic-assisted surgery because I had
no scar tissue. I felt that if Dr. Brown said this
was safe and effective, then that was that. She
explained it all and prepared me for it.” My
need for surgery wasn’t urgent, so I waited for
her to finish her training. When she was ready,
I was ready.”
Judy had a hysterectomy, followed by an
uneventful and nearly pain-free recovery.
“I was surprised by how good I felt,” she says.
“Nothing hurt! Dr. Brown took such good care
of me and made me feel special. She even
admitted me to the Family Birth Center after
the operation, so that she could watch me more
closely. There I was, among all the mothers
and babies. I went home the next day, and did
not take a single pain medication after I was
discharged. I had no bleeding and no other
problems at all. I was able to resume my
normal activities quickly.”
Continued on page 8
“I was surprIsed by
how good I felt.
NothINg hurt! … I was able
to resume my Normal
actIvItIes quIckly.
I weNt home the Next day,
aNd dId Not take a sINgle
paIN medIcatIoN after
I was dIscharged.
”JUDY GILLIAM
da Vinci surgical patient Judy Gilliam had an uneventfuland nearly pain-free recovery.
6 I HouseCall I Volume V Issue 1 Volume V Issue 1 I HouseCall I 7
PAtient ProfileContinued from page 5

the PAtientsFor Canonsburg resident Judy Gilliam, having
a hysterectomy was a matter of trust. The
68-year old retiree, wife and grandmother had
known for several years that she might eventually
need the operation, due to an ovarian cyst and
uterine fibroids. Gilliam wasn’t worried — she
knew that hysterectomy was a common surgical
procedure. Still, she was surprised when
Dr. Brown made a request: was she open to
undergoing robotic-assisted hysterectomy?
Indeed she was. Judy never hesitated.
“Dr. Brown is my doctor and I have all the faith
in the world in her. She’s a good doctor and the
nicest person. She said we could do it the ‘old
way’ if I wanted, but that I was a good candidate
for the robotic-assisted surgery because I had
no scar tissue. I felt that if Dr. Brown said this
was safe and effective, then that was that. She
explained it all and prepared me for it.” My
need for surgery wasn’t urgent, so I waited for
her to finish her training. When she was ready,
I was ready.”
Judy had a hysterectomy, followed by an
uneventful and nearly pain-free recovery.
“I was surprised by how good I felt,” she says.
“Nothing hurt! Dr. Brown took such good care
of me and made me feel special. She even
admitted me to the Family Birth Center after
the operation, so that she could watch me more
closely. There I was, among all the mothers
and babies. I went home the next day, and did
not take a single pain medication after I was
discharged. I had no bleeding and no other
problems at all. I was able to resume my
normal activities quickly.”
Continued on page 8
“I was surprIsed by
how good I felt.
NothINg hurt! … I was able
to resume my Normal
actIvItIes quIckly.
I weNt home the Next day,
aNd dId Not take a sINgle
paIN medIcatIoN after
I was dIscharged.
”JUDY GILLIAM
da Vinci surgical patient Judy Gilliam had an uneventfuland nearly pain-free recovery.
6 I HouseCall I Volume V Issue 1 Volume V Issue 1 I HouseCall I 7
PAtient ProfileContinued from page 5

Robotic-assisted surgery is associated with
a lower rate of complications and reduced
length of stay. Patients have less post operative
pain, and subsequently less need for narcotic
pain medication, and they experience far less
bleeding. They require minimal post-operative
nursing care. Instead of 6- to 12-inch abdominal
incisions and scarring, they have five tiny
incisions that are more like punctures. Without
large wounds, patients are less likely to develop
an infection. Robotic-assisted surgery means
a shorter hospital admission ― usually one
night as opposed to three or four following
open abdominal surgery ― and a faster,
easier recovery. For patients, that’s the real
miracle of robotic-assisted surgery.
For Audrey Smith, a mother of three and
management consultant who lives in Mount
Lebanon, the decision to have robotic-assisted
surgery was more complicated. Smith was
planning a business trip to China when
Dr. McGranahan, her OB-GYN, informed her that
she had large fibroid tumors that necessitated
a hysterectomy. “I was quite anxious,” Smith
recalls. “I had had previous abdominal surgeries
and I knew what was involved; I was laid up for
six weeks with those surgeries and had a lot of
pain. I had this trip to China scheduled for four
weeks after the surgery, which could not be
canceled. I was worried; would I be recovered
enough to go? Plus, I was dealing with a lot of
emotions about having a hysterectomy.”
Pioneering technology
The da Vinci Robotic Surgical Systemis the result of a convergence ofpowerful forces: the science of medicine,
the art of surgery and the technology of thecomputer era, with a bit of science fiction in the mix, too.
The story of this breakthrough surgicaldevice originates in the Italian Renaissance,in the innovative mind of Leonardo da Vinci.da Vinci was undeniably a genius: a painter,sculptor, musician, architect, engineer, inventor and mathematician. He created arguably the most finely detailed andanatomically accurate drawings of thehuman body ever produced. da Vinci alsoloved machines and mechanics. He loved to study and improve existing machines,and designed everything from harmonicasto military tanks. In 1495, he developed the world’s first robot, a medieval knight in armor that could sit, stand, walk andturn its head.
