Sl 000023
-
Upload
towhidulislam -
Category
Documents
-
view
212 -
download
0
description
Transcript of Sl 000023
-
Clinical Evaluation and Management of PtosisClinical
Dr.S.Krishnakumar, MS Resident, Aravind Eye Hospital, Madurai
Preoperative History and ExaminationThorough evaluation of the patient is essential to accurately determine the degree and type of ptosis. These values are needed to select the appropriate surgical procedure and to inform the patient about the expectation of the surgical outcome. Photographic documentation on pre and post operatively should be done.
Past Medical HistoryA thorough history with particular attention to signs / symptoms of thyroid disease, myasthenia gravis or muscular disorders such as myotonic dystrophy, chronic progressive external ophthalmoplegia or any related myopathies must be elicited. History of medical allergies, bleeding diathesis and haematologic problems must be looked into.
MedicationsCurrent use of medications such as cholinesterase inhibitors for strabismus or glaucoma, platelet inhibitors of any other anticoagulants, cardiac and psychoactive agents must be looked into. Cholinesterase inhibitors must be discontinued at least 3 weeks prior to surgery to prevent prolonged respiratory suppression following intra operative neuromuscular blockade. Anticoagulants are stopped 1-2 weeks pre operatively.
Past ocular historyThe time of onset and associated findings of ptosis are important. In a child pre and perinatal history may be helpful in determining whether a ptosis is congenital or acquired (especially traumatic). Old photographs are invaluable in these situations.
In acquired ptosis, the age of onset and duration of progression are noted. History of variability of eyelid height, diplopia, generalized fatigability, trauma, infection, prior ophthalmic surgeries or family history of adult onset may help determining the aetiology of acquired ptosis.
In adults, it is important to record a history of asthenopia or irritative symptoms that may suggest a tear deficiency. Surgery for ptosis in a patient with history of dry eyes, seventh cranial nerve palsy or significant extra ocular muscle abnormalities such as thyroid related orbitopathy, double elevator palsy or chronic progressive external ophthalmoplegia should be approached with caution. Corneal exposure in these patients may be very difficult to manage.
Clinical Assessment
Visual Acuity
Careful vision test is done using an age appropriate method. It was felt in earlier day that ptosis alone did not produce amblyopia and that anisometropic or strabismus were always the cause. However stimulus deprivation per se in ptosis can cause amblyopia. This problem should be looked for and treated.
Refraction
Cycloplegic test refraction is indicated in all children with ptosis since it is known that a significant number have anisometropia primarily due to astigmatism on the ptotic side. Any significant refractive error should be corrected.
Ptosis Measurements
Measurements are begun with simple observation of the patient. The lid level relative to the globe and the other lid is observed. The presence or absence of lid fold or lid crease gives a significant clue about the degree of levator function. An absent lid crease is often accompanied by poor levator function. If a lid crease is present, but higher than normal (normal lid crease is 8-10mm from the lid margin measured above the pupil) and if there is a deeper upper lid sulcus on that side these should be noted as signs of levator disinsertion. When the
-
2 AECS Illumination
patient is asked to look up, both the sulcus and the lid crease may move up superiorly; slightly before the lid itself moves. This is caused by a delay in levator action due to attenuation or stretching of the normal aponeurotic of the tarsus.
Upper lid height
Vertical fissure height is the distance between the upper lid and lower lid margins measured in the papillary plane (it is the widest here) with the eyes in primary gaze. Normal vertical palpebral fissure height is 7-10 mm in males and about 8-12 mm in females.2 Upper lid ptosis can also be compared with normal eye.
This is a measure of the amount of ptosis in the primary position, with patients brows relaxed. The upper lid can be used as a baseline from which to measure the amount of ptosis. The upper lid normally crosses the cornea 0.5 2mm below upper limbus. In normal situation this relationship is maintained in upgaze and downgaze.
Based on palpebral fissure, ptosis can be classified as mild, moderate and severe (corresponding MRDI) Margin reflex distance. Mild upto 2mm 2 Moderate 3mm 1 Severe >4mm 15mm Good : 12 14mm Fair : 5-11mm Poor :
-
Vol. XIII, No.4, October - December 2013 3
MLD (Margin Limbal Distance)
The margin limbal distance can also measure levator function. The MLD is the distance from the 60 clock limbus to the central upper lid margin when the patient looks in extreme up gaze. Each eyelid is measured separately while the patient follows a light to the extreme superior position of gaze. In bilateral blepharoptosis the upper lid of the eye not being measured is elevated by the examiners finger to prevent to see the light. In unilateral blepharoptosis, the difference in the MLD between the normal and abnormal sides indicates the deficiency in levator function. This difference multiplied by 3 gives the approximate number of millimetres of levator that must be resected. In bilateral blepharoptosis, the amount of levator to be resected is the MLD subtracted from the average MLD of 9mm multiplied by 3. This formula was derived empirically from the pre-operative and post operative study of more than 200 transconjunctival levator muscle resections.
