script … · Web viewPP slide 32. Immunization section ... dashboard of patient assignment while...
Transcript of script … · Web viewPP slide 32. Immunization section ... dashboard of patient assignment while...
VCH Admission History Data Base Changes
(BLUE TEXT =WHAT IS SAIDRED = something the facilitator for that session DOESGREEN = Audiovisual/HandoutPURPLE = Handout)
(Group Work/Activity)
Arrange tables and name tents by sss rep area.
As learners arrive :
Sign in on the roster
Pick up handout packet
Sit at table with your SSS rep for your area
Passout the slips of paper for what staff said activity
CAPS/SSS Rep
Units
Val Kibler
RW 3,4,5,6
Spring
ED- adult & Peds
Tom Mack
8N,8S 8T3
Ron Reed
678 vch, 5N
Lisa Grunwald
4A
Lillian McGehee
9N, 9S, 9T3
Heather Freeman
6T3, 6N
Sylinda Littlejohn
Sara Turcotte
PCCU
Nola Vest
10N STU
Stephanie
7N 5S 6S COBS
Kathy Rynczack
7RW TOBS crc
Debi Camp
11s
Joanne
10S, 11N, 4N&S
Laurel Roberts
4E
Gwen Holder
registry, vch pool
https://startest6.mc.vanderbilt.edu/cgi-bin/form-generator/sp/index.cgi?login
log-in with RACF
use MR# 18754309: Charlotte Ztest
Go to Forms
Search for nursing_admission_hx
I. Intro- 5-10 min. Susan or Connie
PP Slide # 2
Good morning and thank you for coming.
a. We have a track record of successfully changing nursing documentation HED, AdminRx, Priority Problems and OPC implementations but we keep adding to the documentation burden without taking anything away or carefully examining what is critical for quality of care for our patients or to meet regulatory /payor requirements. IT IS CRITICAL THAT WE BEGIN TO DO THAT.
b. We are starting to look at other ways to standardize and simplify work and exchange information electronically.
c. We have heard the complaints from our patients who say they are repeatedly asked the same questions.
d. We have heard the complaints from the nurses about the admission process and the need for admission history revisions
e. We have heard from regulatory agencies like CMS and our payors that we need to do more to assure quality patient care like
i. Offer vaccinations to decrease pneumonia and flu outbreaks
ii. Making the information we collect meaningful and sharing that information electronically with all those that need to have it.
f. The Admission History process was been carefully examined and then revised to address concerns. This morning you will learn about those changes. The revisions that are more than changing questions on a form that gets electronically filed and no one ever looks at again.
It is a change in philosophy
i. instead of completing a form we are collecting data for a data base a data base in that they information will be shared and seen by others involved in the patients care and some data carried forward for future admissions.
ii. Instead of documenting the admission history data within 8 hours, data will be gathered in time frames more aligned with when the data will be needed and completed within 24 hours (that is regulated by JCAHO). A dashboard will be used to help staff complete the admission history data base.
g. But as with any change, it is no good if staff dont use it. YOU ARE CRITICAL in assuring adoption. SSS has designed some tools to help assist you in training and implementing these changes on your units. Today you will begin to plan how to help your staff adopt these changes. I know it is difficult with so many competing priorities but this is worth doing it will help our patients and help our staff.
II. Participant Objectives : Gwen
PP Slide # 3 Handout: 1 objectives
Today we will cover the
Why->What->How as it relates to admission Hx changes
We will not be discussing the content of the admission history form. That has been frozen so that we can begin training and implement.
After the implementation, feedback will be gathered re: content but the committee has reviewed the content with a fine tooth comb and there is NO Fluff or item that can be removed.
By the end of the session the leaders will:
Identify concerns with current process and steps taken with new process to address concerns
State the change in philosophy related to collecting data upon admission
Commit to need for change
Describe changes to admission history data base including
3 phases of data collection and associated time frames
Immunizations
Compliance with new visitor policy and documentation of support person
Reminders for nurses via indicator on whiteboard
Auto generated orders for ancillaries for positive screens
Begin a unit-specific training and implementation plan ( template provided)
State resources and tools that are available to assist with education and support of implementation scheduled for 11/29/11.
