Severe Combined Immunodeficiency - OMED 2017 · 9/18/2017 5 XSCID X-linked SCID Failure to thrive...
Transcript of Severe Combined Immunodeficiency - OMED 2017 · 9/18/2017 5 XSCID X-linked SCID Failure to thrive...

9/18/2017
1
Severe Combined Immunodeficiency
Nancy Joseph, D.O.Allergy/Immunology FellowPGY IVUniversity Hospitals, Cleveland Medical Center, Cleveland, OH
Disclosures
No disclosures
Objectives
Define Pathogenesis Clinical Presentation Subtypes/Classification Neonatal Screening Diagnosis Management & Treatment

9/18/2017
2
Lymphocyte Subsets◦ CD3- T cells◦ CD4- Helper T cells◦ CD8- Cytotoxic T cells◦ CD16/56- NK cells◦ CD19- B cells◦ CD45 RA/RO- Naïve T cells/Memory T cells
SCID
• Severe combined immunodeficiency (SCID), (also known as "Alymphocytosis," "Glanzmann–Riniker syndrome," "Severe mixed immunodeficiency syndrome," and "Thymic alymphoplasia") is a genetic disorder characterized by the absence of functional T-lymphocytes,which results in a defective antibody response due to either direct involvement with B lymphocytes or through improper B lymphocyte activation due to non-functional T-helper cells.
• Consequently, both "arms" (B cells and T cells) of the adaptive immune system are impaired due to a defect in one of several possible genes.
• SCID is the most severe form of primary immunodeficiencies,[4] and there are now at least nine different known genes in which mutations lead to a form of SCID.
• It is also known as the bubble boy disease because its victims are extremely vulnerable to infectious diseases and some of them, such as David Vetter, become famous for living in a sterile environment.
• SCID is the result of an immune system so highly compromised that it is considered almost absent.

9/18/2017
3
Definition
Genetic disorder Inhibited T lymphocyte differentiation
Variably affects other lymphocyte lineages (i.e. B or NK cells)
1 in 40,000-50,000 births
Pathogenesis
Mutations in 13 different genes Severe lymphocyte depletion 100% mortality without treatment
Irradiated blood transfusions (GVHD) No live vaccines Common & opportunistic infections
Classification
Classify based upon the presence of molecular defects affecting T cells +/- B or NK cells

9/18/2017
4
Gaspar et al. November 28, 2013; Blood: 122 (23)
Clinical Features
Regardless of underlying molecular defect presentation is similar
Present within first few months of life Opportunistic infections
GVH Underdeveloped lymphoid tissue
http://openi.nlm.nih.gov

9/18/2017
5
XSCID
X-linked SCID
Failure to thrive Chronic thrush PCP
X-linked SCID
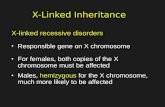
• X-linked severe combined immunodeficiency (X-SCID) is an immunodeficiency disorder in which the body produces very few T cells and NK cells.
• In the absence of T cell help, B cells become defective. • It is an x-linked recessive trait, stemming from a mutated
(abnormal) version of the IL2-RG gene located at xq13.1 on the X-chromosome, which is shared between receptors for IL-2, IL-4, IL-7, IL-9, IL-15 and IL-21

9/18/2017
6
Pathophysiology of X-SCID
T cell T cell
Normal Il2R Abnormal IL2R
Clinical
• Persons afflicted with X-SCID often have infections very early in life, before three months of age.
• This occurs due to the decreased amount of immunoglobulin G (IgG) levels in the infant during the three-month stage. This is followed by viral infections such as pneumonitis, an inflammation of the lung which produces common symptoms such as cough, fever, chills, and shortness of breath.
• A telltale sign of X-SCID is candidiasis, a type of fungal infection caused by Candida albicans.
• Candidiasis involves moist areas of the body such as skin, the mouth, respiratory tract, and vagina; symptoms of oral candidiasis include difficulty in swallowing, pain on swallowing and oral lesions.
• Recurrent eczema-like rashes are also a common symptom. Other common infections experienced by individuals with X-SCID include diarrhea, sepsis, and otitis media.
• Some other common symptoms that are experienced by X-SCID patients include failure to thrive, gut problems, skin problems, and muscle hypotonia
Genetics• X-SCID is caused by a mutation occurring in the xq13.1 locus of the X-chromosome.
• Most often, this disease affects males whose mother is a carrier (heterozygous) for the disorder.
• Because females have two X-chromosomes, the mother will not be affected by carrying only one abnormal X-chromosome, but any male children will have a 50% chance of being affected with the disorder by inheriting the faulty gene.
• Likewise, her female children will have a 50% chance of being carriers for the immunodeficiency. X-SCID can also arise through de novo mutations and X-inactivation.
• A de novo mutation is an alteration in a gene caused by the result of a mutation in a germ cell (egg or sperm) or in the fertilized egg itself, rather than having been inherited from a carrier.
• Since only 1/3 of all X-SCID patients have a positive family history of SCID, it is hypothesized that de novo mutations account for a significant percentage of cases.
• X-inactivation occurs when one of the X-chromosomes on the female becomes inactivated due to a mutation, resulting in the active form of just one chromosome.
• If their normal X-chromosome has been inactivated, female carriers of X-SCID will have a 100% chance of passing the disorder to their children.

