Sle &; kidney
-
Upload
ayan-santra -
Category
Health & Medicine
-
view
718 -
download
0
Transcript of Sle &; kidney

SLE & KIDNEYAyan Santra, PGT, Dept. of PathologyBurdwan Medical College

Definition•Systemic lupus erythematosus (SLE) is an•autoimmune disease in which organs,
tissues, and cells undergo damage mediated by tissue-binding autoantibodies and immune complexes.
•Ninety percent of patients are women of child-bearing years;
•people of both genders, all ages, and all ethnic groups are susceptible.

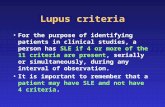
Classification Criteria for the Diagnosis of SLE(≥4 criteria at any point)
• Malar rash Fixed erythema, flat or raised, over the malar eminences• Discoid rash Erythematous circular raised patches with adherent
keratotic scaling and follicular plugging; atrophic scarring may occur
• Photosensitivity Exposure to ultraviolet light causes rash• Oral ulcers Includes oral and nasopharyngeal ulcers, observed by
physician• Arthritis Nonerosive arthritis of two or more peripheral joints, with
tenderness, swelling, or effusion• Serositis Pleuritis or pericarditis documented by ECG or rub or
evidence of effusion

Classification Criteria for the Diagnosis of SLE(≥4 criteria at any point)
• Renal disorder Proteinuria 0.5 g/d or ≥3+, or cellular casts• Neurologic disorder Seizures or psychosis without other
causes• Hematologic disorder Hemolytic anemia or leukopenia
(<4000/L) or lymphopenia (<1500/L) or thrombocytopenia (<100,000/L) in the absence of offending drugs
• Immunologic disorder Anti-dsDNA, anti-Sm, and/or antiphospholipid
• Antinuclear antibodies An abnormal titer of ANA by immunofluorescence or an equivalent assay at any point in time in the absence of drugs known to induce ANAs

Lupus Nephritis•The renal manifestations of SLE is called
lupus nephritis.•Clinical or morphologic involvement of
the kidney in SLE occurs in 50% to 80% of lupus patients at any moment during the course of their disease.
•Renal alterations are found in almost 90% of lupus patients at autopsy

Clinical manifestations•Onset of renal involvement is most
common within the first year •Manifestations varies according to stage
of disease• From asymptomatic to renal failure•The nephritis has the ability to transform
from one morphologic pattern to another spontaneously or after treatment

•In class I and II (mesangial) lupus nephritis, microscopic hematuria is the leading symptom. Proteinuria may be present, but it is not severe or in the nephrotic range.
•In classes III and IV (proliferative) lupus nephritis, nephritic syndrome, with or without nephrotic-range proteinuria, and frequently low complement levels are seen.
• In class V (membranous) lupus nephritis, severe, usually nephrotic-range proteinuria is the most significant symptom, with microscopic hematuria.
•Class VI (chronic sclerosing) lupus nephritis is characterized by chronic renal failure.

Role of Renal Biopsy•It is instrumental in establishing a
diagnosis of SLE or lupus nephritis.•Indications are: •newly diagnosed SLE, •newly appearing renal symptoms; • follow up every 6 months or more after
therapy to gauge the efficacy of treatment and guide further therapeutic management;
• sudden change in renal symptoms & findings

•The biopsy should contain a minimum of 10 glomeruli for light microscopy analysis
•H&E, methenamine-silver, trichrome, and PAS
•Immunofluorescence (IF) should include staining for IgG, IgA, IgM, C3 and C1q
•It is possible to do an adequate and complete classification of the lupus nephritis, without electron microscopy (EM); In cases without IF, EM is essential

Terminologies• Focal-Involving <50% of glomeruli• Diffuse-Involving 50% or more of glomeruli• Segmental-Involving part of a glomerular
tuft(<50%)• Global-Involving all of a glomerular tuft(>50%)• Karyorrhexis: presence of pyknotic and
fragmented nuclei• Mesangial hypercellularity- three or more
mesangial cells in mesangial areas away from the vascular pole, assessed in 3-micron-thick histologic sections