More than four centuries later, in 1942,another creative thinker, Robert Heinlein,wrote a science fiction novel called Waldo,about a man too physically weak to care forhimself. He gained some independence byusing a device that enabled him to manipulatea mechanical arm. Inspired by the book,inventors began designing remotemanipulators, called Waldoes, and by 1950,these early robots were a reality. They were
used primarily to mobilize hazardousmaterials in unsafe environments, muchlike the bomb-detecting robots that policeuse today.
In the 1980s, advances in electronicsand computer technology further propelledthe development of robotics. At the sametime, surgeons were developing minimallyinvasive surgery techniques and in 1987,French surgeon Phillippe Mouret performedthe first laparoscopic gall bladder removal.Following that, there was explosive growthin laparoscopic technology and methods for simple surgical procedures.
The prototype for the da Vinci roboticsurgical system was created in the late 80sin an effort to improve military surgicalcapabilities for the U.S. Army. The DefenseAdvanced Research Projects Agency(DARPA) funded research to test thefeasibility of a remote surgery program foruse in the front lines of battle. The idea wasto substitute robots for human medics andsurgeons, to keep them out of harm’s way.The robotic medic concept never flourished,but the DARPA research advanced thedevelopment of surgical robotics. Anotherinfluence was the NASA-funded work ofscientists at the Jet Propulsion Laboratoryin Pasadena, Calif.
Intuitive Surgical was founded in 1995in Sunnyvale, Calif. and secured licenses
on the robotic technologies. The goal was to take these innovative concepts and turnthem into a marketable medical device thatallowed surgeons to operate intuitively. In conventional laparoscopic surgery, thesurgeon moves the instrument handles inthe direction that is opposite the way sheor he actually wishes to go — an approachthat surgeons describe as counter-intuitive.Within four years, in 1999, the firstda Vinci system was introduced and clearedby the FDA for laparoscopic surgery.
Intuitive Surgical, which is now theglobal leader in robotic-assisted, minimallyinvasive surgical technology, chose to call therobotic surgical system the “da Vinci” inhonor of the artist who created the first robot.With his apparently limitless capabilitiesand creativity, da Vinci blended art andscience in a singular way. His legacy hasendured for centuries and he continues toinspire futuristic thinkers, including thosewho developed the robotic surgical systemthat is transforming many surgical specialties.
Art, Science and ScienceFiction Merge in theda Vinci Surgical System
Debra Carse, 47, of Upper St. Clair, is a
married mother of two and a registered nurse.
As a nurse, she was aware of robotic-assisted
surgery and knew that St. Clair Hospital was
using a da Vinci system. She also knew
Dr. McGranahan well, as a colleague and
as her gynecologist. When Dr. McGranahan
suggested that she have a robotic-assisted,
hysterectomy to treat abnormal uterine bleeding
that had persisted for two years, Debra had
no doubt that this was the right option for her.
“Dr. McGranahan was excited about
robotic-assisted surgery for gynecology,
and everything went exactly as she told me
it would. Dr. Brown assisted her, so I had
the benefit of having both of them there.
Post-op, I had some discomfort from bloating,
but my pain was so minimal that I only took
Motrin.” Debra has exceptional appreciation
for the dramatic contrast between recovery
from open abdominal surgery and
robotic-assisted laparoscopy.
“Without an abdominal incision,
you’re able to move easily —
to stand and sit, to get in and
out of bed, to shower and
even to breathe normally.
All you have are five little
‘poke holes,’ where the
instruments were inserted.
Because there is so much
less manipulation of the
internal organs, you
experience less pain
and swelling. The most
difficult aspect of this
surgery is that you feel
so good, you forget that you had
surgery. When I lifted things, I felt
a pulling sensation that was like a
reminder — ‘oh, yeah, I just had a
hysterectomy, better slow down.’”
“the most dIffIcult
aspect of thIs surgery
Is that you feel so
good, you forget that
you had surgery.
”DEBRA CARSE
Continued on page 10
Debra Carse
8 I HouseCall I Volume V Issue 1
PAtient ProfileContinued from page 7
Volume V Issue 1 I HouseCall I 9

Robotic-assisted surgery is associated with
a lower rate of complications and reduced
length of stay. Patients have less post operative
pain, and subsequently less need for narcotic
pain medication, and they experience far less
bleeding. They require minimal post-operative
nursing care. Instead of 6- to 12-inch abdominal
incisions and scarring, they have five tiny
incisions that are more like punctures. Without
large wounds, patients are less likely to develop
an infection. Robotic-assisted surgery means
a shorter hospital admission ― usually one
night as opposed to three or four following
open abdominal surgery ― and a faster,
easier recovery. For patients, that’s the real
miracle of robotic-assisted surgery.
For Audrey Smith, a mother of three and
management consultant who lives in Mount
Lebanon, the decision to have robotic-assisted
surgery was more complicated. Smith was
planning a business trip to China when
Dr. McGranahan, her OB-GYN, informed her that
she had large fibroid tumors that necessitated
a hysterectomy. “I was quite anxious,” Smith
recalls. “I had had previous abdominal surgeries
and I knew what was involved; I was laid up for
six weeks with those surgeries and had a lot of
pain. I had this trip to China scheduled for four
weeks after the surgery, which could not be
canceled. I was worried; would I be recovered
enough to go? Plus, I was dealing with a lot of
emotions about having a hysterectomy.”
Pioneering technology
The da Vinci Robotic Surgical Systemis the result of a convergence ofpowerful forces: the science of medicine,
the art of surgery and the technology of thecomputer era, with a bit of science fiction in the mix, too.
