Sleep
-
Upload
lithiya-jose -
Category
Documents
-
view
104 -
download
0
Transcript of Sleep

Spurthy college of nursing
AN ASSIGNMENT
ON
Sleep
SUBMITTED TO,
Mrs. GUNAVATHY, MSc(N)
ASSOCIATE READER
SUBMITTED BY,
MISS. LITHIYA JOSE
FIRST YEAR MSC NURSING
SUBMISSION ON,
09– 12– 2011
1

INDEX
SL NO
CONTENT PAGE NO
1. INTRODUCTION 1
2. DEFINITION 1
3. PHYSIOLOGY OF SLEEP 1-3
4. CICARDIAN RHYTHM 4
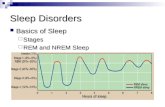
5. STAGES OF SLEEP 4 - 6
6. SLEEP CYCLE 7 - 10
7. FUNCTIONS OF SLEEP 10 – 15
8. NORMAL SLEEP PATTERN 15 - 17
9. MYTHS RELATED TO SLEEP 17 – 18
10. SLEEP PATTERN DISTURBANCES AND MANAGEMENT 18 -25
11. NURSING IMPLICATIONS 26
12. RESEARCH STUDIES RELATED TO SLEEP 27
13. CONCLUSION 27
14. BIBLIOGRAPHY 28
2

Sleep that knits up the ravelled sleave of careThe death of each day's life, sore labour's
bathBalm of hurt minds, great nature's second
course,Chief nourisher in life's feast.
~William Shakespeare, Macbeth
3

4

INTRODUCTION
Sleep is a basic human need. It is a universal biological process common to all people. Historically , sleep was considered a state of unconsciousness. More recently sleep has come to be considered an altered state of consciousness in which the individuals perception of and reaction to the environment are decreased. Some environmental stimuli such as smoke detector alarm, will usually awaken a sleeper, where as other noises will not. It appears that individuals respond to meaningful stimuli while sleeping and selectively disregard un meaningful stimuli.
DEFINITION
Sleep is characterized by minimal physical activity, variable levels of consciousness, changes in the body’s physiologic process and decreased responsiveness to external stimuli.
PHYSIOLOGY OF SLEEP
Sleep is a state of unconsciousness in which the brain is relatively more responsive to internal than external stimuli. The predictable cycling of sleep and the reversal of relative external unresponsiveness are features that assist in distinguishing sleep from other states of unconsciousness. The brain gradually becomes less responsive to visual, auditory, and other environmental stimuli during the transition from wake to sleep, which is considered by some to be stage I of sleep.
Historically, sleep was thought to be a passive state that was initiated through withdrawal of sensory input. Currently, withdrawal of sensory awareness is believed to be a factor in sleep, but an active initiation mechanism that facilitates brain withdrawal is also recognized. Both homeostatic factors (factor S) and circadian factors (factor C) interact to determine the timing and quality of sleep.
The "switch" for sleep is considered to be the ventrolateral preoptic nucleus (VLPO) of the anterior hypothalamus. This area becomes active during sleep and uses the inhibitory neurotransmitters GABA and galanin to initiate sleep by inhibiting the arousal regions of the brain. The VLPO innervates and can inhibit the wake-promoting regions of the brain including the tuberomammillary nucleus, lateral hypothalamus, locus coeruleus, dorsal raphe, laterodorsal tegmental nucleus, and pedunculopontine tegmental nucleus. The hypocretin (orexin) neurons in the lateral hypothalamus helps stabilize this switch. When the hypocretin neurons are lost, narcolepsy can result.[4]
5

The tubero infundibular region projects rostrally to the intralaminar nuclei of the thalamus and to the cerebral cortex. Inhibition of the tubero infundibular region is a critical step toward falling asleep because it results in functional disconnection between the brain stem and the more rostral thalamus and cortex. A decrease in ascending thalamic cholinergic transmissions occurs in association with decreasing cortical responsiveness. In addition to inhibiting higher cortical consciousness, the tuberoinfundibular tract projects caudally into the pontine reticular system and inhibits afferent transmissions from ascending cholinergic tracts.[5]
NREM is an active state that is maintained partly through oscillations between the thalamus and the cortex. The 3 major oscillation systems are sleep spindles, delta oscillations, and slow cortical oscillations. Sleep spindles, a hallmark of stage N2 sleep, are generated by bursts of hyperpolarizing GABAnergic neurons in the reticular nucleus of the thalamus. These bursts inhibit thalamocortical projection neurons. As deafferentation spreads, corticothalamic projections back to the thalamus synchronize. As hyperpolarization of the thalamic reticular neurons progresses, delta waves are produced by interactions from both thalamic reticular and cortical pyramidal sources. Slow cortical oscillations are produced in neocortical networks by cyclic hyperpolarizations and depolarizations.
Although the functions of NREM sleep remain speculative, several theories have been put forth. One theory proposes that decreased metabolic demand facilitates replenishment of glycogen stores. Another theory, which utilizes neuronal plasticity, suggests that the oscillating depolarizations and hyperpolarizations consolidate memory and remove redundant or excess synapses.[6]
REM sleep is generated by the cholinergic mediated "REM-on neurons" in the mesencephalic and pontine cholinergic neurons. The pedunculopontine tegmental nucleus (PPT) and the lateral dorsal tegmental (LDT) neurons use acetylcholine to trigger cortical desynchrony via the thalamus. Cortical desynchrony (also described as low voltage mixed frequency) is the EEG hallmark of REM sleep. An additional EEG hallmark of REM sleep is "sawtooth waves." A pharmacologic offshoot of the cholinergic mediation of REM sleep is stage R increasing with cholinergic agonists and decreasing with anticholinergics.
"REM-off neurons" are the monoadrenergic locus ceruleus and serotonergic raphe neurons. The REM-off neurons use norepinephrine, serotonin, and histamine to inhibit the REM-on cholinergic cells and stop REM sleep. These REM-off neurons become inactive during REM sleep. Medications, such as antidepressants, that increase the amount of norepinephrine or serotonin can cause a pharmacologic suppression of REM sleep.[5, 7]
6

