St. Clair Hospital HouseCall Vol VI Issue 1
-
Upload
dymun-company -
Category
Documents
-
view
219 -
download
1
description
Transcript of St. Clair Hospital HouseCall Vol VI Issue 1

HouseCallVOLUME V ISSUE 2
HouseCallVOLUME VI ISSUE 160
YEARS | 1954 - 2014CELEBRAT ING
Broken Heart Syndrome I From Hospital Gown To Wedding Gown Ask The Doctor I History Minute I Focus On GivingAgain Ranked Among The 100 Top Hospitals® In The Nation
Taking the offensiveagainst pain
A REVOLUTIONARY APPROACH TO KNEE AND HIP REPLACEMENT
inside
Urgent Care Opensat Village Square
Plus
Please see page 18

Brett C. Perricelli, M.D. specializes in complex hip and knee joint replacement surgery at St. Clair Hospital,
spending his days performing total hip arthroplasty (THA) and total knee arthroplasty (TKA). In recent
months, he has become a trailblazer in his specialty, pioneering a revolutionary approach to total
joint replacement that holds the promise of a new era in the field. His approach to controlling pain after
hip and knee surgery represents a dramatic departure from the conventional approach. His protocol is
not just innovative; it may be transformative.
Pain. It’s a fundamental issue in joint replacement. The pain
and disability of osteoarthritis eventually become unbearable,
driving people to orthopaedic surgeons in search of relief.
Joint replacement will bring that relief, or at least significant improve-
ment, but first, there’s the procedure itself — generally considered
by surgeons to be among the more painful of all surgeries. Consider
what is involved: to accommodate the implant, the surgeon makes
multiple cuts in large bones, shaping the ends of the femur and tibia,
and cutting out the arthritis to replace it with metal implants. “It’s
literally sawing the bone in multiple places,” Dr. Perricelli explains.
“There is also dissection of the soft tissue that has multiple nerve
endings.” The resulting post-operative pain can actually be an
impediment to recovery, when it keeps patients from adhering to
their physical therapy (PT) regimen.
Dr. Perricelli takes the offensive against this pain, aggressively
treating it before he even begins the surgery. His comprehensive
approach to analgesia is all about altering the patient’s experience
of pain and facilitating a faster, gentler and more comfortable post-
operative recovery process and more successful rehabilitation. His
“Peri-operative Pain Protocol,” is a regimen that is centered on multi-
modal analgesia — “hitting pain from many angles,” he calls it —
and local peri-articular injections, given with exquisite precision into
the surgical site. Pain is controlled for up to three days after surgery,
with effects that can last much longer. The result is less reliance on
narcotics and fewer narcotic-related side effects, which can inhibit
recovery and create complications that prolong length of stay, increase
patient discomfort and drive up costs. “Joint replacement surgery, and
knee replacement in particular, are difficult for patients,” he explains.
“They feel agonizing pain that is traditionally treated with narcotic
painkillers that leave them groggy and nauseated. In the old paradigm,
pain management means narcotics. My goal is to improve pain control
throughout the peri-operative period — before, during and after
surgery — in order to decrease narcotic use and minimize complications
associated with narcotics. It gets patients back on their feet faster.”
TransformingOrthopaedic Surgery
2 I HouseCall I Volume VI Issue 1
Pioneering TreaTmenT

Volume VI Issue 1 I HouseCall I 3
“My goal is to iMprove
pain control . . .
before, during and
after surgery . . . it gets
patients back on their
feet faster.
”BRETT C. PERRICELLI, M.D.ORTHOPAEDIC SURGEON
Brett C. Perricelli, M.D.

no Post-op Pain
Laverne Lewis, R.N., a former St. Clair Hospital nurse, and a resident
of Upper St. Clair, had TKA surgery November 19. “I was out of bed walking
with a walker that night. I had no pain on my first post-op day until I had
physical therapy. During rehab, I just took an anti-inflammatory and now,
if I have pain, I take Tylenol.” Living in a split level house with three floors,
she has a lot of stairs to climb. Thus, she opted to spend three weeks at
a rehab facility before heading home. “Having PT and OT (occupational
therapy) every day was a big advantage. I also had home PT two or three
times a week, and then outpatient PT at St. Clair. They gave me a walker
but I don’t use it, and I only use my cane when I go out.”
4 I HouseCall I Volume VI Issue 1
Continued from page 3
Pioneering TreaTmenT
it Didn’t Hurt much at all
When Liza Minnelli was asked on a talk show about her knee replacement,
she said the pain was so horrific that it left her eyes permanently crossed.
She was joking, of course — about her eyes. But the pain can be so severe
that sometimes, patients who need to have both knees done will choose not
to return for the second procedure. That was the case for Deb Gossic, 61, a
retired physical education teacher. “I had knee replacement surgery eight
years ago. The pain was worse than labor and lasted much longer. I decided
that no matter how bad my other knee got, I would not go through that again.”
Her other knee did get worse and she took cortisone shots and
endured it, until she heard about Dr. Perricelli. “It was a completely
different experience this time,” she raves. “It was like night and day.
The first time, I was on Vicodin and morphine and I could not sleep due
to the pain. It took me forever just to get dressed for PT.” Her second
TKA took place in October. “I didn’t realize I would have almost no pain.
I woke up in the Recovery Room and I thought that they had not done the
surgery. I asked, ‘What happened? Did you do it?’ I was waiting for the
medication to wear off and the terrible pain to begin. It never did.”
Gossic recalls that her PT began 15 minutes after she got to her room
on the orthopaedic floor. “I had my surgery Tuesday and I was home Friday.
I never took the narcotic pain medication; most of the time, I did well with
Tylenol. I put off the second surgery for eight years. This time, the experience
was amazing. Dr. Perricelli has perfected this, and I’m grateful to him and
to St. Clair for the excellent care.”
“i was waiting
for the
Medication
to wear off
and the
terrible pain
to begin.
it never did.
”DEB GOSSIC KNEE REPLACEMENT PATIENT
Deb Gossic

