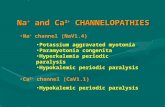
Sodium and chloride channelopathies with myositis: Coincidence or connection?
Click here to load reader
-
Upload
emma-matthews -
Category
Documents
-
view
216 -
download
0
Transcript of Sodium and chloride channelopathies with myositis: Coincidence or connection?

CASES OF THE MONTH
SODIUM AND CHLORIDE CHANNELOPATHIES WITH MYOSITIS:COINCIDENCE OR CONNECTION?EMMA MATTHEWS, MRCP,1 JAMES A.L. MILLER, MRCP,2 MALCOLM R. MacLEOD, FRCP,3,4 JAMES IRONSIDE, FRCPath,5
GARETH AMBLER, PhD,6 ROBIN LABRUM, PhD,7 RICHA SUD, PhD,7 JANICE L. HOLTON, FRCPath,1
and MICHAEL G. HANNA, FRCP1
1Medical Research Council Centre for Neuromuscular Disease, UCL, Institute of Neurology, Queen Square, London WC1N 3BG, UK2Department of Neurology, Royal Victoria Infirmary, Newcastle upon Tyne, UK3Department of Neurology, Stirling Royal Infirmary, Stirling, UK4Department of Clinical Neurosciences, University of Edinburgh, Edinburgh, UK5Division of Pathology, School of Molecular and Clinical Medicine, University of Edinburgh, Western General Hospital,Edinburgh, UK
6Department of Statistical Science, UCL, London, UK7Neurogenetics Unit, National Hospital for Neurology and Neurosurgery, London, UK
Accepted 25 March 2010
ABSTRACT: Introduction: A proximal myopathy develops insome patients with muscle channelopathies, but the causativemolecular mechanisms are unknown. Methods: We reviewed ret-rospectively all clinical and muscle biopsy findings of 3 patientswith channelopathy and additional myositis. Direct DNA sequenc-ing was performed. Results: Pathogenic mutations were identi-fied in each case. Biopsies demonstrated inflammatory infiltrates.Conclusions: Clinicians should consider muscle biopsy in chan-nelopathy patients with severe myalgia and/or subacute weak-ness and accompanying elevated creatine kinase. Chanceassociation of myositis and channelopathy is statistically unlikely.An alternative hypothesis suggests that inflammatory insultscould contribute to myopathy in some patients.
Muscle Nerve 44: 283–288, 2011
The skeletal muscle channelopathies are a group ofepisodic neuromuscular disorders that include theperiodic paralyses and the non-dystrophic myotonias.Causative mutations occur in genes that code forvoltage-gated skeletal muscle ion channels that regu-late muscle membrane excitability. Disturbed ionchannel function results in altered sarcolemmal excit-ability. The resulting symptoms of episodic muscleweakness (due to an inexcitable membrane) and/ormuscle stiffness (myotonia due to a hyperexcitablemembrane) reflect this fact. The natural history ofthese disorders has not been described extensively,although there is evidence, particularly in the peri-odic paralyses, that a significant proximal myopathycan develop.1,2–8 In addition, there are reports ofmoderate to severe myalgia8–13 and elevated creatinekinase (CK)2,6,11,12 in muscle channelopathy patients,although the cause of this is not fully understood.
We examined retrospectively 3 patients with ge-netically confirmed skeletal muscle channelopathy
who underwent muscle biopsies to assess the vari-able combinations of proximal weakness, myalgia,and significantly elevated CK. All 3 biopsiesshowed inflammatory infiltrates. Each patientreceived long-term prednisone and various combi-nations of other immunosuppressive agents.
METHODS
All patients were referred to our national diagnosticservice for skeletal muscle channelopathies in theUK, funded by the Department of Health, NationalCommissioning Group (NCG). We confirmed agenetic diagnosis in each case. Each patient wasexamined personally by one of the investigators.The muscle biopsy pathology was reviewed by J.I.(cases 1 and 2) and J.L.H. (cases 2 and 3).
Genetic Analysis. We performed direct automatedDNA sequencing of all 23 exons of CLCN1 in thepatient with a diagnosis of myotonia congenita(case 2). For the patients with hyperkalemic peri-odic paralysis (case 1) and paramyotonia congenita(case 3) we performed sequencing of SCN4A hot-spots, exon 13 and a portion of exon 24 (c.4289–4524). All primers were tagged with M13 tails. SeeSupplementary Material for primer sequences.
PCR reactions to amplify each exon of CLCN1and SCN4A were performed using the followingreagents and conditions: a 25-ll reaction that con-tained 200 ng of genomic DNA; 2.5 ll of 10� poly-merase chain reaction (PCR) buffer without MgCl2(Applied Biosystems); 2 ll of 25 mM MgCl2; 2.5 llof 2 mM dNTPs; 10 pmol of each primer (forwardand reverse); and 2.5 units of polymerase (Ampli-Taq Gold; Applied Biosystems). Cycling conditionsconsisted of an initial denaturing step of 95�C for10 minutes followed by 30 cycles of 95�C for 30seconds, 58�C for 30 seconds (CLCN1) or 60�C for30 seconds (SCN4A), 72�C for 30 seconds, and afinal extension step of 72�C for 7 minutes.
