Sepsis Procalcitonin and Sepsis - Ortho Clinical Diagnostics
sepsis
-
Upload
free-education-for-all -
Category
Education
-
view
173 -
download
0
Transcript of sepsis

Sepsis: principles of pathophysiology and animal models
Corso di Medicina Interna
Dott. Luigi Mario Castello

EPIDEMIOLOGY
The incidences of severe sepsis and septic shock are rising worldwide due to:• aging of population• survival increase of patients with chronic conditions• immunosuppressive therapy• implantation of vascular catheters, PM, defibrillators, prosthetic devices• HIV infection and malnutrition (especially in poor countries)
Sepsis causes more than 200.000 deaths per year in US
In about 2/3 of cases sepsis affects subjects with chronic diseases
Advanced age and the presence of pre-existing conditions adversely affect the prognosis.

INFECTIONPenetration and proliferation of microorganisms in a tissue.
The presence of microorganisms can be confirmed with a culture of a biological fluid sample (urine, sputum, wound exudate)
BACTEREMIA
Presence of bacteria in the bloodstream.
Bacteremia can be confirmed performing a blood culture which allows to identify the bacterial strain and to perform antibiogram.

EUCAST OBJECTIVES
www.eucast.org
• To form in EUCAST, under the auspices of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the European Centre
for Disease Prevention and Control (ECDC), a network of established experts in the determination of antimicrobial breakpoints and in antimicrobial susceptibility testing.
• To determine, review and revise European clinical breakpoints and epidemiological cut-off values for surveillance of antimicrobial resistance in close collaboration with the European Medicines Agency (EMA) and ECDC.
• To promote the development and standardization of in-vitro antimicrobial susceptibility testing methods used in Europe.
• To promote quality assurance of in-vitro antimicrobial susceptibility testing.• To promote education and training in antimicrobial susceptibility testing.• To advise ECDC and other European Union health agencies on issues related
to antimicrobial susceptibility testing and detection of resistance determinants relevant to public health.
• To collaborate with international groups, ECDC and other European Union health agencies involved in antimicrobial susceptibility testing and/or the epidemiology of antimicrobial resistance in human pathogens.
• To work towards international consensus and harmonization of clinical breakpoints and antimicrobial susceptibility testing.

ANTIBIOGRAM
Definition: in vitro antimicrobial susceptibility test
Semi-quantitative method: based on diffusion (Kirby-Bauer method); small discs containing different antibiotics, are dropped in different zones of the culture on an agar plate. The antibiotic will diffuse in the area surrounding each tablet, and a disc of bacterial lysis will become visible. Since the concentration of the antibiotic was the highest at the centre, and the lowest at the edge of this zone, the diameter is suggestive for the Minimum Inhibitory Concentration, or MIC, (conversion of the diameter in millimeter to the MIC, in µg/ml, is based on known linear regression curves).

Quantitative method: is based on dilution; a dilution series of antibiotics is established (this is a series of reaction vials with progressively lower concentrations of the tested antibiotic). The last vial in which no bacteria grow contains the antibiotic at the Minimal Inhibiting Concentration (MIC).
This is the reference method for antimicrobial susceptibility testing.
It rely on incremental dilution of the antimicrobial agents to determine the minimum inhibitory concentrations (MICs)
ANTIBIOGRAM

ANTIBIOGRAM: DILUTION METHOD

Epidemiological cut-off
Clinical breakpoints
% microorganism

Epidemiological cut-off
EUCAST: EPIDEMIOLOGICAL CUT-OFF

EUCAST: CLINICAL BREAKPOINTS

MICs are expressed in mg/L or mg/mL
Epidemiological cut-off: a micro-organism is defined as wild type (WT) for a species by the absence of acquired and mutational resistance mechanisms to the drug in question
MICs values allows to define the isolated bacterial strain as sensitive, intermediate or resistant to the tested antibiotic
Resistant: poor or no probability to successfully treat the infection with the tested antibiotic
Intermediate: uncertain probability to successfully treat the infection with the tested antibiotic
Sensitive: good probability to successfully treat the infection with the tested antibiotic
CLINICAL USE OF ANTIBIOGRAM RESULTS

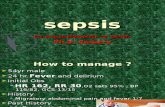
• SIRS (systemic inflammatory response syndrome) is characterized by at least two of the following:– fever (T > 38 °C) or hypothermia (T < 36 °C)– tachypnea (RR > 24 min-1 or PaCO2 < 32 mm Hg)
– tachycardia (HR > 90 min-1)– Leukocytosis (WBC > 12,000 mL-1) or leukopenia
(WBC < 4.000 mL-1)
• Sepsis: SIRS with an infectious cause
DEFINITIONS