REM sleep (stage R) is characterized by muscle atonia, cortical activation, low-voltage desynchronization of the EEG, and rapid eye movements. REM sleep has a parasympathetically medicated tonic component and sympathetically mediated phasic component. The phasic portion of REM sleep is characterized by skeletal muscle twitches, increased heart rate variability, pupil dilation, and increased respiratory rate.
Muscle atonia is present throughout REM sleep, except for phasic muscle twitches. It results from inhibition of alpha motor neurons by clusters of peri–locus ceruleus neurons, which are referred to collectively as the dorsolateral small cell reticular group.
Projection of the presumed cholinergic, dorsolateral, small-cell, reticular group is through the medullary reticular formation, which projects through the ventrolateral reticulospinal tract to inhibitory spinal and bulbar interneurons. Glycinergic interneurons produce postsynaptic inhibition and hyperpolarization of the spinal alpha motor neurons. Tonic cortical activation with EEG desynchronization is promoted by projections from cholinergic lateral dorsal tegmental and pedunculopontine tegmental neurons to the thalamic nuclei. Other projections through brainstem reticular formation neurons are likely to be involved as well.
Phasic rapid eye movements are composed of lateral saccades generated in the paramedian pontine reticular formation and vertical saccades thought to be generated in the mesencephalic reticular formation. REM density is a term used to describe the frequency per minute of the eye movement bursts.
Phasic pontine-geniculate-occipital (PGO) spikes are another neurophysiological feature of REM sleep seen in animals, but not humans. These spikes appear to be generated by lateral dorsal tegmental and pedunculopontine tegmental neuronal bursts. They are projected to the lateral geniculate and other thalamic nuclei, and then to the occipital cortex. PGO bursts precede rapid eye movements by several seconds. Increases in PGO bursts are seen after REM sleep deprivation.
During NREM sleep, the metabolic demand of the brain decreases. This is supported by oxygen positron emission tomography (PET) studies, which show that, during NREM sleep, the blood flow throughout the entire brain progressively decreases. PET studies also show that, during REM sleep, blood flow increases in the thalamus and the primary visual, motor, and sensory cortices, while remaining comparatively decreased in the prefrontal and parietal associational regions. The increase in blood flow to the primary visual regions of the cortex may explain the vivid nature of REM dreaming, while the continued decrease in blood flow to the prefrontal cortex may explain the unquestioning acceptance of even the most bizarre dream content.
7

CIRCARDIAN RHYTHM
Circadian sleep rhythm is one of the several intrinsic body rhythms modulated by the hypothalamus. The suprachiasmatic nucleus sets the body clock to approximately 24.2 hours, with both light exposure and schedule clues entraining to the 24.2-hour cycle. The retinohypothalamic tract allows light cues to directly influence the suprachiasmatic nucleus. Light is called a zeitgeber, a German word meaning time-giver, because it sets the suprachiasmatic clock. A practical purpose has been proposed for the circadian rhythm, using the analogy of the brain being somewhat like a battery charging during sleep and discharging during the wake period.
The nadir of the rhythm is in the early morning. The downswing in circadian rhythm prior to the nadir is thought to assist the brain to remain asleep overnight for full restoration by preventing premature awakening. The morning upswing then facilitates awakening and through the day acts as a counterbalance to the progressive discharge of wake neuronal activity. After the circadian apex in the early evening, the downswing aids sleep initiation. This model explains the relatively steady cognitive function throughout wakefulness.
Body temperature cycles are also under hypothalamic control. An increase in body temperature is seen during the course of the day and a decrease is observed during the night. The temperature peaks and troughs are thought to mirror the sleep rhythm. People who are alert late in the evening (ie, evening types) have body temperature peaks late in the evening, while those who find themselves most alert early in the morning (ie, morning types) have body temperature peaks early in the evening.
Melatonin has been implicated as a modulator of light entrainment. It is secreted maximally during the night by the pineal gland. Prolactin, testosterone, and growth hormone also demonstrate circadian rhythms, with maximal secretion during the night.
STAGES OF SLEEP
The Beginnings of Sleep
During the earliest phases of sleep, you are still relatively awake and alert. The brain produces what are known as beta waves, which are small and fast. As the brain begins to relax and slow down, slower waves known as alpha waves are produced. During this time when you are not quite asleep, you may experience strange and extremely vivid sensations known as
8

hypnagogic hallucinations. Common examples of this phenomenon include feeling like you are falling or hearing someone call your name.
Another very common event during this period is known as a myoclonic jerk. If you've ever startled suddenly for seemingly no reason at all, then you have experienced this odd phenomenon. While it may seem unusual, these myoclonic jerks are actually quite common.
Stage 1
Stage 1 is the beginning of the sleep cycle, and is a relatively light stage of sleep. Stage 1 can be considered a transition period between wakefulness and sleep. In Stage 1, the brain produces high amplitude theta waves, which are very slow brain waves. This period of sleep lasts only a brief time (around 5-10 minutes). If you awaken someone during this stage, they might report that they weren't really asleep.
Stage 2
Stage 2 is the second stage of sleep and lasts for approximately 20 minutes. The brain begins to produce bursts of rapid, rhythmic brain wave activity known as sleep spindles. Body temperature starts to decrease and heart rate begins to slow.
Stage 3
Deep, slow brain waves known as delta waves begin to emerge during stage 3 sleep. Stage 3 is a transitional period between light sleep and a very deep sleep.
Stage 4
Stage 4 is sometimes referred to as delta sleepbecause of the slow brain waves known as delta waves that occur during this time. Stage 4 is a deep sleep that lasts for approximately 30 minutes. Bed-wetting and sleepwalking are most likely to occur at the end of stage 4 sleep.
Stage 5
Most dreaming occurs during the fifth stage of sleep, known as rapid eye movement (REM) sleep. REM sleep is characterized by eye movement, increased respiration rate and increased brain activity. REM sleep is also
9

referred to as paradoxical sleep because while the brain and other body systems become more active, muscles become more relaxed. Dreaming occurs due because of increased brain activity, but voluntary muscles become paralyzed.
The Sequence of Sleep Stages
It is important to realize, however, that sleep does not progress through these stages in sequence. Sleep begins in stage 1 and progresses into stages 2, 3 and 4. After stage 4 sleep, stage 3 and then stage 2 sleep are repeated before entering REM sleep. Once REM sleep is over, the body usually returns to stage 2 sleep. Sleep cycles through these stages approximately four or five times throughout the night.
On average, we enter the REM stage approximately 90 minutes after falling asleep. The first cycle of REM sleep might last only a short amount of time, but each cycle becomes longer. REM sleep can last up to an hour as sleep progresses.
Comparison of Physiological Changes During NREM and REM Sleep
Physiological Process During NREM During REM
brain activity decreases from wakefulness
increases in motor and sensory areas, while other areas are similar to NREM
heart rate slows from wakefulness increases and varies compared with NREM
blood pressure decreases from wakefulness
increases (up to 30 percent) and varies from NREM
blood flow to brain does not change from wakefulness in most regions
increases by 50 to 200 percent from NREM, depending on brain region
respiration decreases from wakefulness
increases and varies from NREM, but may show brief stoppages (apnea); coughing suppressed
airway resistance increases from wakefulness
increases and varies from wakefulness
10

