Spinal Cord Injury (ito nah).doc
Transcript of Spinal Cord Injury (ito nah).doc
-
7/27/2019 Spinal Cord Injury (ito nah).doc
1/21
Spinal Cord Injury
A spinal cord injury usually begins with a sudden, traumatic blow to the spine thatfractures or dislocates vertebrae. The damage begins at the moment of injury whendisplaced bone fragments, disc material, or ligamentsbruise or tear into spinal cord
tissue. Most injuries to the spinal cord don't completely sever it. Instead, an injury ismore likely to cause fractures and compression of the vertebrae, which then crush anddestroy the axons,etensions of nerve cells that carry signals up and down the spinal cordbetween the brain and the rest of the body. An injury to the spinal cord can damage a few,many, or almost all of these aons. !ome injuries will allow almost complete recovery."thers will result in complete paralysis.
Types of Spine Injuries
#. $ithout %eurologic Injury
!ome spinal injuries consist only of ligamentous or bony injuries. If the
damage to these support structures does not compromise the patency of
the spinal canal or directly traumati&e the sensitive cord, neurologic injurywill not be present.
. $ith %eurologic Injury
!ome spinal injuries immediately cause injury to the spinal cord. If the
bone injury disrupts the supportive nature of the spinal column, anymovement of the column can cause unnatural movement of the spine andcompromise the spinal canal, thus injuring the spinal cord.
Mechanisms of Injury
Categories of Movement that may Result in Spinal Cord Injury
Category Mechanism of Injury
(yperetension The head is forced back, and the vertebraeof the cervical region are placed in an
overetendedposition.
(yperfleion The head is forced forward, and thecervical vertebrae are placed in an
overfleion position.
Aial loading !evere blow to the top of the head causes ablunt downward force on the vertebrae and
the spinal column.
)ompression *orces from above and below compress thevertebrae.
+ateral bend The head and neck are bent to one side,beyond the normal range of motion.
"verrotation and distraction The head turns to one side, and the cervicalvertebrae are forced beyond normal limits.
-
7/27/2019 Spinal Cord Injury (ito nah).doc
2/21
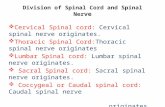
Level of Injury
!pinal cord injuries can also be classified according to the segment of the spinal cord that
is affected- pper cervical /)#0)1 injuries /atlas fractures, atlantoaial subluation, odontoidfractures, and hangman2s fractures1- +ower cervical /)30)41 injuries- Thoracic /T#0T#1 injuries- +umbar /+#0+51 injuries- !acral /!#0!51 injuries. The degree of functional recovery depends on the location andetent of the injury. The level of spinal cord injury is determined by the effect of theinjury on sensory and motor function.. 6etention of all or some of the motor or sensoryfunction below the level of injury implies that the lesion is incomplete. Total loss ofvoluntary muscle control and sensation below the level of injury suggests that the lesion
is complete. )omplete lesions involving spinal cord regions )# to T# result in tetraplegia.)omplete lesions involving spinal cord regions T to +# result in paraplegia. A personwith a complete cord injury follows the dermatome pathways for the level of sensoryloss.
Segmental Spinal Cord Level and Function
+evel *unction)l7)8 %eck fleors
-
7/27/2019 Spinal Cord Injury (ito nah).doc
3/21
)l7T# %eck etensors)3, )9, )5 !upply diaphragm /mostly )91)5, )8 !houlder movement, raise arm /deltoid1: fleion of elbow /biceps1: )8eternally rotates the arm /supinates1)8, );, )4
-
7/27/2019 Spinal Cord Injury (ito nah).doc
4/21
incontinence /inability to control bowel function1
priapism /painful penile erection1
if spinal cord is injured
6espiratory *ailure
the diaphragm receives orders form the brain via
nerves in the cervical spinal cord injury to the cervical spinal cord the nerve supply to the diaphragm is cut the main muscle of
breathing is no longer functional the patient2s breathing efforts
become ineffective patient2s feeling short of breath or havingobvious respiratory difficulty or simply by apnea
%eurogenic !hock
injury to spinal cord interrupt the nerves that
control the constriction of blood vesselscauses generali&ed dilation
of the blood vessels below the area of injury more blood moves
closer to skin2s surfacepatient2s skin appears flushed: warm skin
injury to spinal cord no communication betweenbrain and the blood vessels patient2s heart rate will not increase continuous falling of blood pressure /hypotension1
?aralysis
injury to lower parts of the spinal cord paralysisto the legs
injury to higher parts of the spinal cordparalysisto the arms
SPINL C!R" S#N"R!M$S
Incomplete cord injuries often cause recogni&able neurological syndromes that areclassified according to the area damaged.