Volume VI Issue 1 I HouseCall I 5
a multimodal approach
The old approach to pain management has
numerous drawbacks that affect recovery and
quality of life. Nerve blocks numb the thigh and
knee joint, leading to a decrease in pain but also
severe weakness of the quadriceps muscles, the
major thigh muscles that rehabilitate the knee.
Patients have difficulty getting up and walking,
and the resultant immobility can produce many
complications, such as falls, blood clots and
urinary retention. There is also risk of injury to
the nerve itself. Once the nerve block has worn
off, usually several hours after surgery, the
patient may have severe pain that requires
narcotic medications. These can produce drowsi-
ness, nausea and constipation. The multimodal
approach employed by Dr. Perricelli relies less
on narcotics and blocks, and instead uses
multiple short and long lasting pain medications,
given in a site-specific, rather than systemic,
manner, combined with low doses of oral and
intravenous medications.
Dr. Perricelli describes his three-step
program. “I begin treating pain and nausea
before I start the surgery. We know it’s going
to happen, so why not get a head start on
treatment? The pre-op protocol consists of
giving the anti-inflammatories and an anti-
nausea skin patch in the pre-op holding area.
The second, intra-operative part of the
protocol is more complicated. The patient is
given spinal anesthesia, then IV Tylenol for
pain, IV anti-nausea medication, an anti-bleeding
medication, and steroids to prevent inflammation,
which is a huge factor in pain. I give the two
workhorses — the injections — right into the
operative site. The drug Exparel is suspended
in bubbles of fat, which slowly break down and
release the medicine over 72 hours. I then inject
other anesthetics, anti-inflammatory agents
and epinephrine into the knee at any point where
I think I’m going to cause pain. This is hitting
the pain right where it happens. It’s a painstaking
process and adds time to the procedure, but
it’s worth it.”
The third step is the post-operative care
of the patient. Once on the patient care floor,
the patient receives intravenous Tylenol, oral
Celebrex, Pepcid and Tramadol, a non-narcotic
pain medication. “If the patient needs opioid pain
medication, it’s available,” says Dr. Perricelli.
“Many of my patients don’t need it. They also
don’t need the pain medication pumps for IV
morphine.” Patients are discharged to home
with Celebrex and Tramadol, plus oxycodone
if they need it.
Joint replacement is not pain-free surgery,
Dr. Perricelli emphasizes, but it is far more
comfortable when done in this manner. “The
absence of pain and inflammation is the key.
When you control the immediate pain and
inflammation, the effects are longer lasting.
It’s not like it wears off and then the patient is
miserable. Seeing my patients looking comfort-
able after surgery is the most amazing experience.
One was up and making his own bed when I went
in to his room the day after a hip replacement.
I could hardly believe my eyes.”
Continued on page 6
Dr. Perricelli’s Pain
managemenT Program
Has sHown remarkable
resulTs. His THree-sTeP,
mulTimoDal aPProacH
incluDes Pre- anD
PosT-oP oral, PaTcH anD
inTravenous meDicaTions,
Plus mulTiPle injecTions
aT THe oPeraTive siTe.
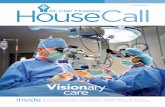
Dr. Perricelli, at far right, injects anesthetics and anti-inflammatory agents directly into the surgical site during knee replacement surgery to reduce or prevent the pain during recovery.

6 I HouseCall I Volume VI Issue 1
Continued from page 5
Pioneering TreaTmenT
up and walking shortly after Hip replacement
That patient was Roger Kurtz, 60, from Bethel Park, a retired auto-
motive interior repair specialist who spent his workdays outdoors, on his
feet and often in contorted positions that led to osteoarthritis in his hips.
Kurtz had his left hip replaced one year ago, using conventional methods,
and he had the right one done in early November; both were done by
Dr. Perricelli. “I went in with a list of 25 questions and he answered
every one without ever looking at his watch. After my first operation,
I came out of the O.R. with a drain in my hip, a catheter, IVs and morphine.
I was in bed all day and in the hospital for four days. I went home on
crutches. The surgery in November was nothing like that. I was out of
bed that evening and walking. I had PT the next day and I never needed
any morphine. I went home in two days with just a cane; I took oxycodone
for three days and then switched to Tylenol.
In rehab, my PT told me that I was three or four weeks ahead of
schedule with my walking. I can tie my own shoes again! My advice to
people who need joint replacement is this: first, don’t be afraid; second,
don’t put it off too long; and third, go to Dr. Perricelli. He said to me,
‘Roger, I can take care of you.’ And he did.”
Tylenol was all she Took
Barbara Sasser never planned to have joint replacement surgery.
At 77, with an active social life, she had no known history of arthritis or
osteoporosis. But in the wee hours of a Sunday in December, she found
herself in the Emergency Department of St. Clair Hospital with a fractured
hip. She had fallen during the night and, according to Dr. Perricelli, the
orthopaedic surgeon who just happened to be on-call, she needed a new
hip joint. “He’s a great person and a great surgeon; he told me I was his
star patient. I was lucky that he was on call. He gave me a new hip and I
was only in the Hospital for a day and a half. I went to rehab for a week
and came home on Christmas Day. I had almost no pain and I never took
anything but Tylenol.” Sasser came home with a walker but used a cane
instead, for just a few days. She has already finished her physical therapy
and is eager to get back to her activities.
changing old Procedures
Implementation of the multimodal pain protocol was an enormous
endeavor for Dr. Perricelli, involving more than six months of design,
development and research. It required not only a change in procedures,
but also a shift in beliefs and attitudes. He conducted several in-service
trainings for staff, educating the nurses, aides and physical therapists
about the protocol and helping them view pain management in a new
way. “We had to change the way people think,” he says. “In the past, pain
management meant major narcotics like opioids and then managing all
their adverse effects; what I am doing is counter to everything the nurses
and I have been doing for years. I wanted the staff to understand the
process and embrace this. The staff grabbed the concept and ran with it.
They’re with the patients 24/7 and they taught me a lot about how to
make the entire protocol better.”
“It took some getting used to,” says Sandy Stanley, BSN, MS, a
charge nurse for St. Clair’s Center of Orthopaedics, “but the nurses like
it and think it’s working well. It’s been amazing. We’re used to giving
narcotic pain medications, but Dr. Perricelli’s patients don’t even use
the word ‘pain.’ Instead they might say that the knee aches,” she says.
Dr. Perricelli’s patients are getting up and walking on the day of surgery,
and going home one day earlier, in general, she says. “I give him a lot
of credit for preparing his patients so well, too; when the patient knows
what to expect, they experience less stress.”
Cindy Crock, R.N., has been a Recovery Room nurse at St. Clair
Hospital since 2008. She has cared for hundreds of joint replacement
patients and she’s enthusiastic about Dr. Perricelli’s pain regimen.
“It’s wonderful; it solves and prevents problems. Typically, after TKA,
when the spinal anesthesia wears off, the patient needs a femoral nerve
block in the Recovery Room. It takes away some of the pain and lasts a
few hours. They also need a pain pump. This can be hard on the patient.”
Dr. Perricelli's patients do not need either and they are stable enough to
leave recovery in under an hour, while the norm is 90 minutes.
David Mayer, CRNP, has worked in orthopaedics for 33 years. As the
nurse practitioner with Dr. Perricelli’s practice, South Hills Orthopaedic
Surgery Associates, he makes daily post-op rounds on knee and hip
replacement patients. “I’ve never seen anything like this,” he says.
“i was out of bed
that evening and
walking, and had
physical therapy
the next day.
” ROGER KURTZ HIP REPLACEMENT PATIENT
Roger Kurtz

