Sleep and Wake Disorders Following Traumatic Brain Injury ... · and sleep. Regardless of injury...
Transcript of Sleep and Wake Disorders Following Traumatic Brain Injury ... · and sleep. Regardless of injury...

317Volume 21 Numbers 3-4
Critical Reviews™ in Physical and Rehabilitation Medicine, 21(3-4): 317-374 (2009)
0896-2960/09/$35.00© 2009 by Begell House, Inc.
Sleep and Wake Disorders Following Traumatic Brain Injury: A Systematic Review of the Literature
Catherine Wiseman-Hakes,1* Angela Colantonio,2,3 and Judith Gargaro2
1Graduate Department of Rehabilitation Science, University of Toronto; 2Department of Occupational Therapy and Occupational Science, University of Toronto; 3Toronto Rehabilitation Institute, Toronto, Ontario, Canada
* Address all correspondence to Catherine Wiseman-Hakes, Graduate Department of Rehabilitation Science, Faculty of Medicine, University of Toronto, 160-500 University Ave.Toronto, ON, M5G 1V7, Canada; Tel.: 416-946-8575; Fax. 416-946-8570; [email protected]
ABSTRACT: Traumatic brain injury is a leading cause of death and disability in both Canada and the United States. Disorders of sleep and wakefulness are among the most commonly reported sequelae postinjury, across all levels of severity. Despite this, sleep and wakefulness are neither routinely, nor systematically, assessed and are only recently beginning to receive more clinical and scientific attention. Objectives: This review aims to systematically appraise the literature regarding sleep and wake disorders associated with traumatic brain injury according to the following domains: epidemiology, pathophysiology, neuropsychological implications, and inter-vention; to summarize the best evidence with a goal of knowledge translation to clinical practice; and to provide recommendations as to how the field can best be advanced in the most scientifically rigorous manner. Methods: Systematic review and rating of the quality of evidence. Results: Forty-three articles were reviewed for levels and quality of evidence. Fifty-six percent of the literature was classified as Level III, and 24 percent were Level IVA. Overall, 89 percent of the studies were rated as moderate quality. A separate summary was provided for the pediatric literature. Conclusions: A comprehensive review of the emerging literature revealed wide ranges in estimates for incidence and prevalence of sleep disorders following TBI depending on characteristics of patients, measures used, and length of follow-up. Few treatments have been found to be effective, and as such more research is recommended. Our overview of the pediatric literature shows that this is an important issue for survivors of all ages. Overall, further work is needed to fully understand this complex disorder and to identify appropriate and timely interventions.
KEY WORDS: traumatic brain injury, mild traumatic brain injury, sport-related concussion, sleep, sleep disorders, insomnia, hypersomnia, excessive somnolescence, treatment
I. BACKGROUND AND INTRODUCTION
A. Overview and Objectives
Traumatic brain injury (TBI), defined as an ac-quired nondegenerative, noncongenital insult to the brain from an external mechanical force, is a leading cause of death and disability in both Canada and the United States for both adults and children.1 Furthermore, although the literature re-
viewed in this paper is truly international in scope, at this time in the United States, “the nature of modern tactical engagement…in the current Iraq and Afghanistan conflicts has resulted in the largest proportion of identified traumatic brain injuries in any conflict in the nation’s history.” 2(p. 1004) In fact, the US Department of Defense reported an incidence of 10,963 diagnosed conflict-related TBIs in the year 2000. However, this incidence was reported as 27,862 by December 31, 2009,

318 Critical Reviews™ in Physical and Rehabilitation Medicine
which represents an increase of 145%.3 TBI can result in significant impairments in physical, neurocognitive, and psychosocial/emotional func-tion, as well as impairments in communication and sleep. Regardless of injury severity, these impairments may be transient or permanent, re-sulting in profound disruption for survivors and their families.
Disorders of sleep and wakefulness are among the most commonly reported sequelae postinjury, across all levels of severity.4,5 Despite this, sleep and wakefulness are neither routinely, nor system-atically, assessed postinjury, and are only recently beginning to receive more clinical and scientific attention. Previous reviews by Ouellet and col-leagues,6 Orff and colleagues,7 and most recently by Zeitzer and colleagues8 indicate that the field is still in a developmental stage and a body of literature is beginning to emerge. These previous reviews focused primarily on the prevalence and nature of sleep disorders and, to a lesser extent, on implications and effective treatment strategies among adult TBI survivors.
As of yet, there has been no systematic ap-praisal of the literature, nor has there been a review that has included literature pertaining to a pediatric population. The literature on pediatrics is of particular relevance given the fact that ap-proximately 500,000 children aged younger than 17 years are hospitalized each year with TBIs in the United States.9,10 This statistic does not include those children with minor TBIs who were either seen by their family physician/pediatrician or remained undiagnosed. Furthermore, TBI is the leading cause of disability in those under the age of 24 years, and the peak age of occurrence for TBI is 15–24 years.11 Thus, the unique con-tributions of this paper are: 1) to systematically update and extend previous reviews on sleep and brain injury6–8 by conducting a thorough critical appraisal of the methodological quality of the lit-erature that includes both children and adults and then, based on the identified strengths, weaknesses, and inconsistencies in the current literature; 2) to summarize the best evidence that currently exists with a goal of translating knowledge to clinical practice; and 3) to provide specific recommenda-tions as to how the field can best be advanced in the most scientifically rigorous manner, given the unique complexities of this disorder.
In summary, the objectives of this review are to systematically appraise the literature regarding sleep and wake disorders associated with TBI according to the following domains: epidemiol-ogy (including sports-related concussion), patho-physiology, neuropsychological implications, and intervention. Furthermore, we will identify practice points and provide recommendations for a research agenda, based on the current body of literature.
In order to provide readers with a clearer understanding of the importance of sleep (and wakefulness) in the rehabilitation and recovery process, we begin with a brief definition of sleep and an overview of the role and functions of sleep.
B. Definition of Sleep and Its Functions
To fully grasp the significance of the impact of sleep disturbances postinjury, it is important to have a clear understanding of the actual definition of sleep and the critical roles and function it plays in human (and animal) physiology and homeostatic regulation. In 1995, Tobler12 defined sleep as a physiological, complex, and integrated behavior characterized by a significant reduction of the response to external stimuli, by a characteristic posture usually in a special environment, by a characteristic change in the neurophysiological recordings of brain activity, and by a homeostatic increase after its restriction. Sleep is a critical function that serves to reverse and/or restore biochemical and/or physiological processes that are progressively degraded during prior periods of wakefulness.
Sleep is believed to be essential for optimal immune function by influencing cellular (T-cell) immunity. Furthermore, an increase in growth hormone secretion is observed immediately fol-lowing sleep onset, concurrently with a rise in cortisol in the latter half of sleep. This is critical for growth and development and is also important from the perspective of recovery from trauma, because not only does human growth hormone stimulate growth and cell reproduction, it also plays a critical role in cell regeneration. Further-more, cortisol plays a crucial role in facilitating the body’s adaptation to physical and mental stress, in the suppression of inflammation, enhancement

319Volume 21 Numbers 3-4
of wound healing, modulation of plasma glucose, and increased production of erythrocytes (red blood cells).13
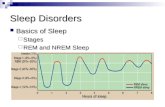
Sleep is divided into non-REM (rapid eye movement) and REM sleep. Studies of non-REM and REM sleep and the importance of their temporal succession in both animals and humans reveal that these stages have been found to play key roles in certain types of memory and learning, as well as cerebral plasticity.14–16 REM sleep, which occurs at the end of each sleep cycle, and the overall length of the REM cycle peaks prior to wakening also play a key role in aspects of memory consolidation and new learn-ing. Furthermore, REM sleep during the neonatal period plays an important role in brain growth, neuronal maturation, connectivity, and synaptic plasticity in infants.17 Thus, recognition of the critical role that sleep plays in endocrine and immune function, thermoregulation, cognition, and behavior underscores the need to evaluate and optimize sleep during recovery from brain injury.
II. METHODOLOGY
An extensive and iterative literature search was conducted using the Ovid, Medline, PsychInfo, CINAHL, and EMBASE databases to ensure the capture of any relevant studies pertaining to the assessment of sleep after TBI. Medical subject heading terms included: brain injuries or brain concussion or brain hemorrhage, traumatic or brain injury, chronic or diffuse axonal injury/sleep disorders/insomnia, and hypersomnia. The search was limited to articles published in English from 1998–2009. Only peer-reviewed full-text articles were considered for this study.
The search was initially exhaustive to include titles relating to both acquired brain injury and TBI, as the terms are sometimes used synonymously. This allowed us to ensure that we captured all relevant studies. Each article abstract was then reviewed to further ensure relevance. Additional search strategies were also employed and as such, the reference lists of all articles were scanned for additional studies that may be relevant for review. Because the literature on the relationship between sleep disturbances and TBI is still developing,
our inclusion criteria were quite broad and all identified articles were reviewed.
We then subdivided the articles into five different domains of scientific inquiry, including epidemiology, pathophysiology, pediatrics, in-tervention, and neuropsychological implications. Because there are a limited number of articles in the different subcategories of focus, all identified articles from Level II to Level V were included. In all, 68 articles were evaluated and 43 articles were included for the purposes of this review. We excluded only those that we deemed to be opinion papers or consensus papers not based on the results of a specific scientific study.
To critically appraise and stratify the quality of the evidence, the articles were evaluated on their research design and scientific rigor. Although it was not our intention to conduct a meta-analysis such as those undertaken by the Cochrane Collabo-ration Group, the ranking criteria were selected from the literature on evidence-based practice in rehabilitation, with a goal of providing guidance to end users about the studies likely to be most valid. Thus, the articles were categorized ac-cording to the scientifically validated hierarchy developed by Holm and edited by Boschen and colleagues (Table 1).18,19 Other rating systems are available;20–22 however, the Holm hierarchy18,19 was chosen in order to better differentiate among the published studies that exist at this point in the development of the literature on sleep and TBI. Given the early stage of development and the inherent complexities of the field, few randomized control trials (RCTs) have been conducted. It is, therefore, necessary to use a hierarchy that gives weight to non-RCT designs and also has a place for well-designed qualitative studies. Although the Holm hierarchy is an appropriate choice, it still did not fully differentiate the literature for our purposes. Thus, the edited and published version used by Boschen and colleagues19 was used for this systematic review.
Boschen and colleagues added two additional levels to the Holm hierarchy: the first is Level IIA, which was added to evaluate review papers that did not meet the criteria for Level I as they included non-RCT designs, and the second is Level IVA, which was added to separate out the well-designed non-experimental research designs such as cost analyses and the qualitative designs

320 Critical Reviews™ in Physical and Rehabilitation Medicine
from the purely opinion and descriptive studies classified as Level V articles.
To fully capture the literature in its current state of evolution, we also considered review articles of multiple well-designed studies (called Level I and Level IIA studies in this hierarchy) in our article inclusion criteria. These review articles were considered separately from the single-study articles because they gave us a better perspective of the historical development of research in the field of sleep and TBI. Single studies were clas-sified into levels based on the extent to which they met the criteria of the individual designated levels within this published hierarchy.
The process of assigning articles to levels was completed independently by two of the authors. Discrepancies were discussed and consensus was reached. Articles categorized as Level I or Level IIA were read and summarized but were not criti-cally reviewed, as they were review articles in and of themselves. Published hierarchies do exist for the evaluation of systematic reviews; however, because none of the review articles identified for this systematic review were systematic in nature, these hierarchies were not applicable.
Each of the articles was evaluated using a template generated for use in this study. The templates addressed the purpose, study design, sample, outcome measures, significant findings, relevant conclusions, and comments made by the authors of the articles, as well as any special notes from the article reviewers. Two of the authors and an undergraduate student completed the templates for the articles.
In order to critically appraise the quality of the articles, information was abstracted from the tem-plates in regard to the following seven questions:
1. Were baseline characteristics described and equivalence of groups evaluated?
2. Was the intervention/methodology de-scribed in detail, that is, sufficient for replication?
3. Was blinding employed?4. What was the sample size per group used
for data analysis?5. What was the attrition rate?6. Were the outcome measures used for the
study standardized?7. Was there a follow-up data collection
point?
TABLE 1Total Number of Articles Retrieved by Level of Evidence
Level of Evidence No. of Articles
Article Type
Level Ia 0 Systematic reviews of randomized controlled trials (RCTs)Level II 2 Properly designed individual RCTs of appropriate size
Level IIAb 2 Systematic reviews of case-controlled, cohort, or other experimental de-signs (including RCTs reviewed together with other experimental designs)
Level III 25Well-designed trials without randomization, single group pre-post, cohort, time series, or matched case-controlled studies (also cross-sectional stud-ies and case series)
Level IV 0 Well-designed non-experimental studies from more than one center or research group
Level IVAb 10 Well-designed individual non-experimental studies, cost analysis studies, and case studies
Level V 6 Reports of expert committees, descriptive studies, clinical observations, opinions of respected authorities, or testimonialsTotal
Total Reviewed 45
aBased on Holm.18
bAdapted from Boschen and colleagues19 to further differentiate the evidence.

321Volume 21 Numbers 3-4
This latter question was added specifically for the purposes of this review. The authors attempted to assess whether the intervention/methodology was described in sufficient detail to allow for understanding of the key elements and to allow for replication. These items were identified based on the items used in meta-analytic and other systematic reviews.23 The presence of the above-listed seven quality elements and their description in the articles was further rated on a three-point scale developed by Boschen and colleagues19 (Table 2). The classification of the quality rating - the sum of the scores of each of the six elements - was made using a trichotomous scheme representing “low” (summed score of <3), “moderate” (summed score of ≥3 and <5), and “high” (summed score ≥5) quality determined by the developers, based on the previous work of Boschen and colleagues. The abstraction and rating were performed independently by two of the authors and discrepancies were discussed and consensus was reached.
In addition, the articles on intervention were assigned a rating using the Downs and Black Rating System.20 As the Downs and Black system is widely known and accepted, we attempted to use this for the evaluation of all of the articles included. However, although it is an excellent
tool for the assessment of the quality of evidence specific to intervention studies, we encountered a number of difficulties in applying it to the nonin-tervention studies reviewed in this article. Thus, the Downs and Black System was applied only to the intervention studies. The use of these two quality assessment methodologies for the interven-tion studies allowed for comparison and a more thorough description of the literature.
III. RESULTS
A. Previous Reviews of Sleep Disorders and Insomnia Following TBI: A Historical Overview of the Literature to Date
To date, three reviews of the literature pertain-ing to sleep and/or insomnia following TBI have been published (Ouellet and colleagues,6 Orff and colleagues,7 and Zeitzer and colleagues8). The thorough Ouellet review,6 which we consider to be Level IIA, was the first to be conducted on the topic of sleep disturbance following TBI. This review made a number of important contributions to our understanding of the early adult literature on this complex topic. The authors aimed to re-
TABLE 2Criteria Used to Assess the Quality of the Studies
Rating of Assessed Characteristic
Baseline Characteristics: Described, “Equivalence”
Blinding Sample Size (per group)
Attrition Standardized Outcomes
Description of Intervention
Length of Follow-Up
1 Both elements present in the article
Double >75 <15% All Sufficient to replicate
>3 months
0.5 Either charac-teristics were described or equivalence was noted, but not both
Single 30-75 15-25% Some Some de-scription
0-3 months
0 Neither presented
No blind-ing or not stated
<30 >25% None No sufficient description
None

322 Critical Reviews™ in Physical and Rehabilitation Medicine
view the evidence on epidemiology, etiology, and treatment of insomnia in the context of TBI, and to propose areas for future research.
With regard to the early literature on preva-lence, Ouellet and colleagues6 reviewed nine studies and concluded that there were significant methodological issues in many of them, including the lack of an operational definition of insomnia, and heterogenous approaches (lack of consistency) to the assessment measures used to evaluate the presence and clinical significance of the insom-nia. Furthermore, they identified that most of the studies varied in terms of the time of evaluation postinjury and the level of severity of the brain injury, making it difficult to draw any specific conclusions regarding prevalence.
Among the studies reviewed by Ouellet and colleagues, they identified a range of reported symptoms of insomnia from 30–70% in patients with TBI, with symptoms of poor sleep initia-tion and maintenance being the most prevalent.6 They also noted a range of time postinjury that symptoms (of insomnia) were present from 6–12 weeks postinjury up to several years. This was an important conclusion/observation because Ouellet and colleagues identified that “insomnia appears to develop a chronic course in a significant pro-portion of TBI patients.”6(p. 188)
In addition, Ouellet and colleagues also iden-tified a number of potential etiological factors that may be associated with the development of insomnia following TBI, including predisposing, precipitating, and perpetuating factors.6 Finally, they reviewed the literature on potential psycho-logical and behavioral consequences of insomnia, and summarized the few studies on intervention, including pharmacotherapy and psychotherapies. The authors concluded the article with some basic practical recommendations based on the literature to date. They felt comfortable conclud-ing that insomnia is a common problem after TBI, the etiology and maintenance of which is complicated. They further concluded that the presence of insomnia in patients with TBI likely has detrimental consequences; however, more research is needed to identify effective treatments. They suggested that because insomnia can be chronic, combinations of pharmacological and psychological treatment options should possibly be used. Data collected from non-TBI patients
suggest that cognitive behavioral therapy (CBT) has promise.
In 2009, Orff and colleagues7 conducted an in-depth review of the literature, which we also identified as being Level IIA. This review, which builds on the previous work by Ouellet and colleagues,6 included a clearly defined search strategy, key search terms, and methodology. This review aimed to address “the etiology and implications of sleep problems in TBI, particu-larly mild TBI (mTBI), across 4 general domains of current scientific inquiry and observation: subjective impressions of poor sleep; objective changes in sleep-related parameters; alterations in circadian rhythms; and neurophysiologic and/or neuropsychologic abnormalities associated with TBI.”7(p. 155)
In the five years since the Ouellet review, the prevalence of sleep disturbances following TBI (both subjectively reported and objectively measured, although the latter has some contrary findings) has been further established, and the literature has thus evolved to more closely look at this complex disorder. With regard to subjective impressions of poor sleep, Orff and colleagues7 identified that the majority of studies surveyed had reasonably large sample sizes and provided replicable findings of insomnia in TBI patients, particularly those with mild TBI (mTBI). Results of the studies surveyed on the topic of objective changes in sleep parameters were not quite so conclusive. The authors identified several studies with objective evidence of changes in sleep quan-tity and quality, as well as other sleep disorders such as obstructive sleep apnea (OSA), periodic limb movements (PLM), and narcolepsy. How-ever, they also cited a number of studies in which objective changes in sleep parameters were not found, despite subjective complaints of the sub-jects. The authors cited similar methodological concerns as those previously addressed by Ouellet and colleagues, and further cited the lack of, or inconsistent reporting on, other important factors such as prior TBIs and past/current medical and psychiatric status, “making it difficult to evalu-ate the role of these variables in sleep-related outcomes and complicating comparisons between studies.”7(p. 163)
Orff and colleagues7 reviewed the literature on TBI and circadian changes, and reported that

323Volume 21 Numbers 3-4
although the literature is relatively sparse and somewhat conflicting at this time, there is a grow-ing body of evidence to suggest that sleep distur-bances following TBI may be due to alteration in the timing and rhythms of sleep (i.e., circadian rhythm sleep disorders) in a subset of patients. In addition, they reviewed the literature on neuro-physiologic and neuropsychological disturbances associated with sleep. They reported endocrine changes that may explain sleep disturbances in this population and also highlighted the limited but important research that suggests that deficits in cognitive performance after TBI may be related, in part, to the degree of sleep disturbance.
Consistent with the Ouellet review, Orff and colleagues also summarized the literature on interventions to date, which remains limited to a few studies addressing pharmacotherapy and CBT. Finally, they discussed limitations of the literature and identified that although the body of work has grown since the Ouellet review in 2004,6 there remain similar methodological limitations such as small sample sizes, considerable variation in age, time since injury, level of severity, and measures used to assess sleep. Orff and colleagues recommend that future research needs to focus on uncovering the specific types, causes, and severity of TBI that most often lead to sleep problems; the consequences of sleep disturbance; and the most effective treatment strategies.
The final review studied for this article is by Zeitzer and colleagues.8 This review, which we identified as being a Level V and lacking the methodological strength of the previous two reviews, was conducted for the US Department of Veterans Affairs (VA). As such, its focus seems to consider insomnia in the context of TBI from the perspective of those assessing and treating veterans diagnosed with mTBI, hampered by a co-morbid sleep disorder. (Note: Sleep apnea may in fact be preexisting because it is, interestingly, present in about half of the Department of VA patient population8[p. 829]). This review lacks a clearly defined objective and systematic review approach; however, the authors state that they will “consider insomnia directly caused by TBI (e.g., secondary to neural damage), indirectly caused by TBI (e.g., secondary to depression), and un-related to TBI but occurring within individuals with TBI.”8(p. 827)
Consistent with previous reviews, Zeitzer and colleagues cited studies of TBI populations of varying severities (mild-moderate) and vary-ing lengths of time postinjury from 6 weeks to greater than 10 years. They reported that insomnia occurs in approximately 40% of individuals with a TBI of any severity, even though it is more com-monly reported among patients with mTBI, and is the most prevalent somatic complaint across all levels of severity. The authors also postulated two components of TBI-related insomnia. First, there is a general predisposition to develop sleep disturbance as a result of alterations or disruptions in neurotransmitters involved in the regulation of sleep (and they state further that the litera-ture on this topic is for the most part limited to those with moderate-severe TBI). Second, acute stressors may trigger insomnia. They highlighted non-sleep comorbidities such as depression, pain and post traumatic stress disorder, all of which are of particular relevance to individuals with TBI in general and to veterans with mTBI. From this discussion, they highlighted two future research questions. First, can mTBI cause disruptions in the regulation of sleep? The authors stated further that the literature on this topic is, for the most part, limited to those with moderate-severe TBI. Second, can acute stressors trigger the insomnia? They highlighted non-sleep comorbidities such as depression, pain, and posttraumatic stress dis-order, all of which are of particular relevance to individuals with TBI in general and to veterans with mTBIs. They also identified two additional research questions: Can mTBI cause disruptions in the neurotransmitters critical for sleep and wakefulness?; and, What is the effect of psychi-atric comorbidities on the occurrence or severity of insomnia in the context of TBI? The latter question aims to assist the physician in treating insomnia as a primary or secondary pathology.
Finally, Zeitzer and colleagues8 briefly sum-marized the literature on pharmacological and non-pharmacological treatments. As per the previous two reviews, the literature on treatment remains limited. As a result, these authors identified some cautionary caveats in the use of pharmacotherapy and described nonpharmacological interventions such as CBT plus various combinations of sleep hygiene, sleep restriction, and relaxation training. The authors highlighted the critical need for further

324 Critical Reviews™ in Physical and Rehabilitation Medicine
nonpharmacological studies as viable alternatives to treatment of insomnia in patients with mTBI. The authors concluded that more systematic re-search is required to “provide a foundation for an evidence-based medical approach to treatment of insomnia in the context of mTBI.”8(p. 832)
B. Single Study Papers
As shown in Table 1, the majority of the literature (56%) is classified as Level III (Well-designed tri-als without randomization, single group pre-post, cohort, time series, or matched case-controlled studies [also cross-sectional studies and case se-ries]). The next largest level is Level IVA, with 24% of the categorized articles (well-designed individual non-experimental studies, cost analysis studies, and case studies). The published literature is getting stronger as there are fewer Level V studies than Level III or IVA studies, but is still clearly in development as there are no Level I studies and few Level II or IIA studies.
Single study papers were organized into the following categories: epidemiology (comparison group studies or single group/cohort studies), pathophysiology, pediatrics, neuropsychology, and intervention (see Tables 3, 4, and 5). It is important to note that there are Level III studies in each of the above categories, but as of yet the Level II
studies are only with regard to pharmacological interventions. Only one of the studies reviewed was considered of low quality, the majority were of moderate quality (89%), and only a few were of high quality (10%). Each of the studies is summarized in detail in Table 5, which lists the level, quality, and key details relating to the conduction of the reported study. Each category of studies will be discussed below in the order in which they appear in the table. Following each summary there will be an in-text box summarizing the research agenda and practice points identified with the authors of the reviewed studies, followed by our recommendations.
1. Epidemiology
The evidence relating to the epidemiology of sleep and wake disturbances following TBI has historically been the primary focus of the lit-erature, comprising 23 of the 43 articles across the five subtopics we identified for this review. Epidemiological investigation of a phenomenon is a necessary starting point as it provides a solid foundation for all further investigations to follow. We subdivided the studies on epidemiology, all of which were rated as Level III study designs, to include nine papers with a comparison group, all of moderate quality, and 12 articles that used a
TABLE 3Article Scope and Level of Articles
Article Scope Total No. of Articles Level II/IIA Level III Level IVA Level V
Epidemiology - Comparison group
9 9
Epidemiology - Single group/cohort
14 5 6 3
Pathophysiology 3 2 1
Pediatrics 6 6
Neuropsychology 4 1 2 1
Intervention 6 2 3 1
Review 3 2 1
Total 45 2/2 26 10 5

325Volume 21 Numbers 3-4
single group design, 10 of which were moderate quality, and two were of high quality.24,25 Both of these studies were also classified as Level III. Among the single group studies, there were five rated as Level III, five rated as Level IVA, and two rated as Level V. The use of a comparison group is a stronger design; however, our quality rating scheme studies included several elements, weighted equally, to assess overall quality so that a study weak in one area can be strong in other areas.
There are several important elements that should be addressed in a good quality epide-miological study. Recruitment is a key issue and recruitment methods must be carefully con-sidered to make sure that any selection bias is eliminated. Recruitment from the perspective of time postinjury is also a factor for consideration in that it allows us to observe the developmental time course of the disorder. Among the articles we reviewed, 65% of the studies (15/23) used consecutive recruitment; however, only 13% (3/23) used consecutive recruitment directly from the acute setting. Twenty-six percent were consecutively recruited as patients entered reha-bilitation and the remaining 26% were recruited while in rehabilitation or upon discharge from rehabilitation. Parcell and colleagues26 recruited all patients with TBI, with no preference for those
with sleep complaints, thus reducing bias in their sample. The remainder of the studies included retrospective chart review or recruitment by advertising. In contrast to the Parcell study, the study by Ouellet and colleagues,4 with the largest sample size of 452, recruited participants with reported symptoms of insomnia via mailings sent to 1500 prospective participants from archives of Québec City’s largest rehabilitation center, local brain injury associations, and support groups. The authors specifically reported using liberal inclusion criteria to try and capture a “broad portrait of the TBI population.”4(p. 201)
It is also important to consider possible con-founders or variables that influence interpretation of the findings, such as preexisting, concurrent, and secondary comorbidities; age at onset of injury; time since injury; severity of injury; etiol-ogy of injury; and gender. In an “ideal” study, the sample population would be large enough to allow stratification on some or all of these variables, so that the findings would be more generalizable and create a more thorough picture of the phenomenon.
Overall, the objective of the epidemiological studies reviewed for this article was to document the incidence, prevalence, and nature of sleep disturbances following TBI, primarily “insomnia” per se, with the inclusion of the most recent data relating specifically to sports-related concussion.
TABLE 4Article Scope and Quality of Articles
Article Scope Total Moderate Quality High Quality3 3.5 4 4.5 5 6.5
Epidemiology - Comparison group 9 6 3
Epidemiology - Single group/cohort 14 1 3 4 4 2
Pathophysiology 3 1 1 1Pediatrics 6a 2 1 1 1Neuropsychology 4 1 2 1Intervention 6 1 1 2 1 1Review 3Total 45 1 8 15 12 3 1
aOne article was of low quality with a rating of 2.5.