Central Cord Syndrome
>amage to the spinal cord in this syndrome is centrally located. (yperetension of thecervical spine often is the mechanism of injury, and the damage is greatest to the cervicaltracts supplying the arms. )linically, the patient may present with paraly&ed arms butwith no deficit in the legs or bladder.
%ro&n'S()uard Syndrome
The damage in this syndrome is located on one side of the spinal cord. The clinical
presentation is one in which the patient has either increased or decreased cutaneoussensation of pain, temperature, and touch on the same side of the spinal cord at the levelof the lesion. @elow the level of the lesion on the same side, there is complete motorparalysis."n the patient2s opposite side, below the level of the lesion, there is loss of pain,temperature, and touch because the spinothalamic tracts cross soon after entering thecord. The posterior columns are interrupted ipsilaterally, but this does not cause a majordeficit because some fibers cross instead of running ipsilaterally. )linically, the patient2s
-
7/27/2019 Spinal Cord Injury (ito nah).doc
5/21
limb with the best motor strength has the poorest sensation. )onversely, the limb with thebest sensation has the poorest motor strength.
nterior Cord Syndrome
The area of damage in this syndrome is, as the name suggests, the anterior aspect of thespinal cord. )linically, the patient usually has complete motor paralysis below the levelof injury /corticospinal tracts1 and loss of pain, temperature, and touch sensation/spinothalamic tracts1, with preservation of light touch, proprioception, and positionsense.
Posterior Cord Syndrome
?osterior cord syndrome is usually the result of a hyperetension injury at the cervicallevel and is not commonly seen. ?osition sense, light touch, and vibratory sense are lostbelow the level of the injury.
-
7/27/2019 Spinal Cord Injury (ito nah).doc
6/21
*T!N!MIC N$R+!*S S#ST$M S#N"R!M$S
Spinal Shoc,!pinal shock is a condition that occurs immediately or within several hours of a spinalcord injury and is caused by the sudden cessation of impulses from the higher braincenters. It is characteri&ed by the loss of motor, sensory, refle, and autonomic functionbelow the level of the injury, with resultant flaccid paralysis. +oss of bowel and bladderfunction also occurs. In addition, the body2s ability to control temperature/poikilothermia1 is lost and the patient2s temperature tends to e=uilibrate with that of theeternal environment. There is no treatment for spinal shock.If the spinal cord injury produces an incomplete transection, the suppression of functionbelow the level of injury is temporary, lasting a few days, to weeks or months. Theduration of spinal shock is variable, depending on the severity of the insult and the
presence of other complications.The return of perianal refle activity signals the end of the period of spinal shock.6eflees associated with the area surrounding the injured cord return last. The skeletalmuscles become spastic and there is increased muscle tone and eaggerated fleor musclemovement.
-
7/27/2019 Spinal Cord Injury (ito nah).doc
7/21
Neurogenic Shoc,
%eurogenic shock, a form of distributive shock, is a condition seen in patients with severecervical and upper thoracic injuries. It is caused by the loss of sympathetic input to thesystemic vasculature of the heart and subse=uent decreased peripheral vascularresistance. !igns and symptoms include hypotension, severe bradycardia, and loss of the
ability to sweat below the level of injury. The same clinical findings pertaining todisruption of the sympathetic transmissions in spinal shock occur in neurogenic shock.
!rthostatic -ypotension
"rthostatic hypotension may occur in a patient with a spinal cord injury because thepatient is unable to compensate for changes in position. The vasoconstricting messagefrom the medulla cannot reach the blood vessels because of the cord injury.
PT-!P-#SI!L!.#
The spinal cord etends from the base of the brain to approimately the level of the firstor second lumbar vertebra. @lood is supplied to the cord by the anterior and posterior
spinal arteries. amageto the spinal cord is most often associated with damage to the vertebral column. Thevertebrae may be fractured, dislocated, or compressed.The more mobile areas of the vertebral column /such as the cervical area1 are mostfre=uently involved. As a result of the injury to the vertebral column, the spinal corditself may be contused, compressed, or dislocated.