The story of this breakthrough surgicaldevice originates in the Italian Renaissance,in the innovative mind of Leonardo da Vinci.da Vinci was undeniably a genius: a painter,sculptor, musician, architect, engineer, inventor and mathematician. He created arguably the most finely detailed andanatomically accurate drawings of thehuman body ever produced. da Vinci alsoloved machines and mechanics. He loved to study and improve existing machines,and designed everything from harmonicasto military tanks. In 1495, he developed the world’s first robot, a medieval knight in armor that could sit, stand, walk andturn its head.
More than four centuries later, in 1942,another creative thinker, Robert Heinlein,wrote a science fiction novel called Waldo,about a man too physically weak to care forhimself. He gained some independence byusing a device that enabled him to manipulatea mechanical arm. Inspired by the book,inventors began designing remotemanipulators, called Waldoes, and by 1950,these early robots were a reality. They were
used primarily to mobilize hazardousmaterials in unsafe environments, muchlike the bomb-detecting robots that policeuse today.
In the 1980s, advances in electronicsand computer technology further propelledthe development of robotics. At the sametime, surgeons were developing minimallyinvasive surgery techniques and in 1987,French surgeon Phillippe Mouret performedthe first laparoscopic gall bladder removal.Following that, there was explosive growthin laparoscopic technology and methods for simple surgical procedures.
The prototype for the da Vinci roboticsurgical system was created in the late 80sin an effort to improve military surgicalcapabilities for the U.S. Army. The DefenseAdvanced Research Projects Agency(DARPA) funded research to test thefeasibility of a remote surgery program foruse in the front lines of battle. The idea wasto substitute robots for human medics andsurgeons, to keep them out of harm’s way.The robotic medic concept never flourished,but the DARPA research advanced thedevelopment of surgical robotics. Anotherinfluence was the NASA-funded work ofscientists at the Jet Propulsion Laboratoryin Pasadena, Calif.
Intuitive Surgical was founded in 1995in Sunnyvale, Calif. and secured licenses
on the robotic technologies. The goal was to take these innovative concepts and turnthem into a marketable medical device thatallowed surgeons to operate intuitively. In conventional laparoscopic surgery, thesurgeon moves the instrument handles inthe direction that is opposite the way sheor he actually wishes to go — an approachthat surgeons describe as counter-intuitive.Within four years, in 1999, the firstda Vinci system was introduced and clearedby the FDA for laparoscopic surgery.
Intuitive Surgical, which is now theglobal leader in robotic-assisted, minimallyinvasive surgical technology, chose to call therobotic surgical system the “da Vinci” inhonor of the artist who created the first robot.With his apparently limitless capabilitiesand creativity, da Vinci blended art andscience in a singular way. His legacy hasendured for centuries and he continues toinspire futuristic thinkers, including thosewho developed the robotic surgical systemthat is transforming many surgical specialties.
Art, Science and ScienceFiction Merge in theda Vinci Surgical System
Debra Carse, 47, of Upper St. Clair, is a
married mother of two and a registered nurse.
As a nurse, she was aware of robotic-assisted
surgery and knew that St. Clair Hospital was
using a da Vinci system. She also knew
Dr. McGranahan well, as a colleague and
as her gynecologist. When Dr. McGranahan
suggested that she have a robotic-assisted,
hysterectomy to treat abnormal uterine bleeding
that had persisted for two years, Debra had
no doubt that this was the right option for her.
“Dr. McGranahan was excited about
robotic-assisted surgery for gynecology,
and everything went exactly as she told me
it would. Dr. Brown assisted her, so I had
the benefit of having both of them there.
Post-op, I had some discomfort from bloating,
but my pain was so minimal that I only took
Motrin.” Debra has exceptional appreciation
for the dramatic contrast between recovery
from open abdominal surgery and
robotic-assisted laparoscopy.
“Without an abdominal incision,
you’re able to move easily —
to stand and sit, to get in and
out of bed, to shower and
even to breathe normally.
All you have are five little
‘poke holes,’ where the
instruments were inserted.
Because there is so much
less manipulation of the
internal organs, you
experience less pain
and swelling. The most
difficult aspect of this
surgery is that you feel
so good, you forget that you had
surgery. When I lifted things, I felt
a pulling sensation that was like a
reminder — ‘oh, yeah, I just had a
hysterectomy, better slow down.’”
“the most dIffIcult
aspect of thIs surgery
Is that you feel so
good, you forget that
you had surgery.
”DEBRA CARSE
Continued on page 10
Debra Carse
8 I HouseCall I Volume V Issue 1
PAtient ProfileContinued from page 7
Volume V Issue 1 I HouseCall I 9

Dr. McGranahan proposed having a robotic-
assisted hysterectomy, and Smith says that
her doctor’s confidence convinced her.
“Dr. McGranahan is fantastic. I went in feeling
so good about having this done, and it turned
out to be a great experience.” Smith echoes
Debra Carse and Judy Gilliam regarding her
recovery experience. “I was out of anesthesia
at 6 p.m. and up and walking at 8 p.m. That
first night I was sore, but able to get out of bed
by myself. I had the surgery on Thursday, went
home Friday and went to the movies on Sunday.
I was back at work one week later. My recovery
was so smooth.”