In the transconjunctival isolation and transcutaneous levator resection approach the formula is useful in determining the site of placement of the first tarsus levator suture. Some patients have vertical strabismus associated with blepharoptosis. In many of these patients, the strabismus should be corrected 3-6 month prior to treatment of any residual blepharoptosis. However, other patients with minimal strabismus require treatment only of blepharoptosis. In these patients the MLD is not valid because the 6-0 clock level in upgaze is abnormal owing to the vertical deviation. In such cases MRD3 is used to determine the degree of levator function and amount of levator muscle that must be resected3.
MRD3
MRD3 is the distance from the ocular light reflex to the central upper lid margin when the patient looks in extreme upgaze. In unilateral ptosis, the difference between normal and abnormal MRD3 multiplied by 3 approximately shows the amount of levator that must be resected. Generally MRD3 is equal to MRD1 but in case of associated superior
rectus weakness or palsy MRD3 > MRD1. In bilateral ptosis, the MRD3 is subtracted from the normal average MRD3 of 7 mm and difference is multiplied 3 to determine approximately the number of millimetre of levator muscle to be respected.
MCD (Margin Crease Distance)
If there is an eyelid crease on either eye, the margin crease distance (MCD) should be measured pre-operatively. The MCD is the distance from the central eyelid margin to the central upper lid skin crease with the upper lid in the down position of gaze and skin fold slightly elevated to expose the crease. At surgery the central upper lid margin is elevated from below with the cotton tipped applicator and the crease corresponds to the pre-operative MCD is chosen as the site for post-operative eyelid crease.
Bells PhenomenonTo test for Bells phenomenon, the examiner attempts to separate the lids while the patients close them tightly. Eye with normal bells phenomenon will be upgaze. If the eyes are not in upgaze or if they move to other position of gaze, such as downgaze (inverse Bells phenomenon) lagophthalmos after surgical correction of ptosis may be associated with increased incidence of exposure keratopathy.
Marcus Gunn Jaw Winking PhenomenonThis synkinesis is best demonstrated by having the patient move the jaw the opposite side, but widely opening the mouth or moving the jaw forward would also elevate eyelid. The internal pterygoid may be involved, but more rarely. In such a situation, cleaching the teeth will elevate the eyelid. The patient is instructed to open and close the mouth and to move the jaw side while the examiner observes the blepharoptotic eyelid for associated movement.
Herings LawIn certain circumstance of bilateral ptosis, if one side has marked ptosis and the other side has
-
4 AECS Illumination
minimal ptosis, the side with minimal ptosis may droop more after the greater ptotic side has been corrected. This is due to the Herings law. This is important to predict the postoperative results of ptosis surgery. The patient may have to be warned that the contralateral eye may droop following correction of the greater ptotic lid.
StrabismusThe patient should also be examined for strabismus. If there is hypotropia on the side of ptosis, a pseudoptosis may exist secondary to depression of the eye. Since correction of the strabismus may relieve the blepharoptosis ocular muscle should be performed prior to treatment of blepharoptosis. An exception may be made for cosmetically acceptable strabismus for which only blepharoptosis needs to be treated. If the patient has horizondal strabismus with ptosis, surgery for both strabismus and ptosis can be performed at the same sitting because the result of one rarely influences the result of the other.
Function of Mullers MuscleThe function of mullers is treated by applying drops of 10% phenylephrine to the eye on the side of blepharoptosis. If the upper lid assumes a normal level 10-15 minutes after instillation of the drops, as operation to resect mullers muscle and conjunctiva can relieve blepharoptosis.
Phenylepherine stimulates the sympathetically innervated mullers muscle and gives the surgeon an idea of what can be accomplished by strengthening it through the resection and advancement of mullers muscle and conjunctiva.
The level of the upper lid after phenylephrine test correlates well with its level after the mullers muscle conjunctiva resection procedure. To measure the response to phenylephrine, it is necessary to measure the MRDI before and after its instillation rather than palpebral fissure width, because the lower lid retracts with stimulation of mullers muscle and conjunctiva.
The level of the upper lid after phenylephrine test correlates with its level after the mullers muscle conjunctiva resection procedure. To
measure the response to phenylephrine, it is necessary to measure the MRD1 before and after its instillation rather than palpebral fissure width, because the lower lid retracts with stimulation of mullers in the lower lid. This would give a false value of the palpebral fissure height.