Secondary Injury
-
7/27/2019 Spinal Cord Injury (ito nah).doc
8/21
- The release of ecess neurotransmitters results in overecitation of the nerve cells.
-
7/27/2019 Spinal Cord Injury (ito nah).doc
9/21
9. ?ercussion6eflees tested in !pinal Trauma
@iceps )578
@rachioradialis )578
Triceps ); 0 4
!uperficial abdominal /below umbilicus1 T;7#C)remasteric T# 0 +#
Dnee jerk +37+9
Ankle Eerk !#
Anal wink !7!9
@ulbocavernosus !37!9
?lantar response @rain7cord continuity
M/!R !%/$CTI+$ !F SPINL PR$C*TI!NS maintaining patient in a
neutral, in7line position.
!?I%A+ A+IF%M
-
7/27/2019 Spinal Cord Injury (ito nah).doc
10/21
7position the little fingers and heels of the hands just lateral to the occipital regionof the skull to support the head7with gentle inward pressure, hold the patient2s head immobile and preventfleionJetension, rotation, and lateral bending motion7lift the head gently off the ground
7position the head at about ground level7for infants, elevate the shoulder7apply no aial pressure
If the patient is in proneK7position your hands according to the patient2s position7if it will be some time until the patient can be moved to the supine position, placeyour hands so that they are comfortable during cervical stabili&ation7reposition your hands just before the patient is moved to the final position
C$R+ICL C!LLR PPLICTI!N
)ervical collar does not immobili&e the cervical spine
?osition the device under the chin and against the chest )ontour it over the shoulders and secure it firmly behind the neck
@e sure closures remain free from dirt, sand, fabric, or hair and make a secure sealbehind the neck
)ollar should fit snugly around the neck but not place pressure against its anteriorsurface
)ollar should direct a limiting force against the jaw and occiput to restrict anyfleionJetension of the head and neck
o not release or rela manual cervical stabili&ation until the patient is fullyimmobili&ed
STN"IN. T0$"!1N
Maintains the spine in alignment
(ave the patient remain immobile
Luickly assess any areas that will be covered by the cervical collar or long spineboard
Apply a cervical collar and place a long spine board behind and against the patient
Move the patient and spine board backward, tilting the patient on his heels untilthe patient and board are supine
$hile thora is supported, caregiver holding cervical stabili&ation rotates his or
her hands against the patient2s head without fleing or etending the head andneck as the patient moves from standing to supine
-$LM$T R$M!+L
"ffer significant protection for the head during impact but not proven to reduce spineinjuries.)onditions in which helmet should be removed
The helmet does not immobili&e the patient2s head within
-
7/27/2019 Spinal Cord Injury (ito nah).doc
11/21
Hou cannot securely immobili&e the helmet to the long spine board
The helmet prevents airway care
The helmet prevents assessment of anticipated injuries
There are, or you anticipate, airway or breathing problems
If helmet removal will cause further injury, do not remove the helmet
(elmet removal !tabili&e the cervical spine by manually stabili&ing the helmet
6emove face mask if present
6emove or retract any eye protection or any chin strap
@e careful not to manipulate the helmet
!tabili&e the head
Frasp the helmet and spread it slightly to clear the ears by pulling laterally justbelow and anterior to the ear enclosure
6otate the helmet to clear the chin, counter rotate to clear the occiput, then rotateto clear the nose and brow ridge
>+< !+I>enervated skin is particularly prone to pressure necrosis.Turn the patient every #7 hours. ?ad all etensor surfaces. ndress the patient toremove belts and back pocket keys or wallets. 6emove the spine board as soon aspossible.
The %ational Acute !pinal )ord Injury !tudies /%A!)I!1 II and III, a )ochrane
review of all randomi&ed clinical trials and other published reports, have verifiedsignificant improvement in motor function and sensation in patients with
-
7/27/2019 Spinal Cord Injury (ito nah).doc
15/21
complete or incomplete !)Is who were treated with high doses ofmethylprednisolone within 4 hours of injury.
o "verall the benefit from steroids is considered modest at best, but for
patients with complete or incomplete =uadriplegia, a small improvementin motor strength in one or more muscles can provide important functional
gains.o The administration of steroids remains an institutional and physician
preference in spinal cord injury. %evertheless, the administration of high7dose steroids within 4 hours of injury for all acute !)I patients is practicedby most physicians.
o The current recommendation is to treat all !)I patients according to the
localJregional protocol. If steroids are recommended, they should beinitiated within 4 hours of injury with the following steroid protocolmethylprednisolone 3C mgJkg bolus over #5 minutes and an infusion ofmethylprednisolone at 5.9 mgJkgJh for 3 hours beginning 95 minutesafter the bolus.
o
+ocal policy will also determine if the %A!)I! II or %A!)I! III protocolis to be followed.