• Severe sepsis: sepsis with signs of organ damage: – Hypotension– Oliguria (urine output < 500 mL/24 hours)– Respiratory failure– Low platlets count– Severe metabolic acidosis (mainly due to lactic
acid production)
DEFINITIONS

Septic shock:
Sepsis with hypotension requiring fluid resuscitascion and vasopressor administration (dopamine, epinephrine or norepinephrine).
Multiple organ dysfunction syndrome (MODS): Loss of function of at least two organs in an acutely ill patient requiring a prompt medical intervention to achieve homeostasis.
DEFINITIONS

RISK STRATIFICATION
Severesepsis
Localized infection
Death
Fever, increase of HR and RRSystemic response
Organ damage
Hypotension and Shock
Septic shockCLINICAL
DETERIORATION

INFECTIONS
PATHOGEN IMMUNE SYSTEM
CLINICAL MANIFESTATION
Toxines Cytokines
Other inflammatory mediators

EARLY PHASE
LATE PHASE
PHASES OF SEPSIS

EARLY PHASE
Hyperdynamic phase:• Low systemic vascular resistance• Initial increase in cardiac output• Sepsis progression leads to a gradual reduction
of CO without changes of peripheral vascular resistance
• Haemodynamic derangement

LATE PHASE
HYPODINAMIC PHASE• Low Cardiac Output (CO)• Low Vascular Resistences
MULTI ORGAN DISFUNCTION SYNDROME
(due to hypoperfusion with low oxygen delivery to tissues)

Imuune response to the lipid A moiety of lipopolysaccharide (LPS, also called endotoxin). A host protein (LPS-binding protein) binds lipid A and transfers the LPS to CD14 on the surfaces of monocytes, macrophages, and neutrophils. LPS then is passed to MD-2, that is bound to toll-like receptor (TLR) 4 to form a molecular complex that transduces the LPS recognition signal into the cell. This signal rapidly triggers the production and release of mediators, such as TNF, that amplify the LPS signal and transmit it to other cells and tissues. Bacterial peptidoglycan and lipopeptides interact with different TLRs. 11 different TLR-based receptor complexes allows animals to recognize many conserved microbial molecules.

Imbalance between:• Proinflammatory agents (prevailing)• Anti-inflammatory agents (decreasing)
This imbalance leads to the onset of the systemic inflammatory response syndrome (SIRS) while the compensatory anti inflammatory response (CARS) is inhibited.
PHATOPHYSIOLOGY OF SEPSIS


Recognition of microbial molecules by tissue
phagocytes
cytokines, chemokines, prostanoids, leukotrienes
increase blood flow to the infected tissue
enhance the permeability of local blood vessels
recruit neutrophils to the site of infection
elicit pain
Systemic responses are activated by neural and/or humoral communication with the hypothalamus and brainstem
enhance local defenses by increasing blood flow to the infected area
Increase the number of circulating neutrophils
elevating blood levels of numerous molecules

TNF- stimulates leukocytes and vascular endothelial cells
Cell-surface molecules that enhance neutrophil-endothelial adhesion at sites of infection
increase prostaglandin and leukotriene production
IL-8 and IL-17 attract circulating neutrophils to the infection site
TNF- , IL-1β, IFN , IL-12, IL-17
interact synergistically with one another and with additional mediators
Endothelial cells and leukocytes
nitric oxide (NO) by activated VEC
vasodilation
prostaglandin I2
thromboxane A2

ANIMAL MODELS FOR THE STUDY OF OF SEPSIS

STRATEGIES
• TOXIN ADMINISTRATION (LPS)• INOCULUM OF BACTERIA• ALTERATION OF A PROTECTIVE BARRIER
(translocation of faecal bacteria from the colon)

TOXIN ADMINISTRATION
• The administration of Toll Like Receptor (TLR) agonists induces septic shock in mice.
• The model in simple.• Low dose LPS administration is the most commonly
used approach

LIMITS
• The evolution of the shock is very quick• Some phases observed in humans are lacking• LPS injection may induce the hypodynamic phase of
the shock immediately; the hyperdynamic phase is skipped.
• A continuous infusion of low dose LPS can be used to induce the hyperdynamic phase but this approach is difficult to manage in mice.