Volume VI Issue 1 I HouseCall I 7
It’s making an enormous difference for patients.
I was at St. Clair when they started doing joint
replacement in the 70s, so I have seen all the
advances over the years. It’s wonderful to see
patients who are not writhing in pain or taking
narcotics, especially the elderly patients. They
don’t have a glazed, groggy look. Patients now
want to go home earlier. Most are discharged
in one or two days.” Mayer says Dr. Perricelli is
an exceptional surgeon. “He has an incredible
knowledge of the knee. He has great surgical
technique and takes his time. He calls every
patient on the night before surgery to see if
they feel ready and to answer last minute
questions. Patients appreciate that.”
Dr. Perricelli is a Pittsburgh native who
graduated from the University of Pittsburgh
School of Medicine. He completed three years
of a general surgery residency at UPMC,
followed by a complete orthopaedic surgery
residency there, under Freddie Fu, M.D.
He served as chief orthopaedic resident in
2009–2010, then completed a fellowship in hip
and knee replacement at OrthoCarolina Hip
and Knee Center in Charlotte, N.C., under
Thomas K. Fehring, M.D. He serves as a
reviewer of research for the Journal of
Arthroplasty and was recently selected by the
American Academy of Hip and Knee Surgeons
for a national leadership program. Through
his training and travels, he has encountered
orthopaedic surgeon colleagues across the
country; they share information about evolving
pain control techniques and review the literature,
and put it all together to create and enhance
this multimodal protocol. “It has a cumulative
effect; it’s synergistic,” he says. “I’m stunned
at how well the protocol solves problems
associated with conventional pain management.
It’s fun for me because my patients are
ecstatic. This approach produces happy patients,
good outcomes, shorter stays and lower costs.
It has surpassed my hopes and expectations,
and it feels awesome to me as a surgeon.
Part of being a physician is to keep learning,
to know and apply the research and stay on top
of things.”
Apparently, it sometimes means choosing
to be an agent of change, a gentle and caring
revolutionary, who brings in new concepts and
practices, and illuminates the path toward a
new direction. “The suffering that patients were
experiencing was unacceptable,” Dr. Perricelli
says. “We needed a new paradigm for joint
replacement surgery.”
“this pain regiMen solves and
prevents probleMs that can
be hard on patients.
”CINDY CROCK, R.N.RECOVERY ROOM NURSE
BRETT C. PERRICELLI, M.D.
Dr. Perricelli earned his medical degree at the University of PittsburghSchool of Medicine. He completed his residency in orthopaedic surgeryat the University of Pittsburgh Medical Center. Dr. Perricelli thencompleted a fellowship in hip and knee replacement at OrthoCarolinaHip and Knee Center, Charlotte, N.C. He practices with South HillsOrthopaedic Surgery Associates, P.C.
To contact Dr. Perricelli, please call 412.283.0260.
Cindy Crock, R.N.

8 I HouseCall I Volume VI Issue 1
HealingBroken Hearts
sTress carDiomyoPaTHy
Accurate diagnosis is key to
THROUGHOUT THE AGES, poets have given metaphorical meaning to the human heart. The heart, they say, holds theessence of a person; a kind person is softhearted, and a brave one, lionhearted. The heart aches when one suffers a loss,and it sings with joy when something wonderful happens. Every human emotion seems to find expression through the heart.
Modern medical science has told us something different. The heart, we have learned, is simply an organ, a muscle composedof soft tissue. It is nevertheless a vital organ, simple in structure but complex, even wondrous, in function. The healthy heartis a workhorse, an engine that never rests, its chambers and valves pumping life-sustaining blood throughout the body ina constant, rhythmic choreography. The heart is so essential that we ascertain the presence of life by the presence of theheartbeat. Encasing it within a bony cage of ribs, vertebrae and sternum, the body protects the heart, in an acknowledgementof this importance, and also vulnerability.
Hearts, cardiologists tell us, do not break. They weaken, they fail, their rhythms go awry and they become damaged whentheir own blood supply is compromised. But hearts don’t actually break. Or do they?

Volume VI Issue 1 I HouseCall I 9
According to Jeffrey Friedel, M.D., Chief of Cardiology at St. Clair
Hospital, there is in fact a clinical condition known as Broken
Heart Syndrome, or Takotsubo Cardiomyopathy. First described
in Japan almost 20 years ago, it is caused by extreme, sudden emotional
trauma or distress, and it causes damage to the heart, sometimes
permanently. “In Broken Heart Syndrome, there is a characteristic pattern
of damage to the heart muscle,” Dr. Friedel says. “The patients who
experience this are predominantly women, over age 65, who present
with symptoms similar to those of a heart attack: sudden chest pain,
shortness of breath, lightheadedness, and sometimes an irregular
heartbeat. An EKG will most often be
abnormal, with a pattern that looks
like a heart attack, and cardiac
enzymes will be elevated, indicating
the injury to the muscle. A cardiac
catheterization will show no blockages,
but a ventriculogram (a diagnostic test
in which the heart is filled with dye
so it can be visualized on X-ray as it
contracts) will show that the apex of
the heart (the bottom front of the
muscle) is enlarged and ballooned
out. It doesn’t move, so it cannot
pump effectively, but other parts of
the heart move normally.”
If detected in time and treated
appropriately, this damage will most
likely heal, although Dr. Friedel says
that a small percentage of patients will
have permanent damage to their hearts
and may require more specialized,
ongoing treatment. “We treat this like
we treat congestive heart failure,
with ace inhibitors, beta blockers and
diuretics. The patient will be admitted
to the hospital, probably for several
days in the ICU or CCU (Coronary
Care Unit), until the EKG is normal
and symptoms are improved.”
Broken Heart Syndrome is believed to be the result of a sudden surge
of the stress hormones adrenaline, epinephrine and norepinephrine.
“These cause spasms of the arterial blood vessels of the heart, which
cause the damage to the heart muscle,” Dr. Friedel explains. “Any sudden
and intense emotional upset or shock can cause this surge of stress
hormones. The classic event is the sudden death of a spouse, but it
can also be triggered by the death of any loved one.” It can be brought
on by extreme rage or fear as well. A heated argument, domestic abuse,
a home invasion, a car accident — even a surprise party — can be the
triggering event. But most often, it is brought on by the sudden, unbearable
loss of a loved one.
suffering the loss of a beloved Pet
Janet Ghise, 70, a resident of Bethel Park, knows all too well that
Broken Heart Syndrome is real. She and her husband, Cornell, traveled to
Cooperstown, N.Y., last summer to see their grandson play in a baseball
tournament, and left their beloved 14-year-old Peekapoo, Maggie, in the
care of a kennel. It was tough to leave Maggie behind, Janet recalls.
“Maggie cried so much when we left her. We weren’t worried, though.
Despite her age, she was healthy and had been to the vet for a check-up
recently. She was fine.”
At the tournament, they enjoyed seeing their grandson hit three
home runs. As they were leaving the
park, both Janet and Cornell found
messages on their cell phones from
the kennel. “As I was reading the
message —‘please call right away’ —
I overheard my husband, on his phone,
say, ‘She’s dead?’ Our dear little Maggie
had died suddenly at the kennel. They
didn’t know what happened to her,
but they could not revive her.”
For Janet, the unexpected death of
her precious pet was a profound loss,
shocking and deeply felt. “Maggie was
special, a good little dog; all the neigh-
bors loved her. It was also a terrible
loss for my husband, but he handled it
differently; Maggie went to work with
him every day and was a constant
companion.” Janet had experienced
other losses in her life but this one,
she says, felt different. “I cried all the
time; I couldn’t seem to stop. I just
could not bear it. I couldn’t talk about
her without crying. I wasn’t myself;
now i know that a broken heart
is real . . . broken hearts can
also be healed.
JANET GHISEBROKEN HEART SYNDROME PATIENT
“
”
Continued on page 10
Janet Ghise