Treatment of pulmonary complications andJor injury in patients with !)I includes
supplementary oygen for all patients and chest tube thoracostomy for those withpneumothora andJor hemothora.
The ideal techni=ue for emergent intubation in the setting of !)I is fiberoptic
intubation with cervical spine control. This, however, has not been proven betterthan orotracheal with in7line immobili&ation. *urthermore, no definite reports ofworsening neurologic injury with properly performed orotracheal intubation and
in7line immobili&ation eist. If the necessary eperience or e=uipment is lacking,blind nasotracheal or oral intubation with in7line immobili&ation is acceptable.Indications for intubation in !)I are acute respiratory failure, decreased level ofconsciousness /Flasgow score P1, increased respiratory rate with hypoia, ?)"more than 5C, and vital capacity less than #C m+Jkg.
In the presence of autonomic disruption from cervical or high thoracic !)I,
intubation may cause severe bradyarrhythmias from unopposed vagal stimulation.!imple oral suctioning can also cause significant bradycardia. ?reoygenationwith #CCO oygen may be preventive. Atropine may be re=uired as an adjunct.Topical lidocaine spray can minimi&e or prevent this reaction.
Possi3le complications of Spinal Cord Injruy2
S,in %rea,do&n2!kin breakdowns /also termed Qdecubitus ulcersQ or Qpressure soresQ1are a major complication associated with spinal cord injury. They occur as a result ofecessive pressure, primarily over the bones of the buttock /particularly the ischial
http://www.spinalinjury.net/html/_pressure_sores.htmlhttp://www.spinalinjury.net/html/_pressure_sores.html -
7/27/2019 Spinal Cord Injury (ito nah).doc
16/21
tuberosities and the trochanters at the hip1. *ollowing a spinal cord injury, there are notonly changes in muscle tone and sensation, but shifts in the supply of blood to the skinand subcutaneous tissues. Additionally, there is a loss of the normal elastic nature of thetissues underlying the skin. Increased stiffness, vascular alterations and alterations inmuscle tone combine to significantly reduce the skin's ability to withstand pressure. It is
estimated that the closing QpressureQ for skin breakdown is between 9C and 5Cmillimeters of mercury /about the same amount of pressure as placing a stamp onto anenvelope1. This complication is combated fairly aggressively through the use of pressure7relieving cushions that are either gel based or consist of a number of air bladders toreduce risk of the person Qbottoming outQ. The cost associated with medical andJorsurgical care of a single decubitus ulcer can run anywhere from R#C,CCC to R5C,CCC peradmission. This does not take into consideration the loss of productivity if the individualis in the work place
!steoporosis and Fractures2 The majority of people with !)I develop osteoporosis. Inpeople without !)I, the bones are kept strong through regular muscle activity or by
bearing weight. $hen muscle activity is decreased or eliminated and the legs no longerbear the body's weight, they begin to lose calcium and phosphorus and become weak andbrittle. It generally takes some time for osteoporosis to occur. In people who use standingframes or braces, osteoporosis is less of a problem. Fenerally, though, 7t years following!)I some degree of bone loss will occur.
sing the legs to provide support in transferring is helpful in increasing the load on thebones, which may reduce or slow down the osteoporotic process. !tanding using astanding frame or a standing table also helps prevent weakening of the bones and so doesusing braces for functional or parallel bar walking. %ewer techni=ues, such as electricalstimulation of the leg muscles, may decrease osteoporosis as well.
nfortunately, at the present time, there is no way to reverse osteoporosis once it hasoccurred. The main risk of osteoporosis is fracture. "nce the bones become brittle, theyfracture easily. An osteoporotic bone takes much longer to heal.