326 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
Slee
p an
d W
ake
Dis
orde
rs fo
llow
ing
Trau
mat
ic B
rain
Inju
ry: S
umm
ary
of R
evie
wed
Art
icle
s
Ref
eren
ceSt
udy
Obj
ectiv
eR
esea
rch
Des
ign
Sam
ple
Size
In
clus
ion/
Excl
usio
n
Subj
ects
Dat
a
Col
lect
ion
Met
hods
/M
easu
res
Sign
ifica
nt
Find
ings
Com
men
tsQ
ualit
ya
Epid
emio
logy
/Pre
vlae
nce/
Des
crip
tion:
Com
paris
on G
roup
Fitc
henb
erg
et a
l. 20
02
US
A
Type
:E
pi/P
rev/
Des
cE
stab
lish
frequ
ency
of
inso
mni
a (d
iagn
osis
us-
ing
DS
M-IV
) in
TB
I and
com
-pa
re it
with
in
som
nia
rate
s in
oth
er r
ehab
ou
tpat
ient
s
Leve
l III
Rec
ruitm
ent:
Pro
spec
-tiv
e co
hort
Con
secu
tive
OR
; Cro
ss-
sect
iona
l; C
ompa
rison
gr
oup
(Con
trols
):re
habi
litat
ion
outp
atie
nts
(sam
e #
SC
I an
d M
SK
)
TBIb
= 50
Con
trols
= 5
0M
SK
= 2
5S
CI =
25
Incl
usio
n:•
Gal
vest
on
Orie
ntat
ion
and
Am
nesi
a (G
OAT
) sc
ore
>75
• ≥
Ran
cho
Los
Am
igos
Lev
el V
IE
xclu
sion
:•
not i
n P
TA s
tate
Age
, yrs
: (P
< .0
5)TB
I: 36
.5 ±
14
.5;
SC
I: 38
.2 ±
13
.5;
MS
K: 4
7.3
± 12
.2G
ende
r:
(P<.
05)
TBI:
44%
FS
CI:
24%
FM
SK
80%
FG
CS:
sTB
I 42%
mod
TBI:
18%
mTB
I: 40
%Ti
me
sinc
e: 3
.8
± 7.
4 m
os.
PS
QI
BD
IS
leep
di
arie
s (T
BI
only
)In
som
ina
diag
nosi
s us
ing
DS
M-
IV c
riter
ia
TBI:
↓ sl
eep
qual
ity (
initi
a-tio
n pr
oble
ms
2x d
urin
g pr
oble
ms)
; ↑
slee
p du
ra-
tion
TBI:
30%
in
som
nia
diag
nosi
s (D
SM
-IV)
TBI:
↓ P
SQ
I gl
obal
sco
res
TBI:
< in
som
-ni
a ra
te th
an
cont
rols
Pre
vale
nce
of
inso
mni
a is
1/3
of
TBI p
opul
atio
nFi
rst p
aper
to u
se
form
al d
iagn
osis
of
inso
mni
a Li
mita
tions
:D
id n
ot s
tratif
y re
sults
by
seve
r-ity
, rel
iabi
lty o
f se
lf-re
port
slee
p di
arie
s
Mod
erat
e:4.
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze:
0.5
Attr
ition
:1S
tand
ardi
zed
outc
omes
: 1D
escr
iptio
n: 1
Follo
w-u
p: 0
Par
cell
et
al. 2
006
Aus
tralia
Type
:E
pi/P
rev/
Des
cE
xplo
re
subj
ect s
leep
re
ports
from
pe
rson
s w
ith
TBI
Leve
l III
Rec
ruitm
ent:
Con
secu
-tiv
e P
R (
≥ 2
wks
pos
t di
scha
rge)
Lo
ngitu
di-
nal s
urve
y de
sign
Con
trols
: gr
ener
al
com
mun
ity,
TBI =
63
Con
trols
= 6
3In
clus
ion:
• 16
-65
yrs
• Fa
cilit
y in
Eng
lish
• N
o tra
nsm
erid
ian
trave
l > 1
tim
e zo
ne in
pre
viou
s 12
mos
• N
o pr
einj
ury
slee
p di
sord
er•
No
benz
odia
-
Age
, yrs
: TB
I 32
.5 ±
1.7
;C
ontro
ls: 3
0.5
± 1.
2G
ende
r:
Bot
h gr
oups
: 43
% F
GC
S: 9
.6 ±
.57
PTA
: 19.
8 ±
2.7:
use
d fo
r se
verit
ym
TBI =
8
7-da
y se
lf re
port
slee
p-w
ake
diar
y (s
leep
and
w
ake
times
, sl
eep
onse
t la
tenc
y,
frequ
ency
, an
d du
ratio
n of
noc
turn
al
awak
enin
gs
and
dayt
ime
TBI:
> sl
eep
chan
ges;
>
nigh
t-tim
e aw
aken
ings
an
d lo
nger
sl
eep
onse
t la
tenc
y; m
ore
frequ
ently
re
porte
d by
m
TBI;
↑ an
xiet
y an
d de
pres
sion
Stre
ngth
s:Fo
llow
-up
and
used
a 7
-day
di-
ary;
Con
side
red
othe
r po
tent
ial
fact
ors
impa
ctin
g sl
eep;
Li
mita
tions
: D
iffer
ence
in
time
used
to n
ote
chan
ges
(TB
I, 8
mos
; Con
trols
3
mos
)
Mod
erat
e:
4.5/
7B
asel
ine:
1B
lindi
ng: 0
Sam
ple
size
: 0.
5A
ttriti
on: 0
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
1

327Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
age
and
gend
er
mat
ched
TB
I refl
ect
on c
hang
es
sinc
e in
jury
an
d co
ntro
ls
refle
ct o
n ch
ange
s in
th
e la
st 3
m
osD
ata
colle
c-tio
n:in
itial
and
3
mos
zepi
nes
or o
ther
sl
eepi
ng m
edic
a-tio
ns•
No
prev
ious
B
I, ne
urlo
gica
l di
sord
er, o
r m
ajor
ph
ysch
iatri
c di
sord
erS
cree
ned
by
neur
opsy
chol
o-gi
st to
det
erm
ined
el
igib
ility
mod
TBI =
13
sTB
I = 2
7;vs
TBI =
14
Tim
e si
nce:
m
ean
230
days
naps
)G
ener
al
slee
p qu
es-
tionn
aire
to
eva
lu-
ate
slee
p ch
ange
s an
d qu
ality
ES
SH
AD
S
asso
ciat
ed
with
↑ r
epor
t-in
g of
sle
ep
chan
ges
Wat
son
et
al. 2
007
US
A
Type
:E
pi/P
rev/
Des
cE
valu
ate
the
prev
alen
ce o
f sl
eepi
ness
fol-
low
ing
TBI
Leve
l III
Rec
ruitm
ent:
Pro
spec
tive
coho
rtC
onse
cu-
tive
ALo
ngitu
dina
l2
com
pari-
son
grou
ps;
C1
non-
cra-
nial
trau
ma
adm
issi
ons;
C2
traum
a fre
e se
lect
ed
from
frie
nds
of T
BI
Dat
a co
llec-
tion:
1 m
o an
d 1
yr
post
inju
ry
TBI =
512
(n
= 3
46 a
t 1 m
o; n
=
410
at 1
yr)
C1
= 13
2 (n
= 1
31 a
t 1 m
o; n
=
124
at 1
yr)
C2
= 10
2 (n
= 1
01 a
t 1 m
o; n
=
88 a
t 1 y
r)In
clus
ion:
• A
ny p
erio
d of
LO
C•
PTA
≥ 1
hr
• O
ther
obj
ectiv
e ev
iden
ce o
f hea
d tra
uma
• H
ospi
taliz
atio
n**
Som
e ha
d pr
e-ex
istin
g co
nditi
ons:
pr
ior T
BI,
alco
hol
abus
e, s
igni
fican
t ps
ychi
atric
dis
orde
r
Age
, yrs
:TB
I: 30
± 1
4C
1: 3
1.4
± 13
.5C
2: 2
4.5
± 8.
1G
ende
r:TB
I: 27
% F
;C
1: 2
8% F
,C
2: 5
6% F
GC
S: ≤
10
at
adm
issi
onIn
jury
sev
erity
: tim
e fro
m in
jury
to
a c
onsi
sten
t G
CS
sco
re o
f 6Ti
me
sinc
e: 1
m
os a
nd 1
yea
r at
follo
w-u
p
Sic
knes
s Im
-pa
ct P
rofil
e (S
IP):
slee
p an
d re
st
subs
cale
co
nsis
ting
of
4 qu
estio
ns
TBI:
55%
en
dors
ed ≥
1
slee
pine
ss
item
s 1
mo
post
inju
ry v
s C
1 41
% a
nd
C2
3%TB
I 27%
en
dors
ed ≥
1
slee
pine
ss
item
s 1
yr
post
inju
ry v
s C
1 23
% a
nd
C2
1%TB
I: sl
eepi
er
than
C1
at 1
m
o bu
t not
1
yr T
BI a
re
slee
pier
par
-tic
ular
ly th
ose
with
mor
e se
-ve
re in
jurie
s;
slee
pine
ss
Stre
ngth
s:
Goo
d fo
llow
-up
Lim
itatio
ns:
Wea
k ou
tcom
e m
easu
re; n
ot s
ep-
arat
ely
valid
ated
; ju
st d
escr
iptiv
e da
ta, l
arge
attr
ition
Maj
ority
wer
e m
TBI a
s sT
BI n
ot
able
to c
ompl
ete
the
SIP
; may
lead
to
und
eres
timat
e of
the
true
slee
pi-
ness
pat
tern
in
TBI
Mod
erat
e:
4.5/
7B
asel
ine:
1B
lindi
ng: 0
Sam
ple
size
: 1A
ttriti
on: 0
Sta
ndar
dize
d ou
tcom
es: 0
.5D
escr
itpio
n: 1
Follo
w-u
p: 1

328 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
↓ in
TB
I bu
t abo
ut
25%
rem
ain
slee
py a
fter
1 yr
(al
so tr
ue
for
C1)
Bee
tar
et
al. 1
996
US
A
Type
:E
pi/P
rev/
Des
cC
ompa
re th
e in
cide
nce
of
slee
p an
d pa
in
in T
BI a
nd
com
para
tive
neur
olog
ic
popu
latio
ns
Leve
l III
Rec
ruitm
ent:
OR
(neu
rops
y-ch
olog
y se
rvic
e)
Cro
ss-s
ec-
tiona
l C
ase-
cont
rol
stud
y C
onse
cutiv
e ch
art r
evie
wC
ompa
rison
gr
oup:
gene
ral
neur
olog
ic
patie
nts
refe
rred
for
neur
opsy
-ch
olog
ical
as
sess
men
t
mTB
I = 1
27m
od to
sTB
I = 7
5C
ontro
ls =
123
Use
d M
ild T
BI
Com
mitt
ee o
f the
H
ead
Inju
ry In
ter-
disc
iplin
ary
Spe
cial
In
tere
st G
roup
of
the
Am
eric
an C
on-
gres
s of
Reh
abili
ta-
tion
Med
icin
e
Age
, yrs
:TB
I: 36
.1 ±
11
.7;
Con
trols
: 43.
3 ±
13.6
Gen
der:
TBI:
32%
F;
Con
trols
: 42%
FG
CS:
NI
Tim
e Si
nce:
TBI:
23.9
± 2
.2
mos
(in
jury
); C
ontro
ls: 3
5.5
± 23
.3 m
os
(sym
ptom
)
Cha
rt re
view
Pat
ient
re-
port
of s
leep
an
d or
pai
n pr
oble
ms
Sle
ep
mai
nten
ance
m
ost c
om-
mon
sle
ep
prob
lem
; TB
I: 55
%
had
inso
mni
a co
mpl
aint
s vs
Con
trols
<3
3%; T
BI:
> in
som
nia
and
pain
com
-pl
aint
s (2
.5 x
m
ore)
; pre
s-en
ce o
f pai
n ↑
inso
mni
a re
port
2 x;
TB
I with
out
pain
: > s
leep
co
mpl
aint
s th
an C
ontro
ls
and
mTB
I >
mod
/sTB
I; m
TBI >
pai
n th
an m
od/
sTB
I; C
om-
plai
nts
↓ w
ith
> tim
e si
nce
inju
ry
Stre
ngth
s:O
ne o
f ear
liest
st
udie
s to
doc
u-m
ent i
ncid
ence
Lim
itatio
ns:
Ret
rosp
ectiv
e an
d su
bjec
tive
data
co
llect
ion
Mod
erat
e:
4/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0D
escr
itpio
n: 1
Follo
w-u
p: 0
Oue
llet &
M
orin
200
6Ty
pe:
Epi
/Pre
v/D
esc:
Leve
l III
Rec
ruit-
TBI =
14
m to
sTB
IC
ontro
ls =
14
Age
, yrs
: TB
I: 30
.4 ±
9.7
Dia
gnos
tic
Inte
rvie
w fo
rTB
I: P
SG
sh
owed
71%
Res
ults
sim
ilar
to
thos
e w
ith p
rimar
yM
oder
ate:
4/
7

329Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
Can
ada
Com
pare
su
bjec
tive
and
obje
ctiv
e m
ea-
sure
s of
sle
ep
in T
BI
LC R
eha-
bilit
atio
n ce
nter
s an
d ad
ver-
tisem
ents
se
nt to
TB
I as
soci
atio
ns
and
sup-
port
grou
ps
mai
ling
lists
); C
ross
-se
ctio
nal;
Com
pari-
sion
gro
up:
heal
thy
good
sle
ep-
ers
mat
ched
on
age
and
ge
nder
to
TBI;
recr
uit-
ed th
roug
h ad
verti
se-
men
ts a
nd
acqu
ain-
tanc
es o
f th
e au
thor
s;
2 ni
ghts
of
PS
G
Incl
usio
n:•
18-5
0 yr
s•
TBI ≤
last
5 y
rs•
Sta
ble
phys
ical
he
alth
• N
o lo
nger
an
inpa
tient
• H
ave
an in
som
-ni
a sy
ndro
me
Exc
lusi
on:
• M
ajor
unt
reat
ed
or u
nsta
ble
co-
mor
bid
cond
ition
• S
leep
diff
icul
ties
befo
re T
BI
• E
vide
nce
of
anot
her
slee
p di
sord
er•
Sig
nific
ant p
ain
• U
nabl
e to
com
-pl
ete
the
ques
-tio
nnai
res
Con
trols
: 30.
0 ±
10.0
Gen
der:
56%
F
GC
S: 4
mild
, 1
mild
-mod
, 4
mod
, 3 m
od-
sev,
2 s
ev (
cri-
teria
in a
rticl
e)Ti
me
sinc
e:21
mos
Inso
mia
S
leep
dia
ryP
SG
Sle
ep s
ur-
vey
ISS
MFI
BD
IB
eck
Anx
iety
In
vent
ory
with
inso
mni
a La
rge
effe
ct
size
s fo
r to
tal
slee
p tim
e w
ake
afte
r sl
eep
onse
t, aw
aken
ings
lo
nger
than
5
min
, and
sl
eep
ef-
ficie
ncy
TBI:
> po
rtion
of
sta
ge 1
sl
eep
Whe
n th
ose
usin
g ps
ycho
-tro
pic
med
s ex
clud
ed, T
BI
had
> aw
ak-
enin
gs la
stin
g lo
nger
than
5
min
and
a
shor
t RE
M
slee
p on
set
late
ncy
inso
mia
or
inso
mni
a-re
late
d to
dep
ress
ion
Lim
itatio
ns:
Sm
all s
ampl
e si
ze a
nd a
lot
of v
aria
bilit
y in
TB
I gro
up a
nd
pres
ence
of s
leep
pr
oble
ms
in C
on-
trol g
roup
Mul
tiple
com
pari-
son
and
lack
of
stat
istic
al p
ower
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
crip
tion:
1Fo
llow
-up:
0
Par
cell
et
al. 2
008
Aus
tralia
Type
:E
pi/P
rev/
Des
cE
valu
ate
chan
ges
in
slee
p qu
ality
an
d ch
ange
s in
obj
ectiv
e re
cord
ed s
leep
pa
ram
eter
s af
ter T
BI a
nd
Leve
l III
Rec
ruitm
ent:
AI (
mod
to
sTB
I);
Cro
ss-
sect
iona
l; S
urve
y an
d la
b-ba
sed
noct
urna
l P
SG
;
TBI =
10
Con
trols
= 1
0In
clus
ion:
• 16
-65
yrs
• E
nglis
h fa
cilit
y•
Nor
mal
bod
y m
ass
inde
x•
No
trans
mer
idia
n tra
vel a
cros
s >
1 tim
e zo
ne in
Age
, yrs
:TB
I: 38
.8 ±
4.3
;C
ontro
ls: 3
7.8
± 44
.4G
ende
r:40
% F
GC
S: 1
0.9
± 1.
040
% m
od T
BI;
40%
sTB
I; 20
%
Dem
o-gr
aphi
c an
d m
edic
atio
n de
tails
at
recr
uitm
ent
and
inju
ry
deta
ils fr
om
med
ical
re
cord
s;
Sle
ep-w
ake
TBI:
poor
er
slee
p qu
ality
an
d hi
gher
le
vels
of
anxi
ety
and
depr
essi
on;
TBI:
↑ in
de
ep (
slow
w
ave)
sle
ep,
↓ in
RE
M, >
Doc
umen
ts o
f im
porta
nce
of
subj
ectiv
e re
port
as c
entra
l to
diag
-no
sis
and
treat
-m
ent b
ut n
eed
to
cons
ider
obj
ectiv
e da
ta a
s w
ell
Pro
vide
s m
any
impo
rtant
pra
ctic
e
Mod
erat
e:
4/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

330 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
inve
stig
ate
the
rela
tions
hip
betw
een
moo
d st
ate
and
inju
ry c
hara
c-te
ristic
s
Com
paris
on
grou
p ag
e-
and
gend
er-
mat
ched
co
ntro
ls
in g
ener
al
com
mun
ity;
PS
G o
ver
2 ni
ghts
with
in
1 w
k; e
valu
-at
ed in
TB
I an
d co
ntro
l pa
irs
prev
ious
12
mos
• N
o pr
einj
ury
slee
p di
sord
er•
No
benz
odia
z-ep
ines
or
othe
r sl
eepi
ng m
edic
a-tio
ns•
No
prev
ious
B
I, ne
urol
ogi-
cal d
isor
der,
or
maj
or p
sych
iatri
c di
sord
er
vsTB
I; P
TA
16.4
4 ±
4.3
days
Tim
e si
nce:
51
6 ±
124
days
diar
y fo
r 7
days
; ES
S
Sle
ep q
ualit
y qu
estio
n-na
ire (
TBI
chan
ges
sinc
e in
jury
an
d C
ontro
ls
chan
ges
in
last
3 m
os);
PS
QI;
Noc
-tu
rnal
PS
G;
HA
DS
> ni
ght-t
ime
awak
en-
ings
; TB
I: >
anxi
ety
and
depr
es-
sion
, whi
ch
co-v
arie
d w
ith th
e ob
-se
rved
sle
ep
chan
ges
poin
ts; i
s a
stro
ng
cont
ribut
or to
clin
i-ca
l and
res
earc
h lit
erat
ure
Sch
reib
er
et a
l. 20
08
Isra
el
Type
:E
pi/P
rev/
Des
c:Id
entif
y th
e ch
arac
teris
-tic
s of
sle
ep
dist
urba
nce
in a
dults
afte
r m
TBI
Leve
l III
Rec
ruitm
ent:
Ret
ro-
spec
tive;
C
onse
cutiv
e O
R (
whe
re
slee
p la
b da
ta a
vail-
able
); C
ross
-se
ctio
nal
Com
pari-
son
grou
p:
mat
ched
an
d re
ferr
ed
for
slee
p ev
alua
tion
as p
art o
f th
e ro
u-tin
e pr
e-em
ploy
men
t as
sess
men
tTB
I 2 n
ight
s P
SG
(no
t on
a w
eeke
nd);
Con
trols
mTB
I = 2
6C
ontro
ls =
20
(app
aren
tly h
ealth
y)In
clus
ion:
• 21
-50
yrs
• D
ocum
ente
d (≥
1
yr s
ince
mTB
I)•
Nor
mal
bra
in C
T,
MR
I•
Neg
ativ
e E
EG
• N
o pa
st h
isto
ry o
f C
NS
pat
holo
gy•
No
pre-
mor
bid
or p
rese
nt m
ajor
ps
ychi
atric
dia
g-no
sis
• N
o sl
eep
apne
a or
res
tless
leg
synd
rom
e
Age
, yrs
:TB
I: 31
.6 ±
8.8
Con
trols
: 33.
8 ±
7.8
Gen
der:
NI
GC
S: N
ITi
me
sinc
e: 1
2 m
os to
21
yrs
PS
GM
SLT
TBI:
slee
p pa
ttern
s di
s-tu
rbed
; sle
ep
arch
itect
ure
alte
red;
<
RE
M s
leep
sc
ores
and
>
NR
EM
sco
res
TBI:
MS
LTdo
cum
ente
d si
gnifi
cant
E
DS
Impo
rtant
to
iden
tify
thos
e w
ho
need
trea
tmen
t for
sl
eep
prob
lem
sLi
mita
tions
:C
ontro
ls w
ere
not a
ll w
ithin
the
norm
al v
alue
sP
ossi
ble
issu
es o
f re
call
bias
Wid
e ra
nge
of
time
post
inju
ryD
iffer
ence
in d
ata
colle
ctio
n st
rate
gy
betw
een
the
2 gr
oups
Mod
erat
e:
4/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

331Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
only
1 n
ight
M
SLT
on
day
betw
een
the
2 ni
ghts
Will
iam
s et
al.
2008
C
anad
a
Type
:E
pi/P
rev/
Des
cC
hara
cter
ize
the
exte
nt a
nd
natu
re o
f dis
-ru
pted
sle
ep
in in
divi
dual
s w
ith lo
ng-
term
sle
ep
com
plai
nts
subs
eque
nt
to m
TBI (
i.e.,
spor
t-rel
ated
co
ncus
sion
) To
det
erm
ine
whe
ther
sle
ep
dist
urba
nces
in
mTB
I are
m
ore
char
-ac
teris
tic o
f ps
ycho
logi
cal,
psyc
hiat
ric,
or id
iopa
thic
in
som
nia
Leve
l III
Rec
ruitm
ent:
LC (
univ
er-
sity
set
ting)
Cro
ss-s
ec-
tiona
l C
ompa
risio
n gr
oup
Face
-to-fa
ce
inte
rvie
w
and
labo
ra-
tory
PS
G
TBI =
9C
ontro
ls =
9In
clus
ion:
• 18
-26
yrs
TBI:
• B
etw
een
6 m
os
and
6 yr
s po
st-
inju
ry
• S
ympt
oms
of
Pos
t Con
cuss
ion
Syn
drom
e (P
CS
) at
the
time
of
inju
ry•
Cle
arly
dis
tin-
guis
h be
twee
n sl
eep
patte
rns
befo
re a
nd a
fter
inju
ry•
Sle
ep d
iffic
ultie
s w
ithin
1 m
o of
in
jury
• S
leep
com
plai
nts
char
acte
rized
by
slee
p on
set o
f >
30 m
in o
n ≥
4 or
da
ys in
a w
eek
Con
trols
:•
No
prev
ious
BI
• N
o sl
eep
diffi
cul-
ties
Age
, yrs
:TB
I: 21
.4 ±
2.4
Con
trols
: 20.
7 ±
2.1
Gen
der:
TBI:
33%
F;
Con
trols
: 56%
FG
CS:
mild
ra
nge;
LO
C fo
r ≤
5 m
inTi
me
sinc
e:
TBI
27.8
± 1
5.5
mos
Per
sona
lity
Ass
essm
ent
Inve
ntor
y (P
AI):
de-
pres
sion
and
an
xiet
y B
rock
A
dapt
ive
Func
tion-
ing
Que
s-tio
nnai
re
(BA
FQ)
PS
QI
Sle
ep D
isor
-de
rsQ
uest
ion-
naire
(S
DQ
)B
rock
sle
ep
and
inso
m-
nia
ques
tion-
naire
Sle
ep lo
g fo
r 2
wks
PS
G fo
r 3
cons
ecut
ive
nigh
tsP
ower
spe
c-tra
l (FF
T)
anal
ysis
of
the
slee
p on
set p
erio
d
TBI:
long
-te
rm tr
oubl
e w
ith in
itiat
ing/
mai
ntai
ning
sl
eep
with
at
tent
ion
and
mem
ory
and
affe
ctiv
e (d
epre
ssio
n an
d an
xiet
y)
abno
rmal
ities
; si
gnifi
cant
di
ffere
nce
show
n in
PA
I, B
AFQ
, PS
QI
TBI:
4%
less
effi
cien
t sl
eep,
sho
rter
RE
M o
nset
la
tenc
ies,
lo
nger
sle
ep
onse
t lat
en-
cies
(va
ri-ab
ility
with
in
sam
ple)
; FFT
re
veal
ed
grea
ter
intra
-sub
ject
va
riabi
lity
in
sigm
a, th
eta,
an
d de
lta
pow
er d
urin
g sl
eep
onse
t TB
I diff
eren
t
Sle
ep d
istu
rban
c-es
can
per
sist
w
ell a
fter
inju
ry;
Stre
ngth
s: V
ery
thor
ough
stu
dyLi
mita
tions
:S
mal
l sam
ple,
sa
mpl
e of
con
-ve
nien
ce (
stu-
dent
vol
unte
ers)
; C
onfir
mat
ion
of
subj
ectiv
e se
lf-re
ports
with
PS
G;
Hig
hlig
hts
need
to
look
at s
port-
rela
ted
conc
ussi
on
Mod
erat
e:
4/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
:1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