Terminologies• Endocapillary hypercellularity- Increased cellularity
internal to the GBM composed of leukocytes, endothelial cells and/or mesangial cells
• Extracapillary hypercellularity- Increased cellularity in Bowman’s space, i.e. > one layer of parietal or visceral epithelial cells, or monocytes/macrophages
• Fibrinoid necrosis- Lytic destruction of cells and matrix with deposition of acidophilic fibrin-rich material
• Sclerosis- Increased collagenous extracellular matrix that is expanding the mesangium, obliterating capillary lumens or forming adhesions to Bowman’s capsule
• Hyaline-Glassy acidophilic extracellular material

Segmental Global
Mesangial proliferation
Endocapillary proliferation(PAS)

Fibrinoid necrosis
Hyaline

Pathologic Findings•Gross Pathology:•Acute disease: enlarged, swollen kidneys
with petechial hemorrhages and focal, shallow, superficial scars.
•With immunosuppressive therapy: a combination of chronic and acute changes, with a contracted or swollen appearance.

Light Microscopy•Glomeruli:• 1. Immune deposits: large and wide spread• Hyaline and hyper eosinophilic in H&E stain• The trichrome stain highlights the deposits as red (or
fuchsinophilic) against the blue-staining glomerular matrix components
• When large enough to completely involve the peripheral circumference of the glomerular capillary, they are referred to as classic wire loops, which produce a rigid, refractile thickening of the glomerular capillary wall in hematoxylin-eosin stained sections,

Lupus nephritis class IV. Trichrome stain highlights the presence of global subendothelial fuchsinophilic deposits. (Masson's trichrome, ×500.)
Lupus nephritis class IV. In addition to wire-loop deposits, there are segmental intraluminal deposits forming hyaline thrombi. (H&E; ×320.)�

• Active class III or IV lupus nephritis have large intracapillary immune deposits forming hyaline thrombi;
• Can be differentiated from true fibrin thrombi by special stains for fibrin (modified Fraser Lendrum stain and phosphotungstic acid hematoxylin [PTAH] stain) and by staining for fibrin-related antigens by immunofluorescence
Lupus nephritis class IV. The hyaline thrombi stain red against the blue-staining glomerular capillary walls. (Masson's trichrome, ×500

• 2. Glomerular proliferations:
• May be: mesangial, endocapillary, and extracapillary
• Endocapillary proliferation can be defined as a proliferation of endothelial cells and mesangial cells together with infiltrating leukocytes (including mononuclear or polymorphonuclear leukocytes) that significantly narrows or occludes the glomerular capillary lumen.
Lupus nephritis class IV. There is relatively uniform diffuse and global endocapillary proliferation. (H&E; ×100.)

• 3. Glomerular Necrosis: feature of class III or IV lupus nephritis ; never observed in pure mesangial proliferative (class II) or membranous (class V) lupus nephritis.
• Consists of a focus of smudgy fibrinoid obliteration of the glomerular tuft, which is often associated with any or all of the following: deposition of intracapillary fibrin, glomerular basement membrane rupture or gap formation, and apoptosis of infiltrating neutrophils forming pyknotic or karyorrhectic nuclear debris
Lupus nephritis class III. There is segmental fibrinoid necrosis with neutrophil infiltration and pyknosis. (H&E; ×500.)

•4. Hematoxylin Bodies: they are rounded, smudgy, lilac-staining structures, seen as cells with degenerated aspect; probably they represent degenerated nuclei and correspond to LE cells described in the blood of patients with SLE.
•Only truly pathognomonic lesion in lupus nephritis but very uncommon(2%).
Lupus nephritis class IV. Several glomerular capillaries contain hematoxylin bodies. Another lobule contains karyorrhectic nuclear debris. (H&E; ×500.)