III. Logistics for meeting
a. Weve asked you to sit with the CAPS or Systems Support Services Rep. designated to support your unit. This is so you can begin to work together on your unit specific plans.
b. At intervals throughout the you will be given time to begin a unit-specific Implementation Plan you will use on your unit
c. We ask that you honor timeframes so that we may complete the planned agenda on time
d. Jot down questions and ah-hahs as you go so you dont lose them. If there are any issues we are not able to address today, we will put on Parking Lot for follow up after the session.
IV. Roles and Responsibilities & Materials
PP Slide # 4
a. SSS :
In addition to this session for unit leadership, sss will provide
CAPS or Systems Support Services Rep. designated to support your unit will be a resource for your leadership team as you work to educate and implement these changes.
During implementation your SSS person will round in your area but since the implementation on Nov 29th is for all of VCH ( except NICU) they will not be able to remain on your unit the entire shift.
Materials: ( most in your handout packet )
Unit Implementation plan template you will be working on today during the session
Copies of the policies ( some still in draft form)
Training Aides to post for staff
Video clip : changes to admission history that highlights the new areas- on sss web site
Practice scenario for staff to complete on a training patient leadership can look at this training patients admit hx forms and see who has practiced. You can use this as a competency check if you like but not required
Training patients name and MRN
LMS module for staff that work infrequently or you just cant get to in person training
FAQ on sss web site will also post all these other resources on the web site.
Flyers re: debriefings
b. Leadership on the Unit is responsible for
Assess current workflow and impact of changes
Conduct unit education and assure staff complete practice scenario
Support during implementation- ( ie identify who will review admission hxs indicators, rounding or 1on 1 f/u with staff , reviewing the dashboard) and assuring staff have a go to person working if they have ?s
Leadership to round during implementation to elicit feedback and monitor progress.
Note: The Nursing admission Hx committee felt very strongly that a LMS module was not the best option for training; that the training should be done in small groups or during staff meetings etc.
Attending debriefing sessions to present issues and concerns and if absent reading the minutes.
Nov 16 730-8 CVICU Conf Room
Nov 17 730-8am 11North Conf Room
Nov 18 12noon -1230 11North Conf Room
PP Slide # 5- KAREN
There were several factors that prompted the work on revising the Nursing Admission Hx The QERI ( quality, education, research and informatics) committee was discussing standardization and simplification and prioritizing projects. Shouts from the staff re: dissatisfaction with the Admission history prompted its rise to the top of the priority list.
(Group Work/Activity)Audits revealed that 97% of admission hx were started but only 10% were completed thru the discharge planning section
What else did we hear our staff say those that recd slips as you came in, stand up and tell us ..
( those with slips of paper should stand up and read the following)
Staff C/o it was too long- cant get it done in first 8 hours.
When I am worried about keeping patient alive, dont have time to think about discharge
NO reminders to prompt them to go back in and finish it
Nurses live in HED and dont like having to go into starpanel to document and then into heo wiz to enter order and then back into hed.
Asking patients the same questions others have already asked and then no one looks at the information we spend time collecting
It doesnt track who has entered which piece of data so I just start a new one even if there is a draft- I want the record to reflect what I have done.
PP Slide # 6 The committee found
(Group Work/Activity)Creating a Sense of Urgency
So we heard that staff were unhappy what did you find out from your review of the admission histories done on your unit?
Instructions:
1. Spend 5 minutes discussing at your table your results and findings from your review of the admission histories done on your unit?
2. Begin to fill out your implementation worksheet:
Denote who is responsible for leading the change on your unit as well as your sss resource ( they should be at the table with you)
Jot down thought about how you can create a sense of urgency for making this change with your staff.
Debrief: any big ahhs???
What is the rush? We have to begin reporting out immunization data to cms on Jan 1 we are falling very short of our goal as you will see. So we want to initiate the changes asap and work out the kinks before jan 1.
Create the Coalition
In May of 2011 a committee was formed and chartered to review and revise the admission history forms. Vickie Thompson and I led that group.