Abbreviations: CK, creatine kinase; EMG, electromyography; MHC,major histocompatibility complex; MRI, magnetic resonance imaging;NCG, National Commissioning Group; PCR, polymerase chain reaction
Correspondence to: M.G. Hanna; e-mail: [email protected]
VC 2011 Wiley Periodicals, Inc.Published online 22 June 2011 in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/mus.22120
Key words: channelopathy; histopathology; myositis; neuromuscular;treatment
Channelopathies with Myositis MUSCLE & NERVE August 2011 283

Samples were sequenced (bidirectionally) usingan ABI Big Dye Terminator sequencing kit (ver-sion 1.1), M13 universal primers, and an auto-mated DNA sequencer (Model 3730xl; ABI). Datawere analyzed using SeqScape Analysis (version2.5) software (ABI).
Histopathology. Each patient had undergone musclebiopsy at another center, and tissue sections stainedfor hematoxylin and eosin (H&E), the Gomori tri-chrome method, lipid, and glycogen in addition toenzyme histochemical preparations for succinic dehy-drogenase, cytochrome oxidase, and nicotinamide ad-enine dinucleotide dehydrogenase tetrazolium reduc-tase were available for review. Immunohistochemicalpreparations available for review were as follows: case1, CD3 and major histocompatibility complex (MHC)class I; case 2, CD3, CD20, spectrin, dystrophin, mero-sin, dysferlin, sarcoglycans, emerin, and desmin; andcase 3, MHC class I, CD3, CD68, and CD20.
RESULTS
Case 1. An 80-year-old man complained of epi-sodes of muscle weakness after periods of pro-longed rest from the age of 4 years. Initially, onlythe lower limbs were affected, but by his late teensthe upper limbs were also involved. The episodesusually lasted hours and occasionally days. A clinicaldiagnosis of familial periodic paralysis was madewhen he was 21 years of age after reports of similarepisodes of weakness in his mother and sister.
From his early 50s, mild proximal muscle weak-ness was noted on examination. At 56 years ofage, following a positive potassium challenge, hisdiagnosis was revised to hyperkalemic periodicparalysis, and he was treated with salbutamol. CKat this time was noted to be 436 U/L. At age 65,he began complaining of progressive difficultiesover 12 months of rising from a low chair andclimbing stairs. Examination confirmed limb weak-ness that was greater proximally than distally. Clear
Table 1. Summary of clinical, biochemical, neurophysiological, and histological findings in each case.
CasePredominant
clinical featuresExaminationfindings Investigations Biopsy findings
Response to steroidtherapy
1 Episodic muscleparalysis.
Progressive proximallimb weakness
Proximal limbweakness,MRC grade3þ/5 to 4þ/5
CK 2729 U/L. EMG showspolyphasic units þ shortduration units, fibrillations,fasciculations, andmyotonic discharges.
Internal nuclei, fiber atrophy,fiber hypertrophy withoccasional split fibers,some regenerating fibersand an increase inendomysial connectivetissue. Dense inflammatorycell infiltrate focusedaround small capillariesand necrotic fiberscomposed mainly ofT lymphocytes.
High-dose prednisone(60 mg) led to severeparalytic attack lasting48 h. A 10-mg dosebetter toleratedwith improvedmuscle strength.
MHC I upregulation onoccasional muscle fibers.
2 Muscle crampsand severemyalgia.
Myotonia.Normal musclepower.
CK 1109 U/L. EMGshows massivemyotonic dischargesat every insertionpoint that precludedanalysis of MUAPconfiguration, voluntaryrecruitment orinterference pattern.
Increased variation in fibersize, evidence of fiberregeneration and 1 necroticfiber. Two foci ofinflammation composedof CD3 immunoreactiveT lymphocytes notedin perimysium andendomysium.
Reduction in CKto 300–400.
Immunohistochemistryunavailable for review.
3 Muscle crampsand episodiclimb edemawith myalgia.
Myotonia. Normalmuscle power.
CK normal. EMG showsmyotonic discharges.
Inflammatory infiltratescomposed of a mixtureof T lymphocytes andmacrophages were presentin the perimysium with asingle endomysial cluster(Fig. 2). Immunohistochemicalstaining for MHC Class Idemonstrated an increasein sarcolemmal andsarcoplasmic expression.
Excellent responsewith significantreduction insymptoms ofedema andmyalgia.
CK, creatine kinase; EMG, electromyography; MUAP, motor unit action potential; MHC, major histocompatibility complex.
284 Channelopathies with Myositis MUSCLE & NERVE August 2011

difficulty rising from a chair without using hishands for leverage was observed, and a degree ofthigh atrophy was noted. EMG showed polyphasicmotor unit potentials intermixed with some short-duration simple units and spontaneous activity,including fibrillation potentials, fasciculationpotentials, and myotonic discharges. His CK was2729 U/L. Muscle biopsy showed internal nuclei,fiber atrophy, fiber hypertrophy with occasionalsplit fibers, some regenerating fibers, and anincrease in endomysial connective tissue. In addi-tion, there was a dense inflammatory cell infiltratefocused around small capillaries and necroticfibers, which was demonstrated by immunohisto-chemistry to consist mainly of T lymphocytes.There was expression of MHC class I on occasionalskeletal muscle fibers. The biopsy findings andoverall clinical picture were consistent with a diag-nosis of polymyositis, and he was started on predni-sone 60 mg once daily. A few hours after the initialdose of steroids he had a severe attack of paralysislasting 48 hours. After recovery he was restarted onprednisone 10 mg once daily, with gradualimprovement of muscle weakness.