That smooth, rapid recovery is a bit of a
mixed blessing, says Dr. McGranahan. “Patients
rave about how quickly they rebound, but I have
learned to advise them to take it easy. Too much
activity can create complications; they can
strain or even separate the internal incisions.
Even though this approach has tremendous
advantages for patients, it is still surgery.
You have to rest and let your body heal.”
Audrey Smith went to China as planned,
and all has gone well. “I feel like I got myself
back, so fast. The physical healing helped my
emotional healing, and I’m glad that I did it.
Having this available to women is such a
positive development; I believe that when you
know you have this option, you’re more likely
to decide to have the surgery you need, rather
than delay it. It’s just awesome, especially
when compared to the conventional surgery.
It felt like a miracle to me.”
In the United States, 600,000 women
undergo hysterectomy every year, for a variety
of reasons: gynecologic cancer; endometriosis;
uterine fibroids; prolapsed uterus; and heavy
bleeding. There are four approaches to removing
the uterus: via a large open abdominal incision;
a vaginal incision; conventional laparoscopy;
or with robotics. Currently, 60 percent of
women who have hysterectomies have the
traditional open abdominal procedure, rather
than a minimally invasive one. The differences
are significant. Following the far more invasive
open abdominal procedure, recovery is
challenging and many women experience
significant pain, bleeding and fatigue. A woman
is unable to drive, shop, do housework, lift
things or return to work for six to eight weeks.
Still, some women need open abdominal
surgery because of the size of their organs or
medical complications such as obesity. Open
procedures, says Dr. McGranahan, do have the
advantage of giving a surgeon the entire range
of dexterity, but the da Vinci duplicates that.
“With the da Vinci, it’s like doing an open
procedure, in the sense that I have the same
wristed mobility, the same 3D visualization,
the same ability to make fine motor movements,”
she explains. “The da Vinci system is an extension
of the surgeon. It’s like doing an open procedure,
but through five very small incisions.”
A native of Upper St. Clair, Dr. Brown knew
since childhood that she wanted to become a
doctor and work at St. Clair Hospital. She
made her dream come true by graduating
from Denison University and then the University
of Louisville School of Medicine. She has two
children, ages 12 and 9, and enjoys the family-
friendly environment within the Patricia J.
Bulseco, M.D., PC, group. “With six doctors
in our group, we each get a day off during the
week, every week. I love OB GYN; I feel a special
connection with female patients, I love surgery,
and I love to deliver babies. Every time, it’s
the miracle of birth.”
Dr. McGranahan is a graduate of the
University of Pennsylvania who attended medical
school at Hahnemann University in Philadelphia
and completed her residency at West Penn
Hospital. She practiced there for seven years
before moving to her present position with the
Bulseco OB-GYN group four years ago. She is
married and the mother of two sons, ages 12
and 10, and lives in Sewickley. “I love what I do,”
“I had the surgery oN
thursday, weNt home
frIday aNd weNt to the
movIes oN suNday.
”AUDREY SMITH
she says. “I’m happy to wake up in the morning
and go to work.”
Dr. McGranahan envisions a future in
which robotic-assisted surgery becomes the
standard for hysterectomy, while abdominal
surgery becomes the exception. “We need to
endeavor to reverse those figures, so that
80 percent of women have minimally invasive,
robotic-assisted surgery. It should not be the
case in 2013 that the majority of women are
having the traditional open surgery. Our
mothers and grandmothers were having
hysterectomies done that way in their mid-40s,
mostly for heavy bleeding. Today we have
many other options for treating heavy bleeding,
so hysterectomy is not the automatic approach
to that. Still, women need hysterectomies for
other reasons, and as women become educated
about this, they will ask for this type of surgery.”
Dr. Brown agrees. “Robotic-assisted surgery
will eventually become the routine for GYN surgery.
Any case you’d normally do open, you should
consider doing robotically, unless the uterus is too
big. Robotic surgery allows for more dissection
than you’d be comfortable doing laparoscopically,
because you can see where the scars are.”
The implications for women’s health are
tremendous. The greatly reduced recovery
time and the quality of the recovery experience
mean that women get back to their normal
lives more quickly. This matters, not only on a
personal level for each woman, but even on a
broad social and economic level. Women are a
major presence in the workforce and their lives
are full. Judy Gilliam, Debra Carse and Audrey
Smith, as well as Drs. Brown and McGranahan,
are like most American women, juggling homes,
marriages, families, jobs, elder care and other
responsibilities. As Dr. McGranahan says,
“So much depends on women. Getting them
healthy and back to normal is a matter of
concern that extends beyond the individual
woman. The da Vinci technology is revolutionizing
women’s health care. And it should — women’s
health is critically important to families and
the community.” �
Benefits of Robotic-AssistedGynecologic Surgery
• 5 tiny poke holes versus a 6- to 12-inchincision with scarring
• Less pain and swelling
• 1-2 weeks versus 6 weeks to resumenormal activity post-op
• 1 night versus a 3-4 night hospital stay
• Less post-operative pain
• Less need for narcotic pain medications
• Reduced opportunity for infection
• Low rate of complications
Volume V Issue 1 I HouseCall I 11
STEPHANIE S. BROWN, M.D.
Dr. Brown specializes in obstetrics and gynecology. She earned hermedical degree at the University of Louisville School of Medicine andcompleted her residency at the Medical College of Ohio Hospital. Dr. Brown is board-certified by the American Board of Obstetrics andGynecology. She practices with the Patricia J. Bulseco, M.D., PC, group.