I felt very tired.” It happened that Janet already had an appointment
scheduled with Dr. Friedel. She had had a stent placed in her artery
following a heart attack in the past, and he was her regular cardiologist.
“I had missed my July appointment and rescheduled for August, and
that turned out to be a good thing. If I had gone to the July appointment,
before Maggie died, I may not have been diagnosed and I could have died.”
Dr. Friedel did an EKG in the office, but he knew as soon as he saw
her that Janet was in trouble. “She is normally energetic and smiling,
but she was ashen and sweating. I sent her directly to the Emergency
Room at St. Clair. A cardiac catheterization showed that her stent looked
fine and there was no blockage. But the bottom of her heart muscle was
destroyed, in a classic Takotsubo presentation.”
Janet is receiving close follow-up care from Dr. Friedel and her heart
is almost back to normal. “Dr. Friedel told me that my heart was healing
itself, but I know that he is healing me, too. I told him about Maggie,
and he understood; he said I lost a family member when I lost Maggie.
I was worried that people would think I was crazy to grieve like this over
a pet, but now I know that lots of people do. I decided to tell my story
because it might help someone else and even save another life. People
need to know about this.”
Broken heart syndrome is a legitimate clinical diagnosis, Dr. Friedel
says. “This is not junk science. It’s well described in the literature and
widely accepted among physicians. Doctors are more aware of the
condition, but it’s probably underdiagnosed. You have to know what you
are looking for and once you see it, there is no mistaking it. The heart
actually changes shape.” That characteristic change in the heart — the
apical ballooning — is the source of the name Takotsubo, which means
“octopus trap” in Japanese. The affected heart closely resembles the
trap that Japanese fishermen use to catch octopuses.
Broken heart syndrome should be taken seriously and treated as
an emergency. People who have the classic symptoms — chest pain,
shortness of breath, weakness — should call 911. Although Broken
Heart Syndrome is not a heart attack, the symptoms are similar and
the condition can lead to sudden cardiac arrest.
an emotional malady
Broken heart syndrome is so similar in presentation to a heart attack
that it’s often initially misdiagnosed. That was the case for Rose Corrado,
72, of Mt. Washington, a semi-retired electrologist whose symptoms
developed after an intense emotional upset. “I was in the shower afterwards
and I felt a twinge in my chest that hit me really hard. I wasn’t afraid;
I thought I had the world’s worst case of indigestion. But I cancelled my
clients and drove myself to an urgent care center, where they immediately
called an ambulance and sent me right to St. Clair Hospital. I was taken
to the Cath Lab and they told me that if there was a blockage I would
either get a stent or have open heart surgery.”
As it turned out, Rose did not have a heart attack, and did not need a
stent or surgery. Instead, she learned that she had Broken Heart Syndrome.
“Dr. Friedel told me that my heart was only working at 30 percent capacity,
as though it was frozen, nearly standing still. He gave me medication to
strengthen my heart and encouraged me to quit working. But I felt okay
and wanted to go back to work; I like to be around people. I have clients
who depend on me.”
Rose says that she has learned an important life lesson from her
experience. “It wasn’t like me to get that upset and now I know that it
is not worth it. Nothing is worth dying over. I’m trying to stay mellow,
because if it happens again, I could die. I like to stay busy with my husband
Tako-tsuboTako tsubo [noun, Japanese] fishing pot for trapping octopus.
In Takotsubo cardiomyopathy, also known as Broken Heart
Syndrome, the heart, affected by acute or sudden distress
or loss, results in apical ballooning. The shape closely
resembles the trap that Japanese fishermen use to catch
octopuses. Broken Heart Syndrome should be taken
seriously and treated as an emergency.
Continued from page 9
Cardiologist Jeffrey Friedel showswhat a broken heart looks like.
10 I HouseCall I Volume VI Issue 1
“broken heart syndroMe is a legitiMate
clinical diagnosis widely accepted
aMong physicians . . . the heart actually
changes shape.
” JEFFREY FRIEDEL, M.D.
sTress carDiomyoPaTHy
LEFT VENTRICLE
NORMALHEART
“BROKEN”HEART
OCTOPUS TRAP(TAKO TSUBO)

Anthony, my four kids and seven grandkids, but I have less energy now.
I have to stop to sit and rest. I am working part-time and I make jewelry.”
Dr. Friedel says that Rose is recovering well. Like Janet Ghise, she
was already his patient, being treated for an aortic valve problem.
“Rose’s underlying heart disease made it easy to assume at first that
she was having a heart attack,” Dr. Friedel says. “Her enzymes were
elevated and she had EKG changes, but it was from extreme stress and
not a blockage.
“Stress is a direct trigger of a lot of serious problems. We know now
that severe physical or emotional stress, even in the absence of significant
plaque, can cause a heart attack through this same mechanism. That surge
of catecholamines (adrenaline hormones) raises the blood pressure and
can cause plaque to rupture and act like a blood clot. We’ve changed our
thinking about heart attacks over the past 10 years. It is not that the plaque
grows and becomes an obstruction, but that it ruptures.”
This has implications for diagnosing heart disease, Dr. Friedel says.
A stress test will not reveal the presence of plaque build-up, so cardiologists
are not relying on them as in the past. Instead, they prefer a cardiac CT scan
or calcium scoring, which looks at plaque within the coronary arteries.
Broken Heart Syndrome can be treated and is usually reversible.
Heart disease in general is far easier to prevent than to treat, says
Dr. Friedel. He encourages everyone to live a healthful lifestyle, learn
to manage stress, and become aware of the symptoms of heart disease.
And, if you have an experience of extreme emotional distress and you
don’t feel right afterwards, seek medical attention. “At St. Clair, we have
all the most advanced tools to treat heart disease. If you have symptoms,
don’t hesitate to come to the Emergency Room so we can make a diagnosis
and begin treatment.”
It may well be that the poets who have found love, courage and character
in the heart were not wrong after all. We are complex beings, and research
into the mind-body connection, a new frontier in medicine, is fascinating
in its possibilities and implications. Before her appointment with Dr. Friedel,
Janet Ghise told her husband Cornell that she hoped her cardiologist
could fix her broken heart. It was, she thought then, just an expression.
“Now I know that a broken heart is real, and it was actually a relief to
know that. It’s real, and it can be life threatening. But broken hearts
can also be healed.”
JEFFREY FRIEDEL, M.D.
Dr. Friedel earned his medical degree at the Pennsylvania State University College of Medicine and completed his residency at Allegheny General Hospital in Pittsburgh. He also completed fellowships in cardiologyand interventional cardiology at Allegheny General Hospital. He is board-certified and practices with South Hills Cardiology Associates, a division of St. Clair MedicalServices.
To contact Dr. Friedel, please call 412.942.7900.
My heart was only working at
30 percent . . . as though it was frozen,
nearly standing still.
ROSE CORRADOBROKEN HEART SYNDROME PATIENT
“
”
Volume VI Issue 1 I HouseCall I 11
Rose Corrado