Ten years later he re-presented with furthercomplaints of leg weakness and difficulties in mo-bilization, which had progressed subacutely over a6-week period. At this time he was on 5 mg/dayprednisone, although it is not clear whether thishad been continuous since commencement 10years earlier. Azathioprine, 50 mg twice daily, wasadded to his therapy, but he continued to deterio-rate and was admitted to the hospital, where proxi-mal lower limb power was documented to rangefrom 3þ/5 to 4þ/5. The azathioprine dose was fur-ther increased to 100 mg twice daily, and he wasdischarged from the hospital. When he wasreviewed in the clinic 2 months later he reportedthat his mobility difficulties fluctuated in severityand self-postulated they were contributed to by hisperiodic paralysis. Improved proximal leg strengthwas recorded. Genetic analysis confirmed the pres-ence of the common T704M point mutation in theSCN4A gene associated with hyperkalemic periodicparalysis.14
Case 2. A 42-year-old woman complained of dailymuscle cramps from early childhood. This was con-firmed on EMG to be myotonia. The family historyrevealed similar symptoms in her mother and twomaternal aunts, and a clinical diagnosis of myoto-nia congenita was made. The patient complainedof severe cramps with increasing age, and shebegan to experience episodes of muscle weaknessafter exertion. Between episodes she reported nor-mal muscle power. Examination was generallyunremarkable, but CK level was found to be 1109
U/L. Muscle biopsy was performed and demon-strated increased variation in fiber size, evidence offiber regeneration, and one necrotic fiber. Foci ofinflammation composed of CD3-immunoreactive Tlymphocytes were noted in the perimysium andendomysium (Fig. 1A). Invasion of intact myofibersby T cells was not evident, and MHC class I immu-nohistochemistry was not available for review. Therewas no evidence of a vacuolar myopathy, and tubu-lar aggregates were not present. She was started onprednisone, and there was a resultant reduction inCK to 300–400 U/L. All attempts to reduce theprednisone dose were unsuccessful, and the patientwas unable to tolerate other immunosuppressants.Genetic sequencing confirmed presence of theF167L mutation in the CLCN1 gene associated withmyotonia congenita.15
Case 3. A 38-year-old man complained of epi-sodes of muscle stiffness when exposed to the coldthat affected predominantly his tongue, hands,and feet from early childhood. This was confirmedby EMG to be myotonia. There was no family his-tory of note. Myotonia occurred daily, but symp-toms remained fairly static until his late teens. Hethen noted episodes of acute muscle swelling pre-dominantly affecting his forearms and thighs. Ini-tially these were non-painful, and CK and musclepower were normal. Later, however, he com-plained of myalgia accompanying the episodes ofswelling, which occurred two or three times permonth and lasted up to 1 week. Examinationbetween episodes continued to demonstrate nor-mal muscle power. Ultrasound examination con-firmed hypoechoic regions within the muscles butnormal subcutaneous tissue. An intermittentperipheral eosinophilia was noted in conjunctionwith the episodes of myalgia. No specific cause forthe eosinophilia was identified. Magnetic resonanceimaging (MRI) scans of the lower limbs performedduring symptomatic episodes confirmed widespreadedema that was not present during asymptomaticperiods (Fig. 2). A muscle biopsy showed no evi-dence of regeneration, necrosis, vacuolation offibers, or tubular aggregates. Inflammatory infil-trates composed of a mixture of T lymphocytes andmacrophages were present in the perimysium,and there was a single endomysial cluster (Fig. 1Band C). Invasion of intact muscle fibers by T cellswas not apparent. Immunohistochemical stainingfor MHC class I demonstrated an increase in sarco-lemmal and sarcoplasmic expression (Fig. 1D). Thebiopsy findings were interpreted as being compati-ble with polymyositis, although the clinical historyand normal CK were not typical.
The patient had an excellent response to pred-nisone given at 20 mg on alternate days, which was
Channelopathies with Myositis MUSCLE & NERVE August 2011 285

reduced to 5 mg on alternate days. The frequencyand severity of muscle swelling and myalgia werereduced, although he unfortunately developedosteopenia. Attempts to introduce other steroid-sparing immunosuppressive agents were unsuccess-ful, as he did not respond to methotrexate, cyclo-sporine, imatinib, or hydroxyurea, and did not tol-erate azathioprine. Genetic analysis confirmed thepresence of the L1436P mutation in the SCN4Agene associated with sodium channel myotonia.5
Statistical Considerations. The prevalence rates ofboth skeletal muscle channelopathies and idio-pathic inflammatory myopathy have each been esti-mated to be 1 in 100,000.16–18 We initially took anull hypothesis that the development of both dis-eases in our 3 cases was coincidental. Consideredstatistically, if the likelihood of developing a skele-tal muscle channelopathy and an IIM is independ-ent, then the chance of having both is 1 in 10�10.The probability of observing UK patients with bothdiseases (if this association were by chance alone)can be calculated using the Poisson distribution,because P-value is small and the UK population is
large; Poisson lambda ¼ 10�10 (independent prob-ability of 2 events in an individual) � 6.5 � 106
(UK population) ¼ 0.0065, and the probability ofobserving 3 or more patients with both diseases(assuming independence) is 4.5 � 10�8. This smallP-value indicates that the occurrence of both dis-eases in the same individual is highly unlikely tobe independent.