Disinsertion of the Levator AponeurosisDisinsertion of the levator aponeurosis from the tarsus is the cause of some cases of congenital and many cases of acquired ptosis. At times a thin eyelid and a high upper lid crease and fold may indicate a disinserted levator aponeurosis preoperatively. The upper lid crease is formed by levator extension attached to the skin. As the levator aponeurosis recedes into the orbit, it carries the crease with it, leading to higher crease and fold. The upper lid is pulled over the cornea in primary position of gaze. If the iris marking can be seen through the translucent upper lid pulled over the eye, the levator with or without mullers muscle may be disinserted or recessed.
Visual Field TestVisual field tests may be obtained in patients who are able to cooperate in order to document peripheral and superior visual field restriction.
Slit Lamp ExaminationSlit lamp examination of anterior, intraocular pressure and fundus examination are a must prior to surgery to rule out other pathologies. Corneal sensation and staining must be done to detect the presence of corneal anaesthesia or decreased sensation as they might result in injury to the cornea post-operatively.
Tear Film AssessmentTear film abnormality must be looked for and ideally Schirmers test is done in all cases, which are going to be taken up for surgery, especially in acquired ptosis. In adults, measures of basal tear secretion is obtained by Schirmer's testing on the anaesthetized eye. In addition, the cornea tear film should be evaluated for evidence of abnormal debris or tear break up.
-
Vol. XIII, No.4, October - December 2013 5
Dry eye syndrome would be a contraindication for ptosis surgeries, especially sling surgeries as it may cause corneal damage post operatively.
Additional ObservationThe lid contour and lashes are also evaluated. In adults, redundant skin and ptosis of the brow may mask a true ptosis or produce ptosis due to mechanical factors. Orbicularis oculi muscle function should be tested. Palpation of the lids and orbit is important because it may reveal the presence of a mass not otherwise appreciable as the cause of acquired ptosis. The destiny of the ptosis operation is determined by the thoroughness of preoperative lid examination.
Normal Measurements of the Lid4,5
The normal palphebral fissure is 26 to 30mm in horizontal dimension and 8-10mm in height (7-10 mm in males and 8-12mm in females). The distance from the papillary light reflex to the upper lid (MRDI) ranges between 2 to 5mm and the distance from papillary light reflex to lower eyelid (MRD2) is between 4.5mm to 5.5mm. The normal lid rests 1-2mm below 120 clock border of the limbus and lower eyelid at 6o clock border of the limbus, although it may be slightly above or below this level. The distance between 2 medial acanthi is normally 30 to 34 mm. The puncta are approximately 6 -7 mm from medial canthal angle. Medial canthal angle is 0 to 2mm below the lateral canthal angle in most individuals. The tarsus is approximately 1mm in thickness and 24 mm to 28 mm in length. The height of the upper lid tarsus is usually 10mm, and the average height of lower lid tarsus is 3-7mm.
Evaluation of Infantile PtosisThe office evaluation of infantile ptosis elicits information similar to the adult ptosis examination but requires the physician to practice preverbal entertainment skills and be willing to approximate measurements.
As in any case of ptosis, palpebral fissure, margin reflex distance, lagophthalmos and levator function are assessed. The presence of bells and
integrity of corneal epithelium are assessed. Motility is examined, especially superior rectus weakness. Head tilt and the use of the brow for lid elevation are documented. Sucking or chewing are used to elicit jaw wink response. The most important measurement however, is the levator function. The levator function is measured in millimetres as the full excursion of lid from downgaze to upgaze, excluding lift resulting from frontalis muscle. Levator function may be classified as good, fair or poor. Millimeter values can be placed on these descriptions.
Good :
-
6 AECS Illumination
Non-surgical Treatment1
1. Lid crutches may be used to support a drooping lid mechanically. The type used is a wire support in the form of a semi lunar soldered to the upper part of the rims of a pair of spectacles.
2. Haptic contact lens with a shelf on which the margin of upper lid rests may be used.
3. Elevation of the lid by a mechanic force: a strip of highly magnetically metal is implanted in the upper lid and a magnet is placed behind the upper rim of the frame.Surgical treatment however, is required in
most cases of ptosis to obtain a satisfactory result from cosmetic and functional points of view. Over 100 modifications of techniques are to be found in literature all of which can be resolved into a few general procedures.
When to correct ptosis surgically6
Correction of ptosis in a child can often be delayed until the patient is several years old, although consistent chin up positionings / complete ptosis may justify early surgery6. In general, congenital ptosis should be repaired when accurate measurements are obtainable and before the child begins school. Most children can undergo repair around 4-5 years of age. Severe ptosis, which may cause amblyopia, must be surgically repaired as soon as possible to preserve normal vision.