The Committee
PP Slide # 7
There were representatives from all areas within VUH and VCH as you can see on this slide
Managing change isnt enough you have to lead it. (Kotter, 1996)
As the Nursing Leaders of VUMC, we must actively LEAD this transformation of practice & documentation
Requires strong leadership & visible support
We cannot manage change from the sidelines
Create at the vision
PP Slide #8
The Objective were to
Collect data once & pass to all systems & users who need to view
Collect data by time it will be needed
Minimize data collection & documentation during critical stabilization period following admission (1st 1-2 hrs.)
Meet minimum regulatory requirements but identify opportunities to alter policies requiring greater than minimum requirements.
Optimum workflow process associated with admission phase of care (up to 24 hrs. max.) will be considered carefully in redesign of documentation tools and processes.
Communicate the Vision:
PP Slide #9
We know that nurses primarily work in HED and the committee tried to format the admission history in HED but it was like trying to fit a square peg in a round hole it just didnt work.
The amount of scrolling back and forth and up and down just made seeing the data collected and what data was missing impossible.
So we went back to starpanel to house the data collected. Eventually the data collected in star will flow into hed and populate the appropriate fields ( ie the ht/wt collected in admission hx will go into the VS tab) but that is not in the phase.
There is a lot of data that will flow to other electronic forms like the opc and team summary and data from Medipac and other sources will pre populate the admission history but you will learn more about that as we go thru the session.
PP Slide #10
There are 4 admission histories
1. adult admit history
2. Peds admit history ( used for pts 18 of less in either vuh or vch)
3. OB admit history- will pull data forward if pts prenatal care done at vumc
4. VPH admit hx- not changing yet
It was identified that the patients that for pts in the cath lab, same day surgery spend less time and therefore there is less time to complete an admission hx and really less data is needed to provider for safe high quality care so a new admit hx for short stay is being designed. It will be completed by the mid point of the patients stay.
If the short stay ends up converting to a regular inpatient status then additional information will be collected. Initially, that means staff will have to start a new admission hx but eventually the data from the short stay admit hx will flow into the admission hx data base for inpts.
For now data collect in the WITT system in the cath lab is available to staff by clicking the link to the PDF report on the OPC.
Data from Periop areas is collected in VPIMS again staff can access this information by clicking on the link to the PDF report on the OPC. In approx 1 year the data from VPMS will populate a shared view of all admit history data in StarPanel.
ED will complete StarPanel Triage Form -If patient is admitted, Admission History database needs to be completed. If not done in ED, needs to be done upon arrival to inpatient unit.
PP Slide #11
The admission hx committee carefully reviewed and removed unnecessary content and We worked with the technical teams to import data and prepoulate the form whenever possible.
At the same time CMS via HiTech, Meaningful Use changes and other regulatory bodies identified content that needed to be added.
Real the net change was 0 it is still long but there is absolutely NO FLUFF everything we are having the nurses collect is needed.
PP Slide #12
Decreased need to toggle into heo/wiz
The other break through was the creation of auto generated orders and alerts that will eliminate the need for nurses to toggle from the admission hx into heo/wiz and enter orders.
Currently if staff identify a positive screen for SW or CM they have to enter an order in heo wiz with these changes, the CM/SW will be alerted without the nurse having to enter anything in heo /wiz.
PP Slide #13
Not a form to complete but data to collect it is an Admission History DATA BASE.
Religion, tobacco status and other info stored and retrieved on subsequent admissions
Data displayed on OPC, Team Summary, Ancillary Dashboards
Positive screens will alert the appropriate department for instance a Social Work screen generates Social Work notification
Immunization screen generates order for vaccine and scheduled for 10am next am in admin rx. Currently, a nurse would have to contact the provider and then enter the order in heo wiz and the vaccine is entered to be given on discharge. This shows up as prn in admin rx so many vaccines are missed in the hurry to get patients discharged.
PP Slide #14
Each piece of data will have the electronic signature of the person who entered that data
Open the admission Hx in the Edit Mode and scroll to the bottom . Click signatures.
If a correction is needed or additional information added from a different person the name of the person collecting each piece is visible
CLICK TO GET ZOOMED IN VIEW OF SLIDE
PP Slide #15
Many eyes will see that data that is collected on the admission history.
PP Slide #16
Currently, data collected flows on to the opc but with the revisions more data will go to the opc. Data will also be sent to dashboards for ancillary services, be placed on team summary. Eventually will feed readmission risk scale and flow into HED
Others may not open the admission hx form in star but see the data in a way that is good for their workflow.