DISCUSSION
The precise natural history of the skeletal musclechannelopathies has not been extensively docu-mented, but development of a proximal myopathyis recognized, especially in the periodic paralyses.It is unclear whether the myopathy is related tothe severity and frequency of paralytic attacks.6,19
There is some evidence that development of myop-athy may be associated with increasing age.6,20
In addition, moderately elevated CK (1000–2000U/L) and moderate to severe myalgia have beenreported in the skeletal muscle channelopathies,although there is no evidence to link these directlyto the presence of myopathy or to explain theirpathogenesis.
FIGURE 1. In case 2, a prominent focus of perimysial inflammation was found (A). Similarly, the inflammation in case 3 was predomi-
nantly perimysial (B) with focal extension into the perimysium [arrow in (C)]. The inflammatory cells included abundant T lymphocytes
(C) and increased expression of MHC class I at the sarcolemma and within the sarcoplasm of fibers (D). (A) Case 2. (B–D) Case 3.
(A, B) Hematoxylin and eosin stain; (C) CD3 immunohistochemistry; (D) MHC class I immunohistochemistry. Bar in (A) represents 50
lm in (A)–(D). [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
286 Channelopathies with Myositis MUSCLE & NERVE August 2011

A characteristic history in conjunction with spe-cialized neurophysiological techniques21 allows adiagnosis in the majority of cases of skeletal musclechannelopathy, and it is now rare when a musclebiopsy is performed in the UK.
In our 3 cases a clinical diagnosis of skeletalmuscle channelopathy had been made prior to themuscle biopsy and was later confirmed genetically.Biopsy was performed due to additional clinicalfeatures that were considered unusual or severe fora muscle channelopathy. In case 1 the proximalmyopathy could have been attributed to the myop-athy that is reported in periodic paralysis, but thevery high CK (2729 U/L) was considered to beatypical. The severe myalgia and moderate eleva-tion of CK (1109 U/L) reported in case 2 are alsodescribed features of the channelopathies, and wecannot exclude the possibility that at least some ofthe myalgia was due to myotonia. However, as themyalgia became severe enough to be the patient’sprimary complaint, a biopsy was performed. Theinitial complaint of muscle swelling in case 3 is nota typical feature of the muscle channelopathiesand, with the later development of significant my-algia, a biopsy was considered warranted. We sug-gest that the clinical features of weakness, myalgia,and significantly elevated CK in these 3 cases aresecondary, at least in part, to the observed inflam-matory process.
The biopsy findings in these cases do not fulfillall morphological criteria for IIM, particularly thelack of invasion of intact fibers. However, upregula-
tion of MHC class I expression (cases 1 and 3) issupportive, and it is not unreasonable that a diag-nosis of IIM had been made in these cases, espe-cially when each was considered in isolation. Thereare numerous examples of other genetic muscledisorders in which inflammatory infiltrates havebeen observed and even diagnosed as IIM.22 Wecannot exclude the possibility that the observedinflammatory process is a coincidental finding, andtwo independent pathologies (channelopathy andIIM) were present in each of the 3 individuals.This seems to be statistically unlikely.
It is not known whether this inflammatoryresponse plays a potential pathogenic role in thedevelopment of the myopathy. Morphology datahave been reported for the skeletal muscle channe-lopathies, especially the periodic paralyses, but inmany cases the findings pre-date the availability ofgenetic testing. The presence of vacuolar myopathyand/or tubular aggregates support the diagnosis ofperiodic paralysis. With improved electrophysiolog-ical and genetic diagnostic methods, muscle biopsyis now less common. Without a larger number ofbiopsy samples from similar cases it is not possibleto know how accurately inflammatory muscle infil-trates may correlate with the clinical presentation.
Although there was some improvement insymptoms and a reduction in CK with prednisonein 2 cases, in 1 case high-dose prednisone induceda severe paralytic attack, although low-dose steroidswere better tolerated. Worsening of the paralyticsymptoms of periodic paralysis with glucocorticoids
FIGURE 2. Short T1 inversion recovery (STIR) images of the calves (A) and thighs (B) of case 3, illustrating widespread edema during
a symptomatic period of myalgia and muscle swelling compared with normal imaging when asymptomatic.
Channelopathies with Myositis MUSCLE & NERVE August 2011 287

has been reported.23 Other immunosuppressiveagents had no clear additional benefit.