332 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
from
Con
trols
bu
t not
eas
l-ity
cla
ssifi
ed
into
exi
stin
g in
som
nia
subt
ypes
Gos
selin
et
al.
2009
C
anad
a
Type
:E
pi/P
rev/
Des
cIn
vest
igat
e th
e ef
fect
s of
sp
ort-r
elat
ed
conc
ussi
on o
n su
bjec
tive
and
obje
ctiv
e sl
eep
qual
ity
Leve
l III
Rec
ruitm
ent:
LC (
inde
-pe
nden
t of
the
natu
re
of r
epor
ted
sym
ptom
s)C
ross
-sec
-tio
nal
Use
d co
ncus
sion
di
agno
stic
cr
iteria
Com
paris
on
grou
p:N
o hi
stor
y of
co
ncus
sion
; m
atch
ed o
n ag
e, g
ende
r, ed
ucat
ion,
an
d ag
e st
arte
d pl
ay-
ing
the
spor
tP
SG
on
2 co
nsec
utiv
e ni
ghts
in th
e la
b
AB
I = 1
0C
ontro
ls =
11
Incl
usio
n:•
AB
I: hi
stor
y of
at
leas
t 2 c
oncu
s-si
ons
Exc
lusi
on:
• P
rese
nce
of
neur
olog
ical
or
psyc
hiat
ric d
is-
ease
s•
Ext
rem
ely
early
or
late
hab
itual
be
d tim
es•
Use
of d
rugs
kn
own
to a
ffect
sl
eep
or d
aytim
e sl
eepi
ness
• W
ork
the
nigh
t sh
ift•
Trav
el to
ano
ther
tim
e zo
ne in
last
2
mos
Age
, yrs
:A
BI:
24.3
± 6
.1
yrs;
Con
trols
: 22.
6 ±
2.4
Gen
der:
AB
I: 30
% F
Con
trols
: 34%
FG
CS:
AB
I all
13-1
5#
conc
ussi
ons:
4.
6 ±
2.1
with
at
leas
t 1 in
last
yr
Tim
e si
nce:
NI
PS
GQ
EE
Q: a
s-se
ssm
ent
of 1
0-m
in
perio
d of
w
akef
ul-
ness
30-
min
af
ter
slee
p of
fset
; Pos
t C
oncu
ssio
n S
ymp-
tom
Sca
le
(PC
SS
); P
SQ
I; E
SS
; B
DI;
Loca
lly
deve
lope
d qu
estio
n-na
ire o
n sl
eep
qual
-ity
; Cog
S
port
com
-pu
ter
bat-
tery
: sho
rt ne
urpy
scho
l-og
y ev
alua
-tio
n ad
apte
d fro
m N
FL
batte
ry
AB
I: >
sym
ptom
s,
wor
se s
leep
qu
ality
; >
delta
act
ivity
an
d <
alph
a ac
tivity
dur
ing
wak
eful
ness
; C
oncu
ssio
n se
ems
to b
e as
soci
ated
w
ith a
wak
e-fu
lnes
s pr
ob-
lem
, rat
her
than
sle
ep
dist
urba
nce;
A
thle
tes
with
wor
se
slee
p qu
ality
(P
SQ
I) an
d sy
mpt
oms
(PC
SS
) >
rela
tive
delta
po
wer
dur
ing
dayt
ime;
AB
I lo
wer
PS
QI
asso
ci-
ated
with
↓ in
R
EM
sle
ep
effic
ienc
y P
SQ
I and
P
CS
S c
or-
Dis
crep
ancy
be
twee
n su
bjec
-tiv
e an
d ob
jec-
tive
findi
ngs;
not
ex
plai
ned
by
depr
essi
on n
or
hype
raro
usal
Lim
itatio
ns:
Sm
all s
ampl
e w
ith
excl
usio
ns th
e sa
mpl
e be
cam
e ev
en s
mal
ler,
how
ever
, hig
h-lig
hts
need
to
asse
ss s
leep
an
d w
akef
ulne
ss
follo
win
g sp
ort-
rela
ted
conc
ussi
onO
nly
a pi
lot s
tudy
Mod
erat
e:
4/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

333Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
rela
ted;
Abs
o-lu
te s
pec-
tral p
ower
sh
owed
hig
h in
ter-
subj
ect
varia
tion
in
AB
I; th
eref
ore
anal
yze
on
the
rela
-tiv
e sp
ectra
l po
wer
Epid
emio
logy
/Pre
vale
nce/
Des
crip
tion:
Coh
ort/S
ingl
e G
roup
Bau
man
n et
al.
2007
S
witz
erla
nd
Type
: E
pi/P
rev/
Des
cD
eter
min
e th
e fre
quen
cy
and
clin
ical
ch
arac
teris
tics
of p
osttr
au-
mat
ic S
WD
; as
sess
CS
F hy
pocr
etin
le
vels
6 m
os
afte
r TB
I and
ris
k fa
ctor
s fo
r po
sttra
umat
ic
SW
D
Leve
ll III
Rec
ruitm
ent:
Pro
spec
-tiv
e st
udy;
C
onse
cutiv
e A
; (w
ithin
4
days
of
inju
ry);
Long
itudi
nal;
Sin
gle
grou
p B
asel
ine:
labo
ra-
tory
test
s; 6
m
os: o
ther
ou
tcom
es,
subs
ampl
e re
peat
ed
labo
rato
ry
test
s
TBI =
65
(96
en-
rolle
d; 7
6 av
aila
ble
for
follo
w-u
p)In
clus
ion:
• A
cute
, firs
t eve
r TB
IE
xclu
sion
:•
Sle
ep-w
ake
or
psyc
hiat
ric d
isor
-de
rs d
iagn
osed
pr
ior
to T
BI
Age
, yrs
: 16-
72, m
ean
38 ±
16
yrs
Gen
der:
14%
FG
CS:
mea
n 10
.2,
mTB
I: 40
%m
odTB
I: 23
%sT
BI:
37%
Tim
e si
nce:
6
mos
afte
r TB
I
CT
scan
; C
SF
hypo
-cr
etin
-1 le
v-el
s; H
uman
le
ukoc
yte
antig
en
(HLA
) ty
ping
In
terv
iew
: so
cial
sta
tus
and
resi
dual
sy
mpt
oms
post
inju
ry,
incl
udin
g sl
eep
habi
ts;
Neu
rolo
gica
l ex
amin
ia-
tion
usin
g a
stan
dard
pr
otoc
ol,
with
the
Fol-
stei
n M
MS
EB
DI;
Med
ical
O
utco
mes
S
tudy
For
m
- 36
; ES
S;
SW
D a
re
com
mon
afte
r TB
I, E
DS
/fa-
tigue
= 5
5%;
Pos
ttrau
mat
ic
hype
rsom
nia
= 22
%; L
ow
hypo
cret
in
leve
ls fo
und
in 1
9% 6
m
os a
fter
inju
ry v
s 93
%
in fi
rst d
ays
afte
r in
jury
; 6
mo
hypo
-cr
etin
leve
ls
wer
e lo
wer
in
thos
e w
ith
post
trau-
mat
ic S
WD
; N
o ot
her
sign
ifica
nt
rela
tions
hips
w
ere
foun
d;
Hyp
ocre
tin
Stre
ngth
s:Ve
ry th
orou
ghLi
mita
tions
:A
ttriti
on w
as la
rge
and
not a
ll av
ail-
able
for
labo
rato
ry
follo
w-u
p
Hig
h:
5/7
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 1A
ttriti
on: 0
.5S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 1

334 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
Sle
ep A
pnea
S
cale
of t
he
Sle
ep D
isor
-de
rs Q
ues-
tionn
aire
; U
llanl
inna
N
arco
leps
y S
cale
; PS
G;
MS
LT; A
c-tig
rapy
syst
em p
os-
sibl
e co
ntrib
-ut
or to
pat
ho-
phys
iolo
gy o
f po
sttra
umat
ic
SW
D
Cas
triot
ta
et a
l. 20
07
US
A
Type
:E
pi/P
rev/
Des
cD
eter
min
e th
e pr
eval
ence
an
d co
nse-
quen
ces
of
slee
pine
ss a
nd
slee
p di
sor-
ders
afte
r TB
IE
xplo
re th
e re
latio
nshi
p be
twee
n pr
esen
ce o
f sl
eep
diso
r-de
rs, i
njur
y ch
arac
teris
cs
and
subj
ect
varia
bles
Leve
l IV
AR
ecru
itmen
t: P
rosp
ectiv
e st
udy
AI (
3 ce
nter
s);
Sin
gle
grou
p;
Cro
ss-s
ec-
tiona
l
TBI =
87
Incl
usio
n:•
>18
yrs
old
• ≥
3 m
os p
ost-
inju
ryE
xclu
sion
:•
Pre
senc
e of
ci
rcad
ian
rhyt
hm
diso
rder
• U
se o
f sed
atin
g m
edic
atio
ns•
Una
ble
to g
ive
info
rmed
con
sent
Age
, yrs
: 38.
3 ±
15.1
Gen
der:
28%
FG
CS:
NI
Sev
erity
: mild
8%
, mod
erat
e 17
5, m
oder
ate-
seve
re 6
%,
seve
re 3
3%,
unkn
own
36%
Tim
e si
nce:
64
.3 ±
117
.7
mos
PS
G; M
SLT
; E
SS
; PV
T;
PO
MS
; FO
SQ
23%
OSA
; 46
% a
bnor
-m
al s
leep
st
udie
s; 1
1%
post
traum
atic
hy
pers
omni
a;
6% n
arco
-le
psy;
7%
pe
riodi
c lim
b m
ovem
ents
; 25
% w
ith o
b-je
ctiv
e ED
S;
No
corre
latio
n be
twee
n ES
S
and
MSL
T (r
= 0.
10)
; No
diffe
renc
es in
de
mog
raph
-ic
s an
d in
jury
ch
arac
teris
-tic
s be
twee
n sl
eepy
(SI
) an
d no
n-sl
eep
(NSI
) Su
bjec
ts:
BMI:
SI>N
SI;
PVT:
SI<
NSI
; FO
SQ: S
I
Stre
ngth
s:Fi
rst s
tudy
to
show
that
a s
leep
di
sord
er a
dds
an
addi
tiona
l cog
ni-
tive
burd
enLi
mita
tions
:N
o ob
ject
ive
mea
sure
of d
aily
fu
nctio
ning
Hig
h:
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

335Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
bette
r N
SI
PO
MS
: no
diffe
renc
es
Fitc
henb
erg
et a
l. 20
00
US
A
Type
: E
pi/P
rev/
Des
cR
elat
ion-
ship
bet
wee
n in
som
nia
and
dem
ogra
phci
s,
inju
ry, a
nd
psyc
holo
gica
l va
riabl
es in
po
st-a
cute
TB
I
Leve
l IV
AR
ecru
itmen
t:P
ospe
c-tiv
e st
udy;
C
onse
cutiv
e O
R; C
ross
-se
ctio
nal;
Sin
gle
grou
p
TBI =
91
Incl
usio
n:•
Dia
gnos
is o
f TB
I on
basi
s of
ex
amin
iatio
n•
Rec
over
y to
pos
t-ac
ute
phas
e•
Med
ical
det
erm
i-na
tion
of n
eed
for
outp
atie
nt n
euro
-re
habi
litat
ion
Exc
lusi
on•
In s
tate
of P
TA•
Rat
ed b
elow
Le
vel V
I on
Leve
ls o
f Cog
ni-
tive
Func
tioni
ng
Sca
le (
LCS
F)•
Usi
ng s
leep
m
edic
atio
n
Age
, yrs
:33
.8 ±
14.
5G
ende
r:41
% F
GC
S:13
-15:
33%
9-12
: 21%
3-8:
46%
Tim
e si
nce:
m
ean
3.3
mos
PS
QI;
BD
I; G
OAT
; LC
FS
Stro
ng
rela
tions
hip
betw
een
inso
mni
a an
d de
pres
-si
on; P
ain
dist
urba
nce
of s
leep
was
si
gnifi
cant
ly
asso
ciat
ed
with
inso
m-
nia;
BD
I: 68
%
depr
esse
d w
ere
suf-
fere
ing
from
in
som
nia
Stre
ngth
s:In
dent
ifies
a
deve
lopm
enta
l pa
ttern
that
may
pr
ogre
ss fr
om a
ph
ysio
logi
cal b
asis
to
a s
econ
dary
di
sord
er a
ssoc
i-at
ed w
ith d
epre
s-si
on
Mod
erat
e:4.
5/7
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 1A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0
Oue
llet,
Bea
ulie
u-B
onne
au &
M
orin
200
6 C
anad
a
Type
:E
pi/P
rev/
Des
c;
To d
eter
min
e th
e fre
quen
cy
of in
som
nia
acco
rdin
g to
D
SM
-IV a
nd
Inte
rnat
iona
l C
lass
ifica
tion
of S
leep
Dis
-or
ders
(IC
SD
) cr
iteria
. To
de-
scrib
e cl
inic
al
and
soci
ode-
Leve
l IV
AR
ecru
itmen
t:LC
(Fr
ench
-sp
eaki
ng
from
re
habi
lita-
tion
cent
er
arch
ives
and
on
mai
ling
lists
of T
BI
asso
ciat
ions
in
Que
bec)
; M
aile
d qu
es-
tionn
aire
TBI =
452
Incl
usio
n:•
≥ 16
yrs
• TB
I: m
inor
, mild
, m
oder
ate
or
seve
re
Age
, yrs
:40
.2 ±
13.
1G
ende
r: 3
5% F
GC
S: N
IS
ever
ity:
59.9
% s
TBI
23.3
% m
odTB
I13
.7%
mTB
I(c
riter
ia in
clud
es
GC
S)
Tim
e si
nce:
mea
n 7.
8 yr
s
Que
stio
n-na
ire b
ookl
et
entit
led
“Qua
lity
of s
leep
an
d le
vel
of fa
tigue
fo
llow
ing
a TB
I”: L
ocal
ly
deve
lope
d qu
estio
nsIS
SM
ulti-
dim
en-
sion
al
Inso
mni
a pr
eval
ent
afte
r TB
I, 64
.3%
with
sl
eep
onse
t in
som
nia,
76
.6%
w
ith s
leep
m
aint
enan
ce
inso
mni
a;
Pre
dict
ors
of in
som
nia:
le
sser
sev
er-
ity o
f BI,
Lim
tatio
ns:
Onl
y su
bjec
tive
data
U
nder
resp
rese
nta-
tion
of m
TBI
Thos
e w
ith in
-so
mni
a pr
oble
ms
may
hav
e be
en
mor
e m
otiv
ated
to
resp
ond
Not
abl
e to
de-
term
ine
inso
mni
a su
btyp
es
Mod
erat
e:4.
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0.5
Des
critp
ion:
1Fo
llow
-up:
0

336 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
mog
raph
ic
char
acte
ristic
s of
inso
mni
a in
TB
I
Cro
ss-s
ec-
tiona
l; S
in-
gle
grou
p;
Sig
nific
ant
othe
rs
com
plet
ed a
br
ief p
aral
lel
eval
uatio
n
fatig
ue
inve
ntor
y In
-di
ce d
e dé
-tre
sse
psy-
chol
ogiq
ue
de
L’E
nquê
te
San
té Q
ué-
bec
(Fre
nch
adap
tatio
n of
Psy
chia
t-ric
Sym
p-to
m In
dex)
S
igni
fican
t O
ther
’s
Eva
luat
ion
Que
stio
n-na
ire (
si-
gific
ant o
ther
ve
rsio
ns
of IS
S a
nd
othe
r ab
ove
ques
tions
)
Rao
et a
l. 20
08 U
SA
Type
:E
pi/P
rev/
Des
cTo
ass
ess
the
prev
alen
ce o
f an
d ris
k fa
c-to
rs fo
r sl
eep
dist
urba
nces
in
acut
e po
sttra
u-m
atic
TB
I
Leve
l III
Rec
ruitm
ent:
PAC
(w
ithin
3
mos
of
traum
a);
Long
itudi
nal
obse
rva-
tiona
l stu
dy;
Sin
gle
grou
p; D
ata
colle
ctio
n:
1) w
ithin
2
wks
of i
njur
y to
ass
ess
hist
ory
of
TBI =
54
Incl
usio
n:•
≥ 18
yrs
• A
ble
to p
rovi
de
info
rmed
con
sent
• A
dmitt
ed to
hos
-pi
tal w
ith e
xper
i-en
ce o
f LO
C•
GC
S ≤
15
• P
ositi
ve C
T fin
d-in
gsE
xclu
sion
:•
Prio
r TB
I•
Ope
n he
ad in
jury
• H
isto
ry o
f oth
er
Age
, yrs
:43
.2 ±
17.
7G
ende
r:41
% F
GC
S:m
ean
12.5
±
3.6;
65%
mild
, 11%
m
oder
ate,
and
19
% s
ever
eTi
me
sinc
e:≥
3 m
os
Stru
ctur
ed
Clin
ical
In
terv
iew
for
DS
M-IV
Axi
s 1
diso
rder
s (S
CID
-IV
); G
en-
eral
Med
i-ca
l Hea
lth
Rat
ing
Sca
le
(GM
HR
); M
OS
; Sel
f-re
port
for
anxi
ety
and
de
pres
sion
Wor
se o
n m
ost s
leep
m
easu
res
afte
r TB
I co
mpa
red
to b
efor
e TB
I; A
nxi-
ety
diso
rder
se
cond
ary
to
TBI w
as m
ost
cons
iste
nt
sign
ifica
nt
risk
fact
or to
be
ass
ocia
ted
with
wor
sen-
Stre
ngth
s:A
sses
s sl
eep
prob
lem
s in
the
acut
e pe
riod;
P
artic
ipan
ts h
ad a
ra
nge
of s
ever
ities
Lim
itatio
ns:
Sub
ject
ive
data
an
d re
call
bias
m
ight
be
an is
sue
Lack
of i
nfo
on
othe
r po
tent
ial
influ
enci
ng fa
ctor
s (p
ain,
med
ical
pr
oble
ms
and
Mod
erat
e:4.
5/7
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 0.
5A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0.5

337Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
psyc
hiat
ric
and
slee
p pr
oble
ms
2) w
ithin
1-
3 m
os o
f in
jury
; for
so
me
both
at
the
sam
e tim
e
type
of i
llnes
sin
g sl
eep
stat
usm
edic
atio
ns
Clin
chot
et
al. 1
998
US
A
Type
:E
pi/P
rev/
Des
cD
efine
and
co
rrel
ate
the
inci
denc
e an
d ty
pe o
f sle
ep
dist
urba
nces
th
at o
ccur
afte
r B
I
Leve
l VR
ecru
itmen
t:P
rosp
ectiv
e st
udy
Con
secu
tive
AI
Sin
gle
grou
pLo
ngitu
dina
lB
asel
ine
and
1 yr
fo
llow
-up
post
dis
-ch
arge
via
te
leph
one
inte
rvie
w
TBI =
145
Incl
usio
n:•
≥ 14
yrs
with
su
stai
ned
BI
Exc
lusi
on:
• N
ot a
cute
inju
ry•
Prim
arily
the
re-
sult
of a
nore
xia
Age
, yrs
:31 G
ende
r:23
% F
GC
S:
Med
ian
= 4
Tim
e si
nce:
m
ean
20 d
ays
Dire
ct o
bser
-va
tion;
Med
i-ca
l rec
ord
extra
ctio
ns;
Agi
tate
d B
ehav
iour
S
cale
; FIM
; W
echs
ler
Mem
ory
Sca
le;
Hal
stea
d R
eita
n
Neu
rops
y-ch
olog
ical
B
atte
ry;
Follo
w-u
p in
terv
iew
: C
omm
unity
In
tegr
atio
n Q
uest
ion-
naire
; Sle
ep
diffi
culti
es,
med
ical
pr
oble
ms,
m
edic
atio
ns,
serv
ices
us
ed
50%
diff
icul
ty
with
sle
ep,
25%
sle
ep-
ing
mor
e an
d 45
% d
iffic
ulty
fa
lling
sle
epG
CS
≤ 7
less
lik
ely
to h
ave
prob
lem
s w
ith s
leep
th
an G
CS
>
7; 6
4%
with
sle
ep
diffi
culty
wak
-in
g up
too
early
; Sle
ep
com
plai
nts
corr
elat
ed
with
pre
senc
e of
fatig
ue, >
G
CS
, bet
ter
imm
edia
te
mem
ory,
po
sitiv
e su
bsta
nce
abus
e hi
stor
y,
> ag
e, a
nd
bein
g fe
mal
e
Lim
itatio
n:La
rge
num
ber
lost
to
follo
w-u
p; th
ose
lost
mor
e lik
ely
to
have
a h
isto
ry o
f su
bsta
nce
abus
eS
elf-r
epor
t of
slee
p di
fficu
lties
Mod
erat
e:4/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 0S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n:
0.5
Follo
w-u
p: 1
Web
ster
Type
:Le
vel I
V A
TBI =
28
Age
, yrs
:O
vern
ight
S
leep
-rel
ated
Stre
ngth
s:M
oder
ate:

338 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
et a
l. 20
01U
SA
Epi
/Pre
v/D
esc
Det
erm
ine
the
occu
renc
e an
d na
ture
of
slee
p-re
late
d br
eath
ing
diso
rder
s in
ad
ults
with
TB
I
Rec
ruitm
ent:
Pro
spec
tive
obse
rvat
ion-
al s
tudy
Con
secu
tive
AI;
Sin
gle
Gro
up
Incl
usio
n:•
18-6
5 yr
s•
<3 m
os p
ostin
jury
• R
anch
o ≥
3E
xclu
sion
:•
Pre
viou
sly
docu
-m
ente
d sl
eep
apne
a, n
arco
-le
psy
or h
abitu
al
snor
ing
• Tr
ache
osto
my
• H
isto
ry o
f oth
er
prem
orbi
d ne
uro-
logi
c or
pul
mo-
nary
con
ditio
ns
34.5
Gen
der:
25%
FG
CS:
low
est
durin
g th
e fir
st
24 h
rs; 7
1%
GC
S ≤
8, 2
5%
GC
S 9
-12,
4%
G
CS
> 1
2 P
TA >
1 d
ayR
anch
o 95
%Le
vel V
I or
VII
Tim
e si
nce:
<3
mos
slee
p st
udy
usin
g po
rta-
ble
6-ch
an-
nel m
onito
r-in
g sy
stem
; ca
lcul
ated
a
resp
irato
ry
dist
urba
nce
inde
x
brea
thin
g di
sord
ers
defin
ed b
y a
resp
irato
ry
inde
x of
5
or g
reat
er
seem
to b
e co
mm
on in
ad
ult s
ubje
cts
with
TB
I; E
vide
nce
of
slee
p ap
nea
was
foun
d in
36%
of
subj
ects
Pro
spec
tive
and
cons
ecut
ive
desi
gn; N
ew in
fo
rega
rdin
g th
e oc
-cu
rren
ce o
f sle
ep
apne
a in
ear
ly
reco
very
pha
se;
Atte
mpt
to e
limi-
nate
con
foun
ding
fa
ctor
sLi
mita
tions
:Low
po
wer
; Hom
oge-
neou
s sa
mpl
e;
Not
abl
e to
col
lect
E
EG
dat
a
4/7
Bas
elin
e: 0
.5B
lindi
ng: 0
.5
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0
Mas
el e
t al.
2001
US
ATy
pe:
Epi
/Pre
v/D
esc
Det
erm
ine
prev
alen
ce,
dem
ogra
phic
s,
and
caus
es o
f E
DS
in a
dults
w
ith B
I and
in
vest
igat
e re
latio
nshi
p be
twee
n su
bjec
tive
and
obje
ctiv
e da
ta
Leve
l III
Rec
ruitm
ent:
Con
secu
tive
AI
Cas
e se
ries
Cro
ss-s
ec-
tiona
lS
ingl
e gr
oup
2 ov
erni
ght
slee
p ev
alu-
atio
ns 1
wk
apar
t; ac
-tig
raph
y fo
r 2
wks
afte
r 2n
d P
SG
TBI =
71
Com
plet
e m
edic
al
hist
ory
and
phys
i-ca
l exa
min
atio
n;
Incl
usio
n: N
one
Exc
lusi
on: N
one
Age
, yrs
:32
± 1
1G
ende
r:38
% F
GC
S: o
nly
for
56%
: Non
hy
pers
omni
a (N
H):
6 ±
4;P
ost t
raum
atic
hy
pers
omni
a (P
TH):
7 ±
5;
Hyp
erso
mni
a w
ith a
bnor
mal
in
dice
s (H
AI):
8
± 5
Ran
cho
≥ Le
vel
IV Tim
e Si
nce:
38
± 6
0 m
os
Act
igra
phy
PS
G; M
SLT
; E
SS
; PS
QI;
Mill
on C
lini-
cal M
ultia
xial
In
vent
ory-
II (M
CM
-II);
Neu
rops
y-ch
olog
ic
batte
ry;
Dia
gnos
is o
f na
rcol
epsy
an
d po
st-
traum
atic
hy
pers
omni
a us
ing
the
ICS
D
Hyp
erso
mni
a w
as c
omm
on
with
hig
h pr
esen
ce o
f sl
eep
apne
a hy
popn
ea
synd
rom
e,
perio
dic
limb
mov
emen
ts,
and
PTH
; N
H: n
= 3
8;
PTH
: n =
21;
H
AI:
n =
12;
No
rela
tion-
ship
bet
wee
n hy
pers
omni
a gr
oups
and
G
CS
, psy
-ch
opat
holo
gy,
time
post
in-
jury
and
de
mog
raph
ic
Sug
gest
may
be
that
pat
ient
s w
ith
TBI h
ave
an in
-ab
ility
to p
erce
ive
thei
r hy
pers
omno
-le
nce
Lim
itatio
n: W
ide
rang
e of
tim
e po
stin
jury
; Sel
f-se
lect
ion
bias
Mod
erat
e:4/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze:
0.5
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0

339Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
varia
bles
; no
sign
ifica
nt
diffe
renc
es o
f no
te o
n th
e ne
urol
ogic
te
sts;
No
sign
ifica
nt
corr
elat
ion
betw
een
ES
S
or P
SQ
I and
M
SLT
Verm
a et
al
. 200
7 U
SA
Type
:E
pi/P
rev/
Des
cD
eter
min
e th
e sp
ec-
trum
of s
leep
di
sord
ers
in
patie
nts
with
ch
roni
c TB
I an
d de
term
ine
if th
e se
verit
y of
sle
ep d
isor
-de
r is
rel
ated
to
sev
erity
of
chro
nic
TBI
Leve
l VR
ecru
itmen
t:R
etro
spec
-tiv
e LC
(r
efer
red
for
eval
uatio
n fo
r sl
eep
diso
rder
); C
ross
-sec
-tio
nal;
Sin
gle
grou
p; O
ne
over
nigh
t P
SG
TBI =
60
Incl
usio
n: N
IE
xclu
sion
: NI
Age
, yrs
: 20
-69,
mea
n 41
Gen
der:
37%
FG
CS:
NI
Sev
erity
as-
sess
ed b
y G
AF:
mild
40%
mod
erat
e 20
%se
vere
40%
Tim
e si
nce:
3 m
os to
2 y
rs
Det
aile
d m
edic
al
hist
ory,
ne
urol
ogic
al
exam
, nec
k si
ze, c
hin
size
and
po
sitio
n, ja
w
alig
nmen
t, an
d or
pha-
ryng
eal
exam
inat
ion;
P
SG
; MS
LT;
ES
S; B
DI;
Ham
ilton
A
nxie
ty
Sca
le
A fu
ll sp
ec-
trum
of s
leep
di
sord
ers
occu
r in
pa
tient
s w
ith
chro
nic
TBI
Com
plic
ated
re
latio
nshi
p w
ith s
ever
ity
of in
jury
ED
S w
as
mos
t com
-m
on p
rese
nt-
ing
sym
ptom
, w
hich
may
le
ad to
oth
er
prob
lem
s lik
e in
som
nia,
an
xiet
y an
d de
pres
sion
Stre
ngth
s:Id
entifi
es a
nd
desc
ribes
the
spec
trum
of s
leep
di
sord
ers;
Sle
ep
dist
urba
nces
can
co
mpr
omis
e re
hab
proc
ess
and
retu
rn to
wor
k;
Lim
itatio
ns:
Ret
rosp
ectiv
e;
1 ni
ght o
f PS
G;
Lack
of e
xclu
sion
of
pos
sibl
e ef
fect
s of
med
s an
d pa
in;
HA
S a
nd B
DI
not c
olle
cted
on
all p
artic
ipan
ts;
GA
F m
ay n
ot b
e be
st e
valu
atio
n of
se
verit
y
Mod
erat
e:4/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze:
0.5
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0
Cas
triot
ta
& L
ai 2
001
US
A
Type
:E
pi/P
rev/
Des
cD
eter
min
eth
e fre
quen
cy
of s
leep
dis
or-
Leve
l III
Rec
ruitm
ent:
Pro
spec
tive
coho
rt st
udy;
Con
secu
tive
TBI =
10
Incl
usio
n:•
Sub
ject
ive
exce
s-si
ve s
leep
• ≥
18 y
rs o
r ol
der
Age
, yrs
:56
.3 ±
5.3
Gen
der:
60%
F;
GC
S: s
TBI 6
0%
Clin
ical
in
terv
iew
; E
SS
; PS
G;
MS
LT
Sle
ep
diso
rder
ed
brea
thin
g w
as fo
und
in
7 su
bjec
ts;
Stre
ngth
s:P
rosp
ectiv
eLi
mita
tions
:S
mal
l sam
ple
Mod
erat
e:3.
5/7
Bas
elin
e: 0
.5B
lindi
ng 0
Sam
ple
size
: 0