•5. Cellular crescents: defined as aggregates comprising two or more layers of proliferating visceral and parietal epithelial cells with infiltrating mononuclear cells lining one fourth or more of the interior circumference of Bowman's capsule.(c.f. single layer of reactive hyperplastic visceral epithelial cells commonly encountered in glomeruli with membranous features or undergoing sclerosis.)
•Encountered frequently in class III or IV lupus nephritis.

•6. Glomerular Scarring: may be focal ,segmental to diffuse, global. Lupus nephritis class IV. Despite
aggressive therapy, repeat renal biopsy two years later shows progression to segmental and global glomerulosclerosis with focal fibrous crescents. There is marked reduction in the degree of interstitial inflammation. (Jones methenamine silver, ×80.)

Tubules and Interstitium•In patients with nephrotic-range proteinuria,
proximal tubules are involved. There are pesence of intracytoplasmic lipid resorption droplets that appear as clear vacuoles in hematoxylin-eosin preparations because of removal of the lipid in the course of tissue processing and protein resorption droplets that appear eosinophilic and strongly PAS-positive and usually trichrome red. The latter change has been referred to as hyaline degeneration of the proximal tubules, �

•Active lesion: interstitial inflammation and edema
•Chronic lesion: tubular atrophy and interstitial fibrosis.
•The interstitial infiltrates consist predominantly of mononuclear leukocytes, including lymphocytes, monocytes, and plasma cells.
•Tubulointerstitial immune deposits: seen in diffuse proliferative lupus nephritis.
• They consist of granular, electron-dense deposits that involve tubular basement membranes, interstitial capillary basement membranes, and interstitial collagen.

Lupus nephritis class IV. High-power view shows a lamellated network of tubular basement membrane splayed around the tubular basement membrane deposits. (Electron micrograph, ×4000.)
Lupus nephritis class IV. The immunofluorescence micrograph shows abundant granular deposits of IgG within the tubular basement membranes and interstitium. (×200.)

• The severity of tubulointerstitial inflammation correlates broadly with glomerular proliferative lesions . It constitutes one of the best morphologic correlates with the degree of renal insufficiency and is an accurate prognosticator of subsequent decline in renal function.
• Tubular atrophy, at least in part the result of interstitial inflammation, is one of the strongest predictors of renal failure , as it is in many other glomerular diseases

Vascular Lesions Arteriosclerosis and arteriolosclerosis Uncomplicated vascular immune deposits Noninflammatory necrotizing vasculopathy
(so-called lupus vasculopathy) Thrombotic microangiopathy
Associated with HUS/TTP syndrome Associated with antiphospholipid antibodies Associated with scleroderma/mixed connective tissue disease
Necrotizing vasculitis (PAN type)

Uncomplicated Vascular Immune Deposits.
• Most common renal vascular lesion in SLE is immune complex deposition in the walls of small arteries and arterioles; deposition occurs to a lesser extent in veins
• Diagnosis requires the demonstration of granular deposits of immunoglobulin (IgG, IgM, and IgA in various combinations), often associated with C1q or C3.
Lupus nephritis class IV. The fluorescence micrograph shows abundant granular staining for IgG within the intima and media of an interlobular artery. (×400.)

Noninflammatory Necrotizing Vasculopathy•Affects predominantly preglomerular
arterioles in the setting of severe active class IV lupus nephritis.
•The affected vessels are severely narrowed and sometimes occluded by abundant intimal and luminal deposits of glassy eosinophilic material that may extend into the media.
•This material is usually fuchsinophilic in trichrome-stained preparations

Lupus vasculopathy. A double panel shows occlusion of preglomerular arterioles by eosinophilic deposits (left) that stain positive with Lendrum stain for fibrin (right). (×500.)

Thrombotic Microangiopathy•Most commonly affect preglomerular
arterioles and interlobular arteries•By LM, the affected vessels are occasionally
narrowed or occluded by intraluminal fibrin thrombi, which may be associated with endothelial swelling and denudation
•By IFM, the affected vessels usually reveal intense, dominant staining for fibrin-related antigens, with variable positivity for IgM and C3.