Based on our observations, we suggest that adiagnostic muscle biopsy should be considered incases of skeletal muscle channelopathy that presentwith the symptoms of severe myalgia and/or suba-cute weakness and an accompanying elevated CK(>1000 U/L) to ascertain the presence of anyinflammatory infiltrates. The therapeutic benefit ofimmunosuppressants has not been not established,but our cases indicate that steroids may have arole. The optimal dose is undetermined, andhigher doses may be detrimental such that cautionwith their use is recommended.
The statistical evidence indicates that the coex-istence of an inflammatory process and skeletalmuscle channelopathy is very unlikely to be purelycoincidental. The possible implications this mayhave for our understanding of the mechanisms ofmuscle damage in the skeletal muscle channelopa-thies remains to be explored.
The authors thank all of the clinical colleagues who referredpatients to our center, particularly Professor Charles Warlow. Thiswork was undertaken at University College London Hospitals/University College London, which received partial support fromthe funding scheme of the Department of Health’s National Insti-tute for Health Research Biomedical Research Centers. E.M. wasfunded by the Brain Research Trust and by the National Centerfor Research Resources (5U54 RR019498-05). M.G.H. receivedresearch funding from the Medical Research Council, MRCCentre (G0601943), Muscular Dystrophy Campaign Centre, andConsortium for Clinical Investigation of Neurological Channelo-pathies (NIH U45 RR198442-01). M.G.H. provides the UKnational patient referral center for skeletal muscle channelopa-thies, funded by the UK Department of Health National Commis-sioning Group. J.L.H. was supported by the Myositis SupportGroup.
REFERENCES
1. Becker PE. Myotonia congenita and syndromes associated with myo-tonia. Stuttgart: Thieme;1977.
2. Plassart E,Eymard B, Maurs L, Hauw JJ, Lyon-Caen O, Fardeau M,et al. Paramyotonia congenita: genotype to phenotype correlationsin two families and report of a new mutation in the sodium channelgene. J Neurol Sci 1996;142:126–133.
3. Nagamitsu S, Matsuura T, Khajavi M, Armstrong R, Gooch C, HaratiY, et al. A ‘‘dystrophic’’ variant of autosomal recessive myotonia
congenita caused by novel mutations in the CLCN1 gene. Neurology2000;55:1697–1703.
4. Miller TM, Dias da Silva MR, Miller HA, Kwiecinski H, Mendell JR,Tawil R, et al. Correlating phenotype and genotype in the periodicparalyses. Neurology 2004;63:1647–1655.
5. Matthews E, Tan SV, Fialho D, Sweeney MG, Sud R, Haworth A,et al. What causes paramyotonia in the United Kingdom? Commonand new SCN4A mutations revealed. Neurology 2008;70:50–53.
6. Links TP, Zwarts MJ, Wilmink JT, Molenaar WM, Oosterhuis HJ. Perma-nent muscle weakness in familial hypokalaemic periodic paralysis. Clini-cal, radiological and pathological aspects. Brain 1990;113:1873–1889.
7. Bradley WG, Taylor R, Rice DR, Hausmanowa-Petruzewicz I, Adel-man LS, Jenkison M, et al. Progressive myopathy in hyperkalemicperiodic paralysis. Arch Neurol 1990;47:1013–1017.
8. Vicart S, Sternberg D, Fournier E, Ochsner F, Laforet P, Kuntzer T,et al. New mutations of SCN4A cause a potassium-sensitive normoka-lemic periodic paralysis. Neurology 2004;63:2120–2127.
9. Rosenfeld J, Sloan-Brown K, George AL Jr. A novel muscle sodiumchannel mutation causes painful congenital myotonia. Ann Neurol1997;42:811–814.
10. Ptacek LJ, Tawil R, Griggs RC, Meola G, McManis P, Barohn RJ,et al. Sodium channel mutations in acetazolamide-responsive myoto-nia congenita, paramyotonia congenita, and hyperkalemic periodicparalysis. Neurology 1994;44:1500–1503.
11. Colding-Jorgensen E, Duno M, Vissing J. Autosomal dominant mono-symptomatic myotonia permanens. Neurology 2006;67:153–155.
12. Fialho D, Schorge S, Pucovska U, Davies NP, Labrum R, Haworth A,et al. Chloride channel myotonia: exon 8 hot-spot for dominant-negative interactions. Brain 2007;130:3265–3274.
13. Trip J, Drost G, Ginjaar HB, Nieman FH, van der Kooi AJ, de VisserM, et al. Redefining the clinical phenotypes of non-dystrophic myo-tonic syndromes. J Neurol Neurosurg Psychiatry 2009;80:647–652.
14. Ptacek LJ, George AL Jr, Griggs RC, Tawil R, Kallen RG, Barchi RL,et al. Identification of a mutation in the gene causing hyperkalemicperiodic paralysis. Cell 1991;67:1021–1027.
15. George AL Jr, Sloan-Brown K, Fenichel GM, Mitchell GA, Spiegel R,Pascuzzi RM. Nonsense and missense mutations of the muscle chlo-ride channel gene in patients with myotonia congenita. Hum MolGenet 1994;3:2071–2072.