EXOGENOUS ADMINISTRATION OF INFECTIOUS AGENTS
Monomicrobial or polymircobial infections
Sites for the inoculum:• Bloodstream (intreavenous)• Peritoneum• Airways

LIMITS AND CONFOUNDING FACTORS
• The administration of high doses of bacteria often lead to a model of intoxication, characterized by a rapid complement mediated lysis, rather than to a reliable model of infection (toxicosis response)
• Different bacterial loads can induce different responses
• The bacteria virulence can affect the results• Different host response depending on the injection
site• Variability linked to the infusion time of the bacteria


ALTERATION OF A PROTECTIVE BARRIER

CAECAL LIGATION AND PUNCTURE
(CLP)The CLP model consists of the perforation of the cecum allowing the release of fecal material into the peritoneal cavity to generate an exacerbated immune response induced by polymicrobial infection.
This model reproduces the most important clinical conditions observed in humans. As in humans, mice that undergo CLP with fluid resuscitation show the first (early) hyperdynamic phase that progresses to the second (late) hypodynamic phase.
The cytokine profile is similar to that seen in human sepsis where there is increased lymphocyte apoptosis.
Due to the multiple and overlapping mechanisms involved in sepsis, researchers need a suitable sepsis model of controlled severity in order to obtain consistent and reproducible results.

METHOD
• Anesthetize the mouse, shave the abdomen and disinfect area• Under aseptic conditions, practice a 1 to 2 cm midline laparotomy and expose the cecum with
adjoining intestine• The cecum is tightly ligated with a silk suture at its base below the ileo-cecal valve, and is
perforated once or twice with a 19-gauge needle. A distance of >1cm produces high grade sepsis while a distance of ≤1 cm produces mid-to-low grade sepsis.
• The cecum is then gently squeezed to extrude a small amount of feces from the perforation sites. The cecum is returned to the peritoneal cavity and the peritoneum and the skin are closed with 6.0 silk sutures.
• Resuscitate mice by injecting subcutaneously 1 ml of pre-warmed 0.9% saline solution using a 25G needle. This fluid resuscitation measure will induce the hyperdynamic phase of sepsis.
• Inject subcutaneously buprenorphine (0.05mg/ kg body weight) or tramadol (20mg/kg body weight) for post operative analgesia.
• The animals are placed temporarily on a heating pad or alternatively returned immediately to a cage with exposure to an infrared heating lamp of 150W until they recover from the anesthesia. The recovery time is from 30 min to 1 hour.
• Provide free access to food and water (hydrogel) placed on the bottom of the cage.• Mice are monitored every 12 hours for survival for one to two weeks or euthanized at different time
points for analysis of different parameters.



MAIN ADVANTAGES OF CLP
The technique is relatively simple and cheap
The model reproduces reliably the different phases of sepsis
The degree of severity may be regulated (length of ligated cecum, diameter of the needle used and number of holes)
The model can be used for different experimental settings (pathophysiology, biomarkers, drugs efficacy, survival studies).
The sacrifice of mice may be performed after a few hours up to a maximum of 28 days
Blood and different tissue samples may be obtained to study proteins, gene activation, signal transduction, organ damage…

LIMITS OF CLP
In some cases the infection may be confined with the formation of pericecal abscesses
The model is characterized by a certain degree of variability that is not easy to control (quantity of feces extruded from the perforation site)
A large number of variables are involved (anesthesia, fluid resuscitation, surgical complications)

COLON ASCENDENS
STENT PERITONITIS
CASP model shows some differences with respect to CLP
The main difference is the insertion of a stent with defined diameter into the ascending colon.
This lead to a constant passage of feces from the colon to peritoneal cavity avoiding abscess formation (the infection can’t be limited).

METHODThe ascending colon is exposed and a catheter (16- gauge) is inserted through the antimesenteric wall into the lumen of the ascending colon and is fixed with two sutures (7/0 Ethilon thread). The inner needle of the stent was removed and the stent was cut 2 mm above the puncture site.
To ensure proper intraluminal positioning of the stent, stool was milked from the cecum into the stent until a small amount appeared.
Stent is then removed 3-9 hours after the implant


CASP VS CLP
The CASP model mimics closely the clinical course of diffuse peritonitis with early and steadily increasing systemic infection and inflammation (systemic inflammatory response syndrome).
CLP reveals a model of intra-abdominal abscess formation with sustained and minor signs of systemic inflammation.