PP Slide #17
Reminders
Currently, unless staff opens the admission hx in star panel they have no way of knowing if all the data has been collected or not.
Indicators on the inpt white board will now help remind staff when portions are incomplete.
Hover over indicator to see what Admission requirement is not yet completed (ie section 1,2,3 or Flu or Pneumovax screening)
PP Slide #18
Currently, staffs are supposed to complete the entire admission history in 8 hours. This has been changed and now staff have 24hours to complete.
The collection of data has been divided into 3 sections; each with different time frames for collection because not all information is needed immediately, especially if the patient is critical.
Section I- contains items that are critical for safe care. And should be collected by end of second hour of stay.
Section II contains items related to the plan of care and should be collected by the end of the eight hour
Section III contains items that are related to discharge plan& functional screens. It should be completed within 24h ( regulatory requirement )
transition to Gwen
PP Slide 19
Critical for safe care
Many of these elements have not changed- allergies, PAML etc.
WE will be highlighting the most important changes to the admit history.
Staff are already accustom to how the form works, ie if you select a certain response you might get an expanded set of items to address.
PP Slide 20
Contact information
New visitor policy: patient is allowed to have support person stay with them 24/7 so we ask who will be staying with the patient
We also need to identify more specifically who we may give information too, who should get instructions re: d/c and who will drive the patient home. These will help facilitate effective d/c teaching and a smooth discharge.
Assuring we are teaching those involved in the patients care post discharge can also help prevent readmissions.
Data will be shown on OPC initially and then other electronic documents later
Note ability to re-use name, phone number, relationship if same as Support Person.
PP slide 21
Legal Documents-
Will ask patients if this is already in the EMR, if family is providing it and we need to scan it in the emr or if family has been instructed to bring document. It doesnt do any good to know the pt has an advanced directive if we dont have it on see the content.
PP slide 22
New Present on Admission Screening-
Awareness is key to improved communication among team members.
Positives will trigger various decision support responses:
PP Slide 23
Pacemaker/ICD triggers HEO decision support w/ MRI orders
Dialysis prohibits some renal dose adjustment warnings in HEO
CPAP home use will trigger protocol order for Respiratory Care evaluation
Medication Pump usage will be shared as appropriate with other disciplines
Patient Pregnant, Patient Lactating sent to Pharmacy for decision support on medications.
PP slide 24
CPAP Summary What You Need to Know
In the past year we have reviewed several cases with negative outcomes, where there was some evidence in the record that indicated the patient had obstructive sleep apnea(OSA) and routinely wore Continuous Positive Airway Pressure (CPAP) at home. Currently we do not have a standardized method of assessment and ordering of Home CPAP, several of these patients actually brought their machines, but therapy was not initiated.
Most care providers are unaware of obstructive sleep apnea(OSA), its effect on the patient at baseline and impact for when the patient is hospitalized(narcotics, sedatives, etc).
The Goal of the POA question is to identify known CPAP user upon admission and engage the respiratory therapist in the care and management of this patients respiratory needs - -a single click will initiate the Home CPAP Evaluation and Initiation protocol and send a message to respiratory therapy and the patients provider.
This is first phase of work - -if you use CPAP at home, we want you to use CPAP in the hospital. In future work we will target patients at risk for OSA. We need to stress to staff the importance of knowing the information and using this data in a meaningful way.
Patients that use CPAP at home need to use CPAP in the Hospital
RT will evaluate machine - will probably use VUMC equipment to assure proper functioning
In addition:
Increased vigilance when general anesthesia, sedation, or intravenous (IV) analgesia/opioids are required.
Elevate head of bed 30-40 degrees if not contraindicated
Communicate that the patient has obstructive sleep apnea during handover to other care providers as well as in transfer to ancillary departments
PP slide 25
Saving as Draft vs Saving as Final
Leaving a question blank or selecting Unable to complete triggers indicators on the inpatient whiteboard.