To contact Dr. Brown, please call 412.561.5666.
SHANNON H. McGRANAHAN, M.D.
Dr. McGranahan specializes in obstetrics and gynecology. She earnedher medical degree at Hahnemann University in Philadelphia andcompleted her residency at The Western Pennsylvania Hospital inBloomfield. Dr. McGranahan is board-certified by the AmericanBoard of Obstetrics and Gynecology. She practices with thePatricia J. Bulseco, M.D., PC, group.
To contact Dr. McGranahan, please call 412.561.5666.
“So much depends on women.Getting them healthy and back to normalis a matter of concern that extends beyond
the individual woman. Women’s healthis critically important to families
and the entire community.”–Shannon McGranahan, M.D.
PAtient ProfileContinued from page 8
10 I HouseCall I Volume V Issue 1

Dr. McGranahan proposed having a robotic-
assisted hysterectomy, and Smith says that
her doctor’s confidence convinced her.
“Dr. McGranahan is fantastic. I went in feeling
so good about having this done, and it turned
out to be a great experience.” Smith echoes
Debra Carse and Judy Gilliam regarding her
recovery experience. “I was out of anesthesia
at 6 p.m. and up and walking at 8 p.m. That
first night I was sore, but able to get out of bed
by myself. I had the surgery on Thursday, went
home Friday and went to the movies on Sunday.
I was back at work one week later. My recovery
was so smooth.”
That smooth, rapid recovery is a bit of a
mixed blessing, says Dr. McGranahan. “Patients
rave about how quickly they rebound, but I have
learned to advise them to take it easy. Too much
activity can create complications; they can
strain or even separate the internal incisions.
Even though this approach has tremendous
advantages for patients, it is still surgery.
You have to rest and let your body heal.”
Audrey Smith went to China as planned,
and all has gone well. “I feel like I got myself
back, so fast. The physical healing helped my
emotional healing, and I’m glad that I did it.
Having this available to women is such a
positive development; I believe that when you
know you have this option, you’re more likely
to decide to have the surgery you need, rather
than delay it. It’s just awesome, especially
when compared to the conventional surgery.
It felt like a miracle to me.”
In the United States, 600,000 women
undergo hysterectomy every year, for a variety
of reasons: gynecologic cancer; endometriosis;
uterine fibroids; prolapsed uterus; and heavy
bleeding. There are four approaches to removing
the uterus: via a large open abdominal incision;
a vaginal incision; conventional laparoscopy;
or with robotics. Currently, 60 percent of
women who have hysterectomies have the
traditional open abdominal procedure, rather
than a minimally invasive one. The differences
are significant. Following the far more invasive
open abdominal procedure, recovery is
challenging and many women experience
significant pain, bleeding and fatigue. A woman
is unable to drive, shop, do housework, lift
things or return to work for six to eight weeks.
Still, some women need open abdominal
surgery because of the size of their organs or
medical complications such as obesity. Open
procedures, says Dr. McGranahan, do have the
advantage of giving a surgeon the entire range
of dexterity, but the da Vinci duplicates that.
“With the da Vinci, it’s like doing an open
procedure, in the sense that I have the same
wristed mobility, the same 3D visualization,
the same ability to make fine motor movements,”
she explains. “The da Vinci system is an extension
of the surgeon. It’s like doing an open procedure,
but through five very small incisions.”
A native of Upper St. Clair, Dr. Brown knew
since childhood that she wanted to become a
doctor and work at St. Clair Hospital. She
made her dream come true by graduating
from Denison University and then the University
of Louisville School of Medicine. She has two
children, ages 12 and 9, and enjoys the family-
friendly environment within the Patricia J.
Bulseco, M.D., PC, group. “With six doctors
in our group, we each get a day off during the
week, every week. I love OB GYN; I feel a special
connection with female patients, I love surgery,
and I love to deliver babies. Every time, it’s
the miracle of birth.”
Dr. McGranahan is a graduate of the
University of Pennsylvania who attended medical
school at Hahnemann University in Philadelphia
and completed her residency at West Penn
Hospital. She practiced there for seven years
before moving to her present position with the
Bulseco OB-GYN group four years ago. She is
married and the mother of two sons, ages 12
and 10, and lives in Sewickley. “I love what I do,”
“I had the surgery oN
thursday, weNt home
frIday aNd weNt to the
movIes oN suNday.
”AUDREY SMITH
she says. “I’m happy to wake up in the morning
and go to work.”
Dr. McGranahan envisions a future in
which robotic-assisted surgery becomes the
standard for hysterectomy, while abdominal
surgery becomes the exception. “We need to
endeavor to reverse those figures, so that
80 percent of women have minimally invasive,
robotic-assisted surgery. It should not be the
case in 2013 that the majority of women are
having the traditional open surgery. Our
mothers and grandmothers were having
hysterectomies done that way in their mid-40s,
mostly for heavy bleeding. Today we have
many other options for treating heavy bleeding,
so hysterectomy is not the automatic approach
to that. Still, women need hysterectomies for
other reasons, and as women become educated
about this, they will ask for this type of surgery.”
Dr. Brown agrees. “Robotic-assisted surgery
will eventually become the routine for GYN surgery.
Any case you’d normally do open, you should
consider doing robotically, unless the uterus is too
big. Robotic surgery allows for more dissection
than you’d be comfortable doing laparoscopically,
because you can see where the scars are.”