Comparison of Physiological Changes During NREM and REM Sleep
Physiological Process During NREM During REM
body temperature is regulated at lower set point than wakefulness; shivering initiated at lower temperature than during wakefulness
is not regulated; no shivering or sweating; temperature drifts toward that of the local environment
SLEEP CYCLES
Sleep proceeds in cycles of REM and NREM, the order normally being
N1 → N2 → N3 → N2 → REM. There is a greater amount of deep sleep (stage
N3) earlier in the sleep cycle, while the proportion of REM sleep increases
later in the sleep cycle and just before natural awakening.
NREM sleep (Non-rapid eye movement sleep)
According to the 2007 AASM standards, NREM consists of three stages.
There is relatively little dreaming in NREM.
Stage N1 refers to the transition of the brain from alpha waves having
a frequency of 8–13 Hz(common in the awake state) to theta waves having a
frequency of 4–7 Hz. This stage is sometimes referred to as somnolence or
drowsy sleep. Sudden twitches and hypnic jerks, also known as
positive myoclonus, may be associated with the onset of sleep during N1.
Some people may also experience hypnagogic hallucinations during this
stage. During N1, the subject loses some muscle tone and most conscious
awareness of the external environment. To put it in simpler form, you are in
a very shallow sleep, can jerk awake easily, are slightly aware of your
surroundings, aren't dreaming, and have no rapid eye movement.
Stage N2 is characterized by sleep spindles ranging from 11 to 16 Hz
(most commonly 12–14 Hz) and K-complexes. During this stage, muscular
activity as measured by EMG decreases, and conscious awareness of the
external environment disappears. This stage occupies 45–55% of total sleep
in adults.
Stage N3 (deep or slow-wave sleep) is characterized by the presence
of a minimum of 20% delta waves ranging from 0.5–2 Hz and having a peak-
to-peak amplitude >75 μV. (EEG standards define delta waves to be from 0
11

to 4 Hz, but sleep standards in both the original R&K, as well as the new
2007 AASM guidelines have a range of 0.5–2 Hz.) This is the stage in
which parasomnias such as night terrors, nocturnal enuresis,sleepwalking,
and somniloquy occur. Many illustrations and descriptions still show a stage
N3 with 20–50% delta waves and a stage N4 with greater than 50% delta
waves; these have been combined as stage N3.
REM sleep (Rapid eye movement sleep)
Rapid eye movement sleep, or REM sleep, accounts for 20–25% of total
sleep time in most human adults. The criteria for REM sleep include rapid
eye movements as well as a rapid low-voltage EEG. Most memorable
dreaming occurs in this stage. At least in mammals, a descending
muscular atonia is seen. Such paralysis may be necessary to protect
organisms from self-damage through physically acting out scenes from the
often-vivid dreams that occur during this stage.
Timing
The human biological clock
Sleep timing is controlled by the circadian clock, sleep-
wake homeostasis, and in humans, within certain bounds, willed behavior.
The circadian clock—an inner timekeeping, temperature-fluctuating, enzyme-
controlling device—works in tandem with adenosine, a neurotransmitter that
inhibits many of the bodily processes associated with wakefulness.
Adenosine is created over the course of the day; high levels of adenosine
lead to sleepiness. In diurnal animals, sleepiness occurs as the circadian
12

element causes the release of the hormone melatonin and a gradual
decrease in core body temperature. The timing is affected by
one'schronotype. It is the circadian rhythm that determines the ideal timing
of a correctly structured and restorative sleep episode.
Homeostatic sleep propensity (the need for sleep as a function of the
amount of time elapsed since the last adequate sleep episode) must be
balanced against the circadian element for satisfactory sleep. Along with
corresponding messages from the circadian clock, this tells the body it needs
to sleep. Sleep offset (awakening) is primarily determined by circadian
rhythm. A person who regularly awakens at an early hour will generally not
be able to sleep much later than his or her normal waking time, even if
moderately sleep-deprived.
Sleep duration is affected by the gene DEC2. Some people have a
mutation of this gene; they sleep two hours less than normal. Neurology
professor Ying-Hui Fu and her colleagues bred mice that carried the DEC2
mutation and slept less than normal mice.
Hypnogram showing sleep cycles from midnight to 6.30 am, with deep sleep early on. There is more REM (marked red) before waking.
13

Stage N3 sleep; EEG highlighted by red box. Thirty seconds of deep sleep, here with greater than 50% delta waves.
REM sleep; EEG highlighted by red box; eye movements highlighted by red line. Thirty seconds of sleep.
FUNCTIONS OF SLEEP
The multiple theories proposed to explain the function of sleep reflect the as-yet incomplete understanding of the subject. (When asked, after 50 years of research, what he knew about the reason people sleep William Dement, founder of Stanford University's Sleep Research Center, answered, "As far as I know, the only reason we need to sleep that is really, really solid is because we get sleepy."[37]) It is likely that sleep evolved to fulfill some primeval function and took on multiple functions over time (analogous to the larynx, which controls the passage of food and air, but descended over time to develop speech cabilities).
If sleep were not essential, one would expect to find:
Animal species that do not sleep at all Animals that do not need recovery sleep when they stay awake longer
than usual Animals that suffer no serious consequences as a result of lack of sleep
14