At the end of each section staff will be asked to validate data electronically imported ( per regulatory requirements)
Saving as Draft ( this will be the most common when form is complete save as Final)
Saves in StarPanel, generates HEO/WIZ orders prn and updates electronic documents and dashboard
Other Nurses can document additional information
Triggers indicators
Will display alert if all questions are not completed
PP slide 26
Saving as Final
Saves in StarPanel, generates HEO/WIZ orders prn and updates electronic documents
Do ONLY after all 3 sections completed
Additional edit must be done in an amendment
Triggers indicators
PP slide 27
Next Section is related to plan of care and should be completed in approximately 6 hours to enable development of individualized Plan of Care within 8 hours of the patients arrival.
PP slide 28
Past Medical Surgical information
Past Medical & Surgical History information is imported and can be displayed by clicking on the link. The patient summary is displayed.
It is the Provider responsibility to enter this information but the nurse needs to review.
PP Slide 29
Tobacco use screening
An increased emphasis has been placed on screening our patient and collecting meaningful information about their usage. The admit hx has now been formatted to remind staff to question the patient re: frequency of use.
PP slide 30
The Opportunity: Centers for Medicare & Medicaid Services (CMS) has recognized the opportunity to reduce or eliminate preventable illnesses such as influenza and pneumonia with a standardized approach to providing vaccines.
Our responsibility is to screen patients for appropriate vaccines and offer vaccines to patients that meet positive screening criteria.
Patients always have the right to decline.
PP Slide 31
5% - 20% of population in US gets the flu
200,000 people are hospitalized from seasonal flu-related complications
between 1976 -2006, flu-associated deaths range from a low of about 3,000 to a high of about 49,000 people.
The 2011-2012 flu vaccine will protect against the three influenza viruses that research indicates will be most common during the season. This includes an influenza A (H1N1) virus, an influenza A (H3N2) virus, and an influenza B virus.
Flu season October till March 1 and everyone six months and older should get vaccinated. The admission hx has been formatted to only display the flu related items during this time frame.
PP slide 32
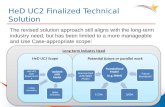
Immunization section of admission hx is one of the major areas of change.
An important component is that there is now a nurse driven protocol and when the patient is identified as needing an immunizations an order is automatically generated in heo/wiz and the vaccine is scheduled in admin rx to be given the following am at 1000.
Link to the immunization record. open this up prior to proceeding to complete this section. It opens in window below so can easily see the pts record. If you need to document Immunization history other than Flu, use historical entry option and you will be able to enter uncertified vaccines. (Flu and history will populate automatically from the screens if already given AND data of admin. Known.)
PP slide 33
There are certain times that the immunization screening will not be completed:
Stat Name pts-because the birthdate is inaccurate for those patients and the rules to trigger questions will not work accurately. Once STAT name replaced with patients real name, can screen for Flu need
Patient unable to provide a hx comatose, cognitive issues
PP Slide 34
In the future.If selected that pt has had an immunization, it will update the immunization record as a historical vaccine.
Positive screens will result in an order for the flu vaccine being automatically generated in HEO/WIZ when the admission history is saved. The vaccine will be scheduled in Admin Rx with frequency of 1XBYRX and Pharmacist will administer ( VCH ONLY). The pharmacist will bring the medication instead of sending it to the unit. This should help decrease confusion re: nurse administering. Pharmacist only works Mon-Fri.
PCCU, heme/onc, ID, rheumatology and cardiology patients who qualify for the flu shot will have alert sent to a StarPanel worklist and be evaluated by the physician staff/clinical pharmacy.
PRETTY COOL.
PP slide 35
Care Organizer and Admin Rx will list the frequency for the vaccine as 1X by RX to indicate that the Pharmacist will administer.
The pharmacist will bring medication instead of it being delivered.
PP Slide 36
There are other screenings if the screening is negative, staff will need to identify that there are no problems. This is to assure that it is truly a negative screen vs just not answered.
Just as before there is a different selection in nutrition screening based upon age of the child.
PP Slide 37
Positive screens will trigger notification to the appropriate department here is an example of the nutrition dashboard but there will also be a SW, CM and other dashboards created to facilitate communication.
In the current process, staff have to open up heo/wiz and place an order to notify the ancillary department of a positive screen an order isnt required but it is the only electronic means we had to communicate up til now.