The implications for women’s health are
tremendous. The greatly reduced recovery
time and the quality of the recovery experience
mean that women get back to their normal
lives more quickly. This matters, not only on a
personal level for each woman, but even on a
broad social and economic level. Women are a
major presence in the workforce and their lives
are full. Judy Gilliam, Debra Carse and Audrey
Smith, as well as Drs. Brown and McGranahan,
are like most American women, juggling homes,
marriages, families, jobs, elder care and other
responsibilities. As Dr. McGranahan says,
“So much depends on women. Getting them
healthy and back to normal is a matter of
concern that extends beyond the individual
woman. The da Vinci technology is revolutionizing
women’s health care. And it should — women’s
health is critically important to families and
the community.” �
Benefits of Robotic-AssistedGynecologic Surgery
• 5 tiny poke holes versus a 6- to 12-inchincision with scarring
• Less pain and swelling
• 1-2 weeks versus 6 weeks to resumenormal activity post-op
• 1 night versus a 3-4 night hospital stay
• Less post-operative pain
• Less need for narcotic pain medications
• Reduced opportunity for infection
• Low rate of complications
Volume V Issue 1 I HouseCall I 11
STEPHANIE S. BROWN, M.D.
Dr. Brown specializes in obstetrics and gynecology. She earned hermedical degree at the University of Louisville School of Medicine andcompleted her residency at the Medical College of Ohio Hospital. Dr. Brown is board-certified by the American Board of Obstetrics andGynecology. She practices with the Patricia J. Bulseco, M.D., PC, group.
To contact Dr. Brown, please call 412.561.5666.
SHANNON H. McGRANAHAN, M.D.
Dr. McGranahan specializes in obstetrics and gynecology. She earnedher medical degree at Hahnemann University in Philadelphia andcompleted her residency at The Western Pennsylvania Hospital inBloomfield. Dr. McGranahan is board-certified by the AmericanBoard of Obstetrics and Gynecology. She practices with thePatricia J. Bulseco, M.D., PC, group.
To contact Dr. McGranahan, please call 412.561.5666.
“So much depends on women.Getting them healthy and back to normalis a matter of concern that extends beyond
the individual woman. Women’s healthis critically important to families
and the entire community.”–Shannon McGranahan, M.D.
PAtient ProfileContinued from page 8
10 I HouseCall I Volume V Issue 1

Life SaverPortable LifeVest can help save lives
T hanks to a “vest,” two St. Clair Hospital patients who
were about to experience life-threatening heart attacks
were able to spend the recent holidays with their families.
But this was more than just an ordinary vest; it was the
LifeVest — the first wearable defibrillator manufactured by
Zoll Medical Corporation in Pittsburgh. Unlike a cardioverter
defibrillator, the LifeVest is worn outside the body rather than
implanted in the chest. It requires no bystander intervention.
Pittsburgh patient, Andrew Tichon, 61, was prescribed
the LifeVest following a diagnosis of ischemic and dilated
cardiomyopathy. After Andrew had been wearing the LifeVest
for about six months, he went to St. Clair Hospital to have open
heart surgery. Following his surgery, he continued to wear the
LifeVest during his recovery at an area rehabilitation facility.
Following rehabilitation, Andrew's heart began to beat out of
rhythm while he was at home. His LifeVest detected the life-
threatening arrhythmia and delivered a treatment shock.
His electrophysiologist, Puvalai M. Vijaykumar, M.D. said
had Andrew not been wearing the LifeVest, he probably would
not have survived that day.
Bridgeville resident Frank Ptaszynski, 59, another patient
of Dr. Vijaykumar, was also prescribed the LifeVest following
balloon angioplasty and stent insertion. While visiting St. Clair
Hospital for another unrelated medical condition, Frank passed
out after his heart lost its life-sustaining rhythm. As with Andrew,
the LifeVest delivered a treatment shock and helped Frank regain
consciousness. Moments later, his heart was restored to a
normal rhythm.
In both of these cases, the LifeVest came to the rescue. Once
fitted, the LifeVest continuously monitors a patient’s heart and, if
a life-threatening heart rhythm is detected, the device delivers a
treatment shock to restore normal heart rhythm. The device alerts
the patient prior to delivering a treatment shock by sounding an
alarm and releasing a conductive gel over the patient's chest.
According to Dr. Vijaykumar, the LifeVest is used for a wide
range of patient conditions, including following a heart attack,
before or after bypass surgery or stent placement, as well as
cardiomyopathy or congestive heart failure.
“We recommend the LifeVest to a patient who is at risk for
sudden cardiac arrest or who recently had a heart attack,” he
says. “Typically, we wait for 40 days following a myocardial infarction
(heart attack) before we can place an implantable cardioverter
defibrillator. Some patients may need to wait for 90 days. These
are people who have a dilated cardiomyopathy, patients who had
a recent balloon angioplasty or a stent placed, and people who had
coronary artery bypass surgery. During this waiting period, the
patient has to be protected from sudden cardiac arrest — and
the LifeVest protects them.”
Comfortable,lightweightgarment iswashableand can beworn all day,except whenbathing andshowering.
Dry, non-adhesivesensing electrodescontinuously monitorpatient’s heart.
This monitor is worn in a holsteraround the waist and from thesensing electrodes collects ECGdata that can be sent to a doctorvia modem.