Outside of a few basal animals that have no brain or a very simple one, no animals have been found to date that satisfy any of these criteria.[38] While some varieties of shark, such as great whites and hammerheads, must remain in motion at all times to move oxygenated water over their gills, it is possible they still sleep one cerebral hemisphere at a time as marine mammals do. However it remains to be shown definitively whether any fish is capable of unihemispheric sleep.
FUNCTIONS OF SLEEP
Restoration
Wound healing has been shown to be affected by sleep. A study conducted by Gumustekin et al. in 2004 shows sleep deprivation hindering the healing of burns on rats.
There are multiple arguments supporting the restorative function of sleep. The metabolic phase during sleep is anabolic; anabolic hormones such as growth hormones (as mentioned above) are secreted preferentially during sleep. The duration of sleep among species is, in general, inversely related to animal size and directly related to basal metabolic rate. Rats with a very high basal metabolic rate sleep for up to 14 hours a day, whereas elephants and giraffes with lower BMRs sleep only 3–4 hours per day.
Energy conservation could as well have been accomplished by resting quiescent without shutting off the organism from the environment, potentially a dangerous situation. A sedentary nonsleeping animal is more likely to survive predators, while still preserving energy. Sleep, therefore, seems to serve another purpose, or other purposes, than simply conserving energy; for example, hibernating animals waking up from hibernation go into rebound sleep because of lack of sleep during the hibernation period. They are definitely well-rested and are conserving energy during hibernation, but need sleep for something else.[5] Rats kept awake indefinitely develop skin lesions, hyperphagia, loss of body mass, hypothermia, and, eventually, fatal sepsis.[44]
Ontogenesis
According to the ontogenetic hypothesis of REM sleep, the activity occurring during neonatal REM sleep (or active sleep) seems to be particularly important to the developing organism (Marks et al., 1995). Studies investigating the effects of deprivation of active sleep have shown that deprivation early in life can result in behavioral problems, permanent
15

sleep disruption, decreased brain mass (Mirmiran et al., 1983), and an abnormal amount of neuronal cell death (Morrissey, Duntley & Anch, 2004).
REM sleep appears to be important for development of the brain. REM sleep occupies the majority of time of sleep of infants, who spend most of their time sleeping. Among different species, the more immature the baby is born, the more time it spends in REM sleep. Proponents also suggest that REM-induced muscle inhibition in the presence of brain activation exists to allow for brain development by activating the synapses, yet without any motor consequences that may get the infant in trouble. Additionally, REM deprivation results in developmental abnormalities later in life.
However, this does not explain why older adults still need REM sleep. Aquatic mammal infants do not have REM sleep in infancy; REM sleep in those animals increases as they age.
Memory processing
Scientists have shown numerous ways in which sleep is related to memory. In a study conducted by Turner, Drummond, Salamat, and Brown,[46] working memory was shown to be affected by sleep deprivation. Working memory is important because it keeps information active for further processing and supports higher-level cognitive functions such as decision making, reasoning, and episodic memory.
Memory seems to be affected differently by certain stages of sleep such as REM and slow-wave sleep (SWS). In one study, cited in Born, Rasch, and Gais, multiple groups of human subjects were used: wake control groups and sleep test groups. Sleep and wake groups were taught a task and were then tested on it, both on early and late nights, with the order of nights balanced across participants. When the subjects' brains were scanned during sleep, hypnograms revealed that SWS was the dominant sleep stage during the early night, representing around 23% on average for sleep stage activity. The early-night test group performed 16% better on the declarative memory test than the control group. During late-night sleep, REM became the most active sleep stage at about 24%, and the late-night test group performed 25% better on the procedural memory test than the control group. This indicates that procedural memory benefits from late, REM-rich sleep, whereas declarative memory benefits from early, SWS-rich sleep.
Preservation
The "Preservation and Protection" theory holds that sleep serves an adaptive function. It protects the animal during that portion of the 24-hour day in which being awake, and hence roaming around, would place the individual at
16

greatest risk. Organisms do not require 24 hours to feed themselves and meet other necessities. From this perspective of adaptation, organisms are safer by staying out of harm's way, where potentially they could be prey to other, stronger organisms. They sleep at times that maximize their safety, given their physical capacities and their habitats. (Allison & Cicchetti, 1976; Webb, 1982).
This theory fails to explain why the brain disengages from the external environment during normal sleep. However, the brain consumes a large proportion of the body's calories at any one time and preservation of energy could only occur by limiting its sensory inputs. Another argument against the theory is that sleep is not simply a passive consequence of removing the animal from the environment, but is a "drive"; animals alter their behaviors in order to obtain sleep. Therefore, circadian regulation is more than sufficient to explain periods of activity and quiescence that are adaptive to an organism, but the more peculiar specializations of sleep probably serve different and unknown functions. Moreover, the preservation theory needs to explain why carnivores like lions, which are on top of the food chain and thus have little to fear, sleep the most. It has been suggested that they need to minimize energy expenditure when not hunting.
Preservation also does not explain why aquatic mammals sleep while moving. Quiescence during these vulnerable hours would do the same and would be more advantageous, because the animal would still be able to respond to environmental challenges like predators, etc. Sleep rebound that occurs after a sleepless night will be maladaptive, but obviously must occur for a reason. A zebra falling asleep the day after it spent the sleeping time running from a lion is more, not less, vulnerable to predation.
Dreaming
Dreaming is the perceived experience of sensory images and sounds during sleep, in a sequence which the dreamer usually perceives more as an apparent participant than as an observer. Dreaming is stimulated by the pons and mostly occurs during the REM phase of sleep.
People have proposed many hypotheses about the functions of dreaming. Sigmund Freud postulated that dreams are the symbolic expression of frustrated desires that had been relegated to the unconscious mind, and he used dream interpretation in the form of psychoanalysis to uncover these desires. See Freud: The Interpretation of Dreams.
Freud's work concerns the psychological role of dreams, which does not exclude any physiological role they may have. Recent research claims that sleep has the overall role of consolidation and organization of synaptic connections formed during learning and experience. As such, Freud's work is
17