Renal Vasculitis•Least common vascular lesion•There is leukocyte infiltration of vessel
walls, often accompanied by necrosis.•IFM: strong staining for fibrin-related
antigens with weak and more variable staining for immunoglobulin and complement;
•representing nonspecific trapping of plasma proteins in areas of necrosis.

Immunofluorescence•Immunostaining for IgG in more than 90%
of cases; there is IgA and IgM staining in 60-70% of cases.
•The presence of the three immunoglobulins (Igs) with C3 and C1q is well-known as “full house” pattern, and it is very characteristic of lupus nephritis.

Electron microscopy•Electron dense deposits are demonstrated
with a distribution similar to the one of the immune deposits detected by IF, according to the class.

Classification of Lupus Nephritis• 2003 International Society of Nephrology/Renal
Pathology Society (ISN/RPS) classification of lupus glomerulonephritis (LGN)
• Class I: minimal mesangial lupus nephritis• Normal glomeruli by light microscopy (LM), but mesangial
immune deposits by immunofluorescence (IF) and/or electron microscopy (EM)
• Class II: mesangial proliferative lupus nephritis• Purely mesangial hypercellularity of any degree or
mesangial matrix expansion by LM with mesangial immune deposits; may be a few isolated subepithelial and/or subendothelial deposits by IF and/or EM, but not visible by LM

Lupus nephritis class I. The glomerulus is normal in cellularity, and the glomerular basement membranes are unremarkable. (PAS; ×500.)
Lupus nephritis class II. There is mild, global, mesangial hypercellularity with thin capillary loops. (H&E, ×500.)

• Class III: focal lupus nephritis• Active or inactive focal, segmental or global
endo- or extracapillary glomerulonephritis involving <50% of all glomeruli, typically with focal subendothelial immune deposits,with or without mesangial alterations
• III (A) Active lesions: focal proliferative LGN• III (A/C) Active and chronic lesions: focal
proliferative and sclerosing LGN• III (C) Chronic inactive lesions with glomerular
scars: focal sclerosing LGN

Lupus nephritis class III. A low-power view shows the focal and segmental distribution of the endocapillary proliferation, with some overlying crescents. Endocapillary proliferation affected less than 50% of the total glomeruli in this biopsy. (Jones methenamine silver stain; ×40.)
Lupus nephritis class III. There is segmental obliteration of glomerular capillary lumina by endocapillary proliferation, including infiltrating leukocytes, with associated fibrinoid necrosis. The adjacent lobules display mild mesangial hypercellularity. (H&E; ×400.)

• Class IV: diffuse lupus nephritis• Active or inactive diffuse, segmental or global endo- or extracapillary
glomerulonephritis involving ≥50% of all glomeruli, typically with diffuse subendothelial immune deposits, with or without mesangial alterations. This class is divided into diffuse segmental (IVS) lupus nephritis when ≤50% of the involved glomeruli have segmental lesions, and diffuse global (IV-G) lupus nephritis when ≥50% of the involved glomeruli have global lesions.
• IV-S (A) Active lesions: diffuse segmental proliferative lupus nephritis• IV-G (A) Active lesions: diffuse global proliferative lupus nephritis• IV-S (A/C) Active and chronic lesions: diffuse segmental proliferative and
sclerosing lupus nephritis• IV-G (A/C) Active and chronic lesions: diffuse global proliferative and
sclerosing lupus nephritis• IV-S (C) Chronic inactive lesions with scars: diffuse segmental sclerosing
lupus nephritis• IV-G (C) Chronic inactive lesions with scars: diffuse global sclerosing
lupus nephritis

Lupus nephritis class IV-G. There is diffuse and global endocapillary proliferation involving all the glomeruli in this biopsy. (H&E, ×180).
Lupus nephritis class IV. The low-power immunofluorescence micrograph shows intense, diffuse staining for IgG in the glomerular mesangium and peripheral capillary loops, consistent with a subendothelial distribution. (×120.)