If a life-threatening arrhythmia is detected,this alarm module alerts the patient with audible, visual and tactile alarms. A consciouspatient can prevent a shock by simultaneouslypressing two response buttons.
In the event of a life-threateningarrhythmia, these dry therapeuticelectrodes will automaticallydeploy conductive gel prior todelivering a shock.
Life-saving technoLogy
12 I HouseCall I Volume V Issue 1

Electrophysiology
The LifeVest also allows physicians like
Dr. Vijaykumar time to assess patients' long-term
arrhythmic risk and make appropriate plans. Once
a patient gets shocked from a LifeVest, the patient
immediately receives an implanted defibrillator.
That waiting period goes away — they do not have
to wait for 40 or 90 days.
Since the LifeVest is lightweight and easy to
wear, Dr. Vijaykumar says it allows patients to
return to their normal activities of daily living, while having the peace of mind
that they are protected from sudden cardiac arrest. “It’s like any vest you may
wear with adjustable straps,” says Dr. Vijaykumar.
The LifeVest is non-invasive and consists of two main components ―
a garment and a monitor. The garment, worn under the clothing, detects
arrhythmias and delivers treatment shocks. The monitor is worn around
the waist or from a shoulder strap and continuously monitors the patient’s heart.
To date, the LifeVest has been prescribed to more than 75,000
patients nationwide. �
As an electrophysiologist, Puvalai Vijaykumar, M.D. can help
determine whether a patient is at high risk for sudden cardiac
arrest or cardiovascular disease. According to the Heart Rhythm
Foundation, electrophysiology, a subspecialty of cardiology,
is now the fastest growing of all the cardiovascular disciplines.
Electrophysiologists, like Dr. Vijaykumar, are cardiologists
who have additional training in the diagnosis and treatment of
abnormal heart rhythms. Dr. Vijaykumar and his staff evaluate
and treat patients who have a variety of cardiac arrhythmias
and abnormal heart rhythms.
Your heart sends out electrical signals throughout the
muscle, thereby acting as a natural pacemaker. These signals
will cause each of your heart’s four chambers to relax and
contract in a rhythmic pattern. If your heart could not send out
a signal, it would be a motionless pump.
“People can have a slow heart beat or a rapid heart beat,”
notes Dr. Vijaykumar. "As electrophysiologists, we evaluate their
abnormal heart rhythm and prescribe the appropriate treatment.
In some cases, we may need to insert a pacemaker or an
implantable cardioverter defibrillator; and in other cases, they
may need a procedure called a radio-frequency ablation.”
Dr. Vijaykumar and his staff routinely handle heart rhythm
problems in patients of all ages. They often work closely with
other cardiologists and specialists to achieve the best outcomes
for these complex cases. �
THE FASTEST GROWING CARDIOVASCULAR DISCIPLINE
PUVALAI M. VIJAYKUMAR, M.D.
Dr. Vijaykumar specializes in electrophysiology and cardiology at St. Clair Hospital. He earned his medical degree at Stanley Medical College andcompleted his medical training at Madras MedicalCollege, both in India. He completed an internship atCabrini Medical Center in Manhattan, and fellowshipsat Coney Island Hospital in Brooklyn and DeborahHeart and Lung Center in Browns Mills, New Jersey. Dr. Vijaykumar is board-certified in cardiology andelectrophysiology. He practices with PittsburghCardiac Electrophysiology Associates, P.C.
To contact Dr. Vijaykumar, please call 412.687.8838.
on average,
Lifevest is
saving one
life a day.
David DeCarlucci, MS, CES, Supervisor, Cardiac/Pulmonary Rehabilitation at St. Clair Hospital, demonstrates the LifeVest while exercising.
Volume V Issue 1 I HouseCall I 13

asK the DoctoR
BrIDGET K. BEIEr, D.O.
Ask the Doctor Q
A
Is there a relationship between diabetes and heart disease?
There is strong link between diabetes and heart
disease. People with both Type I and Type II diabetes
are at increased risk of developing and dying from
heart disease. If you have diabetes, you are twice as
likely as someone without diabetes to suffer a heart
attack or stroke. According to the National Institutes of
Health, about 65 percent of people with diabetes die
of a heart attack or stroke. Even at the time of diabetes
diagnosis, many diabetics already have overt heart
disease (past heart attack, peripheral vascular disease,
or EKG changes). Many patients with diabetes have
multiple risk factors for heart disease, including high
blood pressure, cholesterol abnormalities, and obesity.
The pathogenesis of heart disease in diabetics is
complex. In simple terms, high blood sugar levels over
time can lead to the buildup of fatty materials on the
insides of blood vessel walls. This in turn can cause
abnormal blood flow, leading
to increased chance of
clogging and hardening
of blood vessels.
Chronic inflammation
may also play
a role.
The good news is, there are many ways for diabetics
to reduce their risk of heart disease. Good blood sugar
control is important. The goal HgA1c (this test provides
an average of your blood sugars over the preceding
2- to 3-month period) for most patients with diabetes
is less than 7 percent. Aggressive control of high blood
pressure and high cholesterol are also vitally important.
A goal blood pressure for most people with diabetes
is less than 130/80. In regards to cholesterol, the LDL
(“bad cholesterol”) should be less than 100 in diabetics
without known heart disease. The target LDL in diabetics
who have already been diagnosed with heart disease
is less than 70. Fortunately, there are safe and effective
medications available to help people meet their blood
pressure and cholesterol targets.