340 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
orde
rs a
ssoc
i-at
ed w
ith T
BI;
inve
stig
ate
rela
tions
hip
betw
een
post
traum
atic
sl
eep
dis-
orde
rs a
nd
pret
raum
atic
sl
eep
diso
r-de
rs
yet t
imin
g po
stin
-ju
ry u
ncle
ar-
Cro
ss-s
ec-
tiona
l; S
ingl
e gr
oup;
Use
cr
iterio
n
stan
dard
to
diag
nose
sl
eep
diso
r-de
rs; T
hose
w
ith o
vert
slee
p ap
nea
had
a 2n
d P
SG
with
tit
ratio
n of
na
sal C
PAP
• A
lert
and
ori-
ente
dE
xclu
sion
:•
Med
icat
ions
to
caus
e hy
pers
om-
nole
nce
• P
regn
ancy
• P
atie
nts
with
ca
rdio
pulm
o-na
ry a
nd r
ecen
t ab
dom
inal
and
th
orac
ic in
jurie
s
mTB
I: 40
%Ti
me
Sin
ce:
≥ 72
hrs
; 110
19
1 m
os
Ove
rt O
SA
in
5 su
bjec
tsN
acro
leps
y in
2
subj
ects
Trea
tabl
e sl
eep
diso
r-de
rs s
eem
to
be c
omm
on
in s
leep
y TB
I po
pula
tion
All
10 h
ad
treat
able
sl
eep
diso
r-de
rs; 3
had
sy
mpt
oms
of
hype
rsom
nia
befo
re in
jury
Attr
ition
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0
Cha
put
2009
C
anad
a
Type
:E
pi/P
rev/
Des
cA
sses
s th
e re
latio
nshi
ps
amon
g sl
eep
com
plai
nts,
he
adac
hes,
an
d m
ood
alte
ratio
n in
m
TBI
Leve
l III
Rec
ruitm
ent:
Ret
rosp
ec-
tive
char
t re
view
; C
onse
cutiv
e E
R; S
ingl
e gr
oup;
Lo
ngitu
di-
nal;
Dat
a re
vtrie
val
at 1
0 da
ys
and
6 w
ks;
Sel
f-rep
ort:
in o
rder
to
pre
vent
se
lect
ion
bias
, tho
se
patie
nts
asse
ssed
by
self-
repo
rt
TBI =
443
At 1
0 da
ys: 8
7.8%
At 6
wee
ks: 6
4.1%
Incl
usio
n•
See
n fo
r ≥
1 vi
sit w
here
pos
t-in
jury
sym
ptom
s w
ere
not d
ue to
al
coho
l or
othe
r ill
egal
sub
stan
ce,
or m
edic
atio
n, o
r ot
her
inju
ries,
or
2° to
trea
tmen
t of
othe
r in
jury
• m
TBI d
iagn
osis
by
neu
rosu
rgeo
n ba
sed
on ta
sk
forc
e cr
iteria
Exc
lusi
on:
• ≤
16 y
rs•
Lang
uage
bar
rier
Age
, yrs
:m
ean
46.9
Gen
der:
31.8
% F
Sev
erity
: m
TBI
GC
S: s
cene
: m
ean
13.2
(10
-da
y gr
oup)
and
15
(6-
wk
grou
p)E
mer
genc
y de
partm
ent:
13.9
(10
day
gr
oup)
and
15
(6-w
k gr
oup)
, 42
% a
bnor
mal
C
T-sc
anTi
me
sinc
e:
<10
days
pos
t-tra
uma
and
<6
wks
Rev
iew
of
past
med
i-ca
l his
tory
in
clud
ing
curr
ent
med
icat
ions
, kn
own
alle
r-gi
es, a
s w
ell
as s
mok
ing,
al
coho
l and
dr
ug in
take
ha
bits
; CT
scan
s w
ere
revi
ewed
if
pres
ent;
Riv
erm
ead
post
-co
ncus
sion
sy
mpt
om
asse
ssm
ent
ques
tionn
aire
Sle
ep c
om-
plai
nt p
reva
-le
nce:
13.
3%
and
33.5
%
(sig
nific
antly
m
ore
likel
y at
6
wks
); P
res-
ence
of s
leep
co
mpl
aint
s is
si
gnifi
cant
ly
asso
ciat
ed
with
hea
d-ac
hes,
de
pres
sive
sy
mpt
oms,
an
d fe
elin
g irr
itabl
e at
10
day
s an
d 6
wks
; Ear
ly
deve
lopm
ent
of s
ympt
oms
Lim
itatio
ns:
Did
not
ass
ess
cure
nt s
tress
ors;
S
ubje
ctiv
e na
ture
of
dat
a co
llect
ed
Mod
erat
e:3.
5B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 0S
tand
ardi
zed
outc
omes
: 0.5
Des
critp
ion:
0.
5Fo
llow
-up:
1

341Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
and
hist
ory
wer
e no
t ex
clud
ed
but r
ated
for
pres
ence
or
abse
nce
of
6 ty
pes
of
slee
p co
m-
plai
nts
Kno
wn
hist
ory
of
men
tal r
etar
da-
tion,
dia
gnos
is
dem
entia
or
lear
ning
dis
-ab
ility
impa
iring
th
e co
gniti
ve
and
reas
onin
g pr
oces
s, o
r co
-ex
istin
g ps
ychi
at-
ric il
lnes
s
may
in-
crea
se r
isk
of
chro
nici
ty o
f sy
mpt
oms
See
m to
in
dica
te a
n al
tera
tion
in s
leep
ho
meo
stat
-si
s fo
llow
ing
mTB
I des
pite
ab
senc
e of
ph
ysic
al p
ain
as p
rese
nted
at
10
days
Mak
ley
2009
US
ATy
pe:
Epi
/Pre
v/D
esc
Inve
stig
ate
whe
ther
im-
prov
emen
ts in
sl
eep
effic
ien-
cy c
orre
late
w
ith d
urat
ion
of P
TA a
fter
clos
ed h
ead
inju
ry
Leve
l IV
AR
ecru
itmen
t: P
rosp
ectiv
e;
Con
secu
tive
AI;
Sin
gle
grou
p;
Long
itudi
nal;
Act
igra
phy
with
in 7
2 hr
s of
adm
is-
sion
and
for
dura
tion
of
stay
(m
in
of 7
day
s);
Dai
ly m
ea-
sure
men
t of
PTA
; cle
ared
w
hen
O-
LOG
sco
re
of ≥
25
on
2 co
ns-
cutiv
e da
ys;
Follo
w-u
p
CH
I = 1
4E
xclu
sion
:•
Kno
wn
hist
ory
of
a sl
eep
diso
rder
, an
oxic
inju
ry,
activ
e ps
ychi
atric
ill
ness
, obe
sity
, un
treat
ed th
yroi
d di
seas
e, d
egen
-er
ativ
e ne
urol
ogic
co
nditi
on, s
igni
fi-ca
nt te
trapa
resi
s or
imm
obili
ty
Age
:24
-45
yrs
Gen
der:
NI
GC
S: N
ITi
me
sinc
e: 1
5 da
ys (
9-23
)
Com
plet
e ne
urol
ogic
an
d ph
ysic
al
exam
inat
ion
on a
dmis
-si
on; F
IM
at a
dmis
-si
on a
nd
disc
harg
e;
Act
igra
phy;
O
-LO
G to
m
easu
re
PTA
by
SLP
s bl
ind-
ed to
sle
ep
scor
es; B
ed-
side
sle
ep
logs
kep
t by
nurs
ing
staf
f; Fo
llow
-up:
DR
S; S
uper
-vi
sion
Rat
ing
Sca
le
78%
had
m
ean
Wee
k-1
slee
p ef
ficie
ncy
in
the
seve
rely
im
paire
d ra
nge;
Tho
se
adm
itted
hav
-in
g al
read
y cl
eare
d P
TA
had
sign
ifi-
cant
ly b
ette
r W
eek-
1 sl
eep
effic
ienc
y th
at
thos
e w
ith
ongo
ing
am-
nesi
a; T
hose
w
ith o
ngoi
ng
amne
sia:
ea
ch 1
0-un
it
incr
ease
in
slee
p ef
fi-ci
ency
cor
re-
Act
igra
phy
a go
od
met
hod
to m
ea-
sure
sle
ep p
at-
tern
s in
imm
edia
te
post
-acu
teS
treng
ths:
Effo
rt m
ade
to
mea
sure
/elim
inat
e po
tent
ial c
on-
foun
ding
var
iabl
esLi
mita
tions
:S
mal
l sam
ple
with
la
rge
attri
tion
(onl
y 9
avai
labl
e fo
r an
alys
is)
Mod
erat
e:3.
5B
asel
ine:
0.5
Blin
ding
: 0.5
Sam
ple
size
: 0A
ttriti
on: 0
Sta
ndar
dize
d ou
tcom
es: 0
.5D
escr
itpio
n: 1
Follo
w-u
p: 1

342 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
3 m
osS
WLS
;P
SQ
Ila
ted
with
1
unit
↑ in
O-
LOG
sco
reA
ssoc
iatio
n be
twee
n im
prov
e-m
ent i
n sl
eep
effic
ienc
y an
d re
turn
of
awar
enes
s >
for
thos
e ad
mitt
ed w
ith
PTA
Wor
thin
g-to
n &
Mel
ia
2006
UK
Type
:E
pi/P
rev/
Des
cIn
vest
igat
e th
e im
pact
of
diso
rder
s of
ar
ousa
l and
sl
eep
dis-
turb
ance
on
ever
yday
livi
ng
and
parti
cipa
-tio
n in
reh
abili
-ta
tion
Leve
l VR
ecru
itmen
t:R
etro
-sp
ectiv
e na
tura
listic
ob
serv
atio
n;
Rec
ruitm
ent
AI (
7 ce
n-te
rs);
Cro
ss-
sect
iona
l; S
ingl
e gr
oup
AB
I = 1
35In
clus
ion:
• A
dmis
sion
to s
er-
vice
on
grou
nds
of s
igni
fican
t co
gniti
ve a
nd/o
r be
havi
or d
isor
der
• S
ever
e B
I•
All
able
to p
artic
i-pa
te in
reh
abE
xclu
sion
: NI
Age
, yrs
:38
± 1
1.4
Gen
der:
25%
FG
CS:
rang
e, 3
-7Ti
me
sinc
e:11
9.3
± 10
8.8
mos
Stru
ctur
ed
ratin
g fo
rm:
5 ke
y fe
a-tu
res
incl
ud-
ing
dela
yed
slee
p on
set,
frequ
ent
wak
ing
at
nigh
t, ea
rly
mor
ning
w
akin
g, d
e-la
yed
mor
n-in
g w
akin
g,
and
ED
S
47%
dis
-tu
rban
ce o
f ar
ousa
l and
sl
eep
pat-
tern
s; S
igni
fi-ca
nt a
dver
se
effe
ct o
n ac
tivity
in
66%
of 4
7%;
Dis
orde
red
arou
sal c
ould
pe
rsis
t up
to 1
0 yr
s po
st-in
jury
; C
oncu
rren
t ps
ychi
atric
ill-
ness
, but
not
ep
ileps
y, w
as
asso
ciat
ed
with
aro
usal
an
d sl
eep
diso
rder
; N
onph
ar-
mac
olog
ical
in
terv
entio
ns
Stre
ngth
s:
Firs
t siz
eabl
e st
udy
to a
ddre
ss
the
impa
ct a
nd
man
agem
ent o
f ar
ousa
l dis
orde
rs
afte
r B
I
Mod
erat
e:3/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0D
escr
itpio
n:
0.5
Follo
w-u
p: 0

343Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
used
in 3
4%
of c
ases
ben
-zo
dias
epin
e/hy
pnot
ic
drug
s 20
%Lo
ng-te
rm
outc
ome
from
sB
I affe
cted
by
end
urin
g di
stur
banc
e of
aro
usal
, m
ost c
om-
mon
ly n
oted
as
sle
ep
diso
rder
Path
ophy
siol
ogy
Ayal
on e
t al
. 200
7 U
SA
Type
:P
atho
phys
iol-
ogy
D
escr
ibe
the
phys
iolo
gic
and
beha
vior
al
char
acte
ristic
s of
CR
SD
s fo
llow
ing
mTB
I in
pat
ient
s co
mpl
aini
ng o
f in
som
nia
Leve
l III
Rec
ruitm
ent:
LC; D
escr
ip-
tive;
Coh
ort;
Cro
ss-s
ec-
tiona
l; D
ata
colle
ctio
n ev
ery
2 hr
s fo
r 24
hrs
TBI =
42
Age
, yrs
:m
ean
26(r
ange
, 17-
45)
Gen
der:
20%
FG
CS:
mTB
ITi
me
sinc
e: N
I
Act
igra
phy;
S
aliv
a m
ela-
toni
n; O
ral
tem
pera
ture
; P
SG
; Sel
f-re
port
ques
-tio
nnai
re to
de
term
ine
circ
adia
n pr
efer
ence
: m
orni
ng-
ness
-eve
-ni
ngne
ss
ques
tion-
naire
36%
had
C
RS
D; 1
9%
had
DS
PS
: sh
owed
↑
tem
p, r
hyth
m,
ampl
itude
; 17
% h
ad ir
-re
gula
r sl
eep-
wak
e pa
ttern
: ha
d w
eake
r ci
rcad
ian
rhyt
hmic
-ity
- a
ccou
nt
for
beha
vior
di
ffere
nces
in
slee
p-w
ake
patte
rn?
Dis
tinct
pro
-fil
es o
f 24-
hr
perio
dici
ty
of m
elat
onin
rh
ythm
and
mTB
I mig
ht c
on-
tribu
te to
em
er-
genc
y of
CR
SD
s;
Impo
rtant
to h
ave
corr
ect d
iagn
osis
or
can
inap
pro-
pria
tely
trea
t for
in
som
nia
Mod
erat
e:4.
5/7
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 1A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0

344 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
24-h
r pe
riod-
icity
of o
ral
tem
pera
ture
Bau
man
n et
al.
2005
S
witz
erla
nd
Type
:P
atho
phys
iol-
ogy
A
sses
s th
e C
SF
hypo
cre-
tin-1
leve
ls in
pa
tient
s w
ith
TBI
Leve
l III
Rec
ruitm
ent:
Con
secu
tive
A; C
ohor
t; C
ross
-sec
-tio
nal;
Dat
a co
llect
ion
1-4
days
po
st-T
BI
TBI =
44
Con
trols
= 2
0 (n
o ne
urol
ogic
pro
b-le
ms)
Incl
usio
n:•
Acu
te T
BI,
1-4
days
pos
t-inj
ury
Exc
lusi
on: N
I
Age
, yrs
:m
ean
36
(ran
ge, 1
7-69
)G
ende
r:73
% F
GC
S: 3
1 sT
BI;
8 m
od T
BI;
5 m
TBI
Tim
e si
nce:
1-4
days
TBI:
Hyp
o-cr
etin
-1
leve
ls a
s-se
ssed
ven
-tri
cula
r C
SF
(n =
37)
and
sp
inal
CS
F (n
= 8
) by
ra
dioi
mm
u-no
assa
yC
ontro
ls:
leve
ls a
s-se
ssed
vi
a sp
inal
an
aest
hesi
a an
d so
me
vent
ricul
arU
sed
Mar
shal
l to
cate
goriz
e th
e C
T
Hyp
ocre
tin-1
le
vels
abn
or-
mal
ly lo
w in
95
% o
f mod
-s
TBI a
nd in
97
% o
f tho
se
with
pos
ttrau
-m
atic
bra
in
CT
chan
ges;
S
ite o
f CS
F sa
mpl
e di
d no
t mat
ter;
Mar
shal
l I: 8
, II-
IV: 3
6n
= 9
con-
com
itant
di
seas
es
Cha
nge
in le
vels
m
ay r
eflec
t hyp
o-th
alm
ic d
amag
e an
d m
ay b
e lin
ked
to S
WD
May
als
o re
flect
lo
ss o
f con
scio
us-
ness
Lim
itatio
n:S
mal
l sam
ple
Mod
erat
e:4/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze:
0.5
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
itpio
n: 1
Follo
w-u
p: 0
Qui
nto
et
al. 2
000
US
A
Type
:P
atho
phys
iol-
ogy
D
escr
ibe
the
expe
rienc
e of
D
SP
S in
AB
I
Leve
l IVA
Rec
ruitm
ent:
LC; S
ingl
e su
bjec
t cas
e st
udy
TBI =
1S
leep
ons
et in
som
-ni
a: n
ot r
espo
nsiv
e to
pha
rmac
olog
ical
tre
atm
ent
Age
, yrs
: 48 G
ende
r:M
ale
GC
S: N
ITi
me
sinc
e: N
I
Sle
ep lo
gsA
ctig
raph
yS
leep
ons
et
inso
mni
a w
ith fr
eque
nt
awak
en-
ings
; Chr
o-no
ther
apy
unsu
cces
sful
de
clin
ed;
Pho
toth
erap
y de
clin
ed
Aut
hors
hyp
oth-
esiz
e le
sion
to
supr
achi
asm
atic
nu
cleu
s, w
hich
is
the
site
of h
uman
ci
rcad
ian
cloc
kE
mph
asiz
ed n
eed
to b
e aw
are
of
DS
PS
as p
oten
tial
cons
eque
nce
of
AB
I whe
n di
-ag
nosi
ng s
leep
pr
oble
ms
Mod
erat
e:3.
5/7
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0

345Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
Pedi
atric
Bee
be e
t al
. 200
7 U
SA
Type
:P
edia
tric
Det
erm
ine
the
effe
ct o
f mod
an
d se
vere
TB
I on
slee
p of
sch
ool-a
ged
child
ren
Leve
l III
Rec
ruitm
ent:
Con
curr
ent
pros
pec-
tive
coho
rt A
(chi
l-dr
en a
ged
6-12
yrs
); Lo
ngitu
dina
l 3
grou
ps:
mod
TBI,
sTB
I, or
tho-
paed
ic in
ju-
ry; B
asel
ine
(ret
rosp
ec-
tive
pare
ntal
re
port
of
prei
njur
y sl
eep
at 3
w
ks p
ost),
an
d 6,
12,
an
d 48
mos
po
st-in
jury
mod
TB
I = 5
6sT
BI =
35
Con
trols
= 8
0In
clus
ion:
• 1
nigh
t in
hosp
tial
for
all 3
gro
ups
• N
o ev
iden
ce o
f ab
use
or p
revi
-ou
s ne
urol
ogic
al
diso
rder
• E
nglis
h-sp
eaki
ng
Age
at i
njur
y,
yrs:
9.5
± 2.
0G
ende
r:33
% F
GC
S: u
sed
low
est p
ost-
resu
scita
tion/
inju
ry s
core
Tim
e si
nce:
3
wks
pos
tO
ther
:68
% C
auca
sian
Chi
ld
Beh
avio
ur
Che
cklis
t: 7
item
s on
ly
(ass
esse
d st
abili
ty in
co
mpa
risio
n to
full
scal
e)
mod
TBI
wor
se p
re-
inju
ry s
leep
m
odTB
I and
C
ontro
ls:
smal
l ↓ in
sl
eep
from
pr
e to
pos
t; sT
BI:
↑ in
po
stin
jury
pr
oble
ms:
da
ytim
e sl
eepi
ness
an
d no
ctur
nal
slee
p du
ra-
tion
Lim
itatio
ns:
Tim
ing
of fo
llow
-up
s va
ried;
R
etro
spec
tive
data
co
llect
ion;
Wea
k in
stru
men
t (on
ly 7
ite
ms
and
part
of
larg
er s
cale
)
Mod
erat
e:4.
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 0S
tand
ardi
zed
outc
omes
: 0.5
Des
critp
ion:
1Fo
llow
-up:
1
Kau
fman
et
al.
2001
Is
rael
Type
:P
edia
tric
Sub
ject
ive
and
obje
ctiv
e ch
arac
teriz
a-tio
n th
e lo
ng
term
effe
cts
of
mH
I on
slee
p in
ado
lesc
ents
Leve
l III
Rec
ruitm
ent:
Pro
spec
tive
coho
rt A
(arc
hive
s);
Cro
ss-s
ec-
tiona
l; m
HI:
subj
ectiv
e an
d ob
jec-
tive
mea
-su
res
C1,
C
2: o
bjec
-
mH
I = 1
9C
1 (h
ealth
y) =
16
C2
(hea
lthy)
= 1
5In
clus
ion
• 10
-18
yrs
• H
ospi
tal a
dmis
-si
on w
ith m
HI
(ICD
-10
code
s)•
GC
S ≥
13
• 3
yrs
post
inju
ry•
Com
plai
ned
of
slee
p di
stur
banc
e
Age
, yrs
:13
.5 ±
1.7
Gen
der:
mH
I21
% F
;C
1 19
% F
C2
20%
FG
CS
: ≥ 1
3Ti
me
sinc
e: 3
yr
s po
st-in
jury
Loca
lly
deve
lope
d qu
estio
n-na
ire: m
edi-
cal h
isto
ry,
deta
ils o
f th
e in
jury
, sl
eep
habi
ts,
and
slee
p di
stur
banc
-es
: pre
and
po
st s
leep
mH
I: si
g-ni
fican
t ↓ in
sl
eep
perio
d tim
e, to
tal
slee
p tim
e an
d sl
eep
ef-
ficie
ncy;
mH
I: si
gnifi
cant
↑
min
aw
ake
and
num
ber
of a
wak
en-
ings
>3
min
Stre
ngth
s:Th
roro
ugh
eval
uatio
n; U
se o
f he
alth
y co
ntro
ls;
Sub
ject
ive
cor-
robo
rate
d ob
jec-
tive
for
the
mos
t pa
rt; P
artic
ipan
ts
3 yr
s po
st-in
jury
so
idei
ntifi
es/c
on-
firm
s lo
ng-te
rm
slee
p pr
oble
ms
Mod
erat
e:3.
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0.5
Des
critp
ion:
1Fo
llow
-up:
0

346 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
tiv
e on
ly;
C1,
C2
mat
ched
for
age,
gen
der;
recr
uite
d by
ad
verti
se-
men
t, w
ord
of m
outh
; O
ne d
ata
colle
ctio
n,
incl
udin
g 5
days
of
actig
raph
y
Exc
lusi
on: N
IP
SG
(m
HI
and
C1)
: 1
nigh
t; A
ctig
-ra
phy
(mH
I an
d C
2): 5
da
ys w
ithin
3
mos
of
PS
G
mH
I: su
bjec
-tiv
e re
port
diffi
culty
fa
lling
asl
eep,
di
fficu
lty
wak
ing
in th
e m
orni
ng, d
ay-
time
slee
pi-
ness
, res
tless
sl
eep,
fear
ful
awak
enin
gs
from
sle
ep,
para
som
nias
Lim
itatio
ns:
Sm
all s
ampl
e bu
t re
flect
ive
of th
e re
aliti
es o
f thi
s ty
pe o
f res
earc
h
Milr
oy e
t al.
2007
UK
Type
:P
edia
tric
Obt
ain
ob-
ject
ive
and
subj
ectiv
e re
-po
rts o
f sle
ep
dist
urba
nces
in
sch
ool-a
ged
child
ren
with
m
TBI
Leve
l III
Rec
ruitm
ent:
A (fr
om
data
base
); C
ross
-se
ctio
nal;
2 gr
oups
: m
TBI a
nd
orth
opae
dic
cont
rols
with
in
jury
to
wris
t or
arm
mTB
I = 1
8 (4
3% o
f ad
mis
sion
s)C
ontro
ls =
30
(61%
of
adm
issi
ons)
Incl
usio
n:•
7-12
yrs
• ≥
6 m
os s
ince
la
st h
ospi
tal a
t-te
ndan
ce•
Adm
issi
on <
48
hrs
Exc
lusi
on:
• D
evel
opm
enta
l de
lay,
epi
leps
y,
psyc
hiat
ric, o
r sl
eep
diso
rder
s•
Atte
nds
a sp
ecia
l sc
hool
• O
ther
rec
ent
hosp
italiz
atio
n•
His
tory
of n
onac
-ci
dent
al in
jury
Age
, yrs
: m
ean
TBI:
9.7
± 1.
5C
ontro
ls:
9.7
± 1.
5G
ende
r:TB
I 56%
F,
Con
trols
40%
FG
CS:
GC
S o
f 15
= 16
GC
S o
f 13
= 1
GC
S o
f 14
= 1
2% r
ecor
ded
PTA Tim
e si
nce:
23
.9 m
os; C
on-
trols
25
mos
Act
igra
phy
for
5 ni
ghts
; P
aren
tal a
nd
self-
repo
rt qu
estio
n-na
ires:
Chi
l-dr
en’s
Sle
ep
Hab
its; S
elf-
repo
rt S
leep
S
cale
S
treng
ths
and
diffi
cul-
ties;
Dem
o-gr
aphi
c an
d in
jury
-rel
ated
qu
estio
ns
mTB
I: P
ar-
ents
rep
ort >
sl
eep
dist
ur-
banc
es w
hen
com
pare
d to
C
ontro
ls (
me-
dium
effe
ct
size
); m
TBI
and
Con
trols
: di
d no
t diff
er
on m
easu
res
of s
leep
ef-
ficie
ncy
Hig
her
porti
on in
bo
th g
roup
s w
ith
slee
p di
fficu
lties
th
an e
xpec
ted
Diff
eren
ces
betw
een
pare
ntal
re
port
and
obje
c-tiv
e m
easu
res
of
inte
rest
as
thes
e m
easu
res
serv
e di
ffere
nt p
urpo
ses
and
may
iden
tify
diffe
rent
type
s of
sl
eep
diffi
culti
es;
Sel
f sel
ectio
n bi
as
poss
ible
Mod
erat
e:4/
7B
asel
ine:
1B
lindi
ng: 0
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
critp
ion:
1Fo
llow
-up:
0
Nec
ajau
s-ka
ite e
t al.
Type
:P
edia
tric
Leve
l III
Rec
ruitm
ent:
TBI =
102
Con
trols
= 1
02A
ge, y
rs:
4-16
Loca
lly d
e-ve
lope
d16
.7%
of p
ar-
ents
rep
orte
d Li
mita
tions
:C
riter
ia m
easu
red
Mod
erat
e:3.
5/7

347Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
2005
Li
thua
nia
Inve
stig
ate
the
clin
ical
fe
atur
es a
nd
prev
alen
ce
of s
ympt
oms
of P
CS
in
child
ren
with
m
TBI a
nd
eval
uate
ch
ange
s ov
er
time
A; C
ross
-se
ctio
nal;
Two
grou
ps:
TBI:
sing
le
mTB
I; C
on-
trols
: mild
bo
dy in
jury
; 2
ques
tion-
naire
s m
aile
d se
para
tely
: fir
st, f
or
perio
d du
r-in
g th
e la
st
year
and
du
ring
the
last
mon
th
with
no
ref
to tr
aum
a (to
red
uce
bias
); se
c-on
d (ju
st
TBI g
roup
) fo
r pe
riod
shor
tly a
fter
the
traum
aC
ompa
red
thos
e <2
yrs
po
st-in
jury
to
thos
e 2-
5 yr
s po
st-
inju
ry
Gro
ups
mat
ched
on
gen
der,
age,
da
te o
f adm
issi
on
Gen
der:
28%
FG
CS:
NI
Tim
e si
nce:
1-5
yr
s po
st a
dmis
-si
on
stan
dard
ized
qu
estio
n-na
ire a
d-dr
essi
ng:
heal
th a
nd
sym
ptom
s (ir
ritab
ility
, fe
ars,
sle
ep
diso
rder
s,
lear
ning
pr
oble
ms,
co
ncen
-tra
tion
prob
lem
s,
mem
ory
diso
rder
s,
head
ache
s,
and
con-
com
itant
sy
mpt
oms
prio
r to
tra
uma)
slee
p pr
ob-
lem
s sh
ortly
af
ter
head
tra
uma
wer
e no
t rel
i-ab
le e
stim
ates
of
long
-last
ing
PC
S;
Wea
k m
easu
res;
O
nly
1 da
ta
colle
ctio
n fro
m
Con
trols
; Ret
ro-
spec
tive;
pos
sibl
e is
sues
of r
ecal
l bi
as
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0D
escr
iptio
n:
0.5
Follo
w-u
p: 0
Kor
inth
en-
berg
et
al. 2
004
Ger
man
y
Type
:P
edia
tric
Inve
stig
ate
pred
ictiv
e fa
c-to
rs o
f pos
t-
Leve
l III
Rec
ruitm
ent
Pro
spec
tive
coho
rt C
on-
secu
tive
A
mH
I = 9
8In
clus
ion:
• LO
C <
10 o
r no
ne•
Abl
e to
ans
wer
qu
estio
ns a
t
Age
, yrs
:3-
5 (n
= 2
6),
6-9
(n =
42)
,10
-13
(n =
30)
Gen
der:
EE
GP
roto
col o
f “e
xam
inat
ion
of c
hild
with
m
inor
neu
ro-
At f
ollo
w-u
p:
23%
pre
-se
nted
with
so
mat
ic a
nd
psyc
hiat
ric
Stre
ngth
s:La
rge
sam
ple
size
Thor
ough
in-
vest
igat
ion
with
fo
llow
-up
Mod
erat
e:5/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze: 1

348 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
traum
atic
sy
ndro
me
in
child
ren
with
m
HI
(use
d sp
e-ci
fic c
riter
ia);
Long
itudi
nal;
Obj
ectiv
e an
d su
bjec
-tiv
e m
ea-
sure
sD
ata
col-
lect
ion:
ba
selin
e an
d fo
llow
-up
at
4-6
wks
adm
issi
on•
No
com
plic
a-tio
ns, c
onfu
sion
or
intra
cran
ial
hem
orrh
age
• A
ge 3
-13
yrs
• C
hild
and
par
ents
sp
eak
Ger
man
, pa
rent
ava
ilabl
e fo
r in
terv
iew
Exc
lusi
on: N
I
40%
GC
S: N
ITi
me
sinc
e:
<24
hrs
sinc
e ad
mis
sion
logi
cal
dysf
unct
ion”
; S
truct
ured
va
lidat
ed
inte
rvie
w
com
plai
nts
in-
clud
ing
slee
p di
stru
banc
e an
d fa
tigue
, w
hich
did
no
t cor
rela
te
with
som
atic
, ne
urol
ogic
, or
EE
G fi
ndin
gs
imm
edia
tely
po
stin
jury
Lim
itatio
ns:
Bet
ter
with
a fu
r-th
er fo
llow
-up
Attr
ition
:1
Sta
ndar
dize
d ou
tcom
es: 1
Des
crip
tion:
1Fo
llow
-up:
0.5
Pill
ar e
t al.
2003
Isra
elTy
pe:
Ped
iatri
cA
sses
s th
e pr
eval
ence
an
d ris
k fa
c-to
rs o
f lon
g-te
rm s
leep
di
stur
banc
es
in a
dole
scen
ts
afte
r m
HI
Leve
l III
Rec
ruitm
ent:
Ret
rosp
ec-
tive
coho
rt A
(“ra
ndom
” se
lec-
tion
from
ar
chiv
es);
Cro
ss-
sect
iona
l; M
atch
ed
cont
rolle
d co
mpa
ri-si
on g
roup
(h
ealth
y)
mH
I = 9
8C
ontro
ls =
80
Incl
usio
n:•
7-15
yrs
at i
njur
y•
Adm
itted
to h
osp-
tial w
ith m
HI
• IC
D-1
0 co
des
506.
0•
GC
S ≥
13
on
adm
issi
on to
ER
Exc
lusi
on: N
I
Age
, yrs
: 13
.5 ±
2.3
(ran
ge, 8
-18)
Gen
der:
32%
FG
CS:
14.
7 ±
0.6
on a
dmis
-si
onTi
me
sinc
e:0.
5-6
yrs
Det
aile
d 60
-ite
m q
ues-
tionn
aire
mH
I: 28
%
had
slee
p pr
oble
ms
(vs
Con
trols
11
%; P
<
.05)
; mH
I >
Con
trols
: av-
erag
e sc
ore
of s
leep
co
mpl
aint
s (P
<
.05)
; mH
I w
ith s
leep
co
mpl
aint
s (n
=
27)
had
> bo
dy w
eigh
t, >
BM
I, pa
rent
s le
ss
educ
ated
, ↑
brux
ism
, sh
orte
d w
eeke
nd
slee
p tim
e
Stre
ngth
s:La
rge
sam
ple
Com
preh
ensi
ve
ques
tionn
aire
; La
rge
rang
e po
st-
inju
ry; C
ompa
ri-si
on g
roup
Lim
itatio
ns:
2/3
resp
onse
rat
eN
o in
form
atio
n on
BM
I at t
ime
of
inju
ry
Low
:2.
5/7
Bas
elin
e: 1
Blin
ding
: 0S
ampl
e si
ze: 1
Attr
ition
: 0S
tand
ardi
zed
outc
omes
: 0D
escr
itpio
n:
0.5
Follo
w-u
p: 0
Neu
rops
ycho
logy
Mah
moo
d et
al.
2004
.Ty
pe:
Neu
rops
y-Le
vel I
VAR
ecru
itmen
t:TB
I = 8
7In
clus
ion:
Age
, yrs
:N
IP
SQ
I, B
DI;
Glo
bal s
cale
37%
had
sl
eep
dist
ur-
PS
QI b
ette
r at
id
entif
ying
inso
m-
Mod
erat
e:4.
5/7

349Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
US
Ach
olog
y
Exa
min
e th
e re
latio
nshi
p be
twee
n sl
eep
dist
urba
nces
an
d ne
uroc
og-
nitiv
e ab
ility
po
st-T
BI
Con
secu
tive
AI (
arch
ival
re
cord
s)
Cor
rela
tiona
l C
ross
-sec
-tio
nal
• TB
I bas
ed o
n m
edic
al e
xam
, re
cove
ry to
pos
t-ac
ute
phas
e,
med
ical
ly d
eter
-m
ined
nee
d fo
r re
hab,
cog
nitiv
e fu
nctio
n at
Lev
el
VI (
Leve
ls o
f C
ogni
tive
Func
-tio
n S
cale
)•
Indi
catio
n of
at
leas
t a c
oncu
s-si
on (
LOC
or
conf
usio
n or
po
sitiv
e ne
uroi
m-
agin
g)E
xclu
sion
: NI
Gen
der:
43
.7%
FG
CS:
mild
: 24;
m
od 1
9; s
ev 4
4Ti
me
sinc
e:
97%
with
in a
ye
ar o
f inj
ury;
89
.7%
with
in
6 m
os; 7
0.1%
w
ithin
3 m
os
form
; M
emor
y A
sses
smen
t; S
cale
s; N
eu-
rops
ycho
l-og
y te
sts:
W
ide
rang
e;
Ach
ieve
men
t te
st; (
WR
AT-
3) -
est
imat
e of
pre
mor
bid
IQ; D
igit
Spa
n; D
igit
Sym
bol;
Gro
oved
P
eg B
oard
; B
lock
De-
sign
; Tra
il m
akin
g-B
; C
ontro
lled
Ora
l Wor
d A
sso-
ciat
ion
Test
(C
OW
AT)
banc
es m
TBI
mor
e sl
eep
dist
urbe
d th
an s
ever
eP
erfo
rman
ce
on s
elec
ted
mea
sure
s of
cog
nitiv
e fu
nctio
n ↑
pred
ictio
n of
sle
ep
dist
urba
nce
acco
unt-
ing
for
14%
of
var
ianc
e be
yond
that
ac
coun
ted
by
inju
ry s
ever
ity
and
gend
er
(17%
); E
xecu
tive
func
tioni
ng
and
spee
d of
in
form
atio
n pr
oces
sing
di
fficu
lties
m
ay b
e as
-so
ciat
ed w
ith
slee
p di
stur
-ba
nces
nia
but m
ay h
ave
not h
ave
capt
ured
hy
pers
omni
aN
eed
a re
liabl
e in
dica
tor
bette
r ab
le to
det
ect
and
repo
rt sl
eep
dist
urba
nces
Nee
d to
furth
er
asse
ss th
e in
flu-
ence
of g
ende
r; ex
plor
e th
e th
resh
old
leve
l an
d ch
ange
s ov
er
time
Bas
elin
e: 0
.5B
lindi
ng: 0
Sam
ple
size
: 1A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
crip
tion:
1Fo
llow
-up:
0
Wild
e et
al.
2007
US
ATy
pe:
Neu
rops
ycho
l-og
yE
xam
ine
the
impa
ct o
f co
mor
bid
OS
A on
cog
nitiv
e
Leve
l III
Rec
ruitm
ent:
PA (
3 ce
n-te
rs, s
leep
di
sord
er
cent
ers,
and
a
reha
b
TBI =
35
OS
A =
19N
o O
SA
= 16
Incl
usio
n:•
> 18
yrs
• ≥
3 m
os p
ost-
inju
ry
Age
, yrs
:>1
8G
ende
r:O
SA
: 11%
FN
o O
SA
: 25%
FG
CS:
OS
A 53
%
unkn
own,
16%
Neu
rops
y-ch
olog
ical
pe
rfor-
man
ce:
Psy
chom
o-to
r Vi
gila
nce
test
OS
A ↓
on v
erba
l an
d vi
sual
de
laye
d-re
call
mea
sure
s an
d >
atte
n-tio
n la
pses
Stre
ngth
s:Fi
rst s
tudy
to a
d-dr
ess
this
issu
eO
SA
asso
ciat
ed
with
mor
e im
pair-
men
t of s
usta
ined
at
tent
ion
and
Mod
erat
e:
4/7
Bas
elin
e: 1
B
lindi
ng: 0
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d

350 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
func
tion
of p
er-
sons
with
TB
Ipr
ogra
m)
Cas
e co
ntro
lled;
C
ross
-se
ctio
nal;
2 TB
I gro
ups:
O
SA
and
No
OS
A; C
on-
trolle
d us
ing
age,
edu
ca-
tion,
tim
e po
stin
jury
, an
d se
verit
y of
inju
ry a
nd
GC
S (
whe
n av
ail);
OS
A di
agno
sed
by n
octu
rnal
P
SG
Exc
lusi
on: N
Im
od, 5
% m
od-
sev,
26%
sev
; N
o O
SA
: 50%
; un
know
n, 1
2%
mod
, 19%
mod
-se
v, 1
9% s
evTi
me
sinc
e: ≥
3
mos
pos
t-inj
ury
Rey
Com
-pl
ex F
igur
e R
ey A
udi-
tory
-Ver
bal
Lear
ning
; D
igit
Spa
n fro
m W
MS
-R
; Fin
ger
tapp
ing;
E
SS
on
nigh
t of P
SG
an
d M
SLT
Effe
ct
size
s us
ing
Coh
en’s
d
med
ium
and
la
rge
mem
ory;
Tre
at-
men
t of O
SA
did
not i
mpr
ove
outc
omes
Lim
itatio
ns:
Lack
ed d
ata
on
leve
ls o
f sev
erity
, di
fficu
lt to
gen
eral
-iz
e fin
ding
s; S
mal
l sa
mpl
e bu
t effe
ct
size
s go
od
outc
omes
:1D
escr
iptio
n: 1
Follo
w-u
p: 0
Wis
eman
-H
akes
et
al. 2
010
Can
ada
Type
:N
euro
psyc
hol-
ogy
A
sses
s as
pect
s of
co
gniti
on a
nd
com
mun
icat
ion
over
a c
ours
e of
trea
tmen
t fo
r P
TH
Leve
l IVA
Rec
ruitm
ent:
LC Sin
gle
case
st
udy
Trea
tmen
t: 17
wks
1)
Bas
elin
e:
12 m
os
post
inju
ry,
lora
zepa
m
1 m
g an
d ci
talo
pram
20
mg
for
1 m
o 2)
At
1 yr
1 m
o,
cita
lopr
am ↑
40
mg
3) A
t 1
yr 2
mos
:
TBI =
1A
ge, y
rs:
late
teen
sG
ende
r: m
ale
GC
S: in
itial
3,
hosp
ital 5
PTA
> 1
mo
Tim
e si
nce:
11
mos
Dai
ly C
ogni
-tiv
e-C
omm
u-ni
catio
n an
d S
leep
Pro
file
(D-C
CA
SP
)E
SS
Sta
nfor
d S
leep
ines
s S
cale
PS
GM
aint
enan
ce
of W
akef
ul-
ness
Tes
ting
(MW
T) (
at
follo
w-u
p)
Rel
atio
nshi
p be
twee
n qu
ality
of
slee
p an
d la
ngua
ge p
ro-
cess
ing
Pro
long
ed
RE
M la
tenc
yP
ositi
ve r
ela-
tions
hip
be-
twee
n sl
eep
and
lang
uage
pr
oces
sing
, su
stai
ned
atte
ntio
n/vi
gila
nce,
m
emor
y an
d ch
ange
s in
m
edic
atio
n
Lim
itatio
ns:
Sin
gle
case
stu
dy
and
expl
orat
ory
in
natu
re
Mod
erat
e:
4/7
Bas
elin
e: 0
.5
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0.5
Des
crip
tion:
1Fo
llow
-up:
0

351Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
add
met
h-yl
phen
idat
e 20
mg;
4)
1 w
eek
late
r m
ethy
lphe
-ni
date
↑ 4
0 m
g da
ily 5
) S
leep
Stu
dy
2: m
odafi
nil
repl
aced
m
ethy
lphe
-ni
date
and
m
irtaz
epin
e w
as a
dded
Bas
elin
e, 1
7 w
ks d
aily
da
ta c
olle
c-tio
n, fo
llow
-up
at 3
yrs
8
mos
Able
to
impr
ove
daily
fu
nctio
ning
an
d re
sum
e at
tend
ance
at
scho
ol
Hen
ry e
t al.
2000
US
ATy
pe:
Neu
rops
ycho
l-og
yTo
inve
stig
ate
neur
opsy
-ch
olog
ical
, ps
ycho
logi
cal
and
beha
vior
al
func
tioni
ng
follo
win
g no
n-im
pact
BI
Leve
l VR
ecru
itmen
t:R
etro
spec
-tiv
e O
R
Cro
ss-s
ec-
tiona
lIn
terv
iew
ed
at o
ne p
oint
in
tim
eC
ompa
red
with
pub
-lis
hed
norm
s
Non
impa
ct T
BI
= 32
Incl
usio
n:•
His
tory
of w
hip-
lash
with
brie
f or
no
LOC
and
no
evi
denc
e of
cr
ania
l tra
uma
• N
o ph
ysic
al e
vi-
denc
e th
at h
ead
stru
ck w
ind-
shie
ld/h
eadr
est
• S
ubje
ctiv
e re
port
of a
n al
tera
tion
in m
enta
l sta
tus
at a
ccid
ent w
ith
no o
bjec
tive
evid
ence
Exc
lusi
on:
Age
, yrs
: m
ean
41.8
(ran
ge, 8
-64)
Gen
der:
53%
FG
CS:
NI
Tim
e si
nce:
1
wk
to 5
yrs
Clin
ical
in
terv
iew
s co
rrob
orat
ed
via
inte
r-vi
ews
with
si
gnifi
cant
ot
hers
/co-
wor
kers
Neu
ro-
psyc
hol-
ogy
batte
ry:
Wec
hsle
r A
dult
Inte
lli-
genc
e S
cale
-
revi
sed
(WA
IS-R
), W
MS
-R,
Rey
figu
res,
H
oope
r,
Cog
nitiv
e de
f-ic
its o
bser
ved
parti
cula
rly
with
exe
cu-
tive
func
tion-
ing
(atte
ntio
n an
d co
n-ce
ntra
tion)
; PA
SAT
mos
t se
nsiti
ve te
st;
Som
e ex
peri-
ence
of m
ild
depr
essi
on;
Pro
blem
s ob
serv
ed w
ith
beha
vior
al
cont
rol,
slee
p an
d se
xual
ity;
EE
Q s
how
ed
Whi
plas
h ca
n pr
o-du
ce w
ide-
rang
ing
circ
uitry
dys
func
-tio
n (s
imila
r to
m
TBI)
Mod
erat
e:
3.5/
7B
asel
ine:
0.5
B
lindi
ng: 0
Sam
ple
size
: 0.
5A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
crip
tion:
0.
5Fo
llow
-up:
0

352 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
P
revi
ous
whi
plas
h or
clo
sed
BI,
neu-
rolo
gica
l dis
orde
r se
izur
e, p
sych
iatri
c pr
oble
m s
ubst
ance
ab
use
or m
edic
al
cond
ition
or
med
i-ca
tion
that
com
-pr
omis
e ne
rvou
s sy
stem
inte
grity
Bos
ton
nam
-in
g an
d ve
r-ba
l flue
ncy,
Tr
ails
A a
nd
B W
isco
nsin
C
ard
Sor
t, S
troop
, au
dito
ry,
cons
onan
t tri
gram
s,
PAS
AT
front
-cen
tral
slow
ing
and
↑ in
spi
ke
activ
ity
Inte
rven
tion
Jha
et a
l. 20
08 U
SA
Type
:In
terv
entio
nTe
st th
e ef
ficac
y of
m
odafi
nil i
n tre
atin
g fa
tigue
an
d E
DS
Leve
l II
Dow
ns a
nd
Bla
ck:
23/2
8 R
ecru
it-m
ent:;
PA
; D
oubl
e-bl
ind,
pl
aceb
o-co
ntro
lled
cors
sove
r tri
al: 4
wk,
w
asho
ut
perio
d, 4
wk
open
labe
l tri
al a
t end
of
mod
afini
l: 2
x 10
0 m
g tw
ice
a da
y fo
r 8
wks
w
ith 2
wks
gr
adua
ted
in
(man
ufac
tur-
er p
rovi
ded)
Dat
a co
llec-
tion:
bas
e-
E1
= 24
(dr
ug fi
rst)
E2
= 22
(pl
aceb
o fir
st)
Incl
usio
n:•
1 yr
pos
t-TB
I (s
ever
e en
ough
to
req
uire
inpa
-tie
nt r
ehab
)•
18-6
5 yr
s•
Rep
ort f
atig
ue
and/
or E
DS
co
mpr
omis
ing
func
tioni
ngE
xlcu
sion
:•
neur
olog
ic/n
eu-
ron
psyc
hiat
ric
diag
nosi
s•
Oth
er d
iagn
osis
fo
r E
DS
• C
oncu
rren
t sig
-ni
fican
t sys
tem
ic
dise
ase
• E
pile
psy
• C
ardi
ovas
cula
r di
seas
e•
Sig
nific
ant
Age
, yrs
: 38.
25±
12.2
0G
ende
r:31
.4%
FG
CS:
sev
ere:
3-
8 (5
1%);
mod
erat
e 9-
12
(23.
5%; m
ild
13-2
5 (2
5.5%
); Ti
me
sinc
e:
5.77
± 4
.97
yrs
Mod
ified
Fa
tigue
Im-
pact
Sca
le;
Fatig
ue S
e-ve
rity
Sca
le;
ES
S; M
OS
-12
item
; S
F-12
; Pos
t C
oncu
ssio
n;
Ass
essm
ent
Cog
nitiv
e Te
stin
g (Im
pact
) C
onno
r’s
cont
inuo
us
perfo
rman
ce
test
IIB
DI I
I
ES
S: E
1>E
2 at
wee
k 4
but
not a
t wee
k 10
: onl
y sh
ort-t
erm
be
nefit
In
som
nia
repo
rted
mor
e of
ten
with
dru
g th
an p
lace
bo;
Saf
e an
d w
ell
tole
rate
d;
Ther
e w
ere
no s
igni
fican
t di
ffere
nces
be
twee
n m
odaf
inil
and
plac
ebo
and
no c
onsi
sten
t an
d pe
rsis
-te
nt c
linic
ally
si
gnifi
cant
di
ffere
nces
Stre
ngth
s:Th
orou
gh c
om-
plet
e in
form
atio
n w
ith d
emog
raph
-ic
s, m
etho
dolo
gy;
Ack
now
ledg
ed
com
plex
ity o
f fa-
tigue
and
rel
atio
n-sh
ip w
ith s
leep
i-ne
ssLi
mita
tions
: A
ll sl
eep
mea
-su
res
self-
repo
rt;
Sta
ndar
d do
s-ag
e, th
eref
ore
not
able
to ta
ilor
to
indi
vidu
al (
mod
ify
to m
eet i
ndiv
idua
l re
spon
ses
(ex.
ta
per)
); S
ingl
e ce
nter
; Mul
tiple
st
at te
sts,
Clin
ical
si
gnifi
canc
e co
m-
plic
ated
as
mos
t di
d op
en la
bel
Hig
h:
6.5/
7B
asel
ine:
1
Blin
ding
: 1S
ampl
e si
ze:
0.5
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
iptio
n: 1
Follo
w-u
p: 1

353Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
line,
wee
k 4,
wee
k 10
, w
eeks
4
and
10 a
fter
cros
sove
r
psyc
hiat
ric o
r be
-ha
vior
sym
ptom
s •
Non
-Eng
lish
• P
regn
ant f
emal
es
or p
oten
tial c
hild
-be
arin
g un
less
us
ing
cont
race
p-tiv
es
Cas
triot
ta
2008
US
ATy
pe:
Inte
rven
tion
Det
erm
ine
whe
ther
trea
t-m
ent o
f sle
ep
diso
rder
s id
entifi
ed in
BI
adul
ts r
esul
ts
in r
esol
u-tio
n of
thos
e di
sord
ers
and
impr
ovem
ent
of s
ympt
oms
and
dayt
ime
func
tion
Leve
l III
Dow
ns
and
Bla
ck:
17/2
8R
ecru
itmen
t: P
rosp
ectiv
e un
sele
cted
pa
tient
s A
I (3
cen
ters
); Lo
ngitu
dina
l; B
asel
ine
and
3 m
os;
neur
opsy
-ch
olog
ical
te
stin
g pe
rform
ed
at 1
0:30
to
con
trol
for
diur
nal
varia
tion;
on
ly th
ose
with
sle
ep
diso
rder
did
th
e sl
eep
asse
ssm
ent
agai
n at
3
mos
TBI =
57
Incl
usio
n:•
> 18
yrs
• ≥
3 m
o po
st-
inju
ryE
xclu
sion
:•
Pre
senc
e of
ci
rcad
ian
rhyt
hm
diso
rder
• U
nabl
e to
giv
e in
form
ed c
onse
nt•
Use
of s
edat
ing
med
icat
ions
Age
, yrs
:38
.6 ±
14.
8G
ende
r:25
% F
GC
S: u
sed
with
C
T fin
ding
s ac
-co
rdin
g to
crit
e-ria
to e
stab
lish
seve
rity
30%
sT
BI;
5% m
od-
sTB
I; 18
% m
od
TBI;
9% m
TBI;
38%
mis
sing
Tim
e si
nce:
67
.8 ±
126
.3
mos
Sle
ep:
NP
SG
; M
SLT
; ES
S;
Neu
rops
y-ch
olog
ical
: P
VT;
PO
MS
; FO
SQ
; U
rine
sam
-pl
e to
test
fo
r dr
ugs/
med
icat
ions
; Tr
eatm
ent:
CPA
P fo
r O
SA
; M
odafi
nil f
or
narc
olep
sy
and
PTH
P
ram
ipex
ole
for
Per
i-od
ic L
imb
Mov
emen
t S
yndr
ome
(PLM
S)
39%
had
ab
norm
al
slee
p st
udie
s:
23%
OSA
, 3%
PTH
, 5%
na
crol
epsy
, 7%
PLM
S;
21%
ED
S;
GC
S ↓
for
slee
p di
sor-
dere
d; S
leep
di
sord
ered
>
redu
ctio
ns
in te
nsio
n an
d an
ger
and
ESS
th
an n
on-
diso
rder
ed;
Apne
a/hy
-po
pnea
Inde
x im
prov
ed w
ith
treat
men
t ↑
Amou
nt o
f R
EM T
reat
-m
ent m
ay
resu
lt in
N
PG r
esol
u-tio
n w
ithou
t ch
ange
in
slee
pine
ss o
f
Stre
ngth
s:R
igor
ous
met
h-od
s; u
sed
esta
b-lis
hed
crite
ria a
s m
uch
as p
ossi
ble
Lim
itatio
ns:
Med
icat
ions
not
tit
rate
d; L
arge
m
issi
ng s
ever
ity
data
; Sub
sam
ples
sm
all;
MS
LT n
ot
the
right
m
ea-
sure
as
it se
ems
that
sle
ep a
nd
wak
eful
ness
are
2
sepa
rate
act
ive
proc
esse
s
Mod
erat
e:
5/7
Bas
elin
e: 1
B
lindi
ng: 0
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 1
Des
crip
tion:
1Fo
llow
-up:
1