Lupus nephritis class IV. This example has diffuse wire-loop deposits without appreciable endocapillary proliferation. (Masson's trichrome, ×600.)
Wire-loop deposit. By immunofluorescence there is a large subendothelial deposit that conforms to the contour of the glomerular basement membrane, producing a smooth comma-shaped outer contour. (×1000.)

• Class V: membranous lupus nephritis• Global or segmental subepithelial immune
deposits or their morphologic sequelae by LM and by IF or EM, with or without mesangial alterations
• Class V lupus nephritis may occur in combination with class III or IV, in which case both will be diagnosed
• Class V may show advanced sclerosis• Class VI: advanced sclerosing lupus nephritis• >90% of glomeruli globally sclerosed without
residual activity

• Lupus nephritis class V . There are heavy mesangial immune deposits of IgG with more delicate granular subepithelial deposits.(Immunofluorescence micrograph, ×600.)
Lupus nephritis class V . There is regular thickening and rigidity of the glomerular capillary walls accompanied by global mesangial hypercellularity. (H&E; ×500.)

• Indicate the proportion of glomeruli with active and with sclerotic lesions in class III.
• Indicate the proportion of glomeruli with fibrinoid necrosis and/or cellular crescents in class IV.
• Class V may occur in combination with class III or IV, in which case both will bediagnosed.
• Note: Indicate the grade (mild, moderate, severe), tubular atrophy, interstitial inflammation and fibrosis, severity of arteriosclerosis, or other vascular lesions

Lupus nephritis class VI. Extensive glomerular sclerosis shows vestiges of fibrous crescents. The global sclerosis affected more than 90% of glomeruli in this biopsy. Several glomeruli pictured here are segmentally sclerotic. Atrophic tubules alternate with groups of compensatorily hypertrophied tubules. (Masson's trichrome, ×80.)


Definition of active and chronic glomerular lesions according to the2003 ISN/RPS classification of lupus nephritis• Active lesions(0-24)• Endocapillary
hypercellularity (0-3 +) • Leukocyte Infiltration (0-3
+). Neutrophil exudation is defined as more than two neutrophils per glomerulus.
• Subendothelial hyaline deposits (0-3 +)
• Fibrinoid necrosis/karyorrhexis (0-3 +)×2
• Cellular crescents (0-3 +)×2
• Interstitial Inflammation (0-3 +)
• Chronic lesions(0-12)• Glomerular sclerosis
(segmental, global)(0-3)• Interstitial fibrosis(0-3)• Tubular atrophy (0-3)• Fibrous crescents(0-3)0, absent; 1+, less than 25% of glomeruli affected; 2+, 25% to 50% of glomeruli affected; 3+, more than 50% of glomeruli affected

DIFFERENTIAL DIAGNOSIS•Any immune complex GN•IgA nephropathy •HSP •C1q nephropathy •Idiopathic membranous GN(In lupus-
associated membranous GN, there are mesangial,subendothelial deposit,TID and ANA. IF characteristically shows a “full house” pattern.)

Pathogenesis•Three major mechanisms of immune
deposition in the kidney have been identified:
•(a) binding of autoantibodies to intrinsic glomerular antigens,
• (b) binding of autoantibodies to nonglomerular autoantigens that have been planted in the glomerulus, and
•(c) deposition of preformed circulating immune complexes.

•Role of Immunoglobulin :•predominant immunoglobulin isotype in
glomerular deposits is IgG•other immunoglobulin classes (IgM, IgA,
and IgE) may codeposit in glomeruli

•Role of Electric Charge of Immunoglobulin:
•Charge characteristics Igs probably play a role in the localization of immune deposits in lupus nephritis, they are not the major determinant of susceptibility to nephritis

•Autoantibody Specificity and Cross-Reactivity for Glomerular Constituents:
•antibodies to nuclear constituents (i.e., anti-ssDNA, dsDNA, histone, RNP, and nucleosomes),
•cytoplasmic constituents (i.e., anti-Sm), and
•cell membrane antigens (i.e., APL and antiendothelial antibodies).