16. Emery AE. Population frequencies of inherited neuromuscular dis-eases—a world survey. Neuromuscul Disord 1991;1:19–29.
17. Fontaine B. Primary periodic paralysis and muscle sodium channel.Adv Nephrol Necker Hosp 1994;23:191–197.
18. Hilton-Jones D. Inflammatory muscle diseases. Curr Opin Neurol2001;14:591–596.
19. Buruma OJ, Bots GT. Myopathy in familial hypokalaemic periodicparalysis independent of paralytic attacks. Acta Neurol Scand 1978;57:171–179.
20. Plassart E, Reboul J, Rime CS, Recan D, Millasseau P, Eymard B,et al. Mutations in the muscle sodium channel gene (SCN4A) in 13French families with hyperkalemic periodic paralysis and paramyoto-nia congenita: phenotype to genotype correlations and demonstra-tion of the predominance of two mutations. Eur J Hum Genet 1994;2:110–124.
21. Fournier E, Arzel M, Sternberg D, Vicart S, Laforet P, Eymard B,et al. Electromyography guides toward subgroups of mutations inmuscle channelopathies. Ann Neurol 2004;56:650–661.
22. Tidball JG, Wehling-Henricks M. Damage and inflammation in mus-cular dystrophy: potential implications and relationships with auto-immune myositis. Curr Opin Rheumatol 2005;17:707–713.
23. Arzel-Hezode M, McGoey S, Sternberg D, Vicart S, Eymard B, Fon-taine B. Glucocorticoids may trigger attacks in several types of peri-odic paralysis. Neuromuscul Disord 2009;19:217–219.
288 Channelopathies with Myositis MUSCLE & NERVE August 2011

BENEFICIAL EFFECT OF ALBUTEROL IN CONGENITAL MYASTHENICSYNDROME WITH EPSILON-SUBUNIT MUTATIONSMENACHEM SADEH, MD,1 XIN-MING SHEN,2 and ANDREW G. ENGEL, MD2
1Department of Neurology, Wolfson Medical Center, Holon and Tel Aviv University, Halochamin Street, Holon 58100, Israel2Department of Neurology and Neuromuscular Research Laboratory, Mayo Clinic, Rochester, Minnesota, USA
Accepted 25 April 2011
ABSTRACT: Mutations in the epsilon subunit of the acetylcholinereceptor (AChR) are a common cause of congenital myasthenicsyndrome (CMS). Patients are usually treated with acetylcholines-terase inhibitors and 3,4-diaminopyridine with modest clinical bene-fit. We report 2 patients with CMS due to mutations in the AChRepsilon subunit. The first patient carries two heterozygous frame-shift mutations, e127ins5 and e1293insG. The second patient ishomozygous for the eC142Y mutation that curtails AChR expres-sion to 22% of wild-type in HEK cells. Treatment with pyridostig-mine and 3,4-diaminopyridine had a limited beneficial effect in thefirst patient, and the second patient became wheelchair-bound dur-ing therapy. The additional use of albuterol produced dramaticimprovement in strength and in activities of daily living in bothpatients. The efficacy and safety of albuterol in patients who harboridentified low-expressor or null mutations in the epsilon or othersubunits of AChRmerits a well-designed clinical trial.
Muscle Nerve 44: 289–291, 2011
Mutations in the epsilon subunit of the acetyl-choline receptor (AChR) are the most commoncause of congenital myasthenic syndrome (CMS).1
The inheritance is recessive, except for mutationsthat cause slow-channel syndromes, and mostpatients are compound heterozygotes. Mutationsin the epsilon subunit may change the kineticproperties of the AChR channel or decrease AChRexpression. Changes in kinetic properties manifestas slow-channel or fast-channel syndromes. Theslow-channel syndromes respond to treatment withlong-lived open-channel blockers of the receptor,such as quinidine or fluoxetine. All other CMSpatients with mutations in the AChE epsilon subu-nit are treated with acetylcholinesterase (AChE)inhibitors and 3,4-diaminopyridine (3,4-DAP) withvariable results. Herein we describe an impressivebeneficial response to treatment with the b2-adre-nergic agonist albuterol in 2 patients with CMSdue to epsilon-subunit mutations.
CASE REPORTS
Patient 1. This 56-year-old woman was born inRomania and came to Israel in 1959. She is ateacher, is married, and has 4 children. Her
parents are not related, and there is no family
history of neurological disease. At the age of3–4 months the patient had a weak cry and diffi-culties in sucking. At the age of 9 months she hadbilateral ptosis. As a child, she had difficulty climb-ing stairs, lifting weights, or elevating her arms.During her pregnancies she felt well, but her weak-ness worsened after each delivery. Tests for anti-bodies against AChR were negative. Repetitivenerve stimulation (RNS) at 3 HZ showed a decre-mental response. She was diagnosed as havingCMS and was treated with pyridostigmine for manyyears with beneficial results. Seven years ago shehad a severe attack of asthma. She was admitted toanother hospital and was treated with high dosesof prednisone. After 2 weeks, her weaknessimproved significantly so that she was able to climbstairs, which she could not do before, and thediagnosis was changed to probable autoimmunemyasthenia gravis.