not ruled out. Nevertheless, Freud's research has been expanded on, especially with regard to the organization and consolidation of recent memory.
Certain processes in the cerebral cortex have been studied by John Allan Hobson and Robert McCarley. In their activation synthesis theory, for example, they propose that dreams are caused by the random firing of neurons in the cerebral cortex during the REM period. Neatly, this theory helps explain the irrationality of the mind during REM periods, as, according to this theory, the forebrain then creates a story in an attempt to reconcile and make sense of the nonsensical sensory information presented to it. Ergo, the odd nature of many dreams.
Hypnotics
Nonbenzodiazepine hypnotics such as eszopiclone (Lunesta), zaleplon (Sonata), and zolpidem (Ambien) are commonly used as sleep aids prescribed by doctors to treat forms of insomnia. Nonbenzodiazepines are the most commonly prescribed and OTC sleep aids used worldwide and have been greatly growing in use since the 1990s. They target the GABAA receptor.
Benzodiazepines target the GABAA receptor also, and as such, they are commonly used sleep aids as well, though benzodiazepines have been found to decrease REM sleep.
Antihistamines, such as diphenhydramine (Benadryl) and doxylamine (found in various OTC medicines, such as NyQuil)
Alcohol – Often, people start drinking alcohol in order to get to sleep (alcohol is initially a sedative and will cause somnolence, encouraging sleep). However, being addicted to alcohol can lead to disrupted sleep, because alcohol has a rebound effect later in the night. As a result, there is strong evidence linking alcoholism and forms of insomnia. Alcohol also reduces REM sleep.
Barbiturates cause drowsiness and have actions similar to alcohol in that they have a rebound effect and inhibit REM sleep, so they are not used as a long-term sleep aid.
Melatonin is a naturally occurring hormone that regulates sleepiness. It is made in the brain, where tryptophan is converted into serotonin and then into melatonin, which is released at night by the pineal gland to induce and maintain sleep. Melatonin supplementation may be used as a sleep aid, both as a hypnotic and as a chronobiotic (see phase response curve, PRC).
Siesta and the "post-lunch dip" – Many people have a temporary drop in alertness in the early afternoon, commonly known as the "post-lunch dip." While a large meal can make a person feel sleepy, the post-lunch dip is mostly an effect of the biological clock. People naturally feel most sleepy (have the greatest "drive for sleep") at two times of the
18

day about 12 hours apart—for example, at 2:00 a.m. and 2:00 p.m. At those two times, the body clock "kicks in." At about 2 p.m. (14:00), it overrides the homeostatic buildup of sleep debt, allowing several more hours of wakefulness. At about 2 a.m. (02:00), with the daily sleep debt paid off, it "kicks in" again to ensure a few more hours of sleep.
Tryptophan – The amino acid tryptophan is a building block of proteins. It has been claimed to contribute to sleepiness, since it is a precursor of the neurotransmitter serotonin, involved in sleep regulation. However, no solid data have ever linked modest dietary changes in tryptophan to changes in sleep.
Marijuana – Some people use marijuana to induce sleepiness. Users often report relaxation and drowsiness.
Stimulants
Amphetamine (dextroamphetamine, and a related, slightly more powerful drug methamphetamine, etc.) are used to treat narcolepsy. Their most common effects are anxiety, insomnia, stimulation, increased alertness, and decreased hunger.
Caffeine is a stimulant that works by slowing the action of the hormones in the brain that cause somnolence, particularly by acting as an antagonist at adenosine receptors. Effective dosage is individual, in part dependent on prior usage. It can cause a rapid reduction in alertness as it wears off.
Cocaine and crack cocaine – Studies on cocaine have shown its effects to be mediated through the circadian rhythm system. This may be related to the onset of hypersomnia (oversleeping) in regard to "Cocaine-Induced Sleep Disorder."
MDMA, including similar drugs like MDA, MMDA, or bk-MDMA – The class of drugs called empathogen-entactogens keep users awake with intense euphoria. Commonly known as "ecstasy."
Methylphenidate – Commonly known by the brand names Ritalin and Concerta, methylphenidate is similar in action to amphetamine and cocaine; its chemical composition more closely resembles that of cocaine.
Tobacco – Tobacco has been found not only to disrupt but also to reduce total sleep time. In studies, users have described more daytime drowsiness than nonsmokers.
Other analeptic drugs like Modafinil and Armodafinil are prescribed to treat narcolepsy, hypersomnia, shift work sleep disorder, and other conditions causing Excessive Daytime Sleepiness. The precise mechanism of these CNS stimulants is not known, but they have been shown to increase both the release of monoamines and levels of hypothalamic histamine, thereby promoting wakefulness.
19

20

NORMAL SLEEP PATTERNS AND REQUIREMENTS
It has been suggested that maintaining a regular sleep wake rhythm is more important than the number of hours actually slept.
Average Sleep Needs
Age Hours
Newborns (0-2 months) 12 - 18
Infants (3 months to 1 year) 14 - 15
Toddlers (1 to 3 years) 12 - 14
Preschoolers (3 to 5 years) 11 - 13
School-aged children (5 to 12 years) 10 - 11
Teens and preteens (12 to 18 years) 8.5 - 10
Adults (18+) 7.5 - 9
1. NewbornsNewborn sleep 16 to 18 hours a day, usually divided in to about
seven sleep periods. NREM sleep is characterized by regular respiration, closed eyes, and the absence of body and eye movements. REM sleep has rapid eye movements that are observable through closed lids, body movements, and irregular respirations. Nearly 50% of sleep is REM.
2. InfantsSome infants sleep 22 hours a day, others 12 to 14 hours a day.
About 20% to 30 % of sleep is REM sleep. At first infants awaken every 3 to 4 hours, eat, and then go back to sleep. Period of awakens gradually increase during the first months. By 4 months most infants sleep through the night and establish a pattern of daytime naps that varies among individuals. At the end of the first year an infant usually takes one or two naps per day and sleeps about 14 of every 24 hours.
3. Adults
21

Stage N1 is considered a transition between wake and sleep. It occurs upon falling asleep and during brief arousal periods within sleep and usually accounts for 2-5% of total sleep time. Stage N2 occurs throughout the sleep period and represents 45-55% of total sleep time. Stage N3 (delta or slow wave sleep) occurs mostly in the first third of the night and constitutes 5-15% of total sleep time. REM represents 20-25% of total sleep time and occurs in 4-5 episodes throughout the night.
3. Elderly
In elderly persons, the time spent in stage N3 sleep decreases, and the time in stage N2 compensatorily increases. Latency to fall asleep and the number and duration of overnight arousal periods increase. This often causes total time in bed to increase which can lead to complaints of insomnia. Sleep fragmentation results from the increase in overnight arousals and may be exacerbated by the increasing number of geriatric medical conditions, including sleep apnea, musculoskeletal disorders, and cardiopulmonary disease.
MYTHS AND FACTS ABOUT SLEEP
Myth 1: Getting just 1 hour less sleep per night won’t affect your daytime functioning. You may not be noticeably sleepy during the day. But even slightly less sleep can affect your ability to think properly and respond quickly, and compromise your cardiovascular health, energy balance, and ability to fight infections.
Myth 2: Your body adjusts quickly to different sleep schedules. Most people can reset their biological clock, but only by appropriately timed cues—and even then, by 1–2 hours per day at best. Consequently, it can take more than a week to adjust after traveling across several time zones or switching to the night shift.
Myth 3: Extra sleep at night can cure you of problems with excessive daytime fatigue. Not only is the quantity of sleep important but also the quality of sleep. Some people sleep 8 or 9 hours a night but don’t feel well rested when they wake up because the quality of their sleep is poor.
Myth 4: You can make up for lost sleep during the week by sleeping more on the weekends. Although this sleeping pattern will help relieve part of a sleep debt, it will not completely make up for the lack of sleep. Furthermore, sleeping later on the weekends can affect your sleep-wake cycle so that it is much harder to go to sleep at the right time on Sunday nights and get up early on Monday mornings.
22