Wedding GownFrom Hospital Gown
in 48 hours
to
minimally invasive surgery
12 I HouseCall I Volume VI Issue 1
Jacki Fury Hennon was a beautiful, beaming bride on October 2, 2010. Escorted by her parents,
and preceded by a procession of seven bridesmaids, Jacki walked slowly down the aisle toward
her waiting fiancé, Christopher Hennon. It was a remarkable sight — not just because Jacki
was a beautiful bride, but because just 48 hours before, she was wearing a very different
kind of gown: a hospital gown, as she lay intubated and under general anesthesia
on the operating table of a St. Clair Hospital surgical suite, in the capable hands
of St. Clair Hospital Obstetrician/Gynecologist Douglas H. MacKay, M.D.

acki’s fantasy wedding almostdidn’t happen. A project
administrator/financial analyst forBayer Corporation in Robinson Township,with a side business as a floral designer, Jackiwas a detail-oriented young woman who knewhow to make things happen. She spent 18months meticulously planning every detail ofthe wedding of her dreams. The reception wasplanned for Jacki’s favorite Pittsburgh place:PNC Park. She did not overlook a single detail, and as the wedding date approached,she felt confident, excited and very happy.Things were going perfectly.
Until wedding week. On the Saturday before the wedding, as Jacki was running lastminute errands with her mother, MaribethFury, she began to feel sick, with nausea andstomach pain. She stayed home all weekend,hoping to feel better with rest. No such luck— her condition grew worse, and on Sundaynight, a worried Chris took her to the Emergency Room at St. Clair Hospital. Bythen, Jacki had a fever and her abdominal painwas severe. “The pain was agonizing, beyondanything in my experience,” Jacki recalls.
An ultrasound showed that Jacki had an ovarian cyst and was advised to see her gynecologist about the cyst as soon as possible.
Jacki felt increasingly anxious; the weddingwas now just days away, and her rehearsal dinner was scheduled for Thursday — a choiceshe made so that she could spend Friday creating bouquets of flowers.
On Wednesday, she and her mother returned to the ER. Doctors there ordered aCT scan and another ultrasound. These testsshowed that the ovarian cyst was so largewithin Jacki’s pelvis that it had created arare, extremely painful and potentially life-threatening condition known as ovarian torsion. Ovarian torsion occurs when theovary and the fallopian tube become twisted,cutting off blood flow to the ovary itself. It can be a surgical emergency.
And so, early Thursday morning, with lessthan 72 hours to go until the wedding, Jackiand Chris met Dr. MacKay, a board-certified
obstetrician/gynecologist who practices in Mt. Lebanon and Peters Township with Advanced Women’s Care of Pittsburgh, P.C.“Dr. MacKay was on-call, and was called in for consultation,” Jacki recalls, “and every-thing changed for the better when he arrived.He reviewed all my tests and labs and toldme I needed surgery; he warned me that Imight lose my left ovary. But I felt hopeful; I knew I was in good hands. I had immediateconfidence in Dr. MacKay. He told me thathe would do the procedure using minimallyinvasive techniques and I would still have mybeautiful wedding.”
Jacki went into surgery almost immediately.The procedure that Dr. MacKay performedwas a “salpingo-oopherectomy” — the removalof the ovary and fallopian tube. Unfortunately,Jacki’s ovarian cyst had twisted tightly aroundthe ovary. “Sometimes, we’re able to twistthe vessels back and then observe to see ifthere is perfusion (blood flow) to the ovary,”Dr. MacKay explains. “It’s similar to a heart
attack, in that the blood supply to the organ is cut off, causing the tissue to die. In Jacki’scase, the ovary and tube could not be saved.”
On Thursday evening, while her guests enjoyed the rehearsal dinner, sans the bride,Jacki recovered at St. Clair. “I woke up in therecovery room to a different world,” she says.“Despite pain from the surgery, my four daysof agony were over.” Her mother and Chriswent to the dinner, but Jacki was not alone;bridesmaid Marlene Hedberg sent her ownmother, Cheryl Rieland, to St. Clair to sitwith Jacki. “I was so grateful. Afterwards,Chris, my sister, bridal party members andmy cousins all came to see me.”
Cancelling the wedding was not an optionfor Jacki. “I was going forward with my wedding,even if it meant being pushed down the aislein a wheelchair with an IV. My gown wasstrapless; an IV would be no problem! I spent18 months planning my wedding and I had 200people coming. Dr. MacKay told me I coulddo it, and I had no doubts. I was a bride.”
“i always try to do this
laparoscopically, for the
sake of the patient. recovery
is faster and there’s less
post-op pain.
”DOUGLAS H. MACKAY, M.D.OBSTETRICIAN/GYNECOLOGIST
J
Volume VI Issue 1 I HouseCall I 13
Continued on page 14
Douglas H. MacKay, M.D.