354 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
neur
opsy
-ch
olog
ical
fu
nctio
n
Fran
cisc
o &
Ivan
hoe
1996
US
A
Type
: Int
erve
n-tio
n
Effe
cts
of
met
hylp
he-
nida
te o
n po
sttra
umat
ic
narc
olep
sy
Leve
l IVA
D
owns
and
B
lack
:11/
28R
ecru
itmen
t:LC
; Sin
gle
case
stu
dy;
Met
hylp
heni
-da
te: 1
0 m
g 2x
/day
then
↑
to 3
0 m
g 2x
/day
ove
r 4
mos
TBI =
1
Cla
ssic
tetra
d of
na
rcol
epsy
(ca
ta-
plex
y, E
DS
, sle
ep
para
lysi
s hy
pnag
o-gi
c ha
lluci
natio
ns);
diag
nosi
s co
n-fir
med
by
PS
G a
nd
MS
LT; N
o st
ruc-
tura
l, m
etab
olic
, or
card
iac
abno
rmal
i-tie
s th
at e
xpla
in th
e sy
mpt
oms
Age
, yrs
: 27
Gen
der:
Mal
eG
CS:
3 a
t in-
jury
site
but
7 a
t E
D; m
od T
BI
Tim
e si
nce:
22
mos
PS
G; M
SLT
1 m
o af
ter
initi
atio
n ca
tapl
exy
and
ED
S s
tarte
d to
impr
ove
6 m
os a
fter
the
star
t of
treat
men
t the
pa
tient
is a
s-ym
ptom
atic
At 1
2 m
os
med
icat
ion
was
invo
lun-
taril
y w
ith-
draw
n an
d sy
mpt
oms
retu
rned
Dru
gs le
adin
g to
no
repi
neph
rine
rele
ase
may
be
help
ful i
n re
vers
-in
g th
e sy
mpt
oms
of n
arco
leps
y
Mod
erat
e:
4.5/
7B
asel
ine:
0.5
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
iptio
n: 1
Follo
w-u
p: 1
Oue
llet a
nd
Mor
in 2
007
Can
ada
Type
:In
terv
entio
nD
eter
min
e th
e ef
ficac
y of
co
gniti
ve b
e-ha
vior
ther
apy
(CB
T) in
TB
I
Leve
l III
Dow
ns a
nd
Bla
ck:1
6/28
Rec
ruitm
ent
OR
; Sin
gle
case
des
ign
with
mul
tiple
ba
selin
es
acro
ss
subj
ects
8
wk
CB
T ad
dres
sing
st
imul
us
cont
rol,
slee
p re
stric
tion
cogn
itive
TBI =
11
Incl
usio
n:•
18-5
0 yr
s•
TBI i
n la
st 5
yrs
• N
ot a
n in
patie
nt•
Inso
mni
a sy
n-dr
ome
(ope
ra-
tiona
l def
initi
on)
• If
taki
ng m
eds
for
6 m
os a
nd
stab
leE
xclu
sion
:•
Maj
or u
ntre
ated
or
uns
tabl
e m
ed-
ical
or
psyc
hiat
-ric
com
orbi
dity
• M
eds
know
n to
Age
, yrs
: 27.
3G
ende
r: 4
6% F
GC
S: 3
-14;
2
no d
ata;
mTB
I to
sTB
I as
eval
uate
d by
m
ultid
isci
plin
ary
team
usi
ng
stan
dard
crit
eria
Tim
e si
nce:
25
.64
mos
Sle
ep d
iary
(T
otal
wak
e tim
e, S
leep
ef
ficie
ncy)
; D
iagn
ostic
In
terv
iew
for
Inso
mni
a;
ISI;
MFI
; D
ysfu
nc-
tiona
l B
elie
fs a
nd
Atti
tude
s A
bout
Sle
ep
Sca
le; B
DI;
BA
I; 2-
nigh
t P
SG
; Sho
rt te
leph
one
Bas
elin
e re
-su
lts s
how
ed
varia
bilit
y as
ex
pect
ed;
clin
ical
and
si
gnfic
ant
redu
ctio
ns
in to
tal w
ake
time
and
slee
p ef
-fic
ienc
y fo
r 8/
11 (
74%
); P
rogr
ess
gene
rally
wel
l m
aint
aine
d at
follo
w-u
p;
Sle
ep e
ffici
-
Stre
ngth
s:G
ood
base
line
tabl
e; C
BT
seem
s pr
omis
ing
Li
mita
tions
: N
eede
d to
incl
ude
desc
riptio
n of
C
BT;
Did
not
as
sess
cog
ni-
tive
func
tioni
ng;
Wom
en w
ere
over
repr
esen
ted;
S
elf-s
elec
ted
so
may
be
mor
e m
o-tiv
ated
to c
hang
e
Mod
erat
e:
4.5/
7B
asel
ine:
0.5
B
lindi
ng: 0
.5S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 1D
escr
iptio
n:
0.5
Follo
w-u
p: 1

355Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
rest
ruct
ur-
ing,
sle
ep
hygi
ene,
ed
ucat
ion
and
fatig
ue
man
age-
men
t; S
leep
di
ary
for
2 w
ks a
t fo
llow
-up
and
3,5,
or
7 w
ks
rand
omly
de
term
ined
ac
ross
su
bgro
ups
of 3
; 1-m
o an
d 3-
mos
fo
llow
-up
prod
uce
inso
mni
a•
Sle
ep d
istu
rban
c-es
bef
ore
TBI
• A
noth
er s
leep
di
sord
er
• U
nabl
e to
com
-pl
ete
ques
tion-
naire
• E
xper
ienc
e si
g-ni
fican
t pai
n
inte
rvie
w a
t fo
llow
-up
by
inde
pend
ent
inte
rvie
wer
cien
cy
augm
ente
d;
↓ fa
tigue
sy
mpt
oms
Oue
llet &
M
orin
200
4 C
anad
a
Type
:In
terv
entio
nTo
test
the
ef-
ficac
y of
CB
T fo
r in
som
nia
with
TB
I in
a pe
rson
with
di
fficu
lty fa
lling
al
seep
and
st
ayin
g as
leep
si
nce
inju
ry
Leve
l III
Dow
ns a
nd
Bla
ck:1
0/28
Rec
ruitm
ent
OR
; Sin
gle
case
stu
dy;
8 w
kly
indi
vidu
al
man
ual-
ized
CB
T se
ssio
ns
(ada
pted
fo
r TB
I) ad
dres
sing
st
imul
us
cont
rol,
slee
p re
-st
rictio
n, c
og
rest
ruct
urin
g,
N =
1D
iagn
ostic
clin
ical
in
terv
iew
det
er-
min
ed h
ad m
ixed
in
som
nia
(ICS
D
and
DS
M)
Age
, yrs
: lat
e 30
sG
ende
r: m
ale
GC
S: 1
3/15
, no
com
a, P
TA 5
-7
days
, mod
erat
e TB
ITi
me
sinc
e: N
I
Sle
ep d
iary
fo
r 5
wks
of
base
line,
8
wks
CB
T,
2 w
ks p
ost
treat
men
t an
d fo
llow
-up
at 1
and
3
mos
PS
G
(5 n
ight
s: 3
pr
e an
d 2
post
) In
som
-ni
a S
ever
ity
Inde
x (IS
I) D
ysfu
nc-
tiona
l Bel
iefs
an
d A
tti-
tude
s ab
out
Sle
ep S
cale
Sle
ep o
nset
↓
from
47
min
to 1
8 an
d no
ctur
nal
awak
enin
gs
↓ fro
m 8
5 to
28
min
; bot
h be
low
clin
ical
cr
iteria
Sle
ep e
ffi-
cien
cy ↑
from
58
% to
83%
P
SG
cor
robo
-ra
ted
data
M
ajor
ity o
f ga
ins
wer
e m
aint
aine
d at
follo
w-u
p (ta
perin
g of
Stre
ngth
s:W
as a
dapt
ed fo
r TB
I Th
e be
havi
oral
re
com
men
datio
ns
in th
e in
terv
entio
n w
ere
sim
ple
and
stra
ight
fow
ard
Pro
mis
e fo
r no
npha
rmac
olog
i-ca
l int
erve
ntio
ns,
parti
cula
rly C
BT
Mod
erat
e:
4/7
Bas
elin
e: 0
.5
Blin
ding
: 0S
ampl
e si
ze: 0
Attr
ition
: 1S
tand
ardi
zed
outc
omes
: 0.5
Des
crip
tion:
1Fo
llow
-up:
1

356 Critical Reviews™ in Physical and Rehabilitation Medicine
TAB
LE 5
(CO
NTI
NU
ED)
and
slee
p hy
gien
e ed
ucat
ion
give
n by
a
clin
ical
ps
ycho
logi
st
5 w
ks o
f ba
selin
e, 8
w
ks C
BT,
2
wks
pos
t-tre
atm
ent
and
follo
w-
up a
t 1 a
nd
3 m
os
MFI
BA
Im
edic
atio
n w
as o
ccur
ing)
IS
I dro
pped
fro
m c
linic
al
to s
ubcl
inic
al
scor
e
Sha
n &
A
shw
orth
20
04
Can
ada
Type
:In
terv
entio
nA
sses
s th
e ef
-fe
cts
of lo
raz-
epam
ver
sus
zopi
clon
e on
co
gniti
on
Leve
l II
Dow
ns a
nd
Bla
ck:
23/2
8R
ecru
itmen
t: C
onse
cutiv
e A
I; D
oubl
e-bl
ind,
cro
ss-
over
tria
l S
elf-r
egul
ate
(0, 0
.5 o
r fu
ll ta
blet
) of
lo
raze
pam
(0
.5-1
.0 m
g)
or z
opic
lone
(3
.75-
7.5
mg)
at
bedt
ime
for
7 da
ysS
tart-
ing
dose
ra
ndom
ly
gene
rate
d A
t 2 w
ks
AB
I and
stro
ke =
18
(A
BI:
6)E
1 =
9E
2 =
9In
clus
ion:
• >1
8 yr
s•
Sec
onda
ry
caus
es o
f ins
om-
nia
okay
: dep
res-
sion
, apn
ea,
rest
less
legs
Exc
lusi
on:
• A
cute
ly il
l•
Non
-Eng
lish/
Fren
ch s
peak
ing
• U
nabl
e to
rea
d qu
estio
ns•
Sev
ere
cogn
itive
im
pairm
ent
Age
, yrs
: 56.
6G
ende
r:44
% F
GC
S: N
ITi
me
sinc
e: N
I
Fols
tein
M
MS
E:
base
line,
du
ring
wee
k 1
and
wee
k 2;
Rat
e qu
ality
of
slee
p fro
m
nigh
t bef
ore
(2 o
f 7 d
ays
but n
ot th
e fir
st 3
day
s)
- lo
cally
de
velo
ped
Tota
l sle
ep
time
re-
cord
ed b
y nu
rsin
g st
aff
ques
tion-
naire
eve
ry
30 m
in o
r 1
hrN
urse
s ra
ted
rest
fuln
ess
The
med
ica-
tions
see
m
to b
e eq
ually
ef
fect
ive
Lim
itatio
ns:
Non
phar
mac
olog
i-ca
l int
erve
ntio
ns
used
Crit
eria
par
-tic
ipan
ts u
sed
for
self-
dosi
ng n
ot
clea
rW
eak
mea
sure
s:lo
cally
dev
elop
ed
as c
onve
nien
ce,
thou
ght m
ore
sens
itive
than
M
orni
ng S
leep
Q
uest
ionn
aire
and
no
gol
d st
anda
rdE
xclu
ded
seve
re
impa
irmen
t
Mod
erat
e:
3.5/
7B
asel
ine:
0.5
B
lindi
ng: 1
Sam
ple
size
: 0A
ttriti
on: 1
Sta
ndar
dize
d ou
tcom
es: 0
Des
crip
tion:
1Fo
llow
-up:
0

357Volume 21 Numbers 3-4
TAB
LE 5
(CO
NTI
NU
ED)
stat
e w
hich
in
terv
entio
n pr
efer
and
drow
si-
ness
on
a 1-
4 sc
ale
test
ing
for
atax
ia
a Ove
rall
qual
ity (
sum
acr
oss
all t
he e
lem
ents
abo
ve; 0
.5 r
ound
ed d
own)
: 5, 6
, or
7 in
dica
te h
igh
qual
ity; 3
or
4 in
dica
te m
oder
ate
qual
ity; a
nd 1
or
2 in
dica
te
low
qua
lity.
b “
TBI”,
ref
ers
to th
e tra
umat
ic b
rain
inju
ry g
roup
; “A
BI”,
ref
ers
to th
e ac
quire
d br
ain
inju
ry g
roup
; “C
ontro
ls”,
“C1”
, “C
2” r
efer
s to
the
cont
rol/c
ompa
rison
gro
up(s
).A
bbre
viat
ions
: ↑, i
ncre
ase;
↓, d
ecre
ase;
A, a
cute
; AI,
acut
e in
patie
nt r
ehab
ilita
tion;
BD
I, B
eck
Dep
ress
ion
Inve
ntor
y; C
PAP,
con
tinuo
us p
ositi
ve a
irway
pre
ssur
e;
CR
SD
s, c
ircad
ian
rhyt
hm s
leep
dis
orde
rs; C
SF,
cer
ebra
l spi
nal fl
uid;
CT,
com
pute
rized
tom
ogra
phy;
CVA
, car
diov
ascu
lar
acci
dent
; DS
PS
, del
ayed
sle
ep p
hase
sy
ndro
me;
EE
G, e
lect
roen
ceph
alog
ram
; ER
, em
erge
ncy
room
; ES
S, E
pwor
th S
leep
ines
s S
cale
; F, f
emal
e; F
OS
Q: F
unct
iona
l Out
com
e of
Sle
ep Q
uest
ionn
aire
; G
CS
, Gla
sgow
Com
a S
cale
sco
re; H
AD
S, H
ospi
tal A
nxie
ty a
nd D
epre
ssio
n S
cale
; HI,
head
inju
ry; I
SS
, Ins
omni
a S
ever
ity In
dex;
LC
, lon
g-te
rm c
omm
unity
-re-
sidi
ng; L
OC
, Los
s of
con
scio
usne
ss; m
TBI,
mild
bra
in tr
aum
atic
inju
ry; m
odTB
I, m
oder
ate
TBI;
MFI
, Mul
tidim
ensi
onal
Fat
igue
Inve
ntor
y; m
HI,
mild
hea
d in
jury
; M
MS
E, M
ini-M
enta
l Sta
te E
xam
; MS
K, m
uscu
losk
elet
al in
jury
; MS
LT, M
ultip
le S
leep
Lat
ency
Tes
t; M
VC
, mot
or v
ehic
le c
ollis
ion;
NFL
, Nat
iona
l Foo
tbal
l Lea
gue;
N
H, n
onhy
pers
omni
a; N
I, N
ot In
dica
ted;
NR
EM
, non
-RE
M; O
-LO
G, o
rient
atio
n lo
g; O
R, o
utpa
tient
reh
abili
tatio
n; P
A, p
osta
cute
; PA
C, p
osta
cute
com
mun
ity;
PO
MS
, Pro
file
of M
ood
Sta
tes;
PR
, pos
treha
bilit
atio
n; P
SG
, pol
ysom
nogr
aphy
; PS
QI,
Pitt
sbur
gh S
leep
Qua
lity
Inde
x; P
TA, p
osttr
aum
atic
am
nesi
a; P
TH, p
ost-
traum
atic
hyp
erso
mni
a; P
VT,
Psy
chom
otor
Vig
ilanc
e Te
st; R
EM
, rap
id e
ye m
ovem
ent;
SC
I, sp
inal
cor
d in
jury
; sTB
I, se
vere
TB
I; vs
TBI,
very
sev
ere
TBI.

358 Critical Reviews™ in Physical and Rehabilitation Medicine
It has been consistently reported in the literature that individuals with TBI experience symptoms of insomnia and other sleep disturbances across the spectrum of recovery from the acute stage and beyond, across all levels of severity, with some patients continuing to report sleep disturbances for many years postinjury.4,6,29–37
Thus, in order to try and present the litera-ture in a manner that might further elucidate our understanding of the developmental course of posttraumatic sleep disturbances over time, we attempted to discuss the studies from the perspec-tives of sleep in the acute stage, early recovery/rehabilitation (to 1 year), and 1–3 years and beyond. However, consistent with the reports of Ouellet and colleagues6 and Orff and colleagues7 in their previous reviews, we experienced diffi-culties in doing so, particularly for those studies (the majority of which we identified) that were cross sectional, that is, evaluating sleep at only one time period.
Most studies clearly identified the average time postinjury of their participants and the range/standard deviation, but the ranges were, in fact, quite wide. Among the studies that utilized a com-parison group (these studies were methodologi-cally stronger than studies that did not involve a comparison group), the ranges of time postinjury were the following (in chronological order from publication date): from 2.7 months to 5 years, average 2 years post;35 2 weeks to 53 months, average 3.8 months post;32 7 to 41 months, average 20.96 months post;4 20 to 1194 days, average 230 days;29 12 months to 21 years, mean not given;36 74 to 1194 days, average 516 days;26 12.3 to 43.3 months, average 27.8 mos;37 and up to 1 year post, specifics not given.27 Thus, among these studies, we identified an overall 21-year range in time postinjury of subjects. The results, however, were not stratified in any of the studies by time postinjury, thus making it extremely difficult to draw any definitive conclusions regarding the developmental time course of the sleep disorders.
Furthermore, sleep disorders may well be con-founded over time by the subsequent development of depression, anxiety, reduced activity and weight gain, again making it difficult to draw specific conclusions about the etiology of these disorders. It is necessary to acknowledge and mitigate potential factors that may confound the results,
whether these are factors that were preexisting to the brain injury or have developed secondary to the brain injury. However, from the perspective of recruitment at various times postinjury, there were studies that reported on sleep findings, including both prevalence and nature, at specific time points across different levels of severity. Thus, we have attempted to summarize the literature regarding the prevalence and nature of sleep disorders following TBI based on the source of patient recruitment: acute/postacute, rehabilitation, and community. Only those studies that delineated recruitment by time postinjury and level of severity, as well as stratified results according to the source of patients (e.g., acute care, rehabilitation settings) and level of severity, are included below. Thus, those studies that did not stratify their findings by level of severity are not included in our analysis. In addition, we only included studies that had substantial measures of sleep versus a single item documenting sleep problems.
a. Patients Recruited From Acute and Post-acute Care
We identified five studies that recruited participants from acute care settings.26,28,30,32,39
Acute mild. Chaput and colleagues38 con-ducted a retrospective chart review to determine the prevalence of sleep complaints in a sample of 443 patients diagnosed with mTBI. The authors used two time points: 10 days postinjury and again at 6 weeks postinjury. Of this sample, 13.3% reported sleep changes at 10 days postinjury, and this increased to 33.5% at 6 weeks postinjury with a smaller sample. Furthermore, the prevalence of sleep complaints at 6 weeks was 2.9 times more likely if such a symptom was present at 10 days (P = .004) and was associated with concomitant headaches, depressive symptoms, and irritability. Given the large sample size and the fact that they recruited all of those patients within the diag-nostic category rather than just those with sleep complaints, the sample bias is minimized and the results are more generalizeable to the whole mTBI population. The nature of the sleep complaints, however, was not delineated.
Acute and postacute moderate-severe. Makley and colleagues28 followed a sample of 14 patients

359Volume 21 Numbers 3-4
with moderate-severe injuries recruited at 9 to 23 days postinjury from acute care, and reported that 78% had severely impaired mean sleep effi-ciency (<63%), as measured by actigraphy. These patients were subdivided into two groups, those with ongoing posttraumatic amnesia (PTA) and those whose PTA had resolved. Of significance, they reported that sleep efficiency improved once patients were no longer in a state of PTA (P = .032). Baumann and colleagues24 consecutively recruited 96 patients within the first 4 days after TBI; at 6 months following TBI, 65 patients were evaluated using a combination of polysomnography (PSG), Multiple Sleep Latency Test (MSLT), actigraphy and clinical interview. The authors determined that at 6 months postinjury, among patients across all levels of severity (60% moderate-severe), 72% had sleep problems, 28% had subjective daytime sleepiness, 25% had objectively measured day-time sleepiness, 17% reported fatigue, and 22% reported “sensu strictu” (an increased sleep need over 24 hours). An additional 5% had insomnia. The authors further noted that in 43% of patients, the only possible cause of these problems was directly attributed to the TBI.
Rao and colleagues30 recruited a sample of 54 patients within 3 months of trauma across all levels of severity; however, all had experienced a loss of consciousness. Results of the Medical Outcome Scales for sleep indicated significantly increased sleep disturbance (P = .018), decreased sleep adequacy (P = .023), and increased daytime sleepiness (P = .0002) in comparison to self-reports of preinjury sleep. Watson and colleagues39 looked specifically at the prevalence of hypersomnia in a consecutive sample of 346 patients with TBI recruited from admissions to a Level 1 trauma hos-pital, in comparison with trauma controls (without TBI) and trauma-free controls. Data on sleepiness were collected at 1 month postinjury, with follow-up at 1 year. The level of severity was determined by the time taken to follow commands according to the motor component of the Glasgow Coma Scale (GCS). Although 78% of subjects took less than 24 hours to follow commands, they presented with serious enough symptoms in the emergency room that they were admitted to hospital and as such we have included them in our discussion of patients with moderate-severe TBI. At 1 month postinjury, 55% of all TBI subjects endorsed one
or more sleepiness items on the Sickness Impact Profile, in comparison with 41% of trauma controls and 3% of trauma-free controls (P < .001).
b. Patients Recruited From Rehabilitation Populations
Mild. We identified only four recent studies in which mild subjects from a rehabilitation outpa-tient population were recruited. Beetar and col-leagues35 conducted a retrospective chart review to determine the prevalence of sleep complaints in a consecutive series of 202 patients with TBI referred for neuropsychological assessment. The sample included 127 mTBI patients, 75 moderate-severe TBI patients, and 123 non-TBI controls. The authors found that, overall, 56.4% of the TBI patients had significantly more complaints of in-somnia in comparison with controls (30.9%; P < .001), and the mTBI group reported approximately 50% more insomnia complaints than those with moderate-severe injuries (P < .001). This study was an important early contribution to the litera-ture on sleep and TBI. Even though the authors did not use an operational definition of insomnia, their large sample size, use of a control group, and delineation of results by severity provided a strong foundation for future research. With regard to prevalence, Clinchot and colleagues40 also reported on a sample of patients recruited from consecutive admissions to rehabilitation and contacted at 1 year postinjury. The authors found that approximately 75% of subjects (GCS score of 13–15) subjectively reported sleep disturbance.
Schreiber and colleagues36 studied the nature of sleep disturbance, conducting a retrospec-tive study of 26 patients with mTBI and sleep disturbance who were consecutively admitted to ambulatory rehabilitation. In comparison with healthy age- and sex-matched controls (who had routine sleep evaluations as part of a preemploy-ment assessment procedure), the mTBI group had objective changes in sleep architecture, including increased light sleep (nREM) in 54.5% of subjects in comparison with controls (46.6%), and signifi-cantly lower total sleep time (P < .05). They also reported increased excessive daytime sleepiness objectively measured by MSLT in comparison with controls (higher number of falling asleep

360 Critical Reviews™ in Physical and Rehabilitation Medicine
episodes (P ≤ .05) and shorter time to fall asleep (P < .0005). Baumann and colleagues24 (also dis-cussed in the section above on acute and postacute moderate-severe TBI) reported objectively mea-sured sleep efficiency of 92% among their mild subjects; however, they identified 2 subjects (13%) with sleep efficiency well below the age-adjusted 25% percentile values. It is important to consider that the findings of these three studies may not be generalized to the population of mTBI as a whole. Despite the fact that the subjects were classified as mild, they all required rehabilitation and/or were referred for neuropsychological evaluation, thus placing them in a more “involved or severe/complicated” category of “mild” injury.
Moderate-severe. Although we identified seven studies that examined the prevalence and/or nature of sleep disturbances in samples recruited from a moderate-severe rehabilitation population,25,31,32,40–43 only the most recent (and higher quality) study stratified or reported results according to severity,25 with the exception of the earlier work by Clinchot.40 Clinchot and col-leagues40 (recruitment described above) found that approximately 57% of patients with a GCS score of 8–12, 24% of patients with a GCS score of 5–7, and 40% of patients with a GCS score of 3–4, reported subjective sleep complaints. Castriotta and colleagues25 conducted an objective evalua-tion of sleep in 87 patients who were at least 3 months postinjury and were recruited from the rehabilitation services at three academic medical centers. Abnormal sleep studies were found in 46% of subjects. With regard to the nature of the sleep disturbances, 20% had OSA, 11% had posttrau-matic hypersomnia, 6% had narcolepsy, and 7% had PLM. Among all subjects, 22% had objective excessive daytime sleepiness as measured by the MSLT. Interestingly, they identified no differences in injury severity and/or time postinjury between sleepy and non-sleepy subjects with TBI.
Finally, we identified two studies that recruited patients from rehabilitation, and although they identified objectively measured sleep and wake disturbances among participants, neither study identified any significant differences in injury severity or time postinjury between sleepy and non-sleepy subjects.25,31 Castriotta and colleagues25 examined the prevalence of sleep disorders in a prospective sample of 87 patients with TBI who
were recruited from the rehabilitation services at three academic medical centers. Abnormal sleep studies (PSGs) were found in 46% of participants, including 23% with OSA, 11% with posttraumatic hypersomnia, and 7% with PLMs. Objective excessive daytime sleepiness was found in 25% of participants. Consistent with the findings of Verma,31 OSA was more common in obese partici-pants (body mass index [BMI] > 30). Furthermore, these investigators did not find any differences in severity of injury or time postinjury between sleepy and nonsleepy participants (P < .05).
c. Patients Recruited From the Community
We identified eight articles in which samples of individuals with TBI who had returned to the community were recruited.4,26,27,29,31,37,39,44
Mild. Williams and colleagues37 studied the extent and nature of sleep complaints in a sample of nine university students with previous mTBIs (range, 1.4–3.6 years postinjury) in comparison with age- and gender-matched controls. They identified 4% less efficient sleep, shorter REM onset latencies, and longer sleep onset latencies in comparison with controls, objectively measured by PSG. Although this study is quite thorough and rigorous in design, the small sample size and “sample of convenience” (i.e., student volunteers), weakens the generalizability of the findings. Sch-reiber and colleagues36 characterized the nature of sleep disturbances in a sample of 26 chronic mTBI patients with sleep complaints who were at least 1 year postinjury. They reported changes in sleep architecture (as measured by PSG), includ-ing increased light non-REM sleep, in 54.5% of patients (±13.4%) in comparison with controls (46.6% ± 10.4%).
Moderate-severe. Parcell and colleagues29 reported on a sample of 63 participants with TBI consecutively recruited after discharge from rehabilitation, in comparison with 63 age- and sex-matched controls. Eighty percent of patients reported subjective changes in sleep relative to controls (23%), including more nighttime awakenings, and longer sleep-onset latency. In another study,26 Parcell and colleagues recruited 10 community-based participants with TBI and 10 age- and sex-matched controls. The authors