SLEEP PATERN DISTURBANCES
Sleep Disorders and Sleeping Problems
There are many reasons for poor sleep. For example, excessive
exposure to bright light within hours of bedtime or simply resisting the urge
to fall asleep can trigger a "second wind," which then can temporarily make
it difficult to fall asleep afterwards. Following sleep hygienic principles may
solve problems of physical or emotional discomfort. When the culprit is pain,
illness, drugs, or stress, the cause must be treated.Sleep disorders (including
the sleep apneas, narcolepsy, primary insomnia, periodic limb movement
disorder (PLMD), restless leg syndrome(RLS), and the circadian rhythm sleep
disorders) are treatable. Fatal familial insomnia, or FFI, a genetic disease
with no known treatment or cure, is characterized by increasing insomnia as
one of its symptoms; ultimately sufferers of the disease stop sleeping
entirely, before dying of the disease.
Older people are more easily awakened by disturbances in the
environment and may to some degree lose the ability to consolidate sleep.
SYMPTOMS, TREATMENT, AND HELP FOR COMMON SLEEP DISORDERS
At some time, most of us have experienced what it’s like to have trouble falling asleep, to lie awake in the middle of the night, or feel sleepy and fatigued during the day. However, when sleep problems are a regular occurrence—when they get in the way of your daily routine and hamper your ability to function—you may be suffering from a sleep disorder.
Sleep disorders and other sleeping problems cause more than just sleepiness. Poor quality sleep can have a negative impact on your energy, emotional balance, productivity, and health. If you’re experiencing sleeping problems, learn about the signs and symptoms of common sleep disorders, what you can do to help yourself, and when to see a doctor.
23

Understanding sleep disorders and sleeping problems
Sleep can often be a barometer of your overall health. In many cases, people in good health tend to sleep well, whereas repeated sleeping problems may indicate an underlying medical or mental health problem, be it minor or serious. Sleeping well is essential to your physical health and emotional well-being. Unfortunately, even minimal sleep loss can take a toll on your mood, energy, efficiency, and ability to handle stress. Ignoring sleep problems and disorders can lead to poor health, accidents, impaired job performance, and relationship stress. If you want to feel your best, stay healthy, and perform up to your potential, sleep is a necessity, not a luxury.
It’s not normal to feel sleepy during the day, to have problems getting to sleep at night, or to wake up feeling unrefreshed. But even if you’ve struggled with sleep problems for so long that it does seem normal, you can learn to sleep better. You can start by tracking your symptoms and sleep patterns, and then making healthy changes to your daytime habits and bedtime routine. If self-help doesn’t do the trick, you can turn to sleep specialists who are trained in sleep medicine. Together, you can identify the underlying causes of your sleeping problem and find ways to improve your sleep and quality of life.
Signs and symptoms of sleep disorders and sleeping problems
Everyone experiences occasional sleeping problems. So how do you tell whether your sleeping problem is just a minor, passing annoyance or a sign of a more serious sleep disorder or underlying medical condition?
Start by scrutinizing your symptoms, looking especially for the telltale daytime signs of sleep deprivation. If you are experiencing any of the following symptoms on a regular basis, you may be dealing with a sleep disorder.
Is it a sleep disorder?
Do you . . . feel irritable or sleepy during the day? have difficulty staying awake when sitting still, watching television or
reading? fall asleep or feel very tired while driving? have difficulty concentrating? often get told by others that you look tired? react slowly? have trouble controlling your emotions? feel like you have to take a nap almost every day? require caffeinated beverages to keep yourself going?
If you answered “yes” to any of the previous questions, you may have a sleep disorder.
24

Insomnia: The most common type of sleep disorder
Insomnia, the inability to get the amount of sleep you need to wake up feeling rested and refreshed, is the most common sleep complaint. Insomnia is often a symptom of another problem, such as stress, anxiety, depression, or an underlying health condition. It can also be caused by lifestyle choices, including the medications you take, lack of exercise, jet lag, or even the amount of coffee you drink.
Common signs and symptoms of insomnia include:
Difficulty falling asleep at night or getting back to sleep after waking during the night.
Waking up frequently during the night. Your sleep feels light, fragmented, or unrefreshing. You need to take something (sleeping pills, nightcap, supplements) in
order to get to sleep. Sleepiness and low energy during the day.
Whatever the cause of your insomnia, being mindful of your sleep habits and learning to relax will help you sleep better and feel better. The good news is that most cases of insomnia can be cured with lifestyle changes you can make on your own—without relying on sleep specialists or turning to prescription or over-the-counter sleeping pills.
25

Other common types of sleep disorders
In addition to insomnia, the most common sleep disorders are sleep apnea, restless legs syndrome (RLS), and narcolepsy.
Sleep disorder 1: Sleep apnea
Sleep apnea is a common sleep disorder in which your breathing temporarily stops during sleep due to blockage of the upper airways. These pauses in breathing interrupt your sleep, leading to many awakenings each hour. While most people with sleep apnea don’t remember these awakenings, they feel the effects in other ways, such as exhaustion during the day, irritability and depression, and decreased productivity.
Sleep apnea is a serious, and potentially life-threatening, sleep disorder. If you suspect that you or a loved one may have sleep apnea, see a doctor right away. Sleep apnea can be successfully treated with Continuous Positive Airway Pressure (CPAP), a mask-like device that delivers a stream of air while you sleep. Losing weight, elevating the head of the bed, and sleeping on your side can also help in cases of mild to moderate sleep apnea.
Symptoms of sleep apnea include:
Loud, chronic snoring Frequent pauses in breathing during sleep Gasping, snorting, or choking during sleep Feeling unrefreshed after waking and sleepy during the day, no matter
how much time you spent in bed Waking up with shortness of breath, chest pains, headaches, nasal
congestion, or a dry throat.
Sleep disorder 2: Restless legs syndrome (RLS)
Restless legs syndrome (RLS) is a sleep disorder that causes an almost irresistible urge to move your legs (or arms). The urge to move occurs when you’re resting or lying down and is usually due to uncomfortable, tingly, aching, or creeping sensations.
Common signs and symptoms of restless legs syndrome include:
Uncomfortable sensations deep within the legs, accompanied by a strong urge to move them.
The leg sensations are triggered by rest and get worse at night. The uncomfortable sensations temporarily get better when you move,
stretch, or massage your legs. Repetitive cramping or jerking of the legs during sleep.
26