Pneumonia4 telectasis4 spiration2 ?atients with spinal cord injuries above the T9level of injury are at risk to develop restriction in respiratory function, termed restrictivelung disease. This occurs five to #C years following spinal cord injury and can beprogressive in nature. The =uadriplegic individual as part of a health care maintenanceroutine should have pulmonary function studies at yearly or every7other7year intervalsbetween five and #C years post injury. As the medical treatment of spinal cord7injuredindividuals continues to improve, respiratory complications of !)I are becoming moreprominent. Ade=uate health maintenance and protection from this complication areappropriate and necessary as part of the long7term care of the spinal cord7injuredindividual.
-eterotopic !ssification2 (eterotopic ossification is a condition not well understoodthat occurs in acute spinal cord injury and consists of the laying down of bone outside thenormal skeleton, usually occurring at large joints such as the hips or knees. The primary
-
7/27/2019 Spinal Cord Injury (ito nah).doc
17/21
problem with heterotopic ossification, or (", is the risk for joint stiffening and fusion.!hould the hip or knee become fused in a certain position, a surgical release is necessaryto allow range of motion to occur. nfortunately, it takes between # and #4 months forheterotopic bone to mature once it has developed. Activities that are used to prevent thedevelopment of (" include range of motion programs and other functional activities that
move the joints within a functional range. )urrently treatment is limited with theeception of preventing the joint fusion /termed ankylosis1.
Spasticity2After spinal cord injury the nerve cells below the level of injury becomedisconnected from the brain. *ollowing the period of spinal shock changes occur in thenerve cells that control muscle activity. !pasticity is an eaggeration of the normalreflees that occur when the body is stimulated in certain ways. After spinal cord injury,when nerves below the injury become disconnected from those above, these responsesbecome eaggerated.
Muscle spasms, or spasticity, can occur any time the body is stimulated below the
injury. This is particularly noticeable when muscles are stretched or when there issomething irritating the body below the injury. ?ain, stretch, or other sensations from thebody are transmitted to the spinal cord. @ecause of the disconnection, these sensationswill cause the muscles to contract or spasm.
Almost anything can trigger spasticity. !ome things, however, can make spasticity moreof a problem. A bladder infection or kidney infection will often cause spasticity toincrease a great deal. A skin breakdown will also increase spasms. In a person who doesnot perform regular range of motion eercises, muscles and joints become less fleibleand almost any minor stimulation can cause severe spasticity.
!ome spasticity may always be present. The best way to manage or reduce ecessivespasms is to perform a daily range of motion eercise program. Avoiding situations suchas bladder infections, skin breakdowns, or injuries to the feet and legs will also reducespasticity. There are three primary medications used to treat spasticity, baclofen, Galium,and >antrium. All have some side effects and do not completely eliminate spasticity.
There are some benefits to spasticity. It can serve as a warning mechanism to identifypain or problems in areas where there is no sensation. Many people know when a urinarytract infection is coming on by the increase in muscle spasms. !pasticity also helps tomaintain muscle si&e and bone strength. It does not replace walking, but it does help tosome degree in preventing osteoporosis. !pasticity helps maintain circulation in the legsand can be used to improve certain functional activities such as performing transfers orwalking with braces. *or these reasons, treatment is usually started only when spasticityinterferes with sleep or limits an individual's functional capacity
utonomic dysrefle5ia2 Autonomic dysrefleia /A>1 is a condition that can occur inanyone who has a spinal cord injury at or above the T8 level. It is related todisconnections between the body below the injury and the control mechanisms for blood
-
7/27/2019 Spinal Cord Injury (ito nah).doc
18/21
pressure and heart function. It causes the blood pressure to rise to potentially dangerouslevels.
A> can be caused by a number of things. The most common causes are a full bladder,bladder infection, severe constipation, or pressure sores. Anything that would normally
cause pain or discomfort below the level of the spinal cord injury can trigger dysrefleia.A> can occur during medical tests or procedures and need to be watched for.
The symptoms that occur with A> are directly related to the types of responses thathappen in the sympathetic and parasympathetic nervous systems. !ymptoms such as apounding headache, spots before the eyes, or blurred vision are thee direct result of thehigh blood pressure that occurs when blood vessels below the injury constrict. The bodyresponds by dilating blood vessels above the injury, causing flushing of the skin,sweating, and occasionally goosebumps. !ome patients describe nasal stuffiness and willfeel very anious. ncontrolled A> can cause a stroke if not treated.