9/18/2017
7
Pathophys• The gene that encodes the common gamma chain in these interleukins is
mutated in X-SCID. • The mutation leads to an absent or abnormally functioning common gamma
chain. The mutation can occur through large, or even single nucleotide, deletions in the IL2RG gene, that disable the common gamma chain so that it is unable to bind with other receptor subunits and signal cytokine activation.
• Normally, when the interleukin binds to the trimeric receptor protein containing the alpha, beta, and gamma subunits, the common gamma subunit activates Janus Kinase 3 (JAK3), which leads to the phosphorylation of Signal Transducer and Activator of Transcription 5, STAT5.
• The STAT5 proteins dimerize and translocate to the nucleus, controlling subsequent downstream signalling.
• Due to the fact that the common gamma chain is absent or abnormal, this downstream pathway is inhibited.
• This change prevents the T-lymphocytes from signaling other cells, like B-lymphocytes and natural killer cells.
• Because these cells never receive these signals, they can never mature and differentiate into full grown immune cells.
Treatment
Bone marrow transplantation (BMT) is a standard curative procedure and results in a full immune reconstitution, if the treatment is successful
Bone Marrow Transplant

9/18/2017
8
X Linked SCID
50% of cases Xq13/IL2RG T-NK-B+
http://www.bioniz.com
SCID
• The second most common form of SCID after X-SCID is caused by a defective enzyme, adenosine deaminase (ADA), necessary for the breakdown of purines.
• Lack of ADA causes accumulation of dATP. • This metabolite will inhibit the activity of ribonucleotide
reductase, the enzyme that reduces ribonucleotides to generate deoxyribonucleotides.
• The effectiveness of the immune system depends upon lymphocyte proliferation and hence dNTP synthesis.
• Without functional ribonucleotide reductase, lymphocyte proliferation is inhibited and the immune system is compromised.
Adenosine Deaminase Deficiency (ADA)

9/18/2017
9
ADA Deficiency
16% of cases Autosomal recessive 20q13 Profound lymphopenia◦ T-NK-B-
Defect of Protein Catabolism

9/18/2017
10

9/18/2017
11
Purine nucleoside phosphorylasedeficiency
An autosomal recessive disorder involving mutations of the purine nucleoside phosphorylase (PNP) gene. PNP is a key enzyme in the purine salvage pathway. Impairment of this enzyme causes elevated dGTP levels resulting in T-cell toxicity and deficiency.
A Great Ending!!!!

9/18/2017
12
Other Causes
IL-7Ra deficiency ◦ 12% of cases◦ T-NK+B+
JAK 3 Kinase deficiency◦ 6% of cases◦ T-NK-B+
Omenn Syndrome◦ 4% of cases◦ T-NK+B-
ZAP70 deficiency
It is characterized by a lack of CD8+ T cells and the presence of circulating CD4+ T cells which are unresponsive to T-cell receptor (TCR)-mediated stimuli.

9/18/2017
13
IL7R SCID
• Recently, two SCID (severe combined immunodeficiency disease) patients with greatly diminished T cells but normal or increased numbers of B and NK cells (T–
B+NK+ SCID) were found to have mutations in the gene for the IL-7 receptor.
• This has established a major role for IL-7-receptor-dependent signaling in T cell development in humans and probably explains the diminished T cell numbers seen in patients with X-linked SCID or SCID that results from Jak3-deficiency.
JAK3
Janus kinase-3 (JAK3) is an enzyme that mediates transduction downstream of the Gamma chain signal.
Mutation of its gene causes SCID

9/18/2017
14
JAK3 SCID
Defects of the JAK3 gene result in a type of T-B+NK- SCID that is transmitted via an autosomal recessive mode of inheritance
JAK3 SCID
SCID due to JAK3 deficiency is rare, accounting for only about 6 percent of all cases of SCID and approximately 1 percent of all cases of immunodeficiency of known genetic origin

9/18/2017
15
Omenn syndrome
• The manufacture of immunoglobulins requires recombinase enzymes derived from the recombination activating genes RAG-1 and RAG-2.
• These enzymes are involved in the first stage of V(D)J recombination, the process by which segments of a B cell or T cell's DNA are rearranged to create a new T cell receptor or B cell receptor (and, in the B cell's case, the template for antibodies).
• Certain mutations of the RAG-1 or RAG-2 genes prevent V(D)J recombination, causing SCID
Bare lymphocyte syndrome
MHC class II is not expressed on the cell surface of all antigen presenting cells. Autosomal recessive.
The MHC-II gene regulatory proteins are what is altered, not the MHC-II protein itself.