Sleep disorder 3: Narcolepsy
Narcolepsy is a sleep disorder that involves excessive, uncontrollable daytime sleepiness. It is caused by a dysfunction of the brain mechanism that controls sleeping and waking. If you have narcolepsy, you may have “sleep attacks” while in the middle of talking, working, or even driving.
Common signs and symptoms of narcolepsy include:
Seeing or hearing things when you’re drowsy or starting to dream before you’re fully asleep.
Suddenly feeling weak or losing control of your muscles when you’re laughing, angry, or experiencing other strong emotions.
Dreaming right away after going to sleep or having intense dreams Feeling paralyzed and unable to move when you’re waking up or dozing
off.
Circadian rhythm sleep disorders
We all have an internal biological clock that regulates our 24-hour sleep-wake cycle, also known as ourcircadian rhythms. Light is the primary cue that influences circadian rhythms. When the sun comes up in the morning, the brain tells the body that it’s time to wake up. At night, when there is less light, your brain triggers the release of melatonin, a hormone that makes you sleepy.
When circadian rhythms are disrupted or thrown off, you may feel groggy, disoriented, and sleepy at inconvenient times. Circadian rhythms have been linked to a variety or sleeping problems and sleep disorders, including insomnia, jet lag, and shift work sleep difficulties. Abnormal circadian rhythms have also been implicated in depression, bipolar disorder, and seasonal affective disorder, or the winter blues.
Jet lag sleeping problems
Jet lag is a temporary disruption in circadian rhythms that occurs when you travel across time zones. Symptoms include daytime sleepiness, fatigue, headache, stomach problems, and insomnia. The symptoms typically appear within a day or two after flying across two or more time zones. The longer the flight, the more pronounced the symptoms. The direction of flight also makes a difference. Flying east tends to cause worse jet lag than flying west.
In general, it usually takes one day per time zone crossed to adjust to the local time. So if you flew from Los Angeles to New York, crossing three time zones, your jet lag should be gone within three days. However, jet lag can be worse if you:
27

Shift work sleeping problems
Shift work sleep disorder is a circadian rhythm sleep disorder that occurs when your work schedule and your biological clock are out of sync. In our 24-hour society, many workers have to work night shifts, early morning shifts, or rotating shifts. These schedules force you to work when your body is telling you to go to sleep, and sleep when your body is signaling you to wake.
While some people adjust better than others to the demands of shift work, most shift workers get less quality sleep than their daytime counterparts. As a result of sleep deprivation, many shift workers struggle with sleepiness and mental lethargy on the job. This cuts into their productivity and puts them at risk of injury.
There are a numbers of things you can do to reduce the impact of shift work on sleep:
Take regular breaks and minimize the frequency of shift changes. When changing shifts, request a shift that’s later, rather than earlier as
it’s easier to adjust forward in time, rather than backward. Naturally regulate your sleep-wake cycle by increasing light exposure
at work (use bright lights) and limiting light exposure when it’s time to sleep. Avoid TV and computer screens, use black-out shades or heavy curtains to block out daylight in your bedroom.
Consider taking melatonin when it’s time for you to sleep.
Delayed sleep phase disorder
Delayed sleep phase disorder is a sleep disorder in which your 24-hour cycle of sleep and wakefulness—your biological clock—is significantly delayed. As a result, you go to sleep and wake up much later than other people. For example, you may not get sleepy until 4 a.m., at which time you go to bed and sleep soundly until noon, or at least you would if your daytime responsibilities didn’t interfere. Delayed sleep phase disorder makes it difficult for you to keep normal hours—to make it to morning classes, get the kids to school on time, or keep a 9-to-5 job.
It’s important to note that this sleeping problem is more than just a preference for staying up late or being a night owl.
People with delayed sleep phase disorder are unable to get to sleep earlier than 2 to 6 a.m. no matter how hard they try. They struggle to go to sleep and get up at socially acceptable times.
When allowed to keep their own hours (such as during a school break or holiday), they fall into a regular sleep schedule.
Delayed sleep phase disorder is most common in teenagers, and many teens will eventually grow out of it.
28

For those who continue to struggle with a biological clock that is out of sync, treatments such as light therapy and chronotherapy can help. To learn more, schedule an appointment with a sleep doctor or local sleep clinic.
Self-help for sleeping problems and sleep disorders
The first step to overcoming a sleep problem is identifying and carefully tracking your symptoms and sleep patterns.
Keep a sleep diary
A sleep diary is a very useful tool for identifying sleep disorders and sleeping problems and pinpointing both day and nighttime habits that may be contributing to your difficulties. Keeping a record of your sleep patterns and problems will also prove helpful if you eventually find it necessary to see a sleep doctor.
Your sleep diary should include:
what time you went to bed and woke up total sleep hours and perceived quality of your sleep a record of time you spent awake and what you did (“stayed in bed
with eyes closed,” for example, or “got up, had a glass of milk, and meditated.”)
types and amount of food, liquids, caffeine, or alcohol you consumed before bed, and times of consumption
your feelings and moods before bed (e.g. happiness, sadness, stress, anxiety)
any drugs or medications taken, including dose and time of consumption
The details can be important, revealing how certain behaviors can be ruining your chance for a good night’s sleep. After keeping the diary for a week, for example, you might notice that when you have more than one glass of wine in the evening, you wake up during the night.
Improve your sleep hygiene and daytime habits
Learn to recognize & reduce hidden stress
Regardless of your sleep problems, a consistent sleep routine and improved sleep habits will translate into better sleep over the long term. You can address many common sleep problems through lifestyle changes and improved sleep hygiene. For example, you may find that when you start exercising regularly and managing your stress more effectively, your sleep is much more refreshing. The key is to experiment. Use your sleep diary as a jumping off point.
Try the following simple changes to your daytime and pre-bedtime routine:
29