Note : An acquired ptosis from a traumatic injury or a third nerve palsy should not be operated on before 6 months of age, because often some levator function will return. Any other acquired ptosis may be repaired when the cause has been determined. Specially myasthenia gravis must be ruled out.
Indications for surgery in congenital ptosisIn most instances the primary reason for correcting congenital ptosis is cosmetic. In case of unilateral congenital ptosis of such severity that normal visual development is compromised by total
occlusion of visual axis, surgical intervention may be indicated shortly after birth.
In cases of severe bilateral ptosis that interferes with the childs learning walk, surgery may be indicated early. The levator action in these children is always so poor that a frontails sling procedure is necessary.
In general, ptosis causing significant stimulus deprivation or head posturing must be surgically treated without fail. Milder degrees of ptosis need to be corrected only if the patient desires good cosmesis.
ContraindicationsPoor orbicularis muscle function may produce lagophthalmos and corneal exposure. Loss of blink reflex or corneal sensitivity, paralysis of orbicularis or significant keratitis sicca are definite contraindications for ptosis surgery. Total ophthalmoplegia may also result in postoperative corneal exposure as the cornea is exposed during sleep.
Some ophthalmologists feel the presence or absence of Bells phenomenon is of significant importance in ptosis surgery in most circumstances, its absence is not a contraindication for surgery in patients with congenital ptosis. However, extreme caution should be exercised in these patients, as also in those with decreased random movement during sleep.
Choice of Surgery for PtosisIn general there are three major groups of ptosis surgery.1. External levator resection (including
aponeurotic repair) for >4mm for levator function.
2. Posterior tarso muller muscle resection (not generally used in congenital ptosis unless due to congential horners).
3. Frontalis suspension.In severe unilateral ptosis, bilateral suspension
can be considered combined with weakening of opposite normal levator. This beard technique
-
Vol. XIII, No.4, October - December 2013 7
leads to excellent symmetric results. However many surgeons prefer to leave the normal eyelid alone.
Principles of surgical correction of ptosisOne inherent drawback to all ptosis procedure is that perfect cosmetic and functional results cannot be expected in every case. In general, the
If in doubt most surgeons prefer to overcorrect, because, over correction is easier to treat than an under correction. An under-correction requires a second ptosis surgery under less favourable conditions than the first. This is because the second surgery will have to be done in the presence of scar tissue, bleeding, obliteration and / or distortion of normal anatomic landmarks.
final result depends on the nature of ptosis, the type of operation selected and the skill with which operation is performed6.
Levator resection is performed on all levator maldevelopment (congenital dysmyogenic) ptosis cases with levator action of 4 or more whereas frontalis sling is performed when the levator action is 3 mm or less.
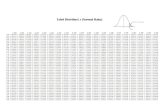
Guidelines for correction of levator maldevelopment ptosis in millimeters6.
Degree of Ptosis Levator Function Amount of levator resection
Ideal preoperative correction
1.5 2 mm (mild) Good (8 or more)Good (8 or more)- usual
Small (10-13) Moderate (14 -17)
Under correct by1 - 3mm
3 mm (moderate) Fair (5-7) sometimesPoor (4 or less) rare
Large (18-22)Maximal (23 or more)
Match the level of normal lid and correct ptosis fully.
4 or more (severe) Fair (5-7) sometimesPoor (4 or less) usual
Super maximal(27 or more)Frontalis sling
Over correct by 1-2mm
The aim of any operation should be to lift the ptotic lid above the papillary aperture when the eyes are in the primary position. The height of the two lids regardless of whether the ptosis is unilateral or bilateral should be equal. There should also be adequate mobility of the lid when blinking, a normal lid fold and no diplopia.
References
1. System of ophthalmology edited by Sur Stewart Duke Elder. Congenital deformities Vol.3 part. 2
2. Clinical ophthalmology. Jack J. Kanski. Fifth Edition. Butterworth Heinemann publishers. P 32-39.
3. Allen M Puttrman. Basic oculoplastic surgery in Vol.3. Chap 33 P.2251. Edited by Peyman GA, Sanders DR, Goldberg MF. Ist Indian eition. Jaypee brothers.
4. Putterman Am: Basic oculoplastic surgery. In Peyman GA, Sanders DR, Goldberg MF (eds). Principles of practice of ophthalmology. P2248-2250 philadelphia, WB saunders, 1980.
5. Putterman Am: Evaluation of the cosmetic oculoplastic surgery 2nd Ed. P12-26. Philadelphia, WB saunders, 1993.
6. Paediatric Ophthalmology and Strabismus Sec.6. 2001-2002. P-172.