14 I HouseCall I Volume VI Issue 1
She got through it, she says, with adrenaline, teamwork, strengthand a lot of love. “I left the hospital on Friday and went immediately to have a pedicure. I spent that afternoon on my patio, surrounded by relatives and hundreds of flowers and ribbons. I pointed to the flowers I needed, and they handed them to me. I made all my bouquets, just as planned.”
in sickness
anD in HealTH
On wedding day,Jacki had some anxiousmoments as she donnedher gown. Would it still fit over her threeincisions and sore,swollen belly? “Therewas a moment of panic,as the dress was tight,but it fit. My hair andmakeup were done at
the house and everyone helped me. When I walked down the aisle,my parents were pretty much holding me up. During the ceremony,there was a lighthearted moment when we got to the words ‘… in sicknessand in health.’ Everybody in the church laughed.” Fortuitously, Jackiand Chris, an asset integration technician at Crown Castle Internationalin Southpointe, had planned a delayed honeymoon. “I could not havegotten on a plane, so it worked out. And yes, I danced at my wedding!Just not much!”
Jacki’s experience illustrates the beauty of minimally invasive surgery, says Dr. MacKay. “The cyst was so large that I might have done a large abdominal incision, but I always try to do this laparoscopically, for the sake of the patient. Recovery is faster and there’s less post-op pain. Pain is related to the length of the incision. With a large, openincision, Jacki could not have had her wedding.This was a challenging diagnosis becauseoften, with ovarian torsion, the torsion isintermittent. It comes and goes, twistingand untwisting, and the ultrasound may actually have been normal when theylooked. It’s best to be conservative with a young woman and not rush to operate, because she is in her child-bearing years.”
Jacki and Chris definitely wanted a family, and she became pregnantthe following May. “It was reassuring to us that I became pregnant so easily. We were thrilled. But then I miscarried in July, and we kepttrying, but had no luck for over a year. We had testing done and wewere preparing for me to start Clomid (a prescription medication thatstimulates ovulation). We had an appointment with Dr. MacKay todiscuss that, and when he walked into the room, he greeted us by saying, ‘Congratulations.’ We were confused — he’s congratulating us for deciding to go on Clomid? But then he said, ‘You’re pregnant!’”
That was December 14, 2012. Eight months later, Madelyn Hennonwas born, on August 16, at St. Clair Hospital. She was delivered byDr. MacKay, and she is a happy, healthy baby.
“For the past three years, Dr. MacKay has just happened to be on call every time I needed him, even though there are six doctors inhis practice,” says Jacki. “He’s an excellent surgeon, and he has a kind,warm bedside manner. He’s been there for me through every step of this journey. I’m so grateful to him, and my family loves him. Dr. MacKay is my hero.”
DOUGLAS H. MACKAY, M.D.
Dr. MacKay earned his medical degree at the Ohio State University School of Medicineand completed his residency in obstetricsand gynecology at West Penn Hospital, Pittsburgh. Dr. MacKay is board-certified by the American Board of Obstetrics and Gynecology. He practices with AdvancedWomen’s Care of Pittsburgh, P.C.
To contact Dr. MacKay, please call 724 .941.1866 or 412.561.5666.
minimally invasive surgery
Continued from page 13
Christopher and Jacki Hennon with daughter Madelyn.

ask THe DocTor
SCoTT A. HolEkAMP, M.D.
Ask the Doctor Q
A
Is it a sign of something serious if I notice
blood while using the bathroom?
Bleeding is a common reason why patients visit a
colorectal surgeon’s office. Patients may experience
significant blood in the toilet bowl; it may be mixed
in their stool, they may pass blood clots, or they may
notice it on toilet paper. Some have bleeding that
is not obvious, otherwise known as occult. In these
cases, a primary care physician discovers it with
simple blood or stool tests. Bleeding may accompany
constipation, diarrhea, or be spread throughout the
day; and it may or may not be associated with pain.
Although common causes of rectal bleeding
include benign conditions such as
hemorrhoids and fissures, we
must always be vigilant for risk
factors of colon polyps or
cancer, which can also cause
bleeding. The gold standard for
examining the entire colon is
the colonoscopy. Although
the American Cancer Society
recommends a screening
colonoscopy starting at age 50
for the general population, the
risk of having a polyp or
cancer is influenced by
age, medical history,
and family history.
We consider these
factors when determining at what age patients should
undergo their first and subsequent colonoscopies.
After ruling out more serious causes, a simple
history and physical will diagnose the majority of
rectal bleeding. Internal hemorrhoids tend to bleed
painlessly and have bright red blood. Anal fissures
can also have bright red bleeding, but are generally
accompanied by excruciating pain with bowel
movements. External hemorrhoids generally present
with pain instead of bleeding.
Dietary and bowel habits significantly affect the
incidence of hemorrhoids and fissures. Making sure
that the patient’s stools are soft and regular is key
to successful symptom management. In addition,
medical therapies can help reduce the inflammation
and muscle spasm that exacerbate symptoms. For
internal hemorrhoids, painless office procedures
such as banding or infrared coagulation can act as
an adjunct to medical and dietary therapy. Finally,
surgical therapy is an option for patients who have
continued symptoms despite dietary, medical and
office treatment. By looking for and addressing the
underlying cause of a patient’s symptoms, we are
able to offer a more durable solution.
As with any medical condition, it is important
to talk to your doctor if you are having any of these
symptoms, including bleeding or changes in
bowel habits.
Volume VI Issue 1 I HouseCall I 15
SCOTT A. HOLEKAMP, M.D.
Dr. Holekamp specializes in colorectal surgery. He earned his medical degree at theUniversity of Cincinnati College of Medicine. He completed his residency in generalsurgery at the Beth Israel Medical Center, New York City, and a fellowship in colonand rectal surgery at the University of Miami/Jackson Memorial Hospital.Dr. Holekamp practices with Colorectal Surgical Associates, a division of St. ClairMedical Services.
To contact Dr. Holekamp, please call 412.572.6192.
Scott A. Holekamp, M.D.