Keep a regular sleep schedule, going to sleep and getting up at the same time each day, including the weekends.
Set aside enough time for sleep. Most people need at least 7 to 8 hours each night in order to feel good and be productive.
Make sure your bedroom is dark, cool, and quiet. Cover electrical displays, use heavy curtains or shades to block light from windows, or try an eye mask to shield your eyes.
Turn off your TV, smartphone, iPad, and computer a few hours before your bedtime. The type of light these screens emit can stimulate your brain, suppress the production of melatonin, and interfere with your body’s internal clock.
Pharmacological treatments
Other treatments
There are various techniques and products which aim to improve
sleep. These range from returning to sleep on the floor since beds are
a relatively recent invention in human history, to various mattress
designs.
RESEARCH STUDIES RELATED TO SLEEP
A 2010 review of published scientific research suggested that exercise
generally improves sleep for most people, and helps sleep disorders
such as insomnia. The optimum time to exercise may be 4 to 8 hours
before bedtime, though exercise at any time of day is beneficial, with
the possible exception of heavy exercise taken shortly before bedtime,
which may disturb sleep. However there is insufficient evidence to
draw detailed conclusions about the relationship between exercise and
sleep. White noise appears to be a promising treatment for insomnia
Anthropology of sleep
Research suggests that sleep patterns vary significantly across
cultures. The most striking differences are between societies that have
plentiful sources of artificial light and ones that do not.The primary
difference appears to be that pre-light cultures have more broken-up
sleep patterns. For example, people might go to sleep far sooner after
the sun sets, but then wake up several times throughout the night,
punctuating their sleep with periods of wakefulness, perhaps lasting
several hours. The boundaries between sleeping and waking are
blurred in these societies. Some observers believe that nighttime sleep
30

in these societies is most often split into two main periods, the first
characterized primarily by deep sleep and the second by REM sleep.
Some societies display a fragmented sleep pattern in which people
sleep at all times of the day and night for shorter periods. In
many nomadicor hunter-gatherer societies, people will sleep on and off
throughout the day or night depending on what is
happening. Plentiful artificial lighthas been available in the
industrialized West since at least the mid-19th century, and sleep
patterns have changed significantly everywhere that lighting has been
introduced. In general, people sleep in a more concentrated burst
through the night, going to sleep much later, although this is not
always true.
In some societies, people generally sleep with at least one other
person (sometimes many) or with animals. In other cultures, people
rarely sleep with anyone but a most intimate relation, such as a
spouse. In almost all societies, sleeping partners are strongly regulated
by social standards. For example, people might only sleep with
their immediate family, extended family, spouses, their children,
children of a certain age, children of specific gender, peers of a certain
gender, friends, peers of equal social rank, or with no one at all. Sleep
may be an actively social time, depending on the sleep groupings, with
no constraints on noise or activity.
People sleep in a variety of locations. Some sleep directly on the
ground; others on a skin or blanket; others sleep on platforms or beds.
Some sleep with blankets, some with pillows, some with simple
headrests, some with no head support. These choices are shaped by a
variety of factors, such as climate, protection from predators, housing
type, technology, and the incidence of pests.
NURSING IMPLICATIONS
Sleep apnoea is largely dealt with in primary care, with people with the condition approaching their GP for advice and treatment. However, nurses in the community may become involved if they detect problems during domicilary visits or surgery appointments, where patients may mention unusual sleepiness in themselves or their partners.
31

Questions about sleep patterns can also be asked at check-up appointments or during lifestyle discussions. Excessive daytime sleepiness with associated relationship problems or reduced motivation will almost certainly affect the way people act and approach other factors in their lives and nurses need to be sensitive to this.
Hospital nurses have a unique opportunity to observe patients sleeping, particularly at night, though clues may be discernible during the day. Any unusual patterns of waking or snoring should be explored with the patient to establish if there might be an underlying problem. Sleep patterns should be explored on admission and during any subsequent discussion on lifestyle (Kron, 1987).
A nurse's understanding of the condition, its diagnosis and treatment may help patients to manage it while in hospital. For example, they may be reluctant to bring CPAP equipment to hospital, thinking it might disturb other patients or that there will not be room for it by the bed.
The nurse role in the use of the CPAP device will differ from that in its use in acute respiratory settings. Here the emphasis is on ensuring the patient can manage the device at home. This would include an explanation and demonstration of how the device works and how to prevent potential problems such as chafing from the mask or nasal cannula, particularly around the nose and ears or conjunctivital oedema. Dehydration or nausea can also cause problems (Mallett and Dougherty, 2000).
CONCLUSION
Sleep is a naturally recurring state characterized by reduced or absent consciousness, relatively suspended sensory activity, and inactivity of nearly all voluntary muscles. It is distinguished from quiet wakefulness by a decreased ability to react to stimuli, and is more easily reversible than being in hibernation or a coma. Sleep is also a heightened anabolic state, accentuating the growth and rejuvenation of the immune, nervous, skeletal and muscular systems. It is observed in all mammals, all birds, and many reptiles, amphibians, and fish.
Sleep is a behavioral state that is a natural part of every individual’s life. We spend about one-third of our lives asleep. Nonetheless, people generally know little about the importance of this essential activity. Sleep is not just something to fill time when a person is inactive. Sleep is a required activity, not an option. Even though the precise functions of sleep remain a mystery, sleep is important for normal motor and cognitive function. We all recognize and feel the need to sleep. After sleeping, we recognize changes that have occurred, as we feel rested and more alert. Sleep actually appears
32

to be required for survival. Rats deprived of sleep will die within two to three weeks, a time frame similar to death due to starvation
33

BIBLIOGRAPHY
1. Carol Taylor. et.al. (2007). 6th edition. Fundamental of Nursing: The
art and Science of nursing care. Wolters kluwer (India) Pvt. Ltd. New
Delhi.
2. Kelly young Lucie & Lucille A. Joel, 3rd edition. The nursing
experience: Trench, Challenges and Transitions. Mc Graw – Hill Health
promotion division, Toronto.
3. Kozier Barbara. et.al. (2006). 7th edition. Fundamentals of nursing:
Concepts, Process and Practice. Pearson Education Dorling Kindersley
(India) Pvt. Ltd., New Delhi.
4. Moyet & Lynda Juall Carpenito. (2006). 11th edition. Nursing
Diagnosis: Application to clinical practice. Wolters Kluwer Health
(India) Pvt. Ltd. New Delhi.
5. Thresyama C.P. (2003). 3RD edition.Fundamental of nursing procedure.Jaypee brothers medical publications.New Delhi.
6. Manindrer Kaur,Lakhwinder Kaur(2011) ist edition. A text book of nursing foundation. PV Books publication. Jalandhar city.
7. www.google.com
8.www.wikepedia.com
34