When seen at the Wolfson Medical Center in2005 she had bilateral, non-fatigable ptosis, limita-tion of gaze in all directions, and weakness of facialmuscles. Limb muscle weakness was symmetrical,and strength was [Medical Research Council (MRC)scale]: deltoid and triceps 4/5; biceps and infraspi-natus 4þ/5; and iliopsoas 1/5. There was minimalweakness of the quadriceps and adductors, and allother muscles were of normal strength. RNS of thetrapezius and abductor digiti minimi musclesshowed decremental responses of 25% and 11–16%,respectively. Treatment with prednisone and aza-thioprine was instituted. She improved markedlybut also became hirsute, edematous, and developeddermatophytosis. Prednisone treatment was gradu-ally stopped, but therapy with 250 mg/day azathio-prine was continued. Within a period of 2–3 monthsthe patient’s condition deteriorated. High-dose in-travenous immunoglobulin was not beneficial. Thefailure of immunomodulatory treatment againpointed to a CMS, and mutation analysis revealedtwo heterozygous frameshift mutations in the epsi-lon subunit of AChR, �127ins5 and �1293insG. Bothhave been reported previously.2,3
Treatment was started with 3,4-DAP at a dosethat was gradually increased to 7.5 mg six timesdaily, and pyridostigmine 60 mg six times daily wascontinued. Under this treatment there was a mod-est improvement. If she took an extra 10-mg doseof 3,4-DAP she could take short walks at her home
Abbreviations: AChE, acetylcholine esterase; AChR, acetylcholine recep-tor; CMS, congenital myasthenic syndrome; DAP, diaminopyridine; HEK,human embryonic kidney; MRC, Medical Research Council; RNS,
Correspondence to: M. Sadeh; e-mail: [email protected]
VC 2011 Wiley Periodicals, Inc.Published online 15 July 2011 in Wiley Online Library (wileyonlinelibrary.com). DOI 10.1002/mus.22153
Key words: congenital myasthenic syndrome, acetylcholine receptor,epsilon subunit, albuterol, 3,4-diaminopyridine, ephedrine
CMS and Albuterol MUSCLE & NERVE August 2011 289

for over 30 minutes. On examination, she hadophthalmoplegia with mild bilateral ptosis, mild tomoderate weakness (4/5 on the MRC scale) offacial and proximal arm muscle, and there wassevere weakness of the iliopsoas muscles (1/5 onthe MRC scale).
Treatment with albuterol sulfate, 2 mg threetimes daily, was added. Within a few weeks herstrength improved dramatically. She rose easilyfrom sitting and could walk 2 km without becom-ing tired. Examination now only showed slightweakness of the deltoid muscles, and the iliopsoasmuscles were 4/5 on the MRC scale. There was nochange in the ophthalmoplegia or facial weakness.All other muscles had normal strength. There was nochange in muscle strength during 1 year of follow-up.
Patient 2. This 35-year-old woman had general-ized weakness from the age of 3 months. She weptsilently and had bilateral ptosis; however, shegained motor mile-stones on time. Her parents arefirst cousins. A son of her mother’s brother is simi-larly affected. As a child she had difficulty walking,episodes of shortness of breath, and required hos-pitalization repeatedly for recurrent pneumonia.She was examined in another hospital, underwentelectrophysiological studies, and was diagnosedwith seronegative myasthenia gravis. Therapy withprednisone 60 mg/day for 4 months was of nobenefit and was gradually tapered. At the age of 16years she underwent thymectomy. Her conditionworsened, and the diagnosis was reconsidered at26 years of age. A muscle biopsy to rule out myop-athy only revealed scattered small muscle fibers,some angulated. She had surgery for correction ofptosis. She could barely rise from sitting and couldwalk only a few steps unaided. She was wheelchair-bound by the age of 28 years. Because of severeupper arm weakness she could not dress or washherself or shower.
On examination, she had complete ophthalmo-plegia with mild ptosis and moderate weakness ofthe facial muscles. Neck flexors and extensors wereweak (4/5 on the MRC scale). She had severeweakness of proximal limb muscles: deltoids 3/5;biceps and triceps 4/5; iliopsoas 2/5; and quadri-ceps, adductors, and glutei 3/5. There was onlyvery mild distal muscle weakness. She could notrise from sitting without help.
3-HZ stimulation of the trapezius muscleshowed a decremental response of 25% without adouble response to single stimuli. AChR antibodieswere not detected. Sequencing of the AChR subu-nits revealed a homozygous eC142Y mutation. Thismutation involves the cysteine of the signature cys-loop. Expression of genetically engineered�C142Y–AChR in human embryonic kidney (HEK)
cells by established methods2 revealed its expres-sion was reduced to 22% compared with wild-type.Subsequently, the patient was treated with pyridos-tigmine and 3,4-DAP with only mild beneficialeffects. She was repeatedly hospitalized because ofrecurrent pneumonia episodes.
