Speech and Language Therapy in Huntington’s Disease
-
Upload
dieter-tucker -
Category
Documents
-
view
52 -
download
0
description
Transcript of Speech and Language Therapy in Huntington’s Disease
Speech and Language Therapy in Huntington’s Disease
Rita Twiston Davies, Clinical Lead SLTOxfordshire Health NHS Foundation Trust
Why Speech and Language Therapy?
As the most highly co-ordinated human activitySpeech is often affected relatively early in the
disease.(DYSARTHRIA)
Swallowing impairment can endanger life, result in malnutrition and /or dehydration
(DYSPHAGIA)
Either condition affects quality of life, limiting social interaction and impacting on health and well-being.
What an SLT sees:chorea fatigue
dysarthria
ataxia
dysphagiaMuscle
weakness
rigidity
HD depression
Facial expressionlimited
Word-finding difficultyWeak
voice
akathisiaclumsiness
frustration
chorea
Loss of voluntary movement control
Slow verbal processing
Clinical features
Like Parkinson’s disease: loss of facial expression, shuffling gait, festination and “freezing”, impairment of voluntary movement
Like MS: disease progresses in bouts of deterioration followed by periods of stability
Like MND: muscle weakness and fatigueSensory impairment implicit in muscular
impairmentSlowness of cognitive processing but verbal
comprehension preserved to varying degrees
How does working with people with HD differ?
Motivation/compliance Disease progression Combination of physical,
psychiatric/psychological features Long time-scale of the disease Families
How HD affects communicationDysarthria: Involuntary
movements + impaired co-ordination of voluntary movements lead to
• Poor co-ordination of breathing and voice, affecting volume, and pacing of speech
• Pitch variation of speech reduced
• Reduced co-ordination of oral and facial muscles, affecting intelligibility of speech and facial expression.
• Unpredictable speech patterns, further reducing intelligibility.
Impaired Language processing: • Comprehension of words is
generally retained but slows down
• This affects memory of the message
• So “information overload” happens more easily
• Retrieval of vocabulary is impaired (word-finding difficulty)
• Impacting on speed and accuracy of responses/information –giving
• Verbal communication generally becomes more effortful.
Plus initiation of verbal responses becomes impaired
How HD affects eating, drinking and swallowing
• Increased calorie intake• Effects of medication- reflux, nausea etc• Incoordination of oro-facial muscles and• Respiration /swallow timing • Sensory impairment• Longer mealtimes/increased fatigue• Reduced independence- supported feeding• Reduced oral hygiene –tooth brushing difficult• Reduced ability to protect airway causing increased risk of • airway penetration/choking• Increased risk of aspiration leading to chest infection• Decreased inhibition related to challenging behaviour around
mealtimes.
Feeding decisions in HD- an MDT approacho Sooner or later oral intake becomes an
issue for people with HD. o Independenceo Social interactiono Health –nutrition, hydration,medication,risk managemento Assessing risko Supporting feeding –when, how, what?o Supplementso Enteral feeding- decisions about P.E.Go
o Decisions involve SLT, Physio, OT, Dietetics, Nursing, carers/family as well as doctors.
SLT within the MDT
Role :not comprehensive and subject to variation! To support team in providing optimal and timely care To assess and give appropriate strategies for managing risk
arising from behaviour (communication)/dysphagia To support person with HD as required, in a manner acceptable
to them To monitor disease progression as it affects communication
and /or dysphagia and offer intervention/support whenever appropriate
To support families/carers in managing risk and ensuring well-being as far as possible
To be there when needed – the end and the beginning of all our roles
Interaction
Teamwork is essential for any complex condition. My key people from the wider team:
Physios = information about muscle tone positioning, especially for meals Hydro –a good place for voice /breathing work! OTs= adaptive equipment sensory and cognitive function information/discussion all the “techie “ bits I can’t do in computer sessions with
patients! Dietician =should be joined at the hip for HD! Menus, textures,weight management, supplements etc etc
Nurses= Who are THERE and KNOW! Music/ Art therapists= who help me think “outside the box” about
facilitating communication
What does an SLT do?
• Assess- HD is both progressive and dynamic; individual baselines needed
• formal/informal assessment for communication and eating,drinking,swallowing
• Advise- guidelines for support and risk management-to person and carers
• strategies for person with HD• Carers/families • Liaise- wherever and whenever needed- regular exchanges of
information essential to keep track of changes.