The treatment for A> involves removing the reason for the stimulation. "ne of the firstthings a patient can do is to sit up. This naturally decreases blood prsessure. If there is acatheter in place, it should be checked to be certain that there is not a kink in the tubing.If there is not a catheter in place, the patient should be catheteri&ed. The bowels should bechecked to be ceratin there is no stool in the rectum. If the symptoms are caused by skinbreakdown, the patient should get to an emergency department as soon as possible.
The primary risk of A> is stroke. It is a potentially life7threatening condition. If A> isleft untreated, the body's attempt to control blood pressure will severely decrease theheart rate. This, combined with uncontrolled high blood pressure, can be fatal. *or thisreason, it is very important to treat this condition as soon as possible. The most important
thing patients can do to prevent A> from occurring is to take good care of themselves.?atients should monitor bladder output and should maintain a regular bowel programwhich fully empties the bowels. They should also do regular skin checks to preventpressure sores from occurring.
"eep vein throm3osis2 />GT1 or pulmonary embolism is a potentially severecomplication of spinal cord injury. As mentioned above, there are changes in the normalneurologic control of the blood vessels that can result in stasis or QsludgingQ. >eep veinthrombosis in the lower leg is almost universal during the early phases of recovery andrehabilitation. Thromboses in the thigh, however, are a great concern, as they are at riskfor becoming dislodged and passing through the vascular tree to the lungs. A majorobstruction of the arteries leading to the lung can potentially be fatal. Therapeuticmeasures to reduce or eliminate the risk for deep vein thrombosis include Ace wrappingof the legs and the use of pneumatic compression stockings. Medications administeredsubcutaneously, such as heparin, are useful in reducing blood viscosity and improvingflow. In the event that a thrombosis develops, treatment is begun with intravenousheparin. "nce ade=uate anticoagulation is provided, the patient is switched to ormedication, called )oumadin
http://www.spinalinjury.net/html/_pressure_sores.htmlhttp://www.spinalinjury.net/html/_pressure_sores.html -
7/27/2019 Spinal Cord Injury (ito nah).doc
19/21
Cardiovascular disease2 )ardiovascular disease is a major long7term risk of spinal cordinjury. !)I individuals live in general rather sedentary lives and are at higher risk forcardiovascular disease than the able7bodied population. Therefore, careful assessment ofcardiovascular function and the encouragement of eercise programs are appropriate andnecessary long7term aspects of spinal cord injury management and care. The prescription
of upper etremity eercise programs in spinal cord7injured individuals are similar tothose used in other populations with the eception of the use of adaptive e=uipment suchas racing wheelchairs or monoskis.
Syringomyelia' A post7traumatic enlargement of the central canal of the spinal cord istermed syringomyelia. It occurs in approimately #73O of all spinal cord7injuredindividuals. The primary risk of syringomyelia is a loss of function above the level of theoriginal spinal cord injury. *or eample, in a patient with a thoracic7level spinal cordinjury may complain to his or her physician of numbness and weakness involving theetremities. The condition will progress with time and needs to be treated aggressivelythrough surgical drainage. "ften patients with early evidence of a syrin will be followed
to evaluate the progression of the condition. !ignificant syringomyelia is treated withsurgical decompression and the placement of a drainage tube into the spinal cord.
Neuropathic6Spinal Cord Pain' %europathic /nerve7generated1 pain is a significantproblem in some spinal cord7injured patients. Garying types of pain are described inspinal cord injury. >amage to the spine and soft tissues surrounding the spine can causeaching at the left of the injury. %erve root pain is described as sharp or may be describedas having an electric shock7type =uality. "ccasionally !)I patients will describe phantomlimb pain or pain that radiates from the level of the lesion in a specific pattern that isrelated to injury or dysfunction at the nerve root or spinal cord level. Garious medicationsand nerve block procedures have been described and are of some use in the treatment of
neuropathic pain following spinal cord injury.