Focus on givingHisTory minuTe
For decades, Jack Bogut has graced the radio airwaves of
southwestern Pennsylvania with humor, creativity and an
exceptional talent for storytelling. Highly honored, Jack
is a Pittsburgh institution, familiar and beloved to legions of fans.
Raconteur, interviewer, host, speaker and author, the versatile
radio man is the recipient of numerous
prestigious awards: he was inducted
in 2011 to the Broadcasters Hall of
Fame; he was given the Pittsburgh
Radio and Television Club’s Lifetime
Achievement Award; and he was honored
by the March of Dimes with their AIR
(Achievement in Radio) Lifetime
Achievement Award. And in 2014, he
has received yet another honor, this one
from the hospital that he fondly calls
“St. Care Hospital.” Jack is serving as
a member of St. Clair Hospital’s 60th
Anniversary Honorary Committee, and
he is delighted to do so.
There is a story about this renowned
storyteller, this very public man, which
may come as a surprise to Pittsburghers.
Jack has had a long and happy relation-
ship with St. Clair Hospital — almost as
long as his radio career, which, of course,
included his long-running morning
drive-time show on KDKA-Radio. He
has had a lasting impact on the Hospital,
as a longtime member of the board of
directors, donor, vocal cheerleader for
the Hospital, and, perhaps unexpectedly,
as the designer of the iconic St. Clair
Hospital logo. Bogut explains how this came about.
“I was invited to join the board of directors at St. Clair in 1976,
during the period when the size of the Hospital was being doubled.
I was chairman of the Public Relations Committee, and we were
seeking a strong, clear identity for the Hospital within the community.
The board was concerned that doubling the size of the Hospital could
compromise the quality of care, especially as the construction took
place and created inconvenience for staff, patients and visitors. I felt
that we needed to send a message of a caring hospital. I thought about
how medicine is the “laying on of hands” and that patients come to
St. Clair and place themselves in the hands of the staff. So the image
of a pair of hands came to me.”
It was a stroke of genius. The simplicity of the image — those caring
hands, upright and open, facing each other like parentheses — conveys
much. The hands represent the caregivers who lay their skilled hands
upon the ill, the suffering and the vulnerable, offering sublime care
and compassion. They are the hands of surgeons, nurses, therapists
and many others. The logo color (originally a subtle shade of brown),
has come to be known as “St. Clair blue,” suggesting the hope and
optimism of a sunny, cloudless sky.
Distinctive and memorable, the logo has endured, and is readily
recognizable throughout the community. It greets visitors who enter
the Hospital through the front doors, where the door handles are
shaped like the two sides of the logo. “Every time the door closes
behind someone, the hands come back together,” Jack says.
His love for St. Clair is personal. “My mother was a nurse, so I was
always around medical people growing up, and I love nurses, who are
the heart and soul of the Hospital. My wife Joanie and I have been
patients at St. Clair, and we received excellent care. There’s very little
waiting at the Emergency Department, and the people are warm
and friendly. St. Clair’s growth has been amazing, and people in the
South Hills choose to go to St. Clair Hospital, with good reason —
it’s the best.”
1 9 5 4 - 2 0 1 4
C E L E B R A T I N G
Y E A R S
jack boguT:THe making oF an icon
16 I HouseCall I Volume VI Issue 1
“Medicine is the
‘laying on of hands’
. . . patients coMe to
st. clair and place
theMselves in the hands
of the staff. so the
iMage of a pair of hands
caMe to Me.
”
Photo courtesy of John Altdorfer/Mt. Lebanon Magazine.
Iconic radio personality Jack Bogut, host of the “Bogut in The Morning Show,” heard
on WJAS 1320 AM. Jack is the designer of the original St. Clair Hospital logo.
Original St. Clair Hospital logo created
by Pittsburgh radio personality
Jack Bogut in the 1970s.
Jack’s original logotype has evolvedover the years into a major brand icon.
JACK BOGUT

wHy i give
Conrad Rossetti is a Washington County
resident and an avid fly fisherman for whom
the sport is restorative and relaxing. So, while
at St. Clair Hospital’s Outpatient Center in Peters
Township, he saw the framed photograph of fishermen
on Canonsburg Lake hanging behind the reception
desk, it resonated with him. “I was inspired when I
saw that photograph,” he explains. “I’m passionate
about fly fishing. My wife Gerrie and I love the outdoors
and anything to do with water and boats. I saw myself
in the picture.”
The Rossettis decided to make a donation to
sponsor the colorful photograph, one of a collection
of 13 created by regional artist Leroy G. Pettis and
hanging in prominent locations throughout the Center.
The photographs feature 12 Washington County sites,
plus a picture of St. Clair Hospital that adorns the
Center’s Community Room. They are all available
for sponsorship through the St. Clair Hospital
Foundation. Small plaques bearing the donor’s name
will be placed beside each photograph. The Rossettis
were moved to donate by the quality of the photograph
and their high regard for St. Clair Hospital.
“Gerrie and I were impressed by the
Outpatient Center,” Rossetti says. “It
exceeded our expectations: the advanced
technology, the convenience and location of
all the departments, and the addition of the
café. It’s well thought-out and beautiful.”
Conrad Rossetti’s relationship with
St. Clair Hospital grew out of his volunteer
involvement with the Washington affiliate
of Habitat for Humanity. Following a 44-year
career in industrial sales and marketing,
Rossetti retired to his Nottingham County
home in 2005 and was eager to find a new
purpose. “I wanted to remain active and
give back. I’ve been blessed with good
health, a good life and good family. I read a
story about Habitat for Humanity seeking
to establish a “ReStore” for Washington
County. A ReStore is a non-profit home
improvement store and donation center that sells
new and gently used furniture, accessories, building
materials and appliances to the public at a fraction
of the retail cost. When St. Clair began demolition on
the site of the Peters Outpatient Center they donated
the salvage and recyclable items from the previous
structure to the Habitat for Humanity store. As some-
one who spent so much time on that site, overseeing
the salvage operation and literally watching the
Hospital’s vision for the Outpatient Center come to
life, I wanted to ‘pay it forward’ by sponsoring the
Canonsburg Lake photograph.”
Family is important to the Rossettis, whose
children and grandchildren all live within five miles
of their home. Sponsoring artwork at the Outpatient
Center creates a legacy for the close family and, for
Conrad, is a way of honoring his marriage to Gerrie.
“This is a special year — we’ve planned a year-long
series of trips and activities to celebrate our 50th
wedding anniversary. Sponsoring the photograph is
part of that; it’s a nice feeling to know that something
lasting exists to honor my marriage and family.”
CREATEYOUR OWNLEGACYSupport the continued growth of St. Clair Hospital by sponsoring one of 13 picturesque scenes ofour local community displayed in the St. Clair Hospital Outpatient Center-Peters Township. Sponsors will be recognized with a plaque placed near theselected artwork.
For information about sponsoring artwork, please contact the St. Clair Hospital Foundation at 412.942.2465 or [email protected].
making aPersonal connection
Bednar’s Farm & Greenhouse
Henry Covered Bridge
Volume VI Issue 1 I HouseCall I 17
jack boguT:THe making oF an icon
Conrad Rossetti
Washington Courthouse

St. Clair Hospital is bringing the same innovative
processes that helped make its Emergency
Department number one in the nation to
urgent care. The new St. Clair Urgent Care, located
on the ground floor of the St. Clair Hospital Outpatient
Center–Village Square in Bethel Park, is providing
care to people in need of immediate but not emergency
care, says Rachel L. Schroer, D.O., Medical Director
at Urgent Care. “In urgent care, we treat people who
come in with a focused problem that we are able to
fix. The most common problems that we treat are
upper respiratory infections, flu and sore throats;
cuts requiring sutures; sprains and uncomplicated
fractures; and skin infections. We can do X-rays and
point-of-care lab testing on-site for blood sugar,
strep throat, mononucleosis and urinary tract
infections. Urgent care is not a mini-emergency
department; we take care of urgent illnesses and
injuries. If a patient is more critically ill or needs
higher level testing or monitoring, such as with chest
pain or abdominal pain, they need to be evaluated
in our Emergency Room.”
Dr. Schroer transitioned into urgent care after
five years in private practice. She finds urgent care
challenging and satisfying. “It’s wonderful to be able
to see a patient quickly and resolve the problem right
away. There is always a lot of variety. This facility is a
great work setting; we have top-of-the-line technology
and beautiful aesthetics. All the physicians who work
here are board-certified. Patients love the facility, the
excellent care and the convenience.”
David Kish, R.N., Director of Emergency Services
and Patient Logistics for St. Clair Hospital, manages
St. Clair Urgent Care. To Dave, urgent care has many
benefits. “St. Clair has a great network of primary
care physicians. But if patients need to be seen after
hours, urgent care is here to fulfill that need.
18 I HouseCall I Volume VI Issue 1
conTinueD growTH
Urgent Care provides quick, convenient, quality care
close to home.
“the care provided
at urgent care
is designed to
integrate with
our priMary care
and specialty
networks.
” DAVID KISH, R.N. DIRECTOR OF EMERGENCY
SERVICES AND PATIENT LOGISTICS
Continuity of Care DISTINGUISHES ST. CLAIR URGENT CARE
Staffed by board-certified physicians, registered nursesand radiology technologists, St. Clair Urgent Care at Village Square welcomes patients seven days a week, 365 days a year.