In 2010, treatment with albuterol at 2 mg threetimes a day was instituted and resulted in markedimprovement within several weeks. The patientnow raised her arms well, rose from sittingunaided, and walked unsupported. Examinationrevealed ophthalmoplegia with mild ptosis, onlymild weakness of facial muscles, and 4/5 strengthof the deltoid and iliopsoas muscles. All othermuscles were of normal strength. Her strengthremained stable, and she did not have recurrenceof pneumonia during 6 months of follow-up.
DISCUSSION
Albuterol is an essentially exclusive b2-adrenergicagonist. Its main use is in treating bronchospasm byrelaxing airway smooth muscles and is used mostlywith inhalers. Ephedrine, another sympathomimeticagent acting on both a- and b-adrenergic receptors,is also used for treating bronchospasm.
Ephedrine previously was also used for sympto-matic treatment of myasthenia gravis,4 but its usewas abandoned because it was not sufficientlyeffective.5 In the past decade, ephedrine was foundto be beneficial in CMS due to AChE deficiency6
and in Dok-7 myasthenia.7 A favorable response toephedrine was also observed in a case of Lambert–Eaton syndrome.8
The mechanism of action of ephedrine on theneuromuscular junction is not fully understood. Invitro studies9 revealed that it increases quantalrelease and reduces the conductance of the AChRchannel, but only in doses that cannot be attainedin clinical practice. A subsequent single-channelpatch-clamp study10 revealed that ephedrine aswell as albuterol increased the number of briefintraburst closures causing an open-channel block-ade of AChR, but again in doses that cannot beused in clinical practice. In an a-bungarotoxin–induced model of myasthenia gravis in rats, ephed-rine caused some improvement, but this was attrib-uted to a difference in susceptibility to arousal.11
The mechanism by which ephedrine improves theCMS caused by AChE deficiency and Dok-7 myas-thenia remains unknown.
We preferred to use albuterol instead of ephed-rine in our patients because it has fewer adverseeffects and is readily available. The possibleadverse effects of albuterol include tremor, nerv-ousness, arrhythmias, hypertension, and myocardialischemia. Therefore, as long as patients are takingalbuterol they must be carefully monitored for
290 CMS and Albuterol MUSCLE & NERVE August 2011

adverse effects. Our 2 patients reported no adverseeffects over periods of 12 and 6 months, respectively.
Albuterol has been added to treatment withpyridostigmine and 3,4-DAP. It may be less effectiveas a solemedication.However, our observationsindicate that CMS with epsilon-subunit mutationsrespond to albuterol therapy. This informationshould prompt a larger clinical trial to determineits efficacy and safety in patients who harbor low-expressor mutations in the epsilon or other sub-units of AChR. The use of albuterol as a substitutefor ephedrine in AChE deficiency and Dok-7 CMSawaits investigation.
This study was supported in part by a grant from the National Insti-tutes of Health (N26277) and a research grant from the MuscularDystrophy Association (to A.G.E.).
REFERENCES
1. Engel AG, Ohno K, Sine SM. Congenital myasthenic syndromes: pro-gress over the past decade. Muscle Nerve 2003;27:4–25.
2. Ohno K, Quiram PA, Milone M, Wang HL, Harper MC, Pruitt JN II,et al. Congenital myasthenic syndromes due to heteroallelic non-
sense/missense mutations in the acetylcholine receptor epsilon sub-unit gene: identification and functional characterization of six newmutations. Hum Mol Genet 1997;6:753–766.
3. Sieb JP, Kraner S, Schrank B, Reitter B, Goebel TH, Tzartos SJ, et al.Severe congenital myasthenic syndrome due to homozygosity of the1293insG epsilon-acetylcholine receptor subunit mutation. Ann Neu-rol 2000;48:379–383.
4. Edgeworth, H. The effect of ephedrine in the treatment of myasthe-nia gravis: second report. J Am Med 1933;100:1401.
5. Patten BM. Myasthenia gravis: review of diagnosis and management.Muscle Nerve 1978;1:190–205.
6. Bestue-Cardiel M, Saenz de Cabezon-Alvarez A, Capablo-Liesa JL,Lopez-Pison J, Pena-Segura JL, Martin-Martinez J, et al. Congenitalendplate acetylcholinesterase deficiency responsive to ephedrine.Neurology 2005;65:144–146,
7. Palace J, Lashley D, Newsom-Davis J, Cossins J, Maxwell S, KennettR, et al. Clinical features of the DOK7 neuromuscular junctionsynaptopathy. Brain 2007;130:1507–1515.
8. Cereda C, Kuntzer T. The potential use of ephedrine in Lambert–Eaton myasthenic syndrome. Clinical and electrophysiological evalua-tion. J Neurol 2008;255:1259–1260.
9. Sieb JP, Engel AG. Ephedrine: effects on neuromuscular transmis-sion. Brain Res 1993;623:167–171.
10. Milone M, Engel AG. Block of the endplate acetylcholine receptorchannel by the sympathomimetic agents ephedrine, pseudoephe-drine, and albuterol. Brain Res 1996;740:346–352.
11. Molenaar PC, Biewenga JE, van Kempen GT, De Priester JA. Effectof ephedrine on muscle weakness in a model of myasthenia gravis inrats. Neuropharmacology 1993;32:373–376.
CMS and Albuterol MUSCLE & NERVE August 2011 291