Respiratory "ysfunction' 6espiratory complications and infection predominate as post7!)I complications. $hen the injury involves the upper thora, the normal breathingpattern is permanently altered. The diaphragm does most of the work in =uiet breathing.The chest wall muscles /intercostals1 are used primarily for deep breathing or coughing.The abdominal muscles also participate in coughing. $hen the intercostal and abdominalmuscles are paraly&ed, the entire load is taken by the diaphragm. This results in poorcoughing and a high risk of pneumonia. ?neumonia is one of the most commoncomplications of acute spinal cord injury. ?reventive measures are very important toreduce the risk of pneumonia. These include percussion and drainage using gravity toassist: assisted coughing /also termed Q=uadQ coughing1: abdominal binders /to increasethe resistance against which the diaphragm works1: and early mobili&ation /i.e.: gettingthe patient out of bed as soon as possible1
Functional .oals for Specific Levels of Complete Injury
+evel Muscles Tested Abilities *unctional Foals
)#7 )37limited @reathing >epends on a ventilator for
-
7/27/2019 Spinal Cord Injury (ito nah).doc
20/21
)3 movement ofhead and neck
breathing.)ommunication Talking is sometimesdifficult, very limited or impossible. If abilityto talk is limited, communication can beaccomplished independently with a mouth stick
and assistive technologies like a computer forspeech or typing.>aily tasks Assistive technology allows forindependence in tasks such as turning pages,using a telephone and operating lights andappliances.Mobility )an operate electric wheelchair byusing a head control, mouth stick, or chincontrol, or a power tilt wheelchair forindependent pressure relief.
)37
)9
sually has
head and neckcontrol.Individuals at)9 level mayshrug theirshoulders.
@reathing May initially re=uire a ventilator for
breathing, usually adjust to breathing full7timewithout assistance.)ommunication %ormal.>aily tasks $ith speciali&ed e=uipment, mayhave limited independence in feeding andoperating an adjustable bed with an adaptedcontroller.
)5 Elbow flexors
/biceps brachii1
Typically hashead and neckcontrol, canshrug shoulder
and hasshouldercontrol. )anbend hisJherelbows and turnpalms face up.
>aily tasks Independence with eating,drinking, face shavingJwashing, brushing teeth,S hair care after aid in setting up speciali&ede=uipment.
(ealth care )an manage their own health careby doing self7assist coughs and pressure reliefsby leaning forwardMobility May have strength to push a manualwheelchair for short distances over smoothsurfaces. A power wheelchair with handcontrols is used for daily activities. >rivingmay be possible after evaluation by a =ualifiedprofessional to determine special e=uipmentneeds.
)8 Wrist extensors
/etensor carpiulnaris, etensorcarpi radialislongus and radialisbrevis1
(as movement
in head, neckshoulders, armsand wrists. )anshrug shoulders,bend elbows,turn palms upand down andetend wrists.
>aily tasks $ith help of some speciali&ed
e=uipment, can perform with greater ease indaily tasks of feeding, bathing, grooming,personal hygiene and dressing. Mayindependently perform light housekeepingduties.(ealth care )an independently do pressurerelief, skin checks, turn in bedMobility )an independently do transfers but
-
7/27/2019 Spinal Cord Injury (ito nah).doc
21/21
often re=uire a sliding board. )an use a manualwheelchair for daily activities but may usepower wheelchair for greater independence.
); Elbow extensors/triceps brachii1
!imilarmovement as an
individual with)8, maystraightenelbows.
>aily tasks Able to perform household duties.%eed fewer adaptive aids in independent
living.(ealth care Able to do wheelchair pushups forpressure reliefs.Mobility >aily use of manual wheelchair. )antransfer with greater ease.
)4 Finger flexors/*leor digitorumprofundus1
Added strengthS precision offingers resultingin limited handfunction.
>aily tasks )an live independently withoutassistive devices in feeding, bathing, grooming,oral and facial hygiene, dressing, bladdermanagement and bowel management.
T#
T7T8
Finger abductors
/Abductor digitiminimi1
(as normal
motor functionin head, neck,shoulders, arms,handsJfingers,greater use ofribJchest muscle
Mobility (as increased ability to do some
unsupported seated activities.A few individuals capable of limited walkingwith orthodic aids. This re=uires etremelyhigh energy and puts stress on the upper body,offering no functional advantage. )an lead todamage of upper joints.
T;7+#
Added motorfunction fromincreasedabdominalcontrol.
>aily tasks Able to perform unsupportedseated activities.(ealth care (as improved cougheffectiveness.
+7+5
(as additionalreturn of motormovement inthe hips andknees.
Mobility $alking can be a viable function,with the help of speciali&ed leg and anklebraces. +ower levels walk with greater easewith the help of assistive devices.
!#7!5
Ankle plantar
flexors
/Fastrocnemius1
Garious degreesof return ofvoluntarybladder, boweland seualfunctions.
Mobility Increased ability to walk with feweror no supportive devices.