•lupus autoantibodies bind in situ to normal glomerular cellular or matrix components and that these cross-reactivities may play a major role in the development of nephritis

•Role of Binding of Autoantigens to Glomerular Constituents:autoantigens may first become planted within the glomerulus through particular charge or other physical interactions.
•Once planted in the glomerulus, they are then free to interact with circulating autoantibody, causing the formation of immune complexes in situ

Antibodies to nucleosomes (DNA bound to histones)• During apoptosis, the organized cleavage of
chromatin leads to clustering of nucleosomes on the surface of apoptotic cells
• Normally, these apoptotic bodies are efficiently cleared by effector cells before nucleosomes can be released into the circulation
• In SLE, there is evidence of increased or delayed apoptosis or reduced clearance of apoptotic cells, leading to increased exposure of immunogenic nucleosomes to the immune system and the ensuing formation of nucleosome-specific T cells and antinucleosome autoantibodies


•Role of Deposition of Preformed Immune Complexes: the circulating immune complex load may predispose the patient to particular patterns of lupus nephritis
•Small amounts of intermediate-sized, high-avidity complexes=mesangial pattern
•Larger quantities of intermediate-sized complexes or large complexes =subendothelial deposition

•Cellular and Coagulation Factors:•Deposition of immune complex
activation of cytokine networks
leukocyte recruitment, cellular proliferation, matrix production, and intravascular coagulationGLOMERULAR INJURY

•Genetic Factors: several class I and class II MHC genes are involved
•Epidemiologic Factors:•Race: african american> caucasians•Sex: F>M•Klinefelter's syndrome> hyperestrogenic
state> increased bindining of anti-Ro and anti-La Ab

• B-Cell and T-Cell Abnormalities:• Lupus have enhanced B-cell proliferation,
activation, and immunoglobulin production, and the number of Ig-secreting B cells in the peripheral blood is increased .
• Paradoxically, the number of total B lymphocytes in the peripheral blood is often reduced
• B cells secrete IL-2,IL-6,IL-10, TGF, TNF,IFN.• B cells specific for nuclear antigens may get second
signals from TLRs and may be activated, resulting in increased production of antinuclear autoantibodies.
• Impaired T-cell response to mitogens, antigens, and autologous or allogeneic class II MHC molecules
• CD8+ cells from patients with SLE are often unable to downregulate polyclonal immunoglobulin production and synthesis of autoantibodies

•Antibody Specificity:•The production of autoantibodies, especially
ANA, is a defining feature of SLE and probably an integral pathogenetic factor.
•Clinical manifestation of ANA is LE cell.•The LE cell is a neutrophil or monocyte that
has phagocytosed a nucleus, producing a purplish inclusion in a process that is mediated by antibody to the nucleosomal deoxyribonucleoprotein histone complex
•Antibodies to dsDNA are the most specific for SLE
•Anti histone and anti DNP Abs(against nucleosome) are most common in SLE.

•Complement Abnormalities:•Commonly involve C1,C2 and C4. Due to
null allele.•Low C1q levels have been associated with
proliferative lupus nephritis classes III and IV and may predict the occurrence of renal flares.

Demonstration of LE cell• Twenty millilitres of venous blood are
defibrinated by agitation in a universal (1-oz. bottle) container holding a bent paper clip.
• The defibrinated blood is transferred to a conical tube and centrifuged for five minutes at 1,800 r.p.m.
• The upper cellular layer is transferred by a Pasteur pipette to a Wintrobe tube, which is again centrifuged at 1,800 r.p.m. for five minutes.
• Smears are made from the buffy coat, and stained by the Leishman method.
• The number of L.E. cells per 500 leucocytes is then determined.
• The inclusions show varying grades of density and of colour from deep blue to pink.

References•Sternberg's Diagnostic Surgical
Pathology, 5th ed. 2010, Pg•Heptinstall's Pathology of the Kidney (2-
Volume Set), 6th ed•Fogo_Fundamental of Renal Pathology