9/18/2017
16
B CELLS CONTROL
MONOS PT
B CELLSCONTROL

9/18/2017
17
B CELLS PATIENT
Newborn ScreeningSCID Buckley et al◦ Improved survival with diagnosis prior to
infections >80% SCID infants were the first known
family member affected 2010 DHHS requested SCID screening be
made available and be capable of being run on dried blood samples.◦ TREC (T cell receptor excision circles) most
sensitive and specific.
Newborn ScreeningTREC count
◦ TRECs Produced by naive T cells in thymus Excised DNA during VDJ rearrangement Low or undetectable regardless of SCID subtype

9/18/2017
18
http://www.perkinelmer.com
Clinics vol.67 no.5 São Paulo 2012
Borte et al. March 15, 2012; Blood:119(11)

9/18/2017
19
Differential(Low TREC) SCID DiGeorge syndrome Trisomy 21 Rac2 or DOCK8 deficiencies HIV1

9/18/2017
20
PMDsLow TREC count. Now what do I do?
Referral to qualified Immunologist Labs to order◦ CBC with differential◦ Flow cytometry (CD markers)◦ T cell function ◦ +/- serum immunoglobulins (IgA, IgG, IgM)
Rule out DiGeorge Syndrome◦ Thymus transplant
Initial Management
Protective measures◦ Reverse isolation◦ No live vaccines◦ Blood products Irradiated leukodepleted & CMV (-)
◦ Nutrition ◦ IVIG/prophylaxis
Treatment
BMT◦ Preferred MSD (matched sibling donor)
Enzyme replacement therapy◦ Peg-ADA
Gene therapy

9/18/2017
21
Gaspar et al. November 28, 2013; Blood: 122 (23)
Now for some questions….

9/18/2017
22
True or false?
SCID is also known as bubble boy disease
True
True or false?
SCID involves Inhibited T lymphocyte differentiation?

9/18/2017
23
True
What is the most common type of SCID? ADA deficiency X-linked SCID Zap70 Deficiency RAD deficiency
What is the most common type of SCID? ADA deficiency X-linked SCID ZAP70 Deficiency JAK3 Kinase deficiency

9/18/2017
24
Which of the following is not part of SCID treatment/precautions
◦ Reverse isolation◦ live vaccines◦ Blood products : Irradiated leukocyte
depleted & CMV (-)◦ Nutrition ◦ IVIG/prophylaxis
◦ Reverse isolation◦ live vaccines◦ Blood products: Irradiated leukocyte depleted
& CMV (-)◦ Nutrition ◦ IVIG/prophylaxis
What is the curative treatment for SCID IVIG Thymic replacement BMT Prophylactic Antibiotics

9/18/2017
25
What is the curative treatment for SCID IVIG Thymic replacement Bone Marrow Transplant Prophylactic Antibiotics
What is the Diagnosis?
CD3(T cells) Absent CD4(T cells) Absent CD8(T cells) Absent CD19(B cells) Absent
ADA/PNP deficiency

9/18/2017
26
True or False?
The inheritance pattern of PNP is autosomal recessive?
True
What is the diagnosis?
CD3(T cells) Absent CD4(T cells) Absent CD8(T cells) Absent CD19(B cells) Present

9/18/2017
27
X-linked SCID
What is the Diagnosis?
CD3 low CD4 low CD8 absent CD19 low
Zap 70 Deficiency

9/18/2017
28
What is the diagnosis?
CD3(T cells) Normal CD4 Normal CD8 Normal CD19(B cells) Absent
Gotcha!
Not a SCID, it’s X-linked agammaglobulinemia (XLA)
Summary
Genetic primary immunodeficiency with absent cellular and humoral immunity. Regardless of underlying molecular genetic mutation clinical presentation is similar.
Presents prior to six months of age with recurrent diarrhea, pneumonia, fungal cutaneous infections and failure to thrive
Lymphopenic (6 months old < 4000 ug/L) and low TREC count
Rule out DiGeorge 22q11 (thymic transplant)
Remember preventive measures: reverse isolation, NO live vaccines, irradiated CMV(-) blood products, PCP prophylaxis
MSD is preferred treatment. Gene therapy is evolving as preferred treatment over unmatched donors.