• Train – most of my colleagues in Oxfordshire will see one person with
• HD a year, at the outside. • Treat? In HD this is not a given. Audit needed of uptake of SLT with
people with HD.
Evidence base for SLT intervention
Evidence base? What evidence base? Gothenburg FOTT Rosenbek and Jones EHDN Standards of Care Working
Party guidelines Need for research into efficacy of
management techniques
Aims of SLT for people with HD
SAFETY: majority of deaths are from choking/aspiration leading to pneumonia
FUNCTION: use it or lose it –maintaining movement also sustains
sensation Withdrawal from communication
enhances difficulty
QOL: Eating, socialising, communicating –essential pleasures.
People with HD need to know that they are still members of the human race
What Is the right time for SLT intervention?
o NOW!o Don’t wait for behavioural change due to
frustration at communication difficulties!o Don’t wait for person to choke/become
malnourished/dehydrated/ have repeated chest infections
o DO refer as early as possible after diagnosis, preferably when still pre-symptomatic
How HD progression limits communication *Body posture is altered by choreic movements and impoverished
control of voluntary movements- affecting gestural support for speech
*The eyes remain a primary source of communication but impaired postural control may limit this
*Facial expression becomes more limited and chorea may resultin grimacing
*Speech becomes harder to initiate Volume and pitch of voice are harder to control and intonation is
less varied – no subtlety in meaning *Awareness of the subtexts of other people’s communication is
impaired – their tone of voice, facial expression etc. *Finding the right word is impaired –affecting the fluency of the
message/ losing the thread completely *Language processing slows down *Information can be retained, if given in a manageable way. *Verbal reasoning is likely to be impaired- affecting capacity.
Recent communication research: Results of Gothenburg study into effects of HD (IJLCD 2011)
How communication has changed for the individual
CarersFamily members
Effort, concentration, loss
Less depth in conversation
Change in understanding, need for adjustment
Variability, lack of initiative
Person with HD
How HD had changed communication for participants
Negative influences
CarersFamily members
Speed of others’ communication
Fewer people to talk with
Personality change
Lack of eye contact
Emotional Load, depression, stress
Timing of information
People with HD
What each group found helpful
Positive influences on communication
CarersFamily members
People with HD Speaking more
Support Sense of community, Trust
Stimulation
Activities, memories, questions
Need for increased participation
Supporting communication
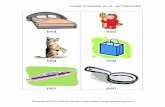
Low tech aids People to talk with Picture shopping lists Weekly planners/activity charts Communication charts Communication/life
books Memo boards Photo reminders Talking Mats Activities!
Not so low-tech aids Buttons/ switches Voice amplifiers VOCAs Computers with :KeyguardsSwitch accessPredictive lexicons
Low Tech Communication support – an example
The lady in this picture was diagnosed with HD over 20 years previously. She showed such enthusiasm for a Life Book, produced with the support of the SLT Assistant and ward staff, that we tried using A5 size pictures so she could communicate what mattered to her at that time:
Her choice of drinksHow she feltYes/No.Here she is being shown pictures
to indicate mood: happy, sad, so-so.
A Higher-Tech approach
This man has good verbal skills but is showing early impairment of language so his voice has been recorded, using everyday requests and information that he has selected, on a Go-Talk aid. He is learning to use pictures to link to these phrases as the time is approaching when he will find it hard to read and pictures will facilitate his use of a VOCA such as this.
Summary
People with HD need a multi-disciplinary approach They are more likely to work with the MDT if first contact is
pre-symptomatic Intervention will be sporadic, according to disease
progression Outcomes are seen in what hasn’t happened- no chest
infections- as well as in what has –still able to self-feed, for example.
This disease affects everyone differently – broad patterns apparent but timing of onset, rate of progression, personal reactions etc vary.
Effective Communication is key, for the individual and for their support network.
Gene therapy/cure still a long way off –research into effective management lacking and needed.
References
IJLCD 2011: papers by Hartelius et al and Ulrika Ferm on communication in HD and on Use of Talking Mats in HD.
Yorkston, Miller, Strand 1995:Management of speech and swallowing in degenrative diseases. Publ; Pro-Ed, Austin Texas.
Rosenbek and Jones 2009: Dysphagia in Movement Disorders
Publ; Plural Publishing -Clinical Dysphagia series- Oxford European Huntington’s Disease Network: Standards of
Care Working Group – in preparation. Huntington’s Disease Association publications:
Communication; Eating and Drinking