361Volume 21 Numbers 3-4
reported objectively measured increases in slow-wave sleep, reductions in REM sleep, and reduced sleep efficiency in comparison with controls, as well as subjective reports of poorer sleep quality.
Ouellet and colleagues4 recruited a sample of 452 participants from mailings distributed to 1500 people with TBIs identified through the archives of the rehabilitation center, as well as TBI associa-tions and support groups. Their sample included 59.9% with severe injuries, 23.3% with moderate injuries, 13.7% with mild injuries, and 3.1% with “minor” TBIs. Participants completed a detailed questionnaire that was then mailed back to the authors, who identified that 50.2% of their sample reported insomnia symptoms and 29.4% fulfilled the diagnostic criteria for an insomnia syndrome. This study continues to have the largest sample size of all of the literature to date pertaining to the prevalence of insomnia following TBI. In ad-dition, it is one of the few that actually delineated between those who presented with symptoms of insomnia and those who met the diagnostic criteria for insomnia, thus providing a more reli-able and valid estimate of the true prevalence. It is not possible, however, to completely eliminate sample bias without having information regard-ing the 1000 others who chose not to participate.
In another study, Ouellet and Morin44 ex-amined the nature of insomnia in the context of TBI by recruiting a sample of 14 adults with TBI who presented with an insomnia syndrome (nine of whom were moderate-severe), and 14 healthy, age- and sex-matched controls. It was not clear from the article how or where the participants were recruited. The authors reported that 71% of subjects had objective findings of insomnia, including more awakenings and shorter REM onset latencies. Furthermore, in comparison with controls, those with TBI had significantly more awakenings lasting longer than 5 minutes (P = .059), as well as significantly shorter REM latency (for those with TBI taking no medications) (P = .050). In the 1-year follow-up to their study of the prevalence of hypersomnia in the acute stage following TBI, Watson and colleagues39 found that 27% of participants continued to endorse subjec-tive symptoms of sleepiness, in comparison with 23% of trauma controls and 1% of nontrauma controls (P < .001). However sleepiness did im-
prove in 84–100% of participants with TBI, with the smallest improvement being 84% in the mild-est group (≤24 hours to respond to commands). Verma and colleagues31 objectively examined the nature and spectrum of sleep disorders in chronic TBI by recruiting a sample of 60 patients who presented with postinjury sleep complaints. It is not clear where or how the participants were recruited. Sixty percent of patients in the sample had moderate-severe injuries. Hypersomnia was the presenting complaint in 50% of all partici-pants, which the authors reported was “mostly due to” underlying sleep apnea, narcolepsy, and PLMs. Of interest, 45% of the sample exceeded a BMI of 30, which is considered to be obese. Insomnia was the presenting complaint in 25% of participants, and half of those had difficulties with sleep onset.
Sport-related concussion. New to the literature is a 2009 study that evaluates sleep following sport-related concussions. Gosselin and col-leagues27 examined both subjective and objective sleep quality in 10 subjects/athletes with a sport-related concussion, and compared their findings to those of 11 nonconcussed control athletes from noncontact sports. The concussed group had a history of 4.6 (±2.1) concussions on average, sustaining at least one in the previous year. Ob-jective measures of sleep included two consecu-tive nights of PSG, and electroencephalography (EEG) spectral power; subjective measures of sleep included the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Post Concussion Symptom Scale, as well as a subjec-tive questionnaire that was developed specifically for the study. The authors reported that although the concussed athletes identified more symptoms and worse sleep quality than controls, this was not corroborated by any polysomnographic vari-ables, or REM and nREM sleep quantitative EEG variables. However, concussed athletes showed considerably more relative delta activity, and reduced alpha activity and relative alpha power, during wakefulness than controls. Based on these findings, the authors concluded that sport-related concussions are thus associated with wakefulness problems, rather than sleep disturbances per se. Although this study has a small sample size and as such the Gosselin and colleagues’ findings are preliminary, their strong methodological design is

362 Critical Reviews™ in Physical and Rehabilitation Medicine
such that this is an important first step in exam-ining this population. Their findings are relevant and timely, given that sport-related concussions occur at a predictable rate in “high-risk” sports (i.e., football, hockey, etc.), ranging from 7–12% of the participant population in any given year, and that the sequelae of sport-related concussion is currently receiving much attention.45–47
d. Prevalence
As the literature has continued to evolve, we have attempted (as have others before us) to identify ranges of the prevalence of sleep disturbances identified among the studies based on time postin-jury of recruitment. The results of these studies confirm that disorders of sleep and wakefulness are prevalent across all stages of recovery from TBI, from the early acute stage until many years postinjury, and across all levels of severity. However, defining conclusive “ranges” contin-ues to be problematic due to the heterogeneity within and between samples, inconsistencies in the measures used, different study objectives, and variations in reporting. Some studies utilized percentages for reporting findings; alternatively, others reported on regression analysis of sleep, along with various associated phenomenon (i.e., depression, anxiety); identified changes in sleep architecture; looked specifically at insomnia as a global phenomenon; reported on the symptoms of insomnia; or, looked at other types of sleep disorders such as hypersomnia in and of itself, or secondary to apnea. As such, a valid synthesis of prevalence rates among studies remains elusive, and larger epidemiological studies across levels of severity and varying time points are warranted.
e. Methodological Limitations
Although the studies continue to become more scientifically rigorous as the literature evolves, the results to date are representative of methodological limitations in study design, as most of the literature is based on a clinical subset of TBI survivors who: a) present with sleep complaints, therefore intro-ducing bias into the sample; and b) have received rehabilitation and therefore represent a subset of
this patient population with likely more severe injuries, even those who are classified as “mild”. Thus it is likely that the data are skewed and are not fully representative of the TBI population as a whole. However, Parcell and colleagues26 specifically identified that their sample of 10 in-cluded “the first ten willing participants, with no preference for patients with sleep complaints,” and Fichtenberg and colleagues32 recruited a prospec-tive sample of 50 consecutive admissions to an outpatient rehabilitation program. The advantage of recruiting consecutively upon admission to the acute setting or from the emergency room is that all patients diagnosed with TBI are included in the study sample and followed regardless of whether they require postacute care. By following patients from the acute stage the issue of time since injury becomes negated, as all of the sample will be entered into the study at time of injury. As soon as recruitment takes place after the acute stage, researchers are already introducing forms of selec-tion bias into the sample that should be addressed when discussing the generalizability of the find-ings. Given that such a small percentage of the studies were able to recruit consecutively from the acute setting the epidemiological understanding of this phenomenon is going to be fraught with issues of generalizability and difficulty in making clear conclusions.
An ideal study would follow a large sample consecutive series of patients from acute care for at least three years to understand how sleep prob-lems manifest themselves, or not, and how these change over time, considering natural recovery by levels of severity.
Confounds. Some of the researchers made sure to exclude concurrent potential confounders, whereas others collected data on potential con-founders (usage of caffeine, alcohol, medications, or drugs, BMI, and emotional state). However, with the exception of emotional state, which is also identified as a concurrent risk factor, the re-sults were not stratified according to any of these confounds, nor were they addressed in discussion. Thus, we are only able to comment that these confounders exist, but are not able to make any definitive comments regarding their influence.
Risk factors. Ten studies identified risk factors specifically associated with insomnia following TBI, and two studies identified risk factors for

363Volume 21 Numbers 3-4
other types of posttraumatic sleep and wake disorders. Beetar and colleagues35 identified pain and mTBI as being risk factors for insomnia complaints in a case-controlled sample of 200 TBI patients of mixed severity. Among a sample of 91 consecutive patients admitted to an out-patient rehabilitation program, Fichtenberg and colleagues41 identified three risk factors associ-ated with insomnia including milder injuries, the presence of pain, and depression. Of the three factors, depression had the strongest association with insomnia. Consistent with Fichtenberg’s findings, Ouellet and colleagues4 reported that among a sample of 460 survivors recruited from the community (averaging 7.85 years postinjury, 83.2% of whom with moderate-severe injuries), risk factors for insomnia included milder injuries, depression, and pain. They also identified high levels of fatigue as a further risk factor.
Among a sample of 60 patients with varying levels of severity, ranging from 3 months to 2 years postinjury, Verma and colleagues31 noted that those with complaints of insomnia had elevated Beck Depression Inventory (BDI) scores and Hamilton Anxiety scores, thus further confirming that de-pression and anxiety are risk factors for insomnia following TBI across all levels of severity. They also identified 45% of their sample as having a significantly high BMI. Chaput and colleagues38 identified headaches, depressive symptoms, and irritability as co-occurring with sleep complaints in a sample of 443 patients with mTBI, at both 10 days and 6 weeks. Rao and colleagues30 also identified depression and anxiety as coexisting risk factors for symptoms of insomnia. Clinchot and colleagues40 was the only study to identify gender (female) as a risk factor for symptoms of insomnia (P = .033), in addition to older age (P = .035), milder injuries, and a GCS score greater than 7 (P = .034). Baumann and colleagues24 identified that severe TBI (sTBI) was associated with the development of posttraumatic hypersomnia (P = .02), but not with the presence, characteristics, and severity of other posttraumatic sleep disorders. The association between more severe TBI and the development of hypersomnia was also confirmed by Watson and colleagues.39 Castriotta and col-leagues25 identified that among the 46% of their sample with abnormal sleep studies (with five different types of sleep and/or wake disorders),
the sample participants were significantly older than the nonsleep-disordered subjects (P < .01) and had a significantly higher BMI (P < .05).
Sample size. TBI is very heterogeneous and as a result it is complicated to conduct research that is generalizable. Ideally, studies would be able to recruit a large number of patients so that stratification on a number of variables would be possible: age at injury, gender, etiology of injury, severity of injury, and time since injury. Only 39% (9/23) of the studies reviewed used sample sizes of greater than 75. Thirty-five percent (8/23) of the studies involved studies with sample sizes of less than 30 and thus were compromised in their statistical analysis and their ability to generalize to the different subgroups of brain injury.
Definition of insomnia. Another method-ological limitation, also identified by Ouellet and Morin,44 is the lack of an operational definition of insomnia. Among the five comparison group stud-ies that evaluated subjective reports of insomnia, sleep, and hypersomnia postinjury,29,32,35,39,44 only two utilized an operational definition of insomnia, the International Classification of Sleep Disorders and the DSM-IV.32,44 Related to this is the lack of consistency in or development of an operational framework for assessing severity of brain injury. Many studies use the GCS score to assess severity but the GCS score is not always available and other factors are included: length of PTA, period of loss of consciousness, cerebral computed tomography (CT) findings, and neuropsychological findings. One study39 determined injury severity based on time taken to follow commands. Baumann and colleagues,24 one of the two methodologically strongest studies reviewed, specifically cited us-ing GCS scores and CT findings based on the Marshall48 criteria (I = no visible intracranial pathology, II–IV = midline shift, and V = mass lesion). It is necessary that there be consistency as to how to combine all of these factors together so that severity distinctions can be enabled when only some of the above features are present.
Measures. As per the comments of Orff and colleagues,7 there is also a significant discrepancy among the measures utilized. Of the 23 studies we evaluated under the epidemiology category, investigators used 19 different methods to evaluate sleep, of which four are objective (PSG, actigraphy, MSLT, Multiple Wake Test [MWT]). There is no

364 Critical Reviews™ in Physical and Rehabilitation Medicine
gold standard of standardized instruments that is accepted. Although locally developed measures and those that are clinically developed may be very useful, it is impossible to compare from one study to the next when different types of measures are being used to assess the outcomes. The issue is that sleep itself is very difficult to assess, as it is composed of many components. It would seem that among the validated instruments, the most commonly used and accepted are the Diagnostic Interview for Insomnia (DII), Insomnia Sever-ity Index (ISI), PSQI, and the ESS. It has been proposed that the MWT may be more suitable for this population than the MSLT, as daytime sleepiness seems to be a hallmark of this condi-tion. One study30 utilized the 12-item Medical Outcome Scale for Sleep,49 which has been found to have good psychometric properties and has been found to be useful for assessing sleep problems in adults. Each of these instruments contributes a unique component to the assessment of insomnia and sleep difficulties and as such should be used in combination, rather than in isolation.
The subjective or self-report measures ranged from the early work of Beetar, which relied on a
chart review, and concluded that “a sleep problem was judged as present if it was mentioned in the chart as reported by the patient,”35(p. 1299) to the more robust PSQI used by Fichtenberg32 (and validated for use with TBI patients), the battery used by Ouellet and colleagues44 that included the DII, ISI, Multidimensional Fatigue Inventory, in addition to other measures and nocturnal PSG, sleep diaries, and ESS used by Parcell and col-leagues.26,29 The most commonly used measures included the PSQI, PSG, and some form of a sleep diary. It is positive to note that as the literature evolves, overall, the use of measures to evaluate sleep and wake disorders have become increas-ingly comprehensive, sensitive, and “robust” over time. This in and of itself, however, further emphasizes the weakness of recent studies that rely on limited and/or weak measures, such as the study by Watson and colleagues.39 Although we recognize that this study was part of a larger study and had the strength of a follow-up in its design, the sole reliance on data obtained via four questions about sleep from the Sickness Impact Profile weakens the validity/generalizability of the overall findings.
TABLE 6
Practice Points Research Agenda1. Sleep and wake disorders are
present across all levels of severity at all stages across the continuum of recovery following TBI.
1. A large scale multi-center collaborative trial involving all those with TBI (i.e., not limited to those who present with sleep prob-lems) recruited in the acute stage, followed longitudinally into the community and evaluated at regular time points is warranted.
2. Sleep and wakefulness should be routinely and systematically as-sessed for the duration of medical and neuropsychological follow-up after TBI.
2. Functional measures should be used in addition to formal mea-sures of cognition.
3. Risk factors for insomnia include mTBI, pain, anxiety, depression, fatigue, and older age.
4. Risk factors for hypersomnia in-clude more severe TBI.
5. Increased BMI (>30) is a risk fac-tor for OSA.
6. The PSQI, followed by the ISI, are appropriate measures for initial screening and corroboration of the impact of the problem.

365Volume 21 Numbers 3-4
2. Pathophysiology
We identified three papers, all of moderate quality, which look at varying aspects of pathophysiol-ogy of sleep/wake disturbances following TBI, including two Level III studies50,51 and one Level IVA study.52 In 2005, Baumann and colleagues50 sought to test the hypothesis that deficiencies in hypocretin-orexin-1 (Orexin A) neurotransmission in acute TBI may play a role in the emergence of subsequent sleep/wake disorders. Orexin A is an excitatory hypothalamic neuropeptide involved in the regulation of the sleep/wake cycle, and its levels are typically reduced in persons with narcolepsy. Hypocretin-1 levels were measured in 44 patients by radioimmunoassay at 1–4 days following TBI (males, n = 32; 31 patients with sTBI, 8 with moderate TBI [modTBI], and 5 with mTBI), and compared with hypocretin-1 levels in healthy controls (n = 20). Their results indicated that in comparison with controls, hypocretin-1 levels were abnormally lower in 95% of patients with moderate-severe TBI, and in 95% of patients with posttraumatic brain CT findings. The authors postulated that hypocretin-1 deficiency following TBI may be reflective of hypothalamic damage (specifically to the posterolateral hypothalamus) and may be linked with the frequent development of posttraumatic sleep wake disorders. These findings are an important contribution to the determination of risk factors.
Ayalon and colleagues51 conducted a study to diagnose and describe the physical and behavioral characteristics of circadian rhythm sleep disorders (CRSDs) in patients with mTBI. Forty-two pa-tients with mTBI and complaints of insomnia were screened, and those who were suspected of having CRSDs underwent further diagnostic evaluation. In total, 15 of the 42 patients (36%) were formally diagnosed with CRSDs, eight patients displayed a delayed sleep phase syndrome (DSPS), and seven patients displayed an irregular sleep-wake pattern (ISWP). All patients exhibited a 24-hour period of melatonin rhythm, and those with DSPS exhibited a 24-hour periodicity oral-temperature rhythm. However, three of the seven patients with ISWP lacked such a daily rhythm. Furthermore, the pa-tients with ISWP exhibited smaller amplitudes of temperature rhythm. Given that the authors found that as many as 36% of their particular sample had
been diagnosed with insomnia when in fact they had a CRSD, they concluded that CRSDs may be a relatively frequent sleep disorder among these patients, and that misdiagnosis of patients with CRSDs as insomniacs may lead to inappropriate prescription of hypnotic medications.
Quinto and colleagues52 described the case of posttraumatic DSPS in a 48-year-old male, 4 years following TBI. (Note: the authors use the term cerebral concussion; however, as the patient was in coma for “several days,” we will consider this to be a severe TBI [sTBI]). Although the pa-tient was 4 years postinjury, the emergence of his sleep onset insomnia was during the acute phase of recovery. Since his injury, it took him 1 to 2 hours to fall asleep. He reported through a sleep diary that he would go to bed between 3:00 and 5:00 a.m., awaken after 1 to 1-and-a-half hours, return to sleep, and awaken between 11:00 a.m. and 12:00 p.m. These findings were confirmed by actigraphy. The patient did not have any other medical or psychiatric disorders. Circadian rhythms are quite strict and are in fact slightly less than 24 hours in humans. The “circadian clock” located in the suprachiasmatic nucleus (SCN) of the hypothalamus serves to keep physiologic functions in synchrony with each other and with the environmental light/dark cycle, thus making a small daily phase advance to entrain to the 24-hour day. A decreased ability to make this phase advance in response to environmental cues is thought to be the underlying pathophysiology behind DSPS, and the authors of this study postulate that damage to the SCN sustained during trauma may result in circadian cycle disorder.
3. Pediatrics
We identified six studies, five of which were of moderate quality, which reported sleep complaints in children and adolescents. Five of these studies focused specifically on mTBI. In a 2001 study of 19 adolescents 3 years following minor head injury (mHI), Kaufman and colleagues53 reported that in comparison with healthy controls, head-injured teens had significantly reduced periods of sleep time, total sleep time, and sleep efficiency, as well as an increased number and length of awakenings, objectively measured by PSG and

366 Critical Reviews™ in Physical and Rehabilitation Medicine
actigraphy over 5 days. Subjectively, those with mHI reported significantly more difficulties falling asleep, difficulty waking in the morning, restless sleep and parasomnias, fearful awakenings from sleep, and increased daytime sleepiness than did healthy controls. Further investigations by this group of authors54 found that in comparison with healthy controls, nearly one third (27/98) of the subjects aged 8–18 years, with 0.5–6 years fol-lowing mHI, had subjective complaints of sleep disturbance and shorter weekend sleep time than did healthy controls. The authors identified that those with mHI and complaints of sleep distur-bance were also more likely to complain of brux-ism and manifested a significantly greater BMI. Furthermore, these subjects came from families with a lower level of parental education. Although no information was available regarding preinjury BMI or any patterns of weight gain postinjury, the authors concluded that risk factors for sleep disturbance in mHI include heavier body mass and lower levels of parental education.
In 2004, Korinthenberg and colleagues55 examined predictive factors of posttraumatic syn-drome in children (range, 3–13 years) with mHI.
The authors used data from EEG, in addition to a published neurological examination protocol and a structured validated interview at two time points (T1: within 24 hours of the injury, and T2: 4–6 weeks postinjury) to identify that at follow-up, 23 of 98 patients continued to present with psychiatric complaints, including sleep disturbance and fatigue. These findings did not correlate with the severity of the injury, or somatic, neurologic, or EEG findings immediately postinjury. In their discussion, the authors stated that the “lack of a correlation with the acute concussional symptoms, acute neurological findings and the acute EEG abnormalities suggests that post traumatic com-plaints in our patients are not primarily caused by organic structural or functional changes.“55(p.116) They noted that parental and patient anxiety is a frequent problem even after mHI, and it correlates with persistent symptoms.
In contrast, however, Necajauskaite and col-leagues56 studied 102 matched pairs of children aged 4–16 years, including a case group with mTBI and comparison group with mild bodily injury but no mTBI. They found that although 16.7% of the parents in the case group reported
TABLE 7
Practice Points Research Questions1. It may be of benefit to measure hypocretin-1 in
patients with moderate-severe TBI (who are being monitored for Intracranial Pressure [ICP]) during the acute stage as a potential marker/risk factor for the emergence of sleep and wake disorders.
1. “Future research specifically designed to explore the role of neurophysiologic and psychological factors in the emergence of CRSDs following mTBI may improve our understanding of the nature of this association.” 51(p.1139)
2. Lesions/damage to the hypothalmus are a risk factor for sleep/wake disorders following TBI.
3. Awareness of DSPS as a possible consequence of TBI is important as its symptoms may be over-looked and attributed to the “typical” postconcus-sion syndrome complex.
4. Proper diagnosis of CRSDs is important as a misdiagnosis of insomnia may lead to inappropri-ate prescription of hypnotic medication, which “may help patients fall asleep, but would not be efficacious in normalization of the sleep-wake cycle.” 51(p. 1139)
5. Treatments with melatonin or bright light may be more appropriate with CRSDs.

367Volume 21 Numbers 3-4
sleep disturbances in their children shortly after the trauma (exact time not defined), they did not find any significant differences in subjective reports of sleep disturbance between the two groups in the month prior to follow-up (1–5 years postinjury; mean, 27 months).
In the most recent study to examine sleep in children with mTBI, Milroy and colleagues57 compared 18 children aged 7–12 years with mTBI with 30 children with orthopaedic injuries (aver-age time postinjury, 24 months). These authors used both subjective and objective measures (parental and self-report sleep questionnaires and actigraphy), and while parents reported greater sleep disturbances in the mTBI group, there were no significant differences between the groups with respect to daytime sleepiness, children’s self-report of sleep disturbance, and actigraphy results.
We found only one study that examined sleep in children with moderate-severe TBI. Beebe and colleagues58 compared parental reports of sleep be-haviors in approximately 100 children (aged 6–12 years), 50 with modTBI and 50 with sTBI, with a comparison group of 80 children with orthopaedic
injuries. The children were followed longitudinally over three time points at approximately 6, 12, and 48 months postinjury. The authors reported that for both groups, daytime sleepiness and nocturnal sleep duration were increased following TBI. The modTBI group reported higher baseline sleep problems than the sTBI group and the orthopaedic group; however, this declined over the follow-up period (the specific time course was not specified) to a level consistent with the general population (6–9%). However, the authors reported that the sTBI group displayed an injury-associated increase in sleep problems, with the prevalence nearly doubling from 16% at baseline to 31% postinjury (again, specific timelines were not specified). The authors cautioned that these results should be con-sidered as preliminary given the limitations of the outcome measure; however, they concluded that sleep problems emerge after severe pediatric TBI (and are present in the postacute stage in modTBI).
In conclusion, there is emerging conclusive evidence to support the incidence and prevalence of sleep disturbances in children and adolescents following TBI, across all levels of severity. There
TABLE 8
Practice Points Research Questions1. Children and adolescents with
mTBI/mHI need to be systematically and routinely assessed for subjec-tive complaints of sleep disturbanc-es and followed-up over time.
1. Sleep (and wake) problems in children and adolescents with both mild and moderate-severe TBIs should be evaluated longitudinally by both objective and subjective measures begin-ning at the onset of injury, to determine any patterns in the developmental course of sleep distrubance.
2. Children with moderate-severe TBIs should be followed and assessed for emergence of sleep problems, with provisions of appropriate sleep interventions.
3. Adolescents with mHI, higher BMI, and lower levels of parental educa-tion are at increased risk for sleep disturbances. Educating adoles-cents and parents about healthy eating and regular activity may be of benefit.
4. Providing parents with education and information during the acute stage post mHI may help to allevi-ate anxiety and improve outcome.