Smoking cessation lowers cardiovascular risk
substantially. Additionally, a low dose daily aspirin may
be beneficial in diabetics at high risk for heart disease,
but is no longer recommended for low risk individuals.
Finally, lifestyle modifications can greatly reduce
the risk of heart disease in diabetics. Diet, exercise and
weight loss can make a big impact. Try to get at least
30 to 60 minutes of exercise most days of the week
and follow a diet that is low in saturated fats and salt. �
BRIDGET K. BEIER, D.O.
Dr. Beier specializes in endocrinology. She earned her medical degree atLake Erie College of Osteopathic Medicine and completed her residency at the University of Connecticut Health Care Center and a fellowship atVirginia Commonwealth University Health System. She is board-certified in internal medicine and endocrinology. She practices with Associates in Endocrinology, P.C.
To contact Dr. Beier, please call 412.942.2140.
14 I HouseCall I Volume V Issue 1

Volume V Issue 1 I HouseCall I 15
Advanced Technologies at St. Clair Hospital’sNew Breast Care Center Enhance Mammography Screening
St. Clair Hospital’s new Breast Care Centerin Bethel Park is quickly gaining a stellarreputation among patients for a spa-like
ambience that offers them an environmentexuding comfort, convenience and beauty.
But patients are also praising the center’s advanced diagnostic imaging technology, particularly a new technology called 3D breast tomosynthesis. A recent study involving 3D breasttomosynthesis found a significant increase in cancerdetection rates, particularly for invasive cancers,and a simultaneous decrease in false-positive rateswith use of mammography, plus 3D tomosynthesis,when compared with mammography alone.
At the St. Clair Hospital Breast Care Center,3D breast tomosynthesis, which is FDA-approved,is often used in conjunction with traditional digital mammography as part of a woman’s annual screening mammogram to capture more breast images.
WHAT IS 3D BREAST TOMOSYNTHESIS?3D breast tomosynthesis uses high-powered computing to convert digital
breast images into a stack of very thin layers or “slices” ― building what is essentially a “3-dimensional mammogram.”
The 3D images allow doctors to examine breast tissue one layer at a time. Very low X-ray energy is used during the screening examination ― which takesabout 10 seconds to acquire ― so a patient’s radiation exposure is safely below the American College of Radiology (ACR) guidelines.
With 3D images, St. Clair Hospital diagnostic radiologists can see tissue detail in a way never before possible. Instead of viewing all of the complexities of a woman’s breast tissue in a flat 2D image, a radiologist can examine the tissue a millimeter at a time. Fine details are more clearly visible, no longer hidden by the tissue above and below.
When used together, 3D breast tomosynthesis and digital mammographyhave been proven to reduce “call-backs,” scenarios in which patients areasked to return for follow-up examinations to rule out any suspicious areas.The use of 3D tomosynthesis has proven particularly beneficial in womenwith dense breast tissue and has reduced the number of unnecessary invasivediagnostic procedures. �
The St. Clair Hospital Breast Care Center is on the Third Floor of the St. Clair HospitalOutpatient Center–Village Square, 2000 Oxford Drive, Bethel Park. To contact the center,please call 412.942.3177.
Diagnostic aDvances
“3D tomosynthesis has proven
particularly beneficial in women
with Dense breast tissue
anD has reDuceD the number
of unnecessary invasive
Diagnostic proceDures.
”

General & Patient Information Physician Referral Service Outpatient Center–Village Square Medical Imaging Scheduling 412.942.4000 412.942.6560 412.942.7100 412.942.8150
St.Clair Hospital1000 Bower Hill RoadPittsburgh, PA 15243www.stclair.org
is a publication of St. Clair Hospital. Articles are for informational purposes and arenot intended to serve as medical advice. Please consult your personal physician.
Follow us on twitter at: www.twitter.com/stclairhospitalHouseCall
In November, St. Clair Hospital formally
dedicated its newly renovated First Floor
Lobby and entryway to the Professional Office
Building, enhancements that have transformed
one of the most trafficked areas of the Hospital
from ordinary to extraordinary.
Much of the renovation was paid for through
a generous gift from the Hospital’s Auxiliary,
which closed out its 67-year history at the
Hospital with a $500,000 donation to the St. Clair
Hospital Foundation. Instrumental in the
Hospital’s founding in the early 1950s, the
Auxiliary donated more than $6 million to St. Clair
throughout the decades. In its honor, the First
Floor Lobby was renamed the “Auxiliary Lobby.”
And while the lobby’s facelift has enhanced
the aesthetics, it also has greatly improved how
patients and visitors navigate the building. The
entrance features a new covered, wide entryway
with automatic doors for patient drop-off or valet
service. Once inside, a new 45-inch electronic
touch-screen Directory makes finding a physician’s
office, Patient Registration, or even Café 4,
a simple, speedy process.
A short walk through the sun-drenched
glass atrium leads to a new art gallery featuring
original paintings and photography of local
artists for sale. Just past the art gallery is a
new Information Desk, where patients and
visitors can talk with a friendly customer
service representative or volunteer before
stepping onto nearby elevators or relaxing
on the brightly lit lobby’s many new couches
and chairs.
When exiting the Hospital or the Professional
Office Building through the Auxiliary Lobby,
patients and visitors have their choice of two
convenient Pay Stations for the Parking Garage’s
new ticket-based system. �
AuxiliAry lobby
Renovations Enhance Patient and Visitor Experience