“St. Clair Urgent Care is open seven
days a week and is staffed by a physician,
registered nurse, X-ray technologist and
patient registrars. The staff is cross-trained
to provide support to each other. Urgent
Care’s goal is to examine and treat each
patient in less than an hour. Our current
average is 56 minutes.”
St. Clair Urgent Care also facilitates
continuity of care, Dave explains. “The
care provided at Urgent Care is designed
to be seamless. For example, St. Clair Urgent Care has treated patients with
orthopedic injuries who were referred and seen immediately by orthopedic
surgeons whose practices are in the same building. In a similar fashion, several
patients who did not have a primary care physician were able to be connected
with PCPs and seen very quickly. Urgent Care’s location inside the Outpatient
Center is ideal, since patients using our lab and diagnostic imaging center can
also benefit from Urgent Care services.”
Both Dr. Schroer and Dave say the key to a smooth continuum of care is
communication, via the electronic health record, or EHR. “A summary of a
patient’s visit to St. Clair Urgent Care is easily accessed electronically by physicians
and facilitates communication between the primary care physician and the staff
at Urgent Care.”
St. Clair Hospital has a commitment to serve the community, says Dr. Schroer,
and St. Clair Urgent Care exemplifies that commitment. “Patients appreciate the
quality and immediacy of the services. People in the St. Clair communities are
accustomed to top-notch care; they expect a high quality of care. St. Clair Urgent
Care is unique because it's integrated. We offer streamlined care, excellent
communication with your own physician, and a convenient, comfortable location.”
RACHEL L. SCHROER, D.O., MEDICAL DIRECTOR
Dr. Schroer earned her medical degree from Lake Erie College of Osteopathic Medicine (LECOM).She completed her residency at UPMC–St. Margaret.Dr. Schroer is board-certified by the American Board of Family Medicine.
MATTHEW S. COOPER, D.O.
Dr. Cooper earned his medical degree from Lake Erie College of Osteopathic Medicine (LECOM). He completed his residency at UPMC-Shadyside. Dr. Cooper is board-certified by the American Board of Family Medicine.
EDIRI A. MONTOYA, M.D.
Dr. Montoya earned her medical degree from the University of Pittsburgh School of Medicine. She completed her residency at Washington Hospital. Dr. Montoya is board-certified by the American Board of Family Medicine.
BETHEL CHURCH RD.
WASHINGTON RD.
Eat’n Park
FORT COUCH RD.
FOR
T COU
CH R
D.
OXFORD DR.
HIGHLAND RD.
St. ClairUrgent
Care
South HillsVillage Mall
HomeDepot
St. ThomasMore ChurchT-line
T-line
OXFORD DR.
Norman Center
Giant EagleMarket District
• 365 DAYS A YEAR
• 9 A.M. TO 9 P.M.(9 A.M. TO 5 P.M. ON MAJOR HOLIDAYS)
• NO APPOINTMENT NECESSARY
URGENT CARE STAFF AND SERVICESSt. Clair Urgent Care, which opened January 13 in the
St. Clair Hospital Outpatient Center–Village Square in
Bethel Park, is staffed by board-certified physicians,
registered nurses, radiology technologists, and patient
registrars. It is open 9 a.m. to 9 p.m. (9 a.m. to 5 p.m. on
major holidays) seven days a week, 365 days a year,
no appointment necessary.
There are six examination rooms, two procedure rooms,
and an X-ray room. St. Clair Urgent Care also has a lab
offering, among other things, urine analysis and rapid
strep testing. St. Clair Urgent Care treats minor injuries
and illnesses. Below is a list of some of the common
ailments and conditions treated there:
St. Clair Urgent Care accepts most major health insurances
and can fill selected prescriptions on-site.
CONVENIENTLY LOCATED
• Allergies and asthma
• Colds, pneumonia and flu
• Coughs and sore throats
• Cuts requiring stitches
• Dehydration
• Earaches
• Eye infections
• Fever
• Fractures and minor
broken bones
• Skin rashes/infections
• Stomach ailments
• Urinary tract infections
Also available:
• Flu shots
• Sports physicals
VILLAGE SQUARE2000 OXFORD DRIVEBETHEL PARK, PA 15102412.942.8800
Volume VI Issue 1 I HouseCall I 19

St.Clair Hospital1000 Bower Hill RoadPittsburgh, PA 15243www.stclair.org
General & Patient Information: 412.942.4000
is a publication of St. Clair Hospital. Articles are for informational purposes and arenot intended to serve as medical advice. Please consult your personal physician.
Follow us on twitter at: www.twitter.com/stclairhospitalHouseCall
Outpatient Center–Village Square: 412.942.7100Physician Referral Service: 412.942.6560
Urgent Care–Village Square: 412.942.8800Medical Imaging Scheduling: 412.942.8150
Outpatient Center–Peters Township: 412.942.8400
St. Clair Hospital has again been named one of the nation’s 100 Top Hospitals®. The annual award — now in its 21st year — is givenby Truven Health Analytics (formerly a division of Thomson Reuters)based on an objective analysis of patient safety, clinical outcomes,patient satisfaction, and value. Hospitals do not apply, nor do theypay, for this honor.
Jean Chenowith, senior vice president of Truven, noted that thewinners are “hospitals that deliver higher quality, higher satisfaction,and lower cost.” Among the other notable honorees in 2014 areDuke University Hospital (Durham, NC) and Vanderbilt UniversityMedical Center (Nashville, TN).
Truven calculates that if all Medicare inpatients had received thesame level of care as those treated in the award-winning hospitals:
• More than 165,000 additional lives could be saved;• Nearly 90,000 additional patients could have avoided medicalcomplications;
• And $5.4 billion could have been saved.St. Clair salutes its outstanding physicians and employees for this
prestigious achievement. To learn more about this honor, visit ourwebsite at www.stclair.org.
RANKED AMONG THE100 TOP®
OSPITALS IN THE NATION.
Again^