368 Critical Reviews™ in Physical and Rehabilitation Medicine
is both subjective and objective evidence docu-menting the prevalence of sleep disturbance in adolescents with mTBI several years postinjury. There is emerging subjective evidence to suggest that sleep disturbances become more prevalent over time in children with sTBI, yet decline over time postinjury in children with modTBI. There is evidence to suggest that sleep problems in children with mTBI do not correlate with initial neuro-logical findings. Clearly, the research on sleep disturbances in children with TBI is in the early stage and warrants further scientific investigation to more clearly identify the nature and patterns of the disturbance, any functional implications, and appropriate interventions.
4. Neuropsychological Implications
Sleep disturbances following TBI have been reported to exacerbate cognitive and behavioral sequelae. We identified four studies of moder-ate quality: three evaluated neuropsychological (and cognitive-communication) function in rela-tion to sleep disorders following TBI, and one documented both sleep and neuropsychological sequelae following nonimpact brain injury. In 2000, Henry and colleagues59 retrospectively investigated the neuropsychological and behav-ioral functioning of 32 adults (aged 18–66 years) with “non-impact brain injury” (i.e., whiplash) up to 65 months postinjury. The authors used a comprehensive battery of standardized neuro-psychological and psychological tests to assess cognition, motor skills, and mood functioning. As the study was retrospective, some subjects had had structural neuroimaging, and three had undergone overnight sleep studies, in addition to neurological examination and interview. Re-sults indicated that patients with whiplash injury demonstrated persistent cognitive, behavioral, and emotional dysfunction years postinjury. Fifty-three percent had problems with sleep (not defined) in addition to difficulties with attention, concentration, executive functions, reduced information processing, word finding, sexuality, anxiety, and depression. Of the three subjects who underwent a nocturnal sleep study, sleep maintenance insomnia was identified with altered sleep stage percentages and altered REM
rhythms. Although the authors cite methodologi-cal limitations as precluding any conclusions regarding causation, finding sleep disturbance following whiplash is not surprising given the shearing injury and potential involvement of the hypothalamus.
In 2004, Mahmood and colleagues60 conducted an investigation of the relationship between sleep disturbance and neurocognitive ability in 87 adults with TBI across all levels of severity who had been admitted to a comprehensive outpatient rehabilitation program. The authors conducted a cross-sectional examination of scores on patients’ neuropsychological examinations, the BDI-II and the PSQI. They reported that: “as would be expected, PSQI scores and BDI-II scores were sig-nificantly correlated because of the partial overlap of depression symptoms and insomnia.”60(p.382) The authors also reported that measures sensitive to higher-order executive functioning and speed of information processing showed a positive relation-ship with PSQI scores. Their findings supported a hypothesis of a predictive relationship between performance on neuropsychological tests and reports of sleep disturbance in adults with TBI.
In 2007, Wilde and colleagues61 examined the impact of comorbid OSA (diagnosed after the TBI) on the cognitive functioning of 19 pa-tients with TBI, in comparison with 16 patients with TBI but without OSA. The subjects were otherwise comparable in terms of age, education, injury severity, time postinjury, and GCS score (where available). The patients with TBI and OSA performed significantly worse on verbal and visual delayed recall measures, and had more at-tention lapses than the patients with TBI without OSA. Interestingly, they did not differ on other measures of visual construction and motor and attention tests. The authors concluded that patients with TBI and OSA had greater impairments in sustained attention and memory than did those patients with TBI without OSA.
In 2010, Wiseman-Hakes and colleagues62 assessed daily self- and clinician (rehabilitation worker) reports of changes in cognitive and communication functioning, including sustained auditory attention/vigilance, speed of language processing, verbal memory, and communica-tion, in response to a course of pharmacological intervention phased in over 17 weeks for post-

369Volume 21 Numbers 3-4
traumatic hypersomnia. The self-report measure used in this study is the newly developed Daily Cognitive-Communication and Sleep Profile (D-CCASP), which is currently undergoing reliability and validity testing (Wiseman-Hakes, 2005, un-published measure). This case-study participant was a young man in his late teens 11 months after sTBI when the study began. As treatment progressed, the authors found a clear positive relationship between improved quality of sleep and language processing (defined as the ability to follow and participate in conversation), sus-tained attention/vigilance (defined as the ability to pay attention and concentrate over time), and memory (defined as the ability to remember things that one has heard, done, or seen). This was seen across the different phases of the medi-cation regime (P < .01). A follow-up conducted at 3 years and 8 months indicated that the gains in sleep, daytime wakefulness, and cognitive-communication function had been maintained. Although the data were limited to one subject, the findings suggest that appropriate, timely, and effective diagnosis, and management of sleep/wake disturbances following TBI, may facilitate improved cognitive-communication function. The authors concluded that their results need to be corroborated with a larger sample size and the addition of standardized neuropsychological and cognitive-communication assessment measures to clinically evaluate reported functional changes.62
5. Intervention
The literature on the treatment of sleep distur-bances following TBI is relatively limited at this time. This may be a reflection of the complexity of this disorder from a number of perspectives; that is, the lack of a clear etiology in many patients, mixed diagnoses, lack of consistency regarding the developmental course of the disorder, and in-teractions with secondary issues such as pain and depression. We identified six papers for review in total: four were of moderate quality and two of high quality. Four of the six articles focused upon pharmaceutical management; of these four, one was for the treatment of fatigue and excessive daytime sleepiness following TBI, one was for the treatment of narcolepsy, another was for the
treatment of insomnia following TBI and stroke, and only one addressed treatments for a number of different types of sleep disorders commonly associated with TBI. The remaining two articles focused on behavioral intervention specifically for insomnia.
These latter two moderate-quality articles by Ouellet and Morin63,64 assessed the efficacy of a protocol of CBT administered by a registered clinical psychologist over a period of 8 weeks. The first paper reports an individual case study and the second reports a single case series. The authors state that cognitive therapy for insomnia consists of “identifying, challenging and altering a set of dysfunctional beliefs and attitudes about sleep,” with the objective of “breaking the cycle of insomnia; dysfunctional thoughts and emotional distress that lead to further sleep disturbances.”63(p.
1299) The authors do a thorough job of delineating the treatment protocol, which was adapted to take into account the deficits in memory, attention, and processing that can occur following TBI.
The results of the case study are promising; the participant experienced reduced sleep onset latencies and nocturnal awakenings, and an in-crease in sleep efficiency. These results were well maintained at follow-up at both 1 and 3 months. The authors built upon these initial results by ex-panding their assessment measures and number of subjects in a single-case series of 11 individuals (six males, five females) with mild to severe TBI. There are a number of relative strengths of this article, despite the small sample size. Subjects were recruited from a variety of locations using a variety of methods, including major rehabilita-tion centers across Quebec, Canada, as well as through advertisements to TBI associations and local support groups. Furthermore, all levels of injury severity were represented, indicating that although the sample size is small, their sample is likely fairly representative of the post-TBI popu-lation. Their results indicated a decline in total overnight wake time relative to baseline, as well as a reduction in overnight sleep variability in 8 of 11 participants. Treatment effects were seen 1–2 weeks after the beginning of therapy. All participants increased their sleep efficiency, and 5 of 11 achieved a sleep efficiency of greater than 90% at the 3-month follow-up. At posttreatment, 7 of 11 no longer fulfilled the diagnostic criteria

370 Critical Reviews™ in Physical and Rehabilitation Medicine
for insomnia. Based on their results, the authors suggest that insomnia associated with TBI can be successfully improved in a large proportion of cases with short-term cognitive behavioral intervention.
The remaining four papers for review ad-dressed pharmacological intervention. Jha and colleagues65 examined the efficacy of modafinil in treating fatigue and excessive daytime sleepiness in individuals with TBI. This high quality, com-prehensive, and well-conceived study consisted of a double-blind placebo cross-over trial in which 53 patients with TBI were randomly assigned to receive up to 400 mg of modafinil, or an equal number of inactive placebo tablets. The partici-pants were a minimum of 1 year postinjury, with a severity level such that they required inpatient rehabilitation (no other information regarding lev-els of severity was provided). For the modafinil regime, patients took 100 mg (one tablet) once per day at noon for 3 days, and then increased to 100 mg 2 times per day for the next 11 days, followed by the maintenance dose of 200 mg twice daily in the morning and at noon. Following the end of the randomized study, both groups were offered a 4-week open label period in which they could receive modafinil using individually clinically monitored titration and a maintenance dosage. However, results indicated that after adjusting for baseline scores and period effects, there were no statistically significant differences between improvements with modafinil versus placebo on any of the outcome measures (Fatigue Severity Scale, the Modified Fatigue Impact Scale, and the ESS). Thus, despite the scientific rigor of this study, there were no consistent and/or persistent clinical improvements.
The next study by Li Pi Shan and Ashworth66 focused specifically on insomnia post-TBI and stroke, and aimed to compare the efficacy of lorazepam and zoplicone as treatment options. This study also followed a double-blind cross-over trial involving 18 patients with TBI or stroke (six patients with TBI, six with a right hemisphere stroke, and six with a left hemisphere stroke; no information about severity or time postinjury). Participants were prescribed 0.5–1.0 mg loraz-epam at bedtime as needed for 7 days, followed by 3.75–7.5 mg zoplicone at bedtime also as needed. Participants were able to regulate their own dosage from 0 to 0.5 to 1 tablet per night,
to “empower them and to simulate what normally happens on our ward.”66(p. 422) Results indicated no significant differences in total sleep time or in subjective measures of sleep. Furthermore, the authors evaluated cognition using the Mini-Mental State Exam (which in our view is an extremely weak and insensitive measure for this purpose, particularly for the TBI population), and found no changes with either medication. The authors concluded that zoplicone and lorazepam are equally effective in the treatment of insomnia for both populations. However, because the authors do not report any baseline information on sleep, the reader is not able to determine any actual level of improvement and any clinical application of their findings is thus negated, which is another weakness of this study.
The most recent study by Castriotta and col-leagues67 aimed to determine whether treatment of specific sleep disorders (which they diagnosed by means of PSG) would result in resolution of those disorders and improvement of symptoms and daytime function. The investigators conducted a thorough, high-quality prospective evaluation of 57 unselected patients with TBI, >3 months postinjury using PSG, MSLT, ESS, and neuro-psychological testing, including the Psychomotor Vigilance Test (PVT), Profile of Mood States, (POMS), and the Functional Outcome of Sleep Questionnaire (FOSQ), prior to and after treat-ment for OSA (23% of 22/57), posttraumatic hypersomnia (PTH) (3%), narcolepsy (5%), PLM (7%), and objective excessive daytime sleepiness (22%). In total, 22 of 57 subjects had abnormal polysomnograms (39%). Treatments included continuous positive airway pressure (CPAP) for OSA, modafinil (200 mg) for narcolepsy and PTH, or pramipexole (0.375 mg) for PLM. In terms of response to treatment, the investigators found that the apneas (and hypopneas, as well as snoring) were eliminated by CPAP; however, there was no significant change in MSLT scores. In addi-tion, they found that PLMs were eliminated with pramipexole. One of three narcolepsy subjects and one of two subjects with PTH had resolutions of hypersomnia with modafinil. However, there were no significant changes in FOSQ, POMS, or PVT results after treatment. The authors concluded that treatment of various sleep disorders after TBI may result in polysomnographic resolution,

371Volume 21 Numbers 3-4
without change in sleepiness or neuropsychologi-cal function.
Overall, the results of these four studies on pharmacotherapy leave us with somewhat of a clinical conundrum. The results of Castriotta and colleagues67 may provide guidance to those treat-ing posttraumatic apnea (and hypopneas), PLMs, and hypersomnia, which makes intuitive sense from a clinical perspective because these disorders are relatively more “clear cut” in their etiology. However, insomnias can be more complex and multi-faceted in their etiology, potentially includ-ing a combination of underlying physiological and psychiatric issues, and thus are often harder to manage pharmacologically without a combina-tion of medications. Furthermore, results of the Shan and Ashworth study66 lead us to conclude that standardized dosages may not be effective, and that any medication regime needs to be fine tuned to the individual needs of the patient, an important protocol built into the final 4 weeks of the study by Jha and colleagues.65 Thus, an ideal treatment regimen may include a trial of cognitive behavior therapy with the addition of pharmacotherapy as needed, specifically tailored to the individuals’ symptoms, body weight, and tolerance. In addition, Castriotta and colleagues67 reported resolution of polysomnographic findings without associated improvements in daytime func-tion, which suggests that a follow-up study may be of benefit, with an individual case-series design in which additional treatments and/or medications could be added that are specific to each participant. Based on the current findings to date, it is clear that intervention for sleep and wake disorders following TBI is an area of significant need with respect to future research directions.
IV. DISCUSSION
This systematic review was conducted to sum-marize the current literature on the topic of sleep and wake disorders following TBI and to critically appraise the research directions. In summary, our findings concur with previous re-views: sleep and wake disorders are a prevalent and complex sequelae of TBI, occurring at all stages across the continuum of recovery from acute, to postacute, to rehabilitation, in both
children and adults, and for a number of patients, continuing for many years postinjury, long into the community. These disorders are complex and multi-factorial, and have an impact on neu-ropsychological functioning and participation in rehabilitation and quality of life. They may evolve from a neurophysiological disruption in brain function to a secondary disorder associ-ated with depression, anxiety, weight gain, and other factors. As such, intervention is equally complex and much more work needs to be done to fully understand the underlying etiologies and to find appropriate treatments. With regard to methodological quality and scientific rigor of the literature, there is a readily observable trend toward higher-quality, more methodologi-cally sound studies as the literature evolves over time. To date, however, most studies have been limited by small sample sizes, large ranges in time postinjury of participants, loss to, or lack of, follow-up, and sample bias due to timing and methods of recruitment. Thus, it is still unclear exactly which members of the TBI population are affected and how the disorder evolves over time. Furthermore, it is unclear why those with mTBI are more likely to present with insomnia or symptoms of insomnia, and whether this is a true manifestation of the disorder or a reflection of other issues such as self-awareness or the challenges of returning to work, school, and/or the community. We recognize, however, that the current state of the literature also reflects the inherent complexities of conducting clinical research with this highly diverse, heterogeneous population.
A. Limitations
Although the current review utilized a systematic approach for the critical appraisal and determina-tion of methodological quality of the literature, we recognize a number of limitations in this methodology. All of the articles included have been peer-reviewed and, as such, there is publica-tion bias. Furthermore, while we have attempted to fully capture all of the recent relevant articles with our search criteria, it is possible that we may have missed articles; thus, this review may not be fully representative of the current literature.

372 Critical Reviews™ in Physical and Rehabilitation Medicine
Given constraints of time, we did not contact any of the study authors directly to clarify any points of confusion; our quality rating system is based upon our understanding of the reporting of the methodology and results, and thus may not be truly representative of the actual study design and quality.
B. What This Review Adds
Despite its limitations, this review adds to the body of knowledge regarding sleep and wake disorders following TBI. To date, it is the most comprehen-sive review, with the inclusion of literature specific to the pediatric population, and is also the first to attempt to delineate the prevalence and nature of sleep disorders by timing of recruitment and levels of severity across the continuum of recovery. It is also the first review to systematically appraise the methodological quality of the current literature.
C. Conclusions and Future Research Directions
Sleep and wake disorders following TBI have received increasingly considerable attention among the clinical and scientific community. Researchers have attempted to quantify the incidence and prevalence of these disorders, as well as to define and describe the nature of the disorder with both subjective and objective measures. Furthermore, attempts have been made to understand the underlying pathophysiological mechanisms and other contributing factors, as well the functional implications and treatment options. However, additional research is needed to fully understand this complex disorder and to identify appropriate and timely interventions. A large, multi-center study is needed that follows all of those with TBI from the acute stage with regular follow-up into the community, such that results can be reliable, valid, and stratified by nature and severity of injury, age, sex, imaging results, and development of the disorder over time. In addition, we recommend that outcomes for either epidemiological or intervention studies should also capture functional outcomes in addition to sleep measures and cognitive measures to fully assess
the impact of the intervention. Finally, we concur with statements by Dr. Richard Castriotta in his recent editorial that “careful study will require much effort and many resources,” which can best be brought to fruition “through collaborative efforts across multiple centers,” with an aim to “elucidate the causes, foster early diagnosis, and develop optimal treatment for these problems.”68(p.
177) These continuing efforts will further inform clinical practice and ultimately contribute to the development of practice guidelines for the systematic evaluation and treatment of sleep and wake disorders following TBI.
ACKNOWLEDGMENTS
This work was supported by the Canadian Insti-tutes of Health Research (CIHR) through a Fel-lowship in Clinical Research and by the Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Pro-gram from the Ministry of Health and Long-Term Care in Ontario, Canada. The views expressed do not necessarily reflect those of the Ministry. None of the authors have any conflicts of interest.
We gratefully acknowledge the assistance of Ms. Reema Farhat and Ms. Sandra Sokoloff, and Ms. Marcia Winterbottom, librarian at the Toronto Rehabilitation Institute, for her assistance with the literature search.
REFERENCES
1. World Health Organization. Neurological disorders: Public health challenges. [published 2010; cited 2010 Mar 18]. Available from: http://www.who.int/neurology/en/.
2. French LM, Parkinson GW. Assessing and treating vet-erans with traumatic brain injury. J Clin Psychol. 2008;64(8):1004–13.
3. United States Department of Defense, Defense and Veterans Brain Injury Center. TBI numbers. [published 2009, cited 2010 Mar 18]. Available from: http://www.dvbic.org.
4. Ouellet MC, Beaulieu-Bonneau S, Morin CM. Insomnia in patients with traumatic brain injury: Frequency, char-acteristics, and risk factors. J Head Trauma Rehabil. 2006;21(3):199–212.
5. Seyone C, Kara B. Head injuries and sleep. In: Lader MH, Cardinali DP, Pandi-Perumal SR, editors. Sleep and sleep disorders: a neuropsychopharmacological ap-

373Volume 21 Numbers 3-4
proach. New York (NY): Landes Bioscience/Eurekah.com & Springer Science + Business Media; 2006.
6. Ouellet MC, Savard J, Morin CM. Insomnia following traumatic brain injury: A review. Neurorehabil Neural Repair. 2004;18(4):187–98.
7. Orff H, Ayalon L, Drummond S. Traumatic brain injury and sleep disturbance: a review of current research. J Head Trauma Rehabil. 2009;24(3):155–65.
8. Zeitzer J, Friedman L, O’Hara R. Insomnia in the con-text of traumatic brain injury. J Rehabil Res Dev. 2009;46(6):827–36.
9. Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005;20(3):229–38.
10. Schneier A, Sheilds B, Hostetler S, Xiang H, Smith G. Incidence of pediatric traumatic brain injury and as-sociated hospital resource utilization in the United States. Pediatrics. 2006;118(2):483–92.
11. Centers for Disease Control and Prevention, Division of Injury Response. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths. [published 2006; cited 2010 Mar 18]. Available from: www.cdc.gov/injury.
12. Tobler I. Is sleep fundamentally different between mam-malian species? Behav Brain Res. 1995;69(1):35–41.
13. Mullington JM. Endocrine function during sleep and sleep deprivation. In: Stickgold R, Walker MP, editors. The neuroscience of sleep. San Diego (CA): Academic Press; 2009. p. 209–212.
14. Maquet P, Smith C, Stickgold R. Sleep and brain plasticity. New York (NY): Oxford University Press Inc; 2003.
15. Walker M. Sleep-dependent memory processing. In: Stickgold R, Walker M, editors. The neuroscience of sleep. San Diego (CA): Academic Press; 2009.
16. Barkoukis TJ, Avidan AY, editors. Review of sleep medicine. Philadelphia (PA): Butterworth, Heinnemann Elsevier Publishing; 2007.
17. Mirmiran M, Ariango R. Role of REM sleep in brain development and plasticity. In: Maquet P, Smith C, Stickgold R, editors. Sleep and brain plasticity. Oxford, United Kingdom: Oxford University Press; 2003.
18. Holm MB. Our mandate for the new millenium: evidence-based practice. Am J Occup Ther. 2000;54(6):575–85.
19. Boschen K, Gargaro J, Gan C, Gerber G, Brandys C. Family interventions after acquired brain injury and other chronic conditions: a critical appraisal of the quality of the evidence. NeuroRehabilitation. 2007;22(1):19–41.
20. Downs S, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
21. Law M. Evidence-based rehabilitation: a guide to practice. Thorofare (NJ): SLACK Inc; 2002.
22. Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro: A database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5(4):223–6.
23. Comper P, Hutchison M, Magrys S, Mainwaring L, Richards D. Evaluating the methodological quality of sports concussion research: a systematic review. Brain Inj. 2010;24(11):1257–71.
24. Baumann CR, Werth E, Stocker R, Ludwig S, Bassetti CL. Sleep-wake disturbances 6 months after traumatic brain injury: a prospective study. Brain. 2007;130(7):1873–83.
25. Castriotta RJ, Wilde MC, Lai JM, Atanasov S, Masel BE, Kuna ST. Prevalence and consequences of sleep disorders in traumatic brain injury. J Clin Sleep Med. 2007;3(4):349–56.
26. Parcell DL, Ponsford JL, Redman JR, Rajaratnam SM. Poor sleep quality and changes in objectively recorded sleep after traumatic brain injury: a preliminary study. Arch Phys Med Rehabil. 2008;89(5):843–50.
27. Gosselin N, Lassonde M, Petit D, Leclerc S, Mongrain V, Collie A, Montplaisir J. Sleep following sport-related concussions. Sleep Med. 2009;10(1):35–46.
28. Makley M, English J, Drubach D, Kreuz A, Celnik P, Tarwater P. Prevalence of sleep disturbance in closed head injury patients in a rehabilitation unit. Neurorehabil Neural Repair. 2008;22(4):341–7.
29. Parcell DL, Ponsford JL, Rajaratnam SM, Redman JR. Self-reported changes to nighttime sleep after traumatic brain injury. Arch Phys Med Rehabil. 2006;87(2):278–85.
30. Rao V, Spiro J, Vaishnavi S, Rastogi P, Mielke M, Noll K, Cornwell E, Schretlen D, Makley M. Prevalence and types of sleep disturbances acutely after traumatic brain injury. Brain Inj. 2008;22(5):381–6.
31. Verma A, Anand V, Verma NP. Sleep disorders in chronic traumatic brain injury. J Clin Sleep Med. 2007;3(4):357–62.
32. Fichtenberg NL, Zafonte RD, Putnam S, Mann NR, Millard AE. Insomnia in a post-acute brain injury sample. Brain Inj. 2002;16(3):197–206.
33. Castriotta RJ, Lai JM. Sleep disorders associated with traumatic brain injury. Arch Phys Med Rehabil. 2001;82(10):1403–6.
34. Burke DT, Shah MK, Schneider JC, Ahangar B, Al-Aladai S. Sleep-wake patterns in brain injury patients in an acute inpatient rehabilitation hospital setting. J Appl Res. 2004;4(2):239–44.
35. Beetar JT, Guilmette TJ, Sparadeo FR. Sleep and pain complaints in symptomatic traumatic brain injury and neurologic populations. Arch Phys Med Rehabil. 1996;77(12):1298–302.
36. Schreiber S, Barkai G, Gur-Hartman T, Peles E, Tov N, Dolberg OT, Pick CG. Long-lasting sleep patterns of adult patients with minor traumatic brain injury (mTBI) and non-mTBI subjects. Sleep Med. 2008;9(5):481–7.
37. Williams BR, Lazic SE, Ogilvie RD. Polysomnographic and quantitative EEG analysis of subjects with long-term insomnia complaints associated with mild traumatic brain injury. Clin Neurophysiol. 2008;119(2):429–38.
38. Chaput G, Giguere J, Chauny J, Denis R, Lavigne G. Relationship among subjective sleep complaints, head-

374 Critical Reviews™ in Physical and Rehabilitation Medicine
aches, and mood alterations following mild traumatic brain injury. Sleep Med. 2009;10(7):713–6.
39. Watson NF, Dikmen S, Machamer J, Doherty M, Temkin N. Hypersomnia following traumatic brain injury. J Clin Sleep Med. 2007;3(4):363–8.
40. Clinchot DM, Bogner J, Mysiw WJ, Fugate L, Corrigan J. Defining sleep disturbance after brain injury. Am J Phys Med Rehabil. 1998;77(4):291–5.
41. Fichtenberg NL, Millis SR, Mann NR, Zafonte RD, Millard AE. Factors associated with insomnia among post-acute traumatic brain injury survivors. Brain Inj. 2000;14(7):659–67.
42. Masel BE, Scheibel RS, Kimbark T, Kuna ST. Excessive daytime sleepiness in adults with brain injuries. Arch Phys Med Rehabil. 2001;82(11):1526–32.
43. Worthington AD, Melia Y. Rehabilitation is compromised by arousal and sleep disorders: Results of a survey of rehabilitation centres. Brain Inj. 2006;20(3):327–32.
44. Ouellet MC, Morin CM. Subjective and objective measures of insomnia in the context of traumatic brain injury: a preliminary study. Sleep Med. 2006;7(6):486–97.
45. Dvorak J, McCrory P, Kirkendall DT. Head injuries in the female football player: incidence, mechanisms, risk factors and management. Br J Sports Med. 2007;41(Suppl 1):i44–6.
46. Covassin T, Swanik CB, Sachs ML. Sex differences and the incidence of concussions among collegiate athletes. J Athl Train. 2003;38(3):238–44.
47. Covassin T, Swanik CB, Sachs M, Kendrick Z, Schatz P, Zillmer E, Kaminaris C. Sex differences in base-line neuropsychological function and concussion symptoms of collegiate athletes. Br J Sports Med. 2006;40(11):923–7.
48. Marshall LF, Marshall SB, Klauber MR, Van Berkum Clark M, Eisenberg H, Jane JA, Luerssen TG, Marmarou A, Foulkes MA. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9(Suppl 1):S287–92.
49. Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep meas-ure. Sleep Med. 2005;6(1):41–4.
50. Baumann CR, Stocker R, Imhof HG, Trentz O, Hersberger M, Mignot E, Bassetti CL. Hypocretin-1 (orexin A) deficiency in acute traumatic brain injury. Neurology. 2005;65(1):147–9.
51. Ayalon L, Borodkin K, Dishon L, Kanety H, Dagan Y. Circadian rhythm sleep disorders following mild trau-matic brain injury. Neurology. 2007;68(14):1136–40.
52. Quinto C, Gellido C, Chokroverty S, Masdeu J. Posttraumatic delayed sleep phase syndrome. Neurology. 2000;54(1):250–2.
53. Kaufman Y, Tzischinsky O, Epstein R, Etzioni A, Lavie P, Pillar G. Long-term sleep disturbances in adolescents after minor head injury. Pediatr Neurol. 2001;24(2):129–34.
54. Pillar G, Averbooch E, Katz N, Peled N, Kaufman Y, Shahar E. Prevalence and risk of sleep disturbances
in adolescents after minor head injury. Pediatr Neurol. 2003;29(2):131–5.
55. Korinthenberg R, Schreck J, Weser J, Lehmkuhl G. Post-traumatic syndrome after minor head injury cannot be predicted by neurological investigations. Brain Dev. 2004;26(2):113–7.
56. Necajauskaite O, Endziniene M, Jureniene K. The prevalence, course and clinical features of post-concussion syndrome in children. Medicina (Kaunas). 2005;41(6):457–64.
57. Milroy G, Dorris L, McMillan TM. Sleep disturbances following mild traumatic brain injury in childhood. J Pediatr Psychol. 2008;33(3):242–7.
58. Beebe DW, Krivitzky L, Wells CT, Wade SL, Taylor HG, Yeates KO. Brief report: parental report of sleep behav-iors following moderate or severe pediatric traumatic brain injury. J Pediatr Psychol. 2007;32(7):845–50.
59. Henry GK, Gross HS, Herndon CA, Furst CJ. Nonimpact brain injury: neuropsychological and behavioral cor-relates with consideration of physiological findings. Appl Neuropsychol. 2000;7(2):65–75.
60. Mahmood O, Rapport LJ, Hanks RA, Fichtenberg NL. Neuropsychological performance and sleep disturb-ance following traumatic brain injury. J Head Trauma Rehabil. 2004;19(5):378–90.
61. Wilde MC, Castriotta RJ, Lai JM, Atanasov S, Masel BE, Kuna ST. Cognitive impairment in patients with traumatic brain injury and obstructive sleep apnea. Arch Phys Med Rehabil. 2007;88(10):1284–8.
62. Wiseman-Hakes C, Murray BJ, Victor C. Sleep/wake disturbance following traumatic brain injury: Impact on functional recovery of cognition and communica-tion: a case study. Brain Inj. 2010;24 (3):376.
63. Ouellet MC, Morin CM. Cognitive behavioral therapy for insomnia associated with traumatic brain in-jury: a single-case study. Arch Phys Med Rehabil. 2004;85(8):1298–302.
64. Ouellet MC, Morin CM. Efficacy of cognitive-behavioral therapy for insomnia associated with traumatic brain injury: a single-case experimental design. Arch Phys Med Rehabil. 2007;88(12):1581–92.
65. Jha A, Weintraub A, Allshouse A, Morey C, Cusick C, Kittelson J, Harrison-Felix C, Whiteneck G, Gerber D. A randomized trial of modafinil for the treatment of fatigue and excessive daytime sleepiness in individuals with chronic traumatic brain injury. J Head Trauma Rehabil. 2008;23(1):52–63.
66. Li Pi Shan RS, Ashworth NL. Comparison of loraz-epam and zopiclone for insomnia in patients with stroke and brain injury: A randomized, crossover, double-blinded trial. Am J Phys Med Rehabil. 2004;83(6):421–7.
67. Castriotta RJ, Atanasov S, Wilde MC, Masel BE, Lai JM, Kuna ST. Treatment of sleep disorders after traumatic brain injury. J Clin Sleep Med. 2009;5(2):137–44.
68. Castriotta RJ. Collaboration in research involving trau-matic brain injury and sleep disorders. J Clin Sleep Med. 2008;4(2):177.