PP Slide 38
Learning Readiness /ADL
Information will display on OPC and eventually feed Readmission screen and Patient Education and Engagement Record (PEER)
PP Slide 39
Child Life Screening
Child Life will be electronically alerted to children with needs Nurses do not need to enter an order in HEO/Wiz.
PP Slide 40
The third and final section relates to discharge and functional screens. It should be completed within approximately 22 hours of admission to allow for development of a Discharge Plan within 24 hrs. of admission (per policy).
PP Slide 41
Positive screens for rehab services require a provider orders; the provider will be alerted to the positive screen so that a decision can then be made re: placing an order.
The nurse will not have to notify the provider.
Use the Complete button ONLY WHEN ALL THE DATA HAS BEEN COLLECTED
PP Slide 42
Can I do all sections at once OF COURSE
The admit history may be completed at one time if that is practical.
Important thing is to get the data collected.
Previously all data had to be collected within 8 hours.
Now have up to 24hrs to collect.
PP Slide 43
Currently, it is not in the nurses workflow to verify if the admission history is complete. Remember our audits showed 97% of the time it was initiated but only 10% of time completed.
Indicators on the whiteboard have been created to help remind staff when the admit hx is incomplete. Hovering over the indicator will display the portion that is incomplete.
PP Slide 44
We need to emphasize to staff- the most import thing is collecting the data- even if it is more than 24hours after admission.
PP Slide 45
Future Enhancements: Notification Bar
Notification Bar at top of CWS to all display dashboard of patient assignment while in HED or HEO/WIZ or any application. This will make it easier to see indicators and to navigate
Braden Tool in HED instead of HEO/WIZ is projected to be available soon
(Group Work/ActivityPractice Scenario15min)
Weve been talking about the changes now is your time to actually practice.
Instructions:
At your table, use the laptop to access starpanel and complete the practice scenario that is in your packet. Use one of the training patients for your area.
Your SSS rep will help get starpanel pulled up and with any questions you have.
Well take 15 minutes to do this.
Admission History Changes
This Practice Scenario highlights some of the changes to the Admission History. Please complete it before Nov 29th so that you become familiar with the revisions.
(IMPORTANT Do NOT use real patients for practice!)
Instructions:
1. Open StarPanel from a Clinical Workstation (CWS)
2. Type one of the MRNs designated for your unit :
3. Document the data below on the 14 year old patient that is being admitted to your unit. Some data will be pre-populated in the Admission History.
SECTION 1:
Complete prior to initiation of treatment (which must be started within 2 hours of admission or as appropriate for short stay patients)
a. Data Collected today click calendar icon to select date.
b. Admitted today @ 0850 from the ED
c. Historian is patient and his mom, Morgan Jones. Her cell phone is 615-888-8888 and she will be his designated support person.
Note: this information will display on the OPC and various places.
d. Advanced Directive and Living Will were scanned into StarPanel at his last clinic visit.
e. Add an allergy that is not already entered and delete one by clicking on the red X.
f. Present on Admission Screening - Patient uses CPAP machine at home and brought it with him.
Note: this data will trigger an alert to RT to follow-up with the patient. It will also display on the OPC and should be conveyed during handovers.
g. Uses other medical equipment at home - 02 Nasal Cannula 1L prn.
Note: this information will alert Case Manager to follow up with the patient
h. Select I verify the pre-populated data has been reviewed for accuracy but do NOT Save as Draft since you will continue your practice on the other 2 sections.
Note: Verification of data imported from other sources and necessary corrections are very important.
Note: If a section cannot be completed (patient unconscious or critically ill, family not present to give information) select unable to complete. This will trigger a reminder to display on the inpatient whiteboard.
SECTION 2:
Complete prior to initiation of plan of care (which must be started within 8 hours of admission or as appropriate for short stay patients)
a. Click to view Problem list
b. Click to open Immunization Record.
Note: Will open in the bottom frame and allow you to view/edit while completing the Immunization Screening section.
1. Flu Immunization Select No to verification of patients age is not < 6 months.
2. Click No to Has patient had flu shot this flu season?
3. Answer legal surrogate question No.
4. Click No to all exclusions
Note: this will generate a protocol order in HEO/WIZ for flu vaccine. It will be scheduled in AdminRx for 1000 the next day.
c. Learning Readiness.
Yes the patient and guardian can read & write
English is primary language
Middle School Education Level
Prefers video instruction
No learning challenges
Note: This information will be displayed on the OPC and eventually will pre-populate a patient education record that is being developed.
d. Select I verify the pre-populated data has been reviewed for accuracy but do NOT Save as Draft since you will continue your practice on the last section.
SECTION 3:
Complete prior to initiation of discharge plan (must be started within 24 hours of admission or as appropriate for shorter stay patients)
a. Patient reports decreased strength in his legs and that he is having trouble getting up from the couch and bed at home.
Note: A positive rehab screen will trigger a physician reminder in HEO/WIZ to consider a rehab consult.
b. Select a Positive Case Management response
Note: This will prompt a Case Management consult.
c. Select I verify the pre-populated data has been reviewed for accuracy
You will not be able to save this form since you are in the training mode.
Let your leadership team know that you have completed this practice.
Provide 3 minute warning
How to train and implement these changes- Karen
According to the 2005 Change Management Best Practice Report.
One-on-one face to face discussions that are honest and straight forward and that offer details of the change on a personal level
Cascading small group meetings to share information, brainstorm solutions and implement new processes
(Group Work/ActivityUnit Implementation Plan20 min.)
At your table for next 20 minutes discuss
Who should be included in your units coalition for change? Who will be involved and help with getting the training done and be a resource during implementation
How the leadership team will visibly demonstrate support for this change.
Identify for your area the general plan to get staff trained. be specific and include timeframes What resources that SSS provides will you use? specific communication plan
Record your plan on the Implementation Worksheet
Provide 1 minute warning
Removing Obstacles & Empowering Action PP Slide #46
a. Leadership must be committed to the change and ALL leadership must be on the same page. Communication from leadership must be consistently the same message. No mixed messages!
b. Hand-pick leaders who are respected by their peers. RNs receive training on how to communicate the advantages of the new process.
For example, it takes 5 positive encounters to overcome 1 negative encounter and nurses spreading the word and demoing how the system is changing should be schooled on how to present the change in a positive manner. They must also believe that the change will improve patient care and continuity of care.
(Group Work/Activity10 min.)
Identify obstacles to remove and develop action plans
Record your plan on the Implementation Plan in your packet
Provide 1 minute warning
Debrief- discussionWhat are some of obstacles and action plans
Create Short Term Wins, Build on the Change & Anchor the Change in culture
Nothing motivates more than success. We need to define and engineer visible performance improvement.
PP Slide #47
Ask the group and allow them to call out answers jot down options that apply to their area.
What are some of the short term wins you hope to see when the changes are implemented? List out 3
How do you think we can hard wire this change?
1. How did you hard wire the change in the past ?
2. What were the challenges to adoption?
Next Steps
PP Slide #48
Trainer Note for VCH there is No Need to Customize the admission history practice scenario
1. Discuss with leadership team and finalize training / support plans.
2. Conduct Training
3. Print and distribute practice scenario
4. Monitor practice by staff
5. Round during implementation
6. Post Debriefing flyer and encourage attendance
PP Slide #49
4. Assess which other resources you might want to use
a. Training aides- you can print
b. Web Based Resources
1) SSS web site- will have short video click of changes as well as all the documents that you have seen today.
2) LMS Module- Title Admission History Changes 2011
PP Slide #50
Mark your calendar with the import dates
More Sessions like this one
11/8 Tue 3p-5p B319 makeup
11/15 730-930 am B319 makeup
Implementation 11/29 Tue
SSS will make rounds
Call Help desk (3-3457) if need assistance
Debriefing Sessions
Nov 29th Tue 4-430pm
Nov 30th Wed 2-230 pm
Dec 1 Thur 730-8am
Conclusion Karen
Thank you for your time and your hard work. Clearly, we were not able to complete all portions of your unit plan for implementing the admission history changes but we hope you are off to a good start and can work with your SSS resource person when you have questions arise.
We will be following up on items we put in our parking lot/bin list and expect to have the LMS module ready by the end of the month. The sss web site will have all the resources posted by end of day Friday we wanted to present